Abstract
Background and aims
COVID-19 pandemic has affected various countries differently due to variance in demographics, income level, health infrastructure, government response, control and enforcement, and cultural traits of different populations. This study aims to identify significant factors behind the unequal distribution of identified cases and deaths in different countries. Our study’s objective is comparative analysis and identification of relations between the spread of COVID-19 pandemic, population characteristics, and government response.
Methods
The top 18 countries worst hit by COVID-19 cases were identified. The data metrics, such as the number of cases, deaths, fatality rates, tests, average life expectancy, and population, were collected and consolidated.
Results
Countries with significant percentage of the older population are vulnerable to a high number of deaths due to COVID-19. Developed countries have higher per capita testing, whereas testing is less intensive in developing/underdeveloped countries. There is a consensus among health experts that COVID-19 has higher fatality rates for people above 60, however, with further age, this increases exponentially. Countries with higher life expectancy are also high-income countries, and the best course of action would be to provide specialized support to self-isolate for people of ages 75 and above.
Conclusion
The behaviour of disease occurring at a large scale and interaction with different populations is studied to understand and differentiate the factors and measures that successfully inhibited the pandemic. The study benchmarks different countries based on their performance and efforts against the pandemic and provides some useful insights on the efficiency of their governance and potential to improve & ramp up their programs. The economic status and existing healthcare infrastructure as they are the key factors in determining the country’s ability to contain and minimize the losses from this pandemic.
Keywords: Country-wise analysis, COVID-19, Life expectancy: Pandemic
1. Introduction
COVID-19 pandemic has affected the world extensively, with more than 8.6 million cases and 450,000 deaths worldwide. However, some countries have been more affected, and others have managed to cut their losses. The need is to analyze factors behind the unequal distribution of identified cases and associated deaths in majorly affected countries. The pandemic has affected various countries differently due to variance in demographics, income level, health infrastructure, government response, control, enforcement, and the cultural traits of different populations. However, multiple relations have been identified between the spread of the pandemic and the characteristics of the population, and we will discuss them here.
It is almost impossible to treat affected patients in the early stages of a new pandemic as there is no literature on how to do so. Research into the disease and the subsequent development of medicine and vaccines can take months to come to fruition. In such an informational blackout, patient data becomes critical for R & D to take place, as well as help authorities make informed decisions to control the pandemic in its early stages. The COVID-19 Pandemic, or ‘Corona Virus Disease-19′, named due to its first occurrence in November 2019 in China, is caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1]. The outbreak was first identified in Wuhan, China, in December 2019 [2]. The World Health Organization declared the outbreak a Public Health Emergency of International Concern on January 30, and a pandemic on March 11 [3]. As of June 19, 2020, more than 8.6 million cases of COVID-19 have been reported in more than 213 countries and territories, resulting in more than 450,000 deaths, while more than 4.5 million people have recovered [12].
The most common symptoms include fever, cough, fatigue, shortness of breath, and loss of sense of smell [[4], [5], [6]]. Complications associated with the disease may include pneumonia and acute respiratory distress syndrome [7]. The time from exposure to onset of symptoms is usually around five days but may range from two to fourteen days [8,9]. There is no known vaccine or specific antiviral treatment [4]. As of now, the primary mode of treatment is symptomatic and supportive therapy [10].
Recommended measures to prevent the spread of this virus include hand washing, covering one’s mouth when coughing, maintaining distance from other people, wearing a face mask in public places/gatherings, and monitoring and self-isolating who suspect they are infected [4,10,11]. Governments and authorities worldwide have responded by implementing travel restrictions, lockdowns, workplace hazard controls, and facility closures. Many countries have also upgraded existing infrastructure and personnel to increase testing capacity and trace contacts of infected persons [14,15].
Comparative analysis of different countries can give us an idea of how to fight the pandemic. By analyzing those countries which show useful statistics, governments can enforce similar policies and legislation in their own countries to improve their condition. Thus, analysis of patient data and comparative analysis of countries can give us the playbook on how to win the fight against COVID-19. We compared the top 18 countries (by COVID-19 cases) on various metrics.
From what we have observed and from the inference that we have drawn, we can say that government response to the pandemic can affect the severity of the pandemic. As we have seen in countries like India, steps like enforcement of lockdowns and social distancing norms effectively curt the spread of the virus.
Testing is of paramount importance when it comes to combating the virus. It is through testing that statistics related to the pandemic are obtained. Keeping this in mind, governments should allocate a more substantial amount of resources towards testing.
2. Problem definition and research objectives of the paper
Here, this paper’s primary focus is a country-wise analysis of the top 18 countries along with the world average and country of origin: China. This analysis aims to identify the factors behind the unequal distribution of identified cases and deaths in different countries. We assume that pandemic has affected various countries differently due to variance in demographics, income level, health infrastructure, government response, control and enforcement, and cultural traits of different populations. Our objective is to identify the relations between the spread of COVID-19 pandemic and the characteristics of a country’s population.
3. Scope of the paper
This study will focus on drawing insights from publically available data and statistics on the Coronavirus. The data that will be considered for the study is COVID-19 patient data, like daily cases, deaths, recoveries, testing data, etc.MS Excel will be used for carrying out the study. The depth of the study will be limited to some exploratory data analysis, data analysis for correlation and cause-and-effect relationships, bivariate analysis, and data visualization. This study focuses on prediction and will not cover any kind of data forecasting. The topic of the study (COVID-19 pandemic) is currently an evolving situation. The insights drawn from this study may not apply down the road. The data considered is publically available; the government reported patient data until June 19, 2020. Data from the worst affected countries (by cases) is considered in this analysis.
4. Research tools
4.1. Tools used
Microsoft Excel is used for this analysis. Data is arranged in descending order using Custom Sort (largest to smallest) along the column where the primary metric was stored for presentation on the bar chart so that country ranks could be easily distinguishable.
4.2. Data
Data is imported from www.worldometers.info/coronavirus [12], which provides real-time data on COVID-19 cases worldwide.
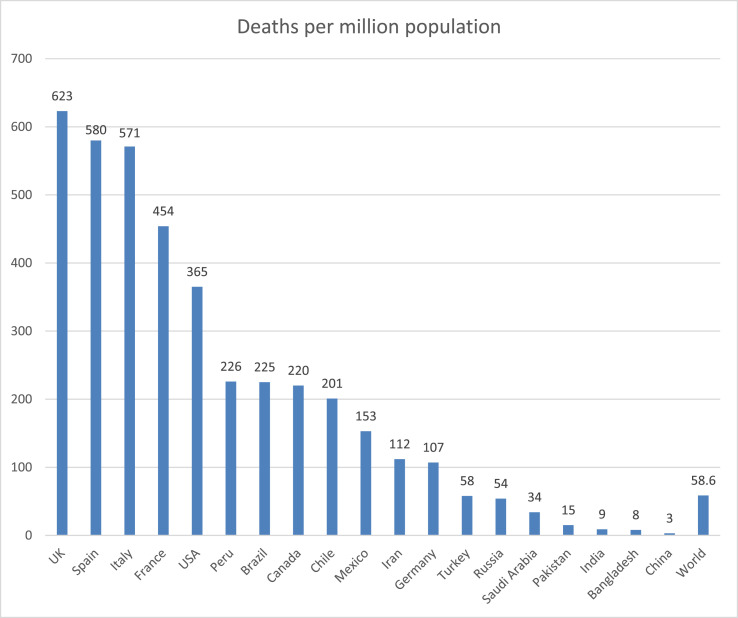
5. Deaths per million population
The number of deaths in a country is essential for gauging the damage dealt with by the COVID-19 pandemic. Then, factors behind such vulnerability can be studied to avoid a similar situation elsewhere or in the future. Fig. 1 shows the deaths per million population due to COVID-19 in the 18 most-affected countries (by COVID-19 cases) alongside the world average and country of origin, China [12].
Fig. 1.
Deaths per million due to COVID-19 (Data source [12]).
UK leads with the highest per capita deaths, and the following three countries, Spain, Italy, and France, also belong to Western Europe. Another common factor among these top 4 countries is that their average life expectancy is higher than 80. Western European countries are most affected by this pandemic because they have experienced the arrival of many cases before the rest of the world. Without time to plan or formulate policies to battle this epidemic, these countries suffered a more significant loss of lives.
Germany is an outlier among European countries with a higher population, as it is evident that their preventive measures were far more successful in controlling this epidemic.
Despite having the third-highest no. of cases in the world (569,000), Russia has managed to keep the deaths low (7841); one of the reasons might be a comparatively lower life expectancy of72 and proper health facilities. High no. of cases also point towards the intensive testing program, and Russia is1stin per capita testing, which points towards efficient management and delivery, considering that it has vast geography and distribution of resources is difficult [12].
India has managed to keep the per capita deaths low, which points towards its success in implementing strict lockdown and social distancing measures, which were mandated in the last week of March 2020. However, it is yet to be seen how the situation changes when restrictions are lifted. It is mainly dependent on the government’s readiness to deal with the epidemic in a country such as India with a population of 1.35 billion and a large section of poor people, as well as an inadequate health infrastructure to handle such crisis (as compared to Europe and USA).
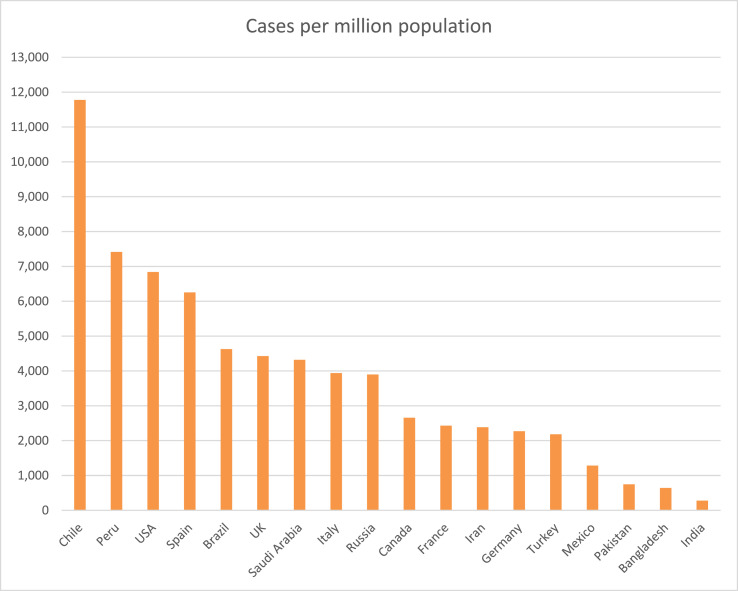
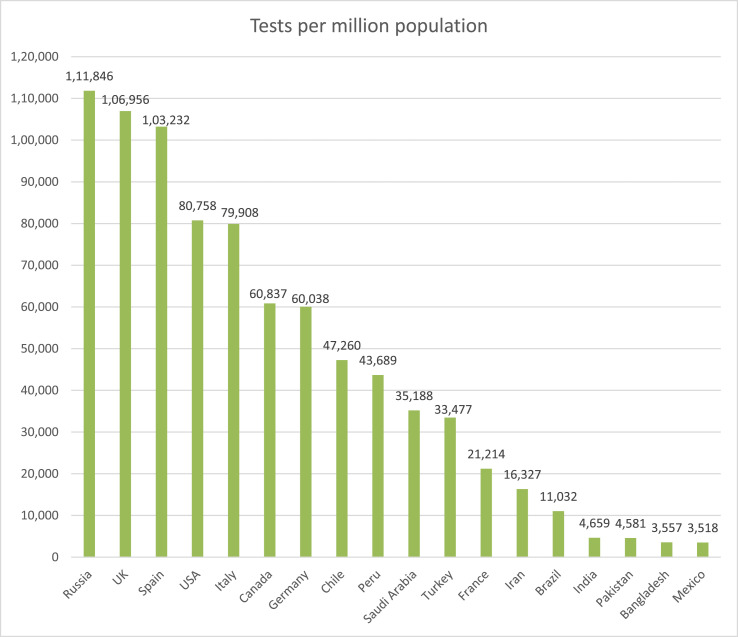
6. Cases vs tests (per million population)
The no. of cases in a country determines how extensively it has spread among the masses, which tells us about the efficacy of the government’s preventive measures. At the same time, a high number of cases per million (with proportionally fewer deaths, i.e., lower fatality rate) could also mean that extensive testing is taking place. Fig. 2 shows the cases per million population in the top 18 COVID affected countries [12].
Fig. 2.
COVID-19 cases per million population (Top 18 countries) (Data source [12]).
The above chart shows the no. of cases per million population (country-wise). Although the USA has the largest no. of cases worldwide, Chile takes the lead in per capita no. of COVID-19 cases. This chart can be observed to see how far the disease has spread among the population. A lower per capita infection points toward one or both of these factors:
-
a.
Effective preventative measures (social distancing and lockdown)
-
b.
Lower per capita testing
The extent of testing is a determinant of the government’s efforts against the pandemic. It is well-established that developed countries are comparatively well-equipped, financially and systemically, to fight this pandemic. Their testing rates are also high due to the less dense population and higher per capita spending on health. Fig. 3 shows the tests per million population of the Top 18 countries [12].
Fig. 3.
No. of tests per million population (Top 18 countries) (Data source [12]).
We compared it with this chart and analyzed the no. of tests per million population:
As we can see, there is a general trend that developed countries have invested more in testing. In these countries, the population is also less dense; their per capita health expenditure is high, and consequentially, per capita testing comes out to be high.
However, in India, even though testing is not that extensive in proportion to its large population, social distancing measures such as nationwide lockdown has been imposed to compensate for the lack of infrastructure to deal with a sudden rise in infected patients.
The data for no. of tests worldwide is not available; hence it has not been included in this analysis.
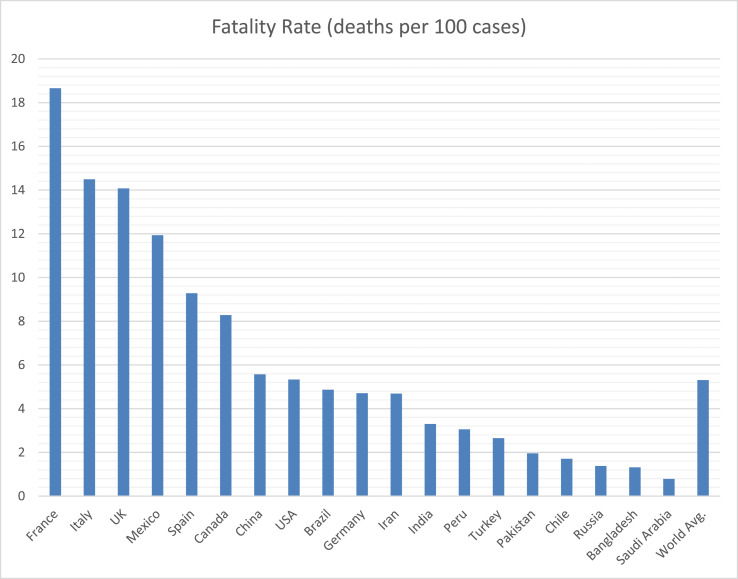
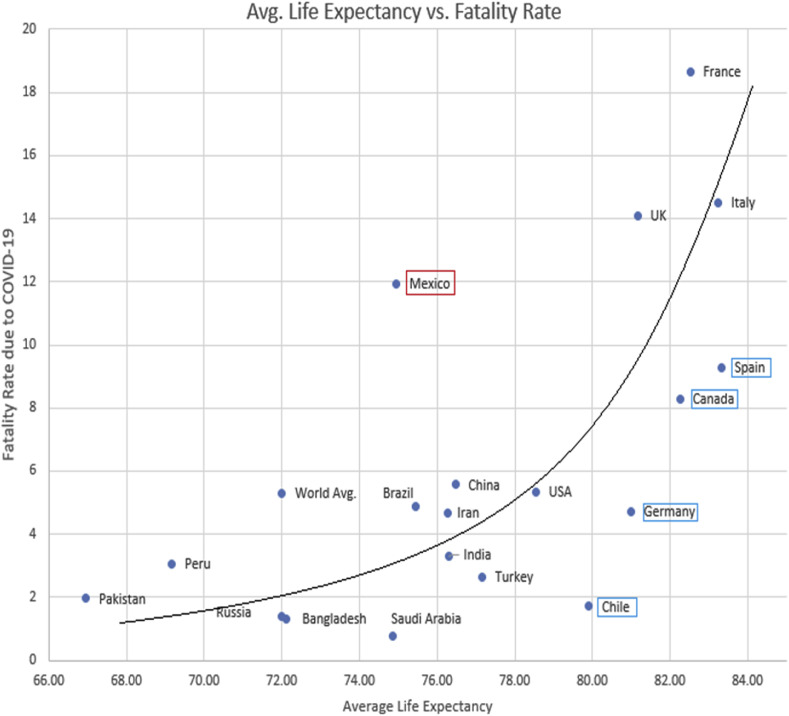
7. Fatality rate vs average life expectancy
A prevalent trend exhibited by the disease is that older people are more vulnerable, and more likely to die, which increases the fatality rate in countries with a significant percentage of older population; however, since the relation between age and fatality is already known, we tried to understand the extent to which age affects the fatality. Fig. 4 shows the fatality rate of COVID patients, i.e., the percentage of people who die after contracting this disease [12].
Fig. 4.
Fatality Rates (Data source [12]).
Fatality differs from deaths per million population as it is focused only on the survival ratio of those infected. A higher fatality rate means more people die from the disease. The first chart shows the fatality rate of the top 18 countries and the world average and also of the origin country, China. To establish a correlation between higher fatality rates and a higher percentage of the older population, we tried to establish some relation between fatality rates and average life expectancies. Fig. 5 shows the average life expectancy of these countries [13].
Fig. 5.
Average Life Expectancies (Data source [13]).
In this analysis, we found that 5 out of the top 6 countries by fatality rates have an average life expectancy above 80, except for Mexico, which has responded poorly to the pandemic due to lax measures and sub-par medical infrastructure. However, Germany and Chile are significant outliers, which, despite having proportionally higher life expectancies exhibited low fatality rates due to COVID-19.
There is a consensus among health experts that COVID-19 is fatal to people above 60; however, the fatality has exponential relationships with life expectancy as exemplified by countries with average life expectancies of more than 80 (Spain, UK, Italy, France, and Canada). It shows that people in the age range of 75–80 are at extreme risk if they get infected.
To further study this trend, we made a graph (Fig. 6 ) to show the correlation between average life expectancy and COVID-19 fatality rates [12,13]. The exponential trend can is quite evident from this graph as the best fit curve with the least distance from all points is an exponential curve, in any case.
Fig. 6.
Average Life Expectancy vs. Fatality Rate (Data source [12,13]).
A freehand curve was drawn to fit the points (countries) on the graph. Upward deviation from the trend-line signifies comparatively poor performance since it points towards a high fatality rate despite having a low average life expectancy. Downward deviation from the curve, on the other hand, signifies better performance, as it means the country has managed to keep the fatality rate low despite having a high average life expectancy. The extent of downward/upward deviation is a determinant of performance against the pandemic.
7.1. Major and minor outliers
-
•
Mexico, with a significant upward deviation from the trend line, points towards very poor performance against the pandemic. Mexico has an average life expectancy of 74.95, yet it has a disproportionately high fatality rate of 12%. It is due to inadequate medical infrastructure and inept government response.
-
•
Chile and Germany, with a significant downward deviation, point towards successful performance in inhibiting the transmission as well as dealing with the affected patients, which is a direct consequence of efforts and measures by the government and public against COVID-19 pandemic.
-
•
Canada and Spain also deviate downwards from the curve, but they are not considered major outliers because, since the curve is exponential, the distance from the curve should increase (more than Germany and Chile) as we move along the x-axis. However, they do deviate downwards, and hence their performance should be considered better than average; as evident from Fig. 6, they have managed to keep their fatality rates lower (8.3% and 9.3%) than France and Italy (18.6% and 14.5%), which have similar life expectancies.
-
•
Bangladesh, Russia, Saudi Arabia, Turkey, and India show a small downward deviation, which signifies comparatively better performance, while Pakistan, Peru, Brazil, Iran, and China show some upward deviation, which shows slightly poor performance.
So, our inference from this analysis is that the fatality of COVID-19 increases exponentially with age. Hence, countries with the older population have to take extraordinary measures for taking care of their older citizens who are at high risk.
Generally, countries with higher life expectancy are also high-income countries/countries with better health infrastructure. They provide proper healthcare facilities, but only after the person has been diagnosed with COVID-19; contrarily, the best course of action would be to provide individual support to self-isolate and encouragement to quarantine for people in that age group (75–85).
Despite having a considerable average life expectancy, a lower fatality rate means that preventive measures are significantly effective and successful. Germany and Chile have exhibited this kind of behaviour.
8. Results and discussion
Three different analyses were carried out for the top 18 countries with the highest no. of cases. China and world average figures &data are given alongside for measuring as to how the most affected countries compare with the metrics of world average and origin country of this pandemic.
8.1. Deaths per million population
-
a.
The top 4 countries with the highest deaths per million population: UK (623), Spain (580) Italy (571), France (454) belong to Western Europe and have an average life expectancy higher than 80.
-
b.
The bottom five countries with the least deaths per million: China (3), India (8), Bangladesh (9) Pakistan (15), and Saudi Arabia (34) – all have average life expectancy below 75 and belong to Asia.
-
c.
US has the highest no. of deaths worldwide (120,000); however, it is 5thin per capita deaths (365).
-
d.
The World Average of deaths per million due to COVID-19 is 58.6. In contrast, 187 people per million people died due to Tuberculosis (TB) in 2018.
-
e.
China managed to keep deaths per million population incredibly low (3), pointing towards extremely effective containment and preventive measures. The virus was contained well and did not spread massively.
-
f.
India, through its strict nationwide lockdown, has also kept the no. of deaths in control.
However, since the disease has not been contained successfully, we need to analyses how the situation evolves after the restrictions are lifted.
8.2. Cases vs tests (per million population)
-
a.
Since per capita testing is independent of the epidemiology of the virus and mostly dependent on the country’s financial resources, high-income countries have more intensive testing programs and consequently higher tests per million population (as they have more resources to spend per capita).
-
b.
UK and Spain have the highest deaths per million population, in response to which they have ramped up their testing. The UK recently saw a major spike in no. of deaths, so the testing program is yet to catch up with Spain, where the peak no. of cases is subsiding now.
-
c.
Chile has the highest no. of identified cases per million population, followed by Peru, USA, and Spain. In absolute terms, the USA, Brazil, and Russia have the highest number of identified cases (in that order).
-
d.
Russia is 1st in per capita testing and has the 3rd highest number of identified COVID-19 cases worldwide after the USA and Brazil, but ranks 13th in several deaths. Such a low fatality rate can be attributed to low average life expectancy (72), excellent medical infrastructure, and an agile and efficient government response to the pandemic.
-
e.
Brazil, India, Pakistan, Bangladesh, and Mexico have abysmally low testing numbers, considering the profound threat of this pandemic in these countries with sub-par medical infrastructure. Brazil is already facing a massive loss of lives, having second-highest no. of deaths, Mexico and India are also seeing a steady rise in deaths due to COVID-19 (7th and 8th in total no. of deaths). While cases and deaths are subsiding in developed countries, low and middle-income countries are especially vulnerable to the spread of this pandemic as it demands extensive and universal healthcare facilities.
8.3. Fatality rate vs average life expectancy
-
a.
The top 3 countries with the highest fatality rates have considerably high average life expectancy:
France – A fatality rate of 18.6%, the average life expectancy of 82.5.
Italy – A fatality rate of 14.5%, the average life expectancy of 83.33.
UK –A fatality rate of 14%, the average life expectancy of 81.16.
World Average fatality rate of 5. 3%, the average life expectancy of 72.
-
b.
5 out of the top 6 countries with the highest fatality rates have an average life expectancy above 80, except Mexico, which has responded poorly to the pandemic due to lax measures and sub-par medical infrastructure.
-
c.
The top 10 countries with the highest fatality rates have an average life expectancy greater than 75, except Mexico (74.95).
-
d.
The fatality rate of COVID-19 increases exponentially with age, which suggests that countries with a significant percentage of the older population are at higher risk.
-
e.
Despite a considerable average life expectancy, a lower fatality rate means that the preventive measures are significantly effective and successful. Germany and Chile have exhibited this kind of behaviour.
-
f.
Older people (above 75) are especially vulnerable; governments need to provide them with extra support for self-isolation and quarantine measures.
-
g.
Chile and Germany are major outliers, despite having a significant percentage of old population; they have managed to keep the fatality rates lower than their counterparts. This points towards efficient governance and successful enforcement of preventive measures.
-
h.
Canada and Spain are minor outliers, as they have life expectancies similar to France and Italy, yet they have managed to keep their fatality rates comparatively lower (8.3% and 9.3%) than their counterparts.
9. Limitations of the study, tool, data
Non-uniform testing leads to misrepresentation of the actual number of cases while comparing different countries. While countries with extensive testing programs are closer to identifying the actual no. of cases present at a given time, countries with inadequate testing (such as Mexico and other less developed countries) have a large number of unidentified cases.
Modeling a complex problem like a pandemic in a simple, two-variable system poses some obvious issues since COVID-19 is a complex problem dependent on multiple variables that may or may not be inter-related. Analyses taking into account only two or four variables at a time may reduce it to a very simplistic solution.
A bivariate analysis, when used in such a manner, essentially suggests that a single independent variable can be used to explain all the variance in the dependent variable when in reality, it may not be so. Bivariate analyses are generally used as a primary step in data exploration and regression modeling, and not as a final step through which an inference can be drawn.
There is no international standards/uniform methodology for data collection, aggregation, and reporting. Every country follows its protocols for reporting data and statistics related to the COVID-19 pandemic. Furthermore, the standards may or may not be followed by different states in the country; different states, districts, jurisdictions, etc. may have different methods of counting. However, this problem is more prominent in underdeveloped and developing countries where, often, there are not any protocols for data collection and representation. This lack of uniformity and consistency in data acquired may lead to inaccuracy and inconsistency in overall statistical observations, which consequently imparts inaccuracy to the analyses that make use of that data.
Countries like Russia, Belarus, Chile, China, and India have been accused of manipulating their COVID data to make their situation looks better. In a global health emergency like the Coronavirus, countries need to realize that cooperation is necessary for us to come out of this with minimal deaths and economic loss. There must be a more significant international oversight to ensure that countries are reporting actual numbers and not manipulating valuable data.
10. Future research implications
Since the testing is non-uniform in different countries, further studies can be done to arrive at the actual number of cases in a country, which are more than the identified number of cases at any given time. One of the significant metrics is the test positivity rate; the higher the test positivity rate, the higher the probability of the untested population being COVID-19 positive. A linear correlation can be done to arrive at an approximate figure of actual no. of COVID-19 cases in a population. Through this analysis, we have identified, that benchmarking different countries based on their performance and their efforts against the pandemic would provide useful insights into the efficiency of the government and its potential to improve & ramp up their programs. These countries should consider their economic status as it is one of the key factors determining the ability to contain and minimize the losses through this pandemic. It could provide an idea of the potential scope of performance improvement for different countries.
The analysis of the statistics related to COVID-19 in different countries will help to assess what further measures can be taken by the government to lower the spread of the virus. One can view to what extend the lockdown was sufficient so that further implementation can be done accordingly, and the right steps can be taken to contain the infection as well as balance the economic activities to ensure the protection of jobs and livelihoods.
In some countries, the graph should be a motive for concern, and stricter measures need to be taken there. As death figures show a higher number in the older population, strict preventive measures should be taken by individuals. The graphs can help in highlighting the faults in the healthcare system and the governing body of countries with higher cases. Additional financial support for health services is required, including sufficient resources to ensure adequate staffing and testing facilities in countries with high cases.
We will be able to learn lessons, especially in terms of public and global health, for any future similar pandemics the governing bodies will be able to prepare accordingly.
11. Conclusion
We compared the top 18 countries (by COVID-19 cases) based on various metrics. Our first analysis found a positive relationship between higher average life expectancy and deaths per million population. Countries with lower average life expectancy exhibited lesser vulnerability in terms of deaths due to COVID. In the subsequent analysis, we saw that developed countries (especially those with universal healthcare access) had higher per capita testing. In addition to that, higher testing has led to the identification of higher no. of cases, so we can safely conclude that there is a difference in observed/identified no. of cases and actual no. of cases of COVID-19 in a country, which largely depends on the extent of testing and diagnosis. In our last analysis, we found a positive correlation between average life expectancy and fatality rates; this is largely because vulnerability to this disease increases exponentially with age, especially after 60, due to weak respiratory and immune systems and increase in underlying health conditions (such as heart ailment, diabetes, etc.) which complicate the effects of the disease. Paper provides an idea of the potential scope of performance improvement for different countries in dealing with the pandemic.
Declaration of competing interest
On the behalf of all the authors in paper, I corresponding author hereby accept that there is no conflicts of interest.
References
- 1.Naming the coronavirus disease (COVID-19) and the virus that causes it". World Health Organization (WHO).
- 2.Novel coronavirus—China." World Health Organization (WHO).
- 3.Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)". World Health Organization (WHO).
- 4.Q & A on COVID-19". European Centre for Disease Prevention and Control.
- 5.Loss of sense of smell as a marker of COVID-19 infection". Ear, Nose, and Throat surgery body of the United Kingdom.
- 6.U.S.Centers for disease control and prevention (CDC).
- 7.Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC).
- 8.Symptoms of novel coronavirus (2019-nCoV)". U.S. Centers for Disease Control and Prevention(CDC).
- 9.Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop Med Int Health. 2020;25(3):278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caring for yourself at home". U.S.Centers for Disease Control and Prevention (CDC).
- 11.Unite against COVID-19".Unite against COVID-19. Government of New Zealand.
- 12.www.worldometers.info/coronavirus Retrieved June 19, 2020.
- 13.https://data.worldbank.org/indicator/SP.DYN.LE00.IN?name_desc=false&view=chart
- 14.Gupta R., Misra A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infection with reference to use of therapeutic and other drugs used in Co-morbid diseases (hypertension, diabetes, etc.) Diabetes & Metabolic Syndrome: Clin Res Rev. 2020;14(3):251–254. doi: 10.1016/j.dsx.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta R., Ghosh A., Singh A.K., Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes & Metabolic Syndrome. Clin Res Rev. 2020;14(3):211–212. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]