Abstract
Objectives
Impulsivity has been identified as an important construct in predicting the initiation and maintenance of substance use among at-risk populations. Interventions emphasizing mindfulness strategies appear particularly promising in reducing substance use and marking change in various aspects of impulsivity.
Methods
The current study used a rolling group mindfulness-based relapse prevention (MBRP) intervention for young adults in residential substance use disorder treatment. We examined change in impulsivity facets measured by the S-UPPS for youth randomly assigned to MBRP (n = 45) versus those assigned to treatment as usual plus 12 step/self-help (n = 34). We also examined how change in impulsivity mediated changes in substance use post-treatment.
Results
In general, results indicated that MBRP is effective at reducing facets of trait impulsivity in treatment-seeking individuals with SUDs. Only positive and negative urgency mediated the relation between treatment assignment and substance use.
Conclusions
MBRP is a viable and useful intervention for young adults in residential treatment for substance use disorders and can aid in marked change in facets of impulsivity. Both positive and negative urgency were significant mechanisms of change in reducing substance use following treatment. Results are discussed focused on the utility of MRBP as a clinical intervention for at-risk, marginalized, and young adults.
Keywords: Addiction treatment, Mindfulness, Drug use, Impulsivity, Self-regulation, Emotion regulation
Introduction
Impulsivity is a multidimensional construct that broadly refers to a tendency towards rapid or unplanned action with a suboptimal regard for future consequences (Brewer and Potenza 2008; Moeller et al. 2001a). Impulsivity is a well-established risk factor for substance use disorders (SUDs) (Verdejo-Garcia et al. 2008; Dawe and Loxton 2004) and SUD treatment outcomes (Winhusen et al. 2013; Loree et al. 2015; Moeller et al. 2001b). Interventions aimed at reducing impulsivity among individuals with SUDs have gained attention among researchers (Conrod et al. 2006). Specifically, interventions emphasizing mindfulness strategies—which aim to increase present moment focus in a non-judgmental, non-reactive, and compassionate manner—appear particularly promising in this regard. Theories of mindfulness suggest that mindfulness strategies like non-reactivity, tolerating distress, and enhancing awareness of urges can strengthen cognitive control and reduce impulsivity. This account is supported by empirical studies showing that mindfulness is negatively correlated with impulsivity (Breslin et al. 2002) and that mindfulness-based interventions have demonstrated effectiveness in reducing both impulsivity and substance use (Tang et al. 2016). In particular, mindfulness-based relapse prevention (MBRP; Bowen et al. 2009) appears to be effective in improving SUD outcomes in samples recently discharged from SUD treatment (Hsu et al. 2013; Witkiewitz et al. 2013a). Although MBRP may effectively reduce impulsivity among individuals in residential SUD treatment, this possibility has not been rigorously investigated. In a study of men in Iran seeking residential treatment for opioid dependence, MBRP was associated with significantly decreased impulsivity (Yaghubi et al. 2017) at post-treatment and at 2-month follow-up. However, the extent to which MBRP changes long-term trajectories of impulsivity dimensions during and after treatment and the effect of these changes on SUD outcomes remain unclear and unstudied.
Marginalized young adults, or those involved in the criminal justice system, child protective services, or those not attending some form of higher education are especially important populations to study. Compared to their peers, marginalized young adults tend to have more difficulty fulfilling adult roles, as evidenced by higher rates of unemployment, higher levels of relationship and housing instability, and more substance use problems (Sussman and Arnett 2014). Marginalized young adults have also been shown to have less favorable substance use treatment outcomes (Davis et al. 2017) and more impulsivity relative to their peers (Chamorro et al. 2012).
Impulsivity is a heterogeneous construct (Caswell et al. 2015) encompassing trait and behavioral facets (King et al. 2014). Past research has empirically derived as few as two and as many as 15 dimensions of trait impulsivity (Kirby and Finch 2010) and even more when considering behavioral components of impulsivity (Stahl et al. 2014). Trait impulsivity is assessed via self-report measures that ask individuals to rate aggregates of their past behavior (e.g., the extent to which one acts quickly without thinking). Conversely, behavioral impulsivity can be further dichotomized into behavioral choice and behavioral response facets (MacKillop et al. 2016). Behavioral choice impulsivity pertains to risky choice and decision-making and is measured by asking individuals to choose between hypothetical smaller, immediate or larger, delayed rewards (e.g., delay discounting; Rachlin and Green 1972). Behavioral response is an individual’s ability to inhibit a motor response (i.e., impulsive action), as is often assessed using the go/no-go or stop signal tasks (Fillmore and Weafer 2013).
In an effort to operationalize facets of trait impulsivity, Whiteside and Lynam (2001) factor analyzed 20 well-established impulsivity and personality-related measures. Results suggested four representative subscales of trait impulsivity, known together as the UPPS, which includes urgency, (lack of) premeditation, (lack of) perseverance, and sensation seeking. More recently, the urgency subscale was revised to include positive and negative urgency facets (UPPS-P; Lynam et al. 2006), increasing the number of potential impulsivity subscales to five. Negative and positive urgency refer to a tendency to engage in rash or unplanned behavior in response to intense negative or positive emotional states, respectively (Lynam et al. 2006). Lack of premeditation is defined as the absence or inability to delay gratification or action in favor of planning or careful thought. For example, individuals with low levels of premeditation typically make decisions without regard for a negative outcome, regardless of past experiences. It is thought that lack of premeditation may be associated with low self-control or a high tolerance for negative consequences of impulsive behavior (Whiteside and Lynam 2001). Lack of perseverance typically refers to the inability to complete tasks. That is, some individuals may have difficulties maintaining attention over long periods of time, reflecting a low sense of responsibility or cognitive difficulties when presented with certain stimuli that require attentional focus (Magid and Colder 2007). Sensation seeking refers to a proclivity towards novelty seeking and is driven, in large part, by positive reinforcement. Behaviors associated with sensation seeking are typically brought on by an anticipated motivation, typically in the form of excitement, arousal, or stimulation, which eventually reinforce engagement in similar behaviors.
Contemporary neurocognitive models posit that both addiction and impulsivity create an imbalance between two systems: the “bottom-up” and the “top-down” system. The bottom-up system, otherwise considered the reactive or impulsive system, tends to be associated with reward processes following a stimulus without consideration of the long-term consequences (Witkiewitz et al. 2013b). Conversely, the top-down system, otherwise known as the regulation or executive system, tends to be associated with planning, cognitive control, and resisting short-term reward in favor of long-term goals (Westbrook et al. 2013). Typically, these top-down processes are able to override most bottom-up interruptions though self-regulatory mechanisms such as delay of gratification, suppression of negative or intrusive thoughts, or inhibition processes (Bechara and Van Der Linden 2005; McClure et al. 2004; Koob and Volkow 2009). Theories of associations between SUD and impulsivity suggest that addiction to one or more substances disrupts this process, such that the bottom-up system overrides the top-down executive control (Koob and Volkow 2009).
Supporting this theoretical model, empirical research indicates that heightened impulsivity is a risk factor associated with the initiation (Verdejo-Garcia et al., 2008) and maintenance of alcohol and drug use among adolescents and young adults (Dick et al. 2010; Lejuez et al. 2010). Specifically, prior research has found that higher impulsivity is associated with earlier initiation of cigarette, alcohol, and cannabis use (Kollins 2003; Chuang et al. 2017). Prior studies also indicate that impulsivity is a risk factor for experimentation, problematic drug use, and an inability to abstain from use (de Wit 2008) and that impulsivity is related to treatment outcomes including higher dropout rates, increased risk for relapse, and more problems associated with substance use after treatment (Loree et al. 2015; Stevens et al. 2014). Conversely, interventions focused on reducing impulsivity may affect substance use and relapse risks. Thus, it follows, impulsivity may be an important mechanism of behavior change for young adults in SUD treatment.
Studies suggest that impulsivity can influence the course of alcohol and substance abuse treatment through several pathways (Loree et al. 2015). For example, individuals who score highly on a variety of impulsivity measures (e.g., Barratt Impulsivity Scale, delay discounting) have higher odds of relapsing during treatment and a lower likelihood of remaining abstinent after completing treatment (Krishnan-Sarin et al. 2007; MacKillop and Kahler 2009). In addition, higher baseline impulsivity has predicted worse outcomes; in one alcohol treatment study, treatment effects were stronger for participants who scored lower on impulsivity measures prior to intervention (Müller et al. 2008). While fewer studies have examined associations between impulsivity and treatment outcomes for other substances, preliminary evidence with individuals addicted to cocaine (Moeller et al. 2001b) and marijuana (Stanger et al. 2012) support the view that impulsivity influences treatment outcomes including treatment completion and abstinence.
Specific dimensions of impulsivity have also been related to alcohol (Coskunpinar et al. 2013), drug use, and treatment-related outcomes (Stevens et al. 2014). For example, in a meta-analysis of 96 studies assessing the association between impulsivity and alcohol use using the UPPS model of impulsivity, negative urgency (r = 0.38) and lack of premeditation (r = 0.37) had the strongest associations with alcohol use disorders (Coskunpinar et al. 2013). Further, sensation seeking (r = 0.38), positive urgency (r = 0.38), and negative urgency (r = 0.34) were associated with alcohol-related problems and higher binge drinking frequency, and lack of perseverance was most strongly associated with drinking quantity (r = 0.28). Additionally, in a review of seven studies examining links between risky decision-making and abstinence/relapse with alcohol and illicit drugs, six showed significant associations (Stevens et al. 2014). Links between various dimensions of impulsivity and specific substances require additional research in various treatment settings and populations.
Because high levels of impulsivity can interfere with SUD interventions (Helstrom et al. 2007) and negatively influence SUD treatment outcomes (Loree et al. 2015; Stevens et al. 2014), mindfulness-based interventions that reduce impulsivity may be particularly helpful adjuncts to SUD interventions. Mindfulness interventions emphasize staying in touch with current experiences rather than avoiding or removing negative stimuli (Chiesa and Serretti 2014). Thus, mindfulness practice may reduce impulsivity through improved awareness of internal experiences (e.g., monitoring impulsive decision-making; Wingrove and Bond 1997) and reduction of experiential avoidance. In a recent meta-analysis, small to moderate correlations were found between trait mindfulness and sensation seeking (r = − 0.15), perseverance (r = − 0.27), positive urgency (r = − 0.44), negative urgency (r = − 0.45), and premeditation (r = − 0.49) (Lu and Huffman 2017). These negative correlations may be due to individuals with low trait mindfulness and scoring high on impulsivity, or vice versa. Other evidence has shown considerable overlap among measures of mindfulness and impulsivity when predicting young adult alcohol use (Murphy and MacKillop 2012), suggesting that reducing impulsivity by increasing mindfulness skills may impact alcohol use outcomes.
MBRP, a recently-developed mindfulness-based intervention for SUDs, integrates mindfulness practice with tangible cognitive-behavioral relapse prevention skills to help individuals cope with stress, anxiety, and ruminating thought processes (Bowen et al. 2009, 2014a). The goal of MBRP is to increase awareness of both internal (e.g., affective, cognitive) and external (e.g., triggers, stressors) processes and, eventually, to tolerate negative affective states through the acknowledgment and acceptance of present moment experience. Several studies have shown support for MBRP in reducing substance use and risk of relapse for adults (Bowen et al. 2014b; Witkiewitz et al. 2014). Fewer MBRP studies have been conducted among young adults receiving SUD treatment specifically (Sancho et al. 2018), but available evidence suggests the efficacy of MBRP in reducing substance use risks for this population (Davis et al. 2018).
Research indicates that MBRP may influence both top-down and bottom-up processes for individuals in SUD treatment (Witkiewitz et al. 2013b). In recent work, individuals in methadone maintenance treatment for opiate use who received MBRP (compared to treatment as usual [TAU]) evidenced reductions (post-test only) in general impulsivity as well as specific subscales including decision-making, acting without thinking, and lack of planning (Yaghubi et al. 2017). Prior research has also found that impulsivity mediates the relation between mindfulness and alcohol-related problems; thus, reductions in impulsivity may be a potential mechanism of the effects of MBRP on substance use outcomes, and specific domains of impulsivity may be particularly important to understand in this regard (Christopher et al. 2013).
Although current research finds small to moderate associations between trait mindfulness and impulsivity (Lu and Huffman 2017), most studies have been cross sectional, which precludes the ability to assess how changes in mindfulness affect changes in impulsivity. Further, trait impulsivity has not been tested as a mechanism of change in mindfulness-based interventions for SUDs. These processes are especially important to study among individuals at heightened risk for impulsive behaviors, such as young adults in residential SUD treatment. The current study contributes to this literature by assessing how MBRP predicts long-term change in the five UPPS-P subscales. We hypothesized that individuals receiving MBRP will evidence decreased impulsivity across all UPPS-P subscales both during the treatment phase (e.g., from study entry to treatment discharge) and post-treatment phase (e.g., from discharge to 6 months follow-up). We also hypothesized that changes in impulsivity for those receiving MBRP would be a mechanism of change predicting post-treatment substance use.
Method
Participants
All participants entering the residential facility had at least one substance use disorder diagnosis. Table 1 presents participant characteristics. The mean age of the sample was 25.3 years (SD = 2.70), just over a third (35.0%) were female, and most (91.3%) were of White race. The majority (90%) of participants were poly-substance users. Further, 65% of clients were unemployed or receiving some form of Social Security entitlements with the median yearly salary reported as $5500. The average length of stay at the treatment facility was 41 (SD = 26.2) days. Most of the participants were referred to the residential facility by criminal justice, probation, or child protective services. We retained 79% of participants through the 6-month post-treatment assessment. There were no differences between those who were lost to follow-up and those who were not in terms of clinical, demographic, or self-reported measures. In the main effects manuscript, we did find that youth assigned to MBRP (versus TAU) showed significantly improved perceived stress, craving, and substance use outcomes during both the treatment phase and post-treatment phase (see Davis et al. 2018 for more information).
Table 1.
Baseline demographic characteristics for MBRP and TAU
| Total M (SD) or n (%) | MBRP M (SD) or n (%) | TAU M (SD) or n (%) | |
|---|---|---|---|
| Participant characteristics | |||
| Days in residential | 41.6 (26.3) | 43.3 (35.1) | 39.3 (30.7) |
| Age | 25.3 (2.70) | 25.3 (2.80) | 25.3 (2.64) |
| Female n (%) | 28 (35.0) | 17 (37.8) | 11 (31.4) |
| Race/ethnicity n (%) | |||
| White | 73 (91.3) | 42 (93.3) | 31 (88.6) |
| African-American | 6 (7.5) | 2 (4.44) | 4(11.3) |
| Native American | 1 (1.25) | 1 (2.22) | |
| Education and employment | |||
| School n (%) | |||
| Not in school | 70 (87.5) | 41 (91.1) | 29 (82.9) |
| Adult educationa | 3 (3.75) | 2 (4.44) | 1 (2.86) |
| 2-year college | 7 (8.75) | 2 (4.44) | 5 (14.29) |
| Last grade completed | 11.9 (1.63) | 11.9 (1.75) | 11.9 (1.48) |
| Employment n (%) | |||
| Full-time | 23 (28.8) | 14(31.1) | 9 (25.7) |
| Part-time | 5 (6.25) | 4 (8.89) | 1 (2.86) |
| Unemployed | 52 (65.0) | 27 (60.0) | 25 (71.43) |
| Salary (median) | 5500 | 6000 | 5000 |
| Salary (mean) | 16,807 (36, 185) | 18, 617 (31,337) | 14, 479 (41, 971) |
| Substance use | |||
| SFSb | 16.1 (9.99) | 14.8 (9.29) | 17.7 (10.7) |
| S-UPPS subscales | |||
| Negative urgency | 3.05 (0.68) | 3.07 (0.67) | 3.08 (0.67) |
| Positive urgency | 2.78 (0.71) | 2.69 (0.62) | 2.67 (0.62) |
| Lack of premeditation | 2.42 (0.61) | 2.51 (0.64) | 2.50 (0.64) |
| Lack of perseverance | 1.92 (0.63) | 1.82 (0.63) | 1.99 (0.62) |
| Sensation seeking | 3.21 (0.68) | 3.18(0.71) | 3.23 (0.67) |
MBRP mindfulness-based relapse prevention, TAU treatment as usual (control condition)
Adult education includes GED classes
SFS is a variable created to contain information on all substances and three substance problem items. The scale calculates the proportion of days each individual uses all 15 substances or experiences problems. These values are averaged and multiplied by 100
Procedure
The study was approved by the University Institutional Review Board. Participants were recruited between September 2015 and November 2016, with follow-up assessments continuing until June 2017. Data for the current study are from a previously completed randomized clinical trial (Davis et al. 2018) investigating the effect of MBRP for young adults in substance use disorder treatment. The study took place at a residential public not-for-profit substance use treatment center in the mid-western USA that provided care to low-income clients with substance use disorders. For more details on the study, study procedure, and treatment fidelity, see Davis et al. 2018).
Recruitment and Consenting
Initial screening included 84 potential participants, of whom 79 were eligible for the study. Eligibility criteria included (a) residency at the treatment center, (b) being aged 18 to 29, (c) proficiency in the English language, and (d) clear cognitive ability to understand and provide consent. Research staff explained that individuals assigned to the experimental group would receive eight additional MBRP group sessions and those assigned to the control group (TAU) would receive eight additional self-help/12-step facilitation groups. Following the intake assessment, participants were randomly assigned to MBRP (n = 44) or TAU (n =35). All participants, regardless of treatment assignment, were given 15 bi-weekly (every 2 weeks) assessments during treatment (baseline, 2 weeks, 1 month) and for 6-month post-treatment (12 assessments). Participants received $10.00 ($150.00 maximum) for each assessment.
MBRP
The experimental group received treatment normally provided by the residential facility as well as eight 1.5-h group sessions of MBRP. Sessions were delivered twice weekly to ensure completion of all 8 sessions. One important difference in our delivery of MBRP compared to the standard version is the use of rolling groups (Witkiewitz et al. 2014). This allowed us to enroll individuals as they entered the residential facility, rather than employ the standard 8-week cohort-based protocol. To orient new group members at each session, a brief orientation was provided (e.g., definition of mindfulness, group expectations, homework assignments) to introduce the basics of mindfulness and key exercises (e.g., the triangle of awareness, the SOBER breathing space). Group size ranged between 3 and 12 participants. Each session was led by two master’s degree-level clinicians who underwent 200 h of training in mindfulness-based interventions and received supervision prior to leading MBRP groups. Each session targeted a specific theme such as attentiveness to personal triggers, present focus awareness, acceptance versus avoidance, responding to emotional and physical experiences in skillful ways, intrusive thought recognition, or kindness in action. Participants were given 20–30 min of homework per day, including guided mindfulness meditations. Briefly, therapist adherence to MBRP protocol was excellent. Data were collected using the MBRP adherence and competence scale (Chawla et al. 2010). More information on treatment fidelity can be found in the original manuscript (Redacted for Review (2018)).
TAU
Control group (TAU) participants received treatment normally provided by the residential facility and were asked to attend up to eight extra social support groups (Alcoholics and Narcotics Anonymous) during their residential stay. This was intended to mitigate the possibility that treatment effects were due solely to the experimental group receiving “extra” attention. Attendance at extra support group meetings was equated to the number of hours the experimental group received additional MBRP sessions. The basic treatment practice employed at the residential treatment center was a mix of cognitive-behavioral treatment and 12-step approach to recovery.
Measures
Control Variables
To ensure our models adequately controlled for outside influences, we controlled for several institutional and individual level variables. In all models, we controlled for the number of days each participant spent in the treatment facility; the number of days each participant spent in jail, hospital, or prison at each time point post-treatment; and gender (female as reference group). This helped to adjust for the lower rates of substance use reported by participants because they were in a controlled environment. All control variables were regressed on all latent intercept and slope factors.
Impulsivity
We used the short form of the UPPS-P (SUPPS-P) impulsive behavior scale (Cyders et al. 2014). The SUPPS-P is a 20-item inventory designed to measure five personality traits (or subscales) that are linked to impulsivity. The five SUPPS-P subscales are: Negative Urgency, Positive Urgency, (lack of) Premeditation, (lack of) Perseverance, and Sensation Seeking. Each item is evaluated on a 4-point Likert scales ranging from “Strongly Agree” (1) to “Strongly Disagree” (4). Some example items are as follows: “When I feel bad, I will often do things I later regret in order to make myself feel better now (negative urgency), “Once I get going on something I hate to stop” (lack of perseverance), “I like to stop and think things over before I do them” (lack of premeditation), “I quite enjoy taking risks” (sensation seeking), and “I tend to lose control when I’m in a great mood” (positive urgency). Mean scores were calculated for each scale, such that higher scores relate to higher impulsivity subscales. All scales demonstrated adequate internal consistency within the current sample (Cronbach’s alpha coefficient: negative urgency = 0.72; positive urgency = 0.89; lack of premeditation = 0.89; lack of perseverance = 0.87; and sensation seeking = 0.83).
Substance Use
The Substance Frequency Scale (SFS) (Dennis et al. 2004) measures the average percent of days of use for alcohol, heavy alcohol, cannabis, illicit drugs, and also days of problems associated with substance use. Higher scores represent increasing frequency of substance use days. An example item is “in the past 2 weeks…how many days have you used any kind of alcohol?” Participants respond with the number of days (range 0–14) they have used each substance. The SFS was reliable in both prior adolescent and young adult samples (Buchan et al. 2002; Lennox et al. 2006). Specifically, the SFS has shown strong reliability, validity, and strong relationship with abuse and dependence symptoms among a large sample of youth in substance use disorder treatment (Dennis et al. 2004). The SFS has good reliability and validity in the current sample (α = .85 and test-retest r = .94).
Data Analyses
To assess change across the five facets of impulsivity, a taxonomy of bi-linear spline latent growth models were estimated (Grimm et al. 2017). Bi-linear spline models are useful when data can be separated into discrete phases. Typically, bi-linear spline models are used when simple growth models cannot fit the functional form of the data. Each discrete phase can be a simple growth model (e.g., linear or quadratic factors), which aids in both model fit, and analyzing the functional form of the data. The segments that connect the phases of growth are called knot or transition points. In the current study, we used bi-linear spline models to assess the effects of treatment assignment (MBRP vs. TAU) during the treatment phase (slope 1) and post-treatment phase (slope 2) with the intercept centered at the pre-treatment assessment. All models tested for the presence of a quadratic effect during the post-treatment phase using changes in model fit (− 2 log likelihood). Results suggested a random intercept and linear slope with a fixed quadratic slope provided the best fit to the data. To determine variation in changes across the impulsivity scales, we regressed each latent growth factor on a dummy variable representing the experimental (MBRP = 1) and control (TAU = 0) conditions.
In addition to assessing how treatment marks changes on impulsivity scales, we fitted a series of model constraints to assess between-group differences (e.g., simple slopes) in the outcomes at substantively meaningful points in time: (1) baseline, (2) treatment completion (i.e., end of the treatment phase), (3) mid-point (14 weeks), and (4) end of study (28 weeks, end of the post-treatment phase). To understand practical significance, we calculated standardized mean differences (Cohen’s d) at all four time points mentioned above, which provide descriptive indicators of effect size. Cohen’s d was calculated with MBRP as the reference group; thus, negative values favor the experimental condition. Variance estimates used to scale d were estimated using total variance of the outcome over time (Lipsey and Wilson 2001).
Analytic Sample
All models were fitted using the full information maximum likelihood (FIML) estimator available in Mplus version 8 (Muthén and Muthén 1998–2012). In each model, individuals contributed any data they had to the likelihood function (i.e., both X and Yvariables). Our final analytic sample was 79 participants.
Results
Treatment-Related Changes Across Impulsivity Subscales
Table 2 provides parameter estimates for our final models for each of the five impulsivity subscales.
Table 2.
Final models for bi-linear spline latent growth curve models for impulsivity subscales. Parameter estimate (SE)
| Negative urgency | Positive urgency | Lack of perseverance | Lack ofpremeditation | Sensation seeking | |
|---|---|---|---|---|---|
| Growth parameters | |||||
| Intercept | 2.91 (0.11)* | 2.77 (0.11)* | 1.83 (0.10)* | 2.24 (0.01)* | 3.11 (0.12)* |
| Treatment linear slope | − 0.18 (0.07)* | − 0.11 (0.07) | 0.01 (0.05) | − 0.06 (0.06) | − 0.03 (0.05) |
| Post-treatment linear slope | 0.13 (0.03)* | 0.08 (0.03)* | 0.03 (0.02) | 0.04 (0.02) | − 0.004 (0.02) |
| Post-treatment quad slope | −0.01 (0.002)* | − 0.01 (0.002)* | − 0.001 (0.002) | − 0.001 (0.002) | 0.002 (0.001) |
| Treatment effect | |||||
| Intercept | 0.04 (0.14) | − 0.16 (0.15) | 0.12 (0.14) | 0.18 (0.13) | 0.06(0.16) |
| Treatment linear slope | −0.21 (0.08)* | − 0.13 (0.09) | − 0.15 (0.06)* | − 0.25 (0.08)* | − 0.08 (0.07) |
| Post-treatment linear slope | − 0.12(0.04)* | − 0.11 (0.04)* | − 0.01 (0.03) | − 0.04 (0.03) | 0.04 (0.03) |
| Post-treatment quad slope | 0.01 (0.003)* | 0.01 (0.003)* | − 0.001 (0.002) | 0.002 (0.003) | − 0.02 (0.003) |
| Random effects (variance) | |||||
| Intercept | 0.19 (0.06) | 0.21 (0.07)* | 0.23 (0.06)* | 0.18 (0.05) | 0.31 (0.07)* |
| Treatment phase slope | 0.08 (0.03) | 0.07 (0.02)* | 0.01 (0.01) | 0.06 (0.02)* | 0.02 (0.01) |
| Post-treatment linear slope | 0.003 (0.001)* | 0.003 (0.001)* | 0.01 (0.00)* | 0.01 (0.001)* | 0.002 (0.001)* |
| Post-treatment quad slope (fixed) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Fit indices | |||||
| -2LL | 4199.1 | 4213.6 | 3771.7 | 3882.2 | 3908.7 |
| AIC | 4289.1 | 4303.6 | 3861.7 | 3972.2 | 3998.7 |
| BIC | 4395.7 | 4410.3 | 9368.3 | 4078.8 | 4105.4 |
| CFI | 0.96 | 0.93 | 0.92 | 0.94 | 0.94 |
| RMSEA | 0.09 | 0.09 | 0.08 | 0.08 | 0.07 |
Control variables are not shown for ease of readability. However, each model controlled for time spent in the residential facility, time spent in jail, prison or other facility, and baseline levels for substance frequency scale. Further, a model building process was utilized for each of the 5 scales such that we estimated an unconditional linear growth model (model 1), an unconditional quadratic growth model (model 2), and a conditional growth model (model 3)
p < .05
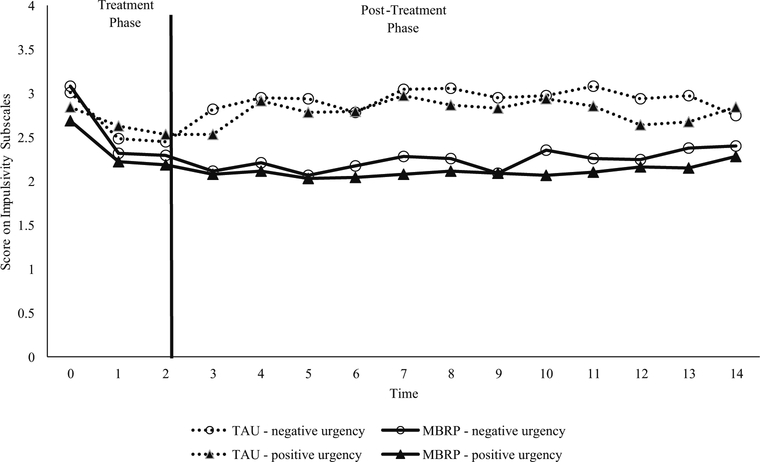
Negative Urgency
As indicated in our final conditional growth model (Table 2; Fig. 1), participants receiving MBRP reported statistically significant declines in negative urgency during the treatment phase whereas participants receiving TAU reported a non-significant decrease (bMBRP = − 0.41, p < 0.00; bTAU =− 0.21, p = 0.22). These declines during the treatment phase were significantly different from each other (Wald χ2 =4.43(1), p = 0.03). Notably, these trajectories diverged markedly upon leaving treatment (blinear = − 0.57, p < 0.00; bquad =0.41, p < 0.00). In general, participants assigned to MBRP maintained low levels of negative urgency throughout the post-treatment phase, evidenced by a non-significant simple slope (simple slopes: blinear = − 0.01, p = 0.82; bquad = 0.001, p = 0.40). However, participants assigned to TAU evidenced a stark increase following treatment discharge (simple slope: blinear = 0.12, p < 0.00; bquad = − 0.01, p = 0.04). As shown in the vertical distance between trajectories (marked by brackets in Fig. 1), the diverging trajectories manifested effect sizes that ranged from small at treatment completion (dtx completion = − 0.26), moderate at the mid-point (d12 weeks = − 0.51), and small at the end of the study (d28 weeks = − 0.21).
Fig. 1.
Change in negative and positive urgency (assessed biweekly) across experimental conditions
Positive Urgency
Similar to negative urgency, MBRP participants reported significant declines in their level of positive urgency (Fig. 1) during the treatment phase with those assigned to TAU reporting a non-significant decline (bMBRP = − 0.20, p = 0.02; bTAU = − 0.07, p = 0.48). Unlike negative urgency, treatment phase slopes were not significantly different from each other, Wald χ2 = 0.93(1), p = 0.34), indicating both groups had similar declines in positive urgency during treatment. However, trajectories diverged at treatment completion with participants assigned to MBRP maintaining low levels of positive urgency throughout the post-treatment phase (simple slopes: blinear = − 0.05, p = 0.19; bquad = 0.004, p = 0.15). In contrast, participants assigned to TAU showed a rather immediate and substantial increase in positive urgency following treatment completion and maintaining high levels throughout the post-treatment phase (simple slopes: blinear = 0.14, p < 0.00; bquad = − 0.01, p < 0.00). Diverging trajectories maintained effect sizes that were small throughout the study period (dtx completion = − 0.18; d12 weeks = − 0.37; d28 weeks = − 0.10).
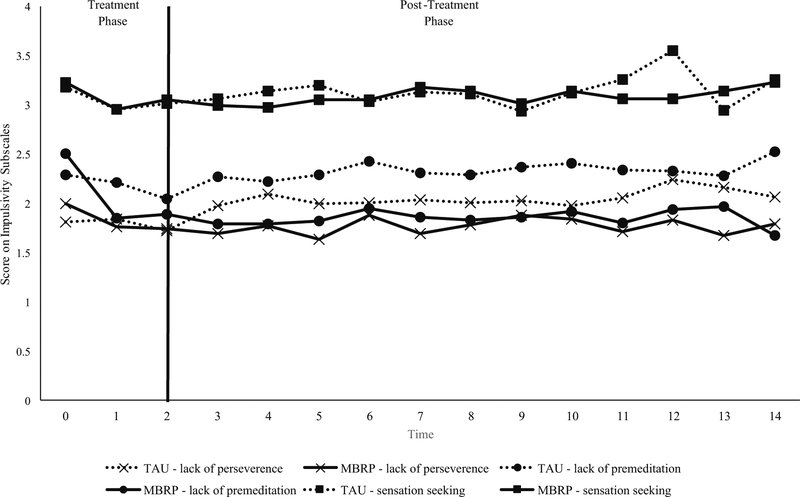
Lack of Premeditation
Significant differences were found in treatment slopes for lack of premeditation (Fig. 2) with participants assigned to MBRP evidencing significant declines in lack of premeditation and those assigned to TAU showing a non-significant slope (bMBRP = − 0.26, p < 0.00; bTAU = − 0.02, p = 0.81). These slopes were significantly different from each other (Wald χ2 = 6.23(1), p < 0.01). Interestingly, participants in both groups did not evidence significant change during the post-treatment phase. That is participants assigned to MBRP (simple slopes: blinear = − 0.01, p = 0.85; bquad = 0.001, p = 0.82) or TAU (simple slopes: blinear = 0.33, p = 0.33; bquad = − 0.01, p = 0.85) did not evidence increases or decreases on lack of premeditation from their treatment discharge levels. Effect sizes ranged from moderate at treatment completion (dtx completion = − 0.43), to rather large at the mid-point (d12 weeks = − 0.66), and end of the study (d28 weeks = − 0.63).
Fig. 2.
Change in UPPS subscales (assessed bi-weekly) across experimental conditions
Lack of Perseverance
Similar to lack of premeditation, we found differences in slopes for lack of perseverance (Fig. 2) during the treatment phase between conditions,bMBRP = −0.12, p = 0.01; bTAU = 0.02, p = 0.76. These slopes were significantly different from each other (Wald χ2 = 4.07(1), p = 0.04). Further, participants in both groups did not evidence significant change during the post-treatment phase. Participants assigned to MBRP (simple slopes: blinear = 0.01, p = 0.76; bquad = − 0.01, p = 0.76) or TAU (simple slopes: blinear = 0.01, p = 0.79; bquad = 0.002, p = 0.39) did not evidence increases or decreases in the report on lack of perseverance from their treatment discharge levels. Effect sizes ranged from small at treatment completion (dtx completion = − 0.16), to moderate at the mid-point (d12 weeks = − 0.38), and end of the study (d28 weeks = − 0.43).
Sensation Seeking
Unlike the other four subscales of impulsivity, sensation seeking (Fig. 2) evidenced no differences between conditions during both the treatment and post-treatment phases. Specifically, during treatment, those assigned to MBRP showed significant decreases in sensation seeking (bMBRP = − 0.13, p = 0.03) and those assigned to TAU had a non-significant change (bTAU = 0.04, p = 0.62). these slopes were not significantly different from each other (Wald χ2 = 4.76(1), p = 0.09). Further, no differences were found during the post-treatment phase between groups. Effect sizes were small or near negligible at all time points (dtx completion = − 0.03; d12 weeks = − 0.01; d28 weeks = − 0.03).
Indirect Effects Modeling
Table 3 includes all indirect effect models for each of the impulsivity subscales. We did not find an indirect effect for lack of premeditation, lack of perseverance, and sensation seeking. We did, however, find that both positive urgency (indirect effect = − 2.05, 95% CI [− 4.20, − 0.18]; standardized = − 0.84) and negative urgency (indirect effect = − 2.08, 95% CI [− 3.59, − 0.53]; standardized = −0.89) were significant indirect effects. That is, post-treatment substance use frequency is expected to decrease by 0.84 and 0.89 standard deviations for individuals assigned to MRBP (versus TAU) via decreases in positive and negative urgency, respectively.
Table 3.
Model based approach for impulsivity subscale mediation
| Negative urgency B [95% CI] | Positive urgency B [95% CI] | Lack of premeditation B [95% CI] | Lack of perseverance B [95% CI] | Sensation seeking B [95% CI] | |
|---|---|---|---|---|---|
| A path | − 1.36 [− 1.93, − 0.78] | − 0.96 [− 1.50, − 0.43] | − 1.20 [− 1.77, − 0.63] | − 065 [− 1.11, − 0.19] | − 0.22 [− 0.69, 0.25] |
| B path | 1.53 [0.61,2.45] | 2.11 [0.20, 4.04] | 0.71 [− 0.71,2.12] | 3.78 [− 4.35, 6.51] | 0.56 [− 0.99, 2.12] |
| C’ path | − 1.11 [− 2.55, 0.33] | − 1.04 [− 3.13, 1.06] | − 0.12 [− 1.88, 1.64] | − 1.37 [− 5.92,3.19] | − 0.87 [− 1.63, − 0.11] |
| Total effect | − 0.97 [− 1.58, − 0.35] | − 1.01[− 1.61, − 0.02] | − 0.96 [− 1.75, − 0.18] | − 1.10 [− 1.83, − 0.37] | − 0.99 [− 1.67, − 0.32] |
| Indirect effect | − 2.08 [− 3.59, − 0.53] | − 2.05 [− 4.20, − 0.18] | − 0.84 [− 2.65, 0.96] | − 2.48 [− 6.97, 2.02] | − 0.13 [− 0.56, 0.31] |
Each model allowed for co-variation between intercepts and slopes. Treatment assignment was regressed on intercept and slope values; however, effects shown above are for treatment effect on change (slopes) during treatment and post-treatment phase. A path = treatment assignment regressed on treatment phase stress slope; B path = stress slope during treatment phase regressed on post-treatment phase slope for craving or substance use; C path = treatment assignment regressed on post-treatment phase craving or substance use. Italic indicates confidence interval does not include 1
Discussion
Impulsivity is a well-established risk factor for substance use, broadly, and alcohol use, drug use, and substance dependence, specifically (Lejuez et al. 2010). As such, interventions aimed at reducing impulsive behavior have important implications for reducing substance use. The main purpose of the current study was to understand differences in trajectories of facets of impulsivity among young adults receiving an intervention designed to target impulsivity (MBRP) versus standard residential SUD treatment. Further, we sought to understand if changes in impulsivity during treatment were a significant mechanism of change between treatment assignment and post-treatment substance use. Consistent with prior research (Yaghubi et al. 2017), results indicated that MBRP was effective at reducing facets of trait impulsivity in treatment-seeking individuals with SUDs. Although contrary to study hypotheses, only positive and negative urgency mediated the relation between treatment assignment and substance use.
This study indicates that the effect of MBRP on impulsivity over time is dimension specific. That is, young adults receiving MBRP evidenced significant reductions in all facets of impulsivity except for sensation seeking during treatment, and these reductions were significantly greater than TAU for all facets except positive urgency. These treatment gains were maintained through the 6-month follow-up, providing empirical evidence that MBRP alters facets of trait impulsivity prospectively. Although both groups evidenced reductions in positive urgency, these reductions were only maintained for the MBRP group. That is, MBRP appears to have specific effects on positive urgency, negative urgency, lack of premeditation, and lack of perseverance. These results are partially consistent with findings from a prior meta-analysis examining associations between dimensions of impulsivity and mindfulness, in which positive urgency, negative urgency, and lack of premeditation evidenced medium effects and sensation seeking evidenced small effects (Stautz and Cooper 2013). The current MBRP intervention did not significantly reduce sensation seeking. However, prior research suggests that sensation seeking has a curvilinear relationship with age, with peak levels between the ages of 12–15, and a slight decline during the late teens and early twenties (Steinberg et al. 2008). Therefore, it is possible that the effect of mindfulness-based interventions on sensation seeking may be hindered because of the strength of this personality trait during young adulthood.
The current study found both positive and negative urgency to be significant mechanisms of change between treatment assignment (MBRP vs. TAU) and long-term substance use (post-treatment). This is consistent with cross-sectional work that has found that, after controlling for mindfulness variables, only negative and positive urgency were related to alcohol consumption (Murphy and MacKillop 2012), indicating that the association between mindfulness and alcohol use may be a function of these specific dimensions of impulsivity. Both positive and negative urgency describe disposition towards rash action in the context of intense affective state (e.g., negative or positive emotional state). Thus, it may be that MRBP mitigates the decision to use alcohol or drugs in response to intense emotional states. In fact, some prior research has found that being higher in negative and positive urgency can predis-pose individuals to use alcohol in response to distress (Settles et al. 2010). Future research may benefit from a more focused investigation of how mindfulness interventions may alter impulsivity during intense emotional states. Identifying which specific mindfulness strategies are most effective in regulating intense emotional states over time is warranted.
It is notable that MBRP appeared to reduce positive and negative urgency during treatment and protect against post-treatment increases in these domains. Specifically, the MBRP group evidenced significant reductions in positive and negative urgency that were maintained to post-treatment, but the TAU group evidenced non-significant decreases during treatment that were counteracted by significant increases post-treatment. This finding is especially notable in light of evidence that reductions in impulsivity are a mechanism of action in 12-step programs (Blonigen et al. 2013). Given that the TAU group attended additional 12-step meetings but did not maintain the reductions in impulsivity observed in the MBRP group, the current study suggests that changes in impulsivity resulting from 12-step program attendance may be short lived at least in this type of cohort. Future research is needed to clarify this finding.
Results from our study may also lend some support to a top-down hypothesis of self-regulation. We measured change in impulsivity dimensions that relate to an ability to resist instant gratification (urgency), increased attention control (perseverance), and heightened ability to assess long-term consequences (premeditation). One core tenet of MBRP focuses on being in the moment and focusing on addressing the difference between reacting (e.g., habitual response to a negative stimuli) and responding (e.g., present focused, non-judgmental response to a negative stimuli). In this sense, MBRP may help by increasing top-down control while also dampening the reactive nature of bottom-up processes. This account is consistent with prior research showing that mindfulness training can improve functional connectivity between parts of the brain that are associated with cognitive control over emotions and thoughts (e.g., dorsolateral and ventromedial prefrontal cortex) (Witkiewitz et al. 2013b). Evidence also suggests that top-down cognitive control is associated with craving cues via increased activity in frontal regions of the brain and decreased activity in striatal regions (Kober et al. 2010; Volkow et al. 2010). It follows that mindfulness training through MBRP may be associated with a greater ability to exhibit top-down control during heightened emotional states. This may manifest as an increased ability to recognize triggers (e.g., signs of emotional distress) that might previously have been outside of conscious awareness and to use skills learned such as acceptance, urge surfing, and equanimity to mitigate impulsive responses by regulating emotions without using substances (Witkiewitz et al. 2005). The current study provides support for this hypothesis, indicating that MBRP may inhibit impulsive decision-making most effectively during time of heightened emotional distress (i.e., positive and negative urgency).
Limitations and Future Research
The current study is not without limitations. First, the use of self-reported impulsivity and substance use may introduce recall bias in outcomes. While several studies have found self-reported substance use to be highly correlated with biochemical measures (Hjorthøj et al. (2012), future research should assess a more comprehensive range of impulsivity facets, such as behavioral choice (e.g., delay discounting) and behavioral response (e.g., cued go/no-go task). Second, while we were able to detect small to moderate effects, our small sample size may have influenced statistical power. Replication studies using larger sample sizes are warranted. Third, individuals were in a controlled environment during the treatment phase, which may have led to reduced opportunities for impulsive behavior. Although the focus on individuals in residential treatment is a strength, and the results indicate that differences between treatment groups exist despite the controlled setting, future studies would benefit from replication studies among youth in outpatient or Breal-world^ settings. Fourth, the MBRP intervention in the current study made use of rolling group admission, allowing new patients at the residential facility to enter the group and departing patients to leave it. This may be a limitation given ordering or timing of specific sessions. However, a recent open trial has shown that rolling MBRP groups have demonstrated feasibility and acceptability comparable to the typical closed group format (Roos et al. 2018).
Acknowledgements
We are grateful to the National Institute on Drug Abuse (Grant Number: 1R36DA041538; PI: Davis), the Fahs-Beck Fund for Research and Experimentation (PI: Davis), and the Campus Research Board (Grant Number: RB15434; PI: Roberts) for funding the current study. Manuscript preparation was supported in part by a grant from the National Institute on Alcohol Abuse and Alcoholism (Grant Number: K99AA026317; PI: Dworkin). We want to thank our research assistants Emily Hartung and Samantha Allen for their help with data collection and data entry. We would also like to thank our community partner for their continued support.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics were approved from the University of Illinois IRB.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bechara A, & Van Der Linden M (2005). Decision-making and impulse control after frontal lobe injuries. Current Opinion in Neurology, 18(6), 734–739. 10.1097/01.wco.0000194141.56429.3c. [DOI] [PubMed] [Google Scholar]
- Blonigen DM, Timko C, & Moos RH (2013). Alcoholics anonymous and reduced impulsivity: a novel mechanism of change. Substance Abuse, 34(1), 4–12. 10.1080/08897077.2012.691448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, et al. (2009). Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse, 30(4), 295–305. 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, & Witkiewitz K (2014a). Mindfulness-based relapse prevention for addictive behaviors In Baer RA (Ed.), Mindfulness-based treatment approaches (Second ed., pp. 141–157). San Diego: Academic Press. [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu S, et al. (2014b). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry, 71(5), 547–556. 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin FC, Zack M, & McMain S (2002). An information-processing analysis of mindfulness: implications for relapse prevention in the treatment of substance abuse. Clinical Psychology: Science and Practice, 9(3), 275–299. 10.1093/clipsy.9.3.275. [DOI] [Google Scholar]
- Brewer JA, & Potenza MN (2008). The neurobiology and genetics of impulse control disorders: relationships to drug addictions. Biochemical Pharmacology, 75(1), 63–75. 10.1016/j.bcp.2007.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan BJ, L. D. M, Tims FM, & Diamond GS (2002). Cannabis use: consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction, 97(Suppl 1), 98–108. [DOI] [PubMed] [Google Scholar]
- Caswell AJ, Bond R, Duka T, & Morgan MJ (2015). Further evidence of the heterogeneous nature of impulsivity. Personality and Individual Differences, 76, 68–74. 10.1016/j.paid.2014.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamorro J, Bernardi S, Potenza MN, Grant JE, Marsh R, Wang S, et al. (2012). Impulsivity in the general population: a national study. Journal of Psychiatric Research, 46(8), 994–1001. 10.1016/j.jpsychires.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla N, Collin S, Bowen S, Hsu S, Grow J, Douglass A, et al. (2010). The mindfulness-based relapse prevention adherence and competence scale: development, interrater reliability, and validity. Psychotherapy Research, 20(4), 388–397. 10.1080/10503300903544257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A, & Serretti A (2014). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse, 49(5), 492–512. 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Christopher M, Ramsey M, & Antick J (2013). The role of dispositional mindfulness in mitigating the impact of stress and impulsivity on alcohol-related problems. Addiction Research & Theory, 21(5), 429–434. 10.3109/16066359.2012.737873. [DOI] [Google Scholar]
- Chuang C-WI, Sussman S, Stone MD, Pang RD, Chou C-P, Leventhal AM, et al. (2017). Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addictive Behaviors, 74, 41–47. 10.1016/j.addbeh.2017.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrod PJ, Stewart SH, Comeau N, & Maclean AM (2006). Efficacy of cognitive-behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Clinical Child and Adolescent Psychology, 35(4), 550–563. 10.1207/s15374424jccp3504_6. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, & Cyders MA (2013). Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research, 37(9), 1441–1450. 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a Short Version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors, 39(9), 1372–1376. 10.1016/j.addbeh.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Smith DC, & Briley DA (2017). Substance use prevention and treatment outcomes for emerging adults in non-college settings: a meta-analysis. Psychology of Addictive Behaviors, 31(3), 242 10.1037/adb0000267. [DOI] [PubMed] [Google Scholar]
- Davis JP, Berry D, Dumas TM, Ritter E, Smith DC, Menard C, et al. (2018). Substance use outcomes for mindfulness based relapse prevention are partially mediated by reductions in stress: results from a randomized trial. Journal of Substance Abuse Treatment, 91, 37–48. 10.1016/j.jsat.2018.05.002. [DOI] [PubMed] [Google Scholar]
- Dawe S, & Loxton NJ (2004). The role of impulsivity in the development of substance use and eating disorders. Neuroscience and Biobehavioral Reviews, 28(3), 343–351. 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, & Waldron H (2004). Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction, 99(Suppl 2), 120–128. 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, et al. (2010). Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology, 15(2), 217–226. 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore MT, & Weafer J (2013). Behavioral inhibition and addiction In MacKillop J & de Wit H (Eds.), The Wiley-Blackwell handbook of addiction psychopharmacology (pp. 135–164). Chichester: Wiley-Blackwell. [Google Scholar]
- Grimm KJ, Ram N, & Estabrook R (2017). Growth modeling: structural equation and multilevel modeling approaches. New York: Guilford Press. [Google Scholar]
- Helstrom A, Hutchison K, & Bryan A (2007). Motivational enhancement therapy for high-risk adolescent smokers. Addictive Behaviors, 32(10), 2404–2410. 10.1016/j.addbeh.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorthøj CR, Hjorthøj AR, & Nordentoft M (2012). Validity of timeline follow-back for self-reported use of cannabis and other illicit substances—systematic review and meta-analysis. Addictive Behaviors, 37(3), 225–233. [DOI] [PubMed] [Google Scholar]
- Hsu SH, Collins SE, & Marlatt GA (2013). Examining psycho-metric properties of distress tolerance and its moderation of mindfulness-based relapse prevention effects on alcohol and other drug use outcomes. Addictive Behaviors, 38(3), 1852–1858. 10.1016/j.addbeh.2012.11.002. [DOI] [PubMed] [Google Scholar]
- King K, Patock-Peckham J, Dager A, Thimm K, & Gates J (2014). On the mismeasurement of impulsivity: trait, behavioral, and neural models in alcohol research among adolescents and young adults. Current Addiction Reports, 1(1), 19–32. 10.1007/s40429-013-0005-4. [DOI] [Google Scholar]
- Kirby KN, & Finch JC (2010). The hierarchical structure of self-reported impulsivity. Personality and Individual Differences, 48(6), 704–713. 10.1016/j.paid.2010.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kober H, Mende-Siedlecki P, Kross EF, Weber J, Mischel W, Hart CL, & Ochsner KN (2010). Prefrontal–striatal pathway underlies cognitive regulation of craving. Proceedings of the National Academy of Sciences, 107(33), 14811–14816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollins SH (2003). Delay discounting is associated with substance use in college students. Addictive Behaviors, 28(6), 1167–1173. 10.1016/S0306-4603(02)00220-4. [DOI] [PubMed] [Google Scholar]
- Koob GF, & Volkow ND (2009). Neurocircuitry of addiction. [Neuropsychopharmacology Reviews]. Neuropsychopharmacology, 35, 217 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, et al. (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence, 88(1), 79–82. 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Magidson JF, Mitchell SH, Sinha R, Stevens MC, & de Wit H (2010). Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders. Alcoholism: Clinical and Experimental Research, 34(8), 1334–1345. 10.1111/j.1530-0277.2010.01217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennox R, Dennis ML, Scott CK, & Funk R (2006). Combining psychometric and biometric measures of substance use. Drug and Alcohol Dependence, 83(2), 95–103. 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. Thousand Oaks: Sage Publications. [Google Scholar]
- Loree AM, Lundahl LH, & Ledgerwood DM (2015). Impulsivity as a predictor of treatment outcome in substance use disorders: review and synthesis. Drug and Alcohol Review, 34(2), 119–134. 10.1111/dar.12132. [DOI] [PubMed] [Google Scholar]
- Lu J, & Huffman K (2017). A meta-analysis of correlations between trait mindfulness and impulsivity: implications for counseling. International Journal for the Advancement of Counselling, 39(4), 345–359. 10.1007/s10447-017-9302-2. [DOI] [Google Scholar]
- Lynam DR, Smith GT, Whiteside SP, & Cyders MA (2006). The UPPS-P: assessing five personality pathways to impulsive behavior (technical report). West Lafayette: Purdue University. [Google Scholar]
- MacKillop J, & Kahler CW (2009). Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence, 104(3), 197–203. 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Weafer J, Gray J, Oshri A, Palmer A, & Wit H (2016). The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology, 233(18), 3361–3370. 10.1007/s00213-016-4372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, & Colder CR (2007). The UPPS Impulsive Behavior Scale: factor structure and associations with college drinking. Personality and Individual Differences, 43(7), 1927–1937. 10.1016/j.paid.2007.06.013. [DOI] [Google Scholar]
- McClure SM, Laibson DI, Loewenstein G, & Cohen JD (2004). Separate neural systems value immediate and delayed monetary rewards. Science, 306(5695), 503 10.1126/science.1100907. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, & Swann AC (2001a). Psychiatric aspects of impulsivity. American Journal of Psychiatry, 158(11), 1783–1793. 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, & Grabowski J (2001b). The impact of impulsivity on cocaine use and retention in treatment. Journal of Substance Abuse Treatment, 21(4), 193–198. 10.1016/S0740-5472(01)00202-1. [DOI] [PubMed] [Google Scholar]
- Müller SE, Weijers HG, Böning J, & Wiesbeck GA (2008). Personality traits predict treatment outcome in alcohol-dependent patients. Neuropsychobiology, 57(4), 159–164. [DOI] [PubMed] [Google Scholar]
- Murphy C, & MacKillop J (2012). Living in the here and now: interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology, 219(2), 527–536. 10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2012). Mplus user’s guide (Seventh ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Rachlin H, & Green L (1972). Commitment, choice and self-control. Journal of the Experimental Analysis of Behavior, 17(1), 15–22. 10.1901/jeab.1972.17-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos CR, Kirouac M, Stein E, Wilson AD, Bowen S, & Witkiewitz K (2018). An open trial of rolling admission mindfulness-based relapse prevention (rolling MBRP): feasibility, acceptability, dose-response relations, and mechanisms. Mindfulness. 10.1007/s12671-018-1054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancho M, De Gracia M, Rodríguez RC, Mallorquí-Bagué N, Sánchez-González J, Trujols J, et al. (2018). Mindfulness-based interventions for the treatment of substance and behavioral addictions: a systematic review. Frontiers in Psychiatry, 9, 95 10.3389/fpsyt.2018.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles RF, Cyders M, & Smith GT (2010). Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behaviors, 24(2), 198–208. 10.1037/a0017631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl C, Voss A, Schmitz F, Nuszbaum M, Tüscher O, Lieb K, et al. (2014). Behavioral components of impulsivity. Journal of Experimental Psychology. General, 143(2), 850 10.1037/a0033981. [DOI] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, et al. (2012). Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology, 20(3), 205–212. 10.1037/a0026543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stautz K, & Cooper A (2013). Impulsivity-related personality traits and adolescent alcohol use: a meta-analytic review. Clinical Psychology Review, 33(4), 574–592. 10.1016/j.cpr.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, & Woolard J (2008). Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Developmental Psychology, 44(6), 1764–1778. 10.1037/a0012955. [DOI] [PubMed] [Google Scholar]
- Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, & Vanderplasschen W (2014). Impulsivity as a vulnerability factor for poor addiction treatment outcomes: a review of neurocognitive findings among individuals with substance use disorders. Journal of Substance Abuse Treatment, 47(1), 58–72. 10.1016/j.jsat.2014.01.008. [DOI] [PubMed] [Google Scholar]
- Sussman S, & Arnett JJ (2014). Emerging adulthood: developmental period facilitative of the addictions. Evaluation & the Health Professions, 37(2), 147–155. 10.1177/0163278714521812. [DOI] [PubMed] [Google Scholar]
- Tang Y-Y, Tang R, & Posner MI (2016). Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug and Alcohol Dependence, 163(S1), S13–S18. 10.1016/j.drugalcdep.2015.11.041. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Lawrence AJ, & Clark L (2008). Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neuroscience and Biobehavioral Reviews, 32(4), 777–810. 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang G-J, Telang F, Logan J, Jayne M, et al. (2010). Cognitive control of drug craving inhibits brain reward regions in cocaine abusers. NeuroImage, 49(3), 2536–2543. 10.1016/j.neuroimage.2009.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, & Tindle HA (2013). Mindful attention reduces neural and self-reported cue-induced craving in smokers. Social Cognitive and Affective Neuroscience, 8(1), 73–84. 10.1093/scan/nsr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- Wingrove J, & Bond AJ (1997). Impulsivity: a state as well as trait variable. Does mood awareness explain low correlations between trait and behavioural measures of impulsivity? Personality and Individual Differences, 22(3), 333–339. 10.1016/S0191-8869(96)00222-X. [DOI] [Google Scholar]
- Winhusen T, Lewis D, Adinoff B, Brigham G, Kropp F, Donovan DM, et al. (2013). Impulsivity is associated with treatment non-completion in cocaine-and methamphetamine-dependent patients but differs in nature as a function of stimulant-dependence diagnosis. Journal of Substance Abuse Treatment, 44(5), 541–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H (2008). Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addiction Biology, 14(1), 22–31. 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA, & Walker D (2005). Mindfulness-based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy, 19(3), 211–228. 10.1891/jcop.2005.19.3.211. [DOI] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, & Hsu SH (2013a). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors, 38(2), 1563–1571. 10.1016/j.addbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Lustyk MKB, & Bowen S (2013b). Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychology of Addictive Behaviors, 27(2), 351–365. 10.1037/a0029258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Warner K, Sully B, Barricks A, Stauffer C, Thompson BL, et al. (2014). Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center. Substance Use & Misuse, 49(5), 536–546. 10.3109/10826084.2013.856922. [DOI] [PubMed] [Google Scholar]
- Yaghubi M, Zargar F, & Akbari H (2017). Comparing effectiveness of mindfulness-based relapse prevention with treatment as usual on impulsivity and relapse for methadone-treated patients: a randomized clinical trial. Addiction and Health, 9(3), 156–165. [PMC free article] [PubMed] [Google Scholar]