Abstract
With a large international sample (n = 8317), the present study examined which beliefs and attitudes about COVID-19 predict 1) following government recommendations, 2) taking health precautions (including mask wearing, social distancing, handwashing, and staying at home), and 3) encouraging others to take health precautions. The results demonstrate the importance of believing that taking health precautions will be effective for avoiding COVID-19 and generally prioritizing one’s health. These beliefs continued to be important predictors of health behaviors after controlling for demographic and personality variables. In contrast, we found that perceiving oneself as vulnerable to COVID-19, the perceived severity of catching COVID-19, and trust in government were of relatively little importance. We also found that women were somewhat more likely to engage in these health behaviors than men, but that age was generally unrelated to voluntary compliance behaviors. These findings may suggest avenues and dead ends for behavioral interventions during COVID-19 and beyond.
Keywords: COVID-19, Health behavior, Rule compliance, Government trust
Highlights
-
•
Examines which beliefs and attitudes about COVID-19 predict 1) following government recommendations, 2) taking health precautions (including mask wearing, social distancing, handwashing, and staying at home), and 3) encouraging others to take health precautions.
-
•
Uses a large international sample (n = 8317) to demonstrate the importance of believing that taking health precautions will be effective for avoiding COVID-19 and generally prioritizing one’s health.
-
•
Finds that perceiving oneself as vulnerable to COVID-19, the perceived severity of catching COVID-19, and trust in government were of relatively little importance.
-
•
Finds that women were somewhat more likely to engage in these health behaviors than men, but that age was generally unrelated to voluntary compliance behaviors.
1. Introduction
In late 2019, the World Health Organization (WHO) was alerted of a cluster of pneumonia cases in Wuhan, China [1]. This viral infection was attributed to a novel coronavirus named 2019-nCOV, which causes the disease COVID-19 (Coronavirus Disease 2019). In early March 2020, the WHO Director-General announced that the spread of COVID-19 must be assessed as a “pandemic” [2]. Preliminary data about fatality rates ranged from 0.5% to 3%, but these rates vary by different parameters such as age and coexisting conditions (diabetes or cardiovascular disease). COVID-19 was found to be highly transmissible, with the average infected person spreading the disease to up to three other individuals [1].
Communities around the world are facing extraordinary challenges to effectively slow the spread of COVID-19 and sustain their healthcare systems. Numerous countries have implemented measures, such as curfews, home quarantine, social distancing, and isolation of infected populations that severely hamper many day-to-day activities [3,4]. Additionally, governments have asked or required citizens to adopt behaviors (such as wearing masks and washing hands regularly) at high levels of compliance that they will need to maintain for an extended period of time, probably until treatments and vaccines are widely available [5]. These measures have the objective of decreasing the “R0”, a measure of reproduction of new infections, to less than one, and thus suppressing the local spread of the virus [6].
This situation raises a unique challenge for scientists and practitioners in understanding how to ensure adequate public cooperation and compliance. Mobilizing an effective public response to a pandemic requires clear communication and trust [7]. Because risk reduction measures such as social distancing and self-quarantine can rarely be enforced entirely by coercion, particularly in democratic societies, the public must understand what is required of them and be persuaded of the importance of complying.
Cognitive health behavior theories argue that a small number of beliefs and attitudes account for the adoption of preventive behavior. In this view, human beings weigh the costs of taking precautions against the benefits that might be obtained from them [8]. The Health Belief Model (HBM [[9], [10], [11]], is one of the most popular frameworks on the subject (for a more complete review see Refs. [12,13]. The HBM has been extensively used to explain various health behaviors including smoking [14], dietary behaviors [15], exercise [16,17], HIV risk behavior [18], and vaccine uptake [19]. And more recently, some HBM studies around the world have emerged to understand people’s behaviors and reactions regarding COVID-19 [20]. Sarwar and colleagues [21] recommend using the health belief model as a guiding theory for “creating public awareness regarding the potential benefits of the preventive approach.”
HBM considers 5 main factors as the determinants of health preventive behaviors: 1) Threat perceptions, 2) Response efficacy beliefs, 3) Self-efficacy, 4) Cues to Actions, and 5) Individual characteristics [9,22]. Threat Perceptions refer to personal beliefs about the likelihood of contracting a condition [22,23]. It includes two sub-components, perceived vulnerability, which refers to the extent to which an individual feels vulnerable to an illness, and perceived severity, which refers to beliefs about how serious the consequences of the condition would be [23]. The model supposes that the stronger people’s beliefs in the severity of an illness and the higher their perceived susceptibility to suffer from it, the more strongly they will be motivated to avoid it [10]. Therefore, assessing a community’s beliefs about COVID-19 is essential to the development of health communication campaigns to promote public compliance.
The success of public health interventions is likely to be partially explained by their ability—and perceived ability—to minimize risks, which in turn can predict adoption of health behaviors. Response efficacy beliefs refer to beliefs about the efficacy of protective behaviors in minimizing health risks. It is crucial that people believe that adopting health behaviors will reduce their vulnerability to the condition or its severity [22,23]. Self-efficacy refers to the confidence or belief in one’s own abilities to engage in the protective behavior [24,25]. Cues to Actions are triggers that are necessary for prompting engagement in preventive behaviors. Government recommendations may serve as more effective cues to actions when individuals trust in their government. Finally, individual characteristics, including demographic variables (e.g., age, gender) and personality variables could also affect compliance behavior [9].
This present study aims to explain and predict voluntary compliance with COVID-19 guidance by identifying personal beliefs and expectations that predict three COVID-19 health behaviors, including following government rules (adapted from Ref. [26], engaging in health protective behaviors (adapted from Ref. [27], and urging others to take health precautions (adapted from Refs. [28]. Building on the Health Belief Model (HBM [[9], [10], [11]], our research empirically tested the effects of five main factors as key determinants of voluntary compliance behaviors [9]: perceived vulnerability [29], perceived severity/disruptiveness of catching the disease [30], perceived efficacy of health behaviors for avoiding the disease [27], trust in government, and individual health importance [26].
Moreover, the present research sought to examine the significance of these predictors in a large, international sample. Much psychological research suffers from small sample sizes [31], and a lack of generalizability [32] because samples are selected from one country only (often, the United States; [33]. COVID-19 poses challenges to leaders worldwide, and thus we sought to provide a global analysis, with a sufficiently large sample size, that can provide insights that might be useful beyond the U.S.
2. Empirical study
2.1. Method
2.1.1. Open science statement
The analyses were preregistered: http://aspredicted.org/blind.php?x=2bk3g7. As noted in the preregistration, we conducted an initial wave of data collection with 4624 participants, conducted exploratory analyses on those data to finalize an analysis plan, and then preregistered this analysis plan before analyzing the full sample with a second wave of data collection, which included 3693 more cases. We consider our analysis exploratory, but preregistered our analysis plan to eliminate researcher degrees of freedom in analysis decisions. All data and analysis code will be made publicly available upon acceptance for publication. Verbatim materials are reported in the supplement.
2.1.2. Participants
Our 8317 participants (68.7% female, 31.3% male; M age = 27.02, SD = 9.95) were users of the smartphone application version of the French-based talent-management platform Praditus, on which people from across the globe complete surveys in exchange for feedback on their personality (www.praditus.com). Although the app contains numerous surveys and personality measures, in the present study, we included only participants who completed a battery of items about COVID-19 as well as the Big 5 Inventory [34]. Participants hailed from 70 different countries and completed the surveys in English (n = 2850), French (n = 2444), Spanish (n = 1216), German (n = 997), Italian (n = 707), Portuguese (n = 80), or Mandarin (n = 23).
2.1.3. Procedure
Participants completed a COVID-19 questionnaire, on which they reported various attitudes, beliefs, and behaviors related to COVID-19 on 1–5 scales from Strongly disagree to Strongly agree. Three subscales assessed voluntary compliance behaviors regarding COVID-19, which were our three outcome variables. One 3-item subscale assessed rule-following behavior (e.g., “I only leave home for reasons sanctioned by the government”, “I follow the rules for sheltering in place”); these items were combined into an index of rule following, α = 0.66. A second 4-item subscale assessed engagement in protective health behaviors, including handwashing, wearing a surgical mask, staying home, and practicing social distancing, which were combined into an index of health precautions, α = 0.65. The third subscale contained 5 items assessing tendencies to give others health recommendations (e.g., “I help others take the correct actions to remain healthy and safe” and “I frequently speak up and encourage others to engage in safe and healthy behavior”), which were combined into an index of giving health advice, α = .82. Verbatim questions from all scales can be found in the supplemental materials.
Five subscales assessed various beliefs about COVID-19 and served as our predictor variables. These included a 5-item scale of perceived invulnerability to COVID-19 (e.g., “I am not at risk for getting infected with COVID-19”, and “I am less likely than most people to get COVID-19”), α = 0.68; a 4-item scale about how disruptive getting COVID-19 would be (e.g., “Having COVID-19 would be disruptive to my physical health” and “Having COVID-19 would be disruptive to my everyday life”), α = 0.85; a 3-item scale assessing personal health importance (e.g., “My health is my top priority” and “Taking care of my health means a lot to me”), α = .74; and a 5-item scale assessing beliefs about whether behavioral health precautions are effective (e.g., “Washing your hands frequently is an effective method for avoiding COVID-19” and “Practicing social distancing is an effective method for avoiding COVID-19”), α = 0.72.
Prior to the first wave of data collection, we intended to include a fifth subscale that contained 3 items assessing trust in government regarding COVID-19 (e.g., “Government officials know best about what is good for citizens in managing COVID-19”, “Everyone should follow official recommendations”, and “Managing COVID-19 is the government’s job”), but the alpha was unacceptably low (α = 0.29). So instead, as indicated in the preregistration, we decided to include only the item with the most face validity for assessing trust in government regarding COVID-19: “Government officials know best about what is good for citizens in managing COVID-19”.
Participants also completed the Big 5 Inventory [34], one of the most popular and well-validated personality scales, which includes five subscales measuring extraversion (sociable, outgoing, energetic), openness (intellectual, imaginative, curious), conscientiousness (orderly, responsible, dependable), agreeableness (trusting, cooperative, warm), and emotional stability (calm, not neurotic, not irritable). This scale was included as a control variable to confirm the robustness of our predictor variables.
3. Results
3.1. Demographics
We first tested for relationships between gender, language, and age with each of our three behavioral outcomes (rule following, health precautions, and giving health advice). As can be seen in Fig. 1 , women were slightly more likely than men to follow rules, t(8280) = 6.93, p < .001; take health precautions, t(8280) = 8.04, p < .001; and make health recommendations to others, t(8280) = 5.02, p < .001.
Fig. 1.
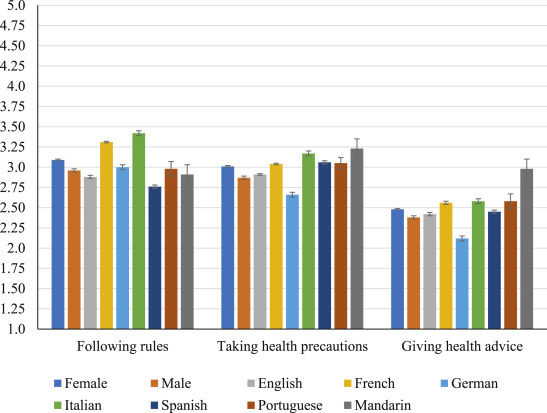
Differences between male and female participants as well as between languages for each of our three behavior outcomes.
There were also significant differences between participants from different nationalities (as categorized by the language in which they took the survey) in terms of rule following, F(6, 8310) = 116.85, p < .001; taking health precautions, F(6, 8310) = 49.73, p < .001; and making health recommendations, F(6, 8310) = 39.03, p < .001. These differences can be observed in Fig. 1, which indicates statistically significant differences where the error bars between nationalities do not overlap. In particular, French and Italian speaking participants were particularly likely to follow the rules, whereas Spanish speaking participants were less likely to follow rules relative to other participants. English speaking participants were significantly more likely to follow rules than Spanish speaking participants and significantly less likely than French, German, and Italian speaking participants.
Italian and Mandarin speaking participants were particularly likely to take health precautions. English speaking participants were significantly more likely to take health precautions than German speaking participants (who were significantly lower than all other groups), but significantly less likely than French, Italian, and Spanish. German participants were also significantly less likely to make health recommendations to others compared to all other participants. Note that we had relatively few Portuguese (n = 80) and Mandarin speaking (n = 23) participants, so their results should be interpreted with caution.
To our surprise, there was virtually no relationship between age and rule following, r = 0.003, p = .779, and only a very small relationship between age and taking health precautions, r = 0.061, p < .001. There was a slightly larger, though still small, relationship between age and giving health advice to others, r = .114, p < .001. This suggests that actual vulnerability to COVID-19 might not be a reliable predictor of rule compliance and health precaution behavior.
4. Correlations
We next examined the bivariate correlations between our three behavioral outcome variables (rule following, taking health precautions, and making health recommendations to others), our five COVID-19 belief predictors (effectiveness of health precautions, health importance, invulnerability, disruptiveness, and government trust), and the Big 5 subscales. Nearly all variables were significantly correlated because of the large sample size. Here, we only interpret relationships that reach at least a threshold of |r| ≥ 0.10, Cohen’s standard for a “small” effect [35]. The correlation matrix is available in Table 1 .
Table 1.
Correlations between three behavioral outcome measures (following rules, taking health precautions, and making health recommendations), and five COVID-19 beliefs (procedures effective, health importance, invulnerability, disruptivity, and trust in government), and the Big 5.
| Following |
Health |
Giving health |
||
|---|---|---|---|---|
| rules | Precautions | advice | ||
| Following rules | r | .587∗∗∗ | .322∗∗∗ | |
| p | <.001 | <.001 | ||
| Health precautions | r | .587∗∗∗ | .454∗∗∗ | |
| p | <.001 | <.001 | ||
| Giving health advice | r | .322∗∗∗ | .454∗∗∗ | |
| p | <.001 | <.001 | ||
| Procedures Effective | r | .476∗∗∗ | .669∗∗∗ | .359∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Health Importance | r | .356∗∗∗ | .533∗∗∗ | .449∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Invulnerabiliity | r | -.049∗∗∗ | -.089∗∗∗ | -.057∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Disruptivity | r | 0.017 | .226∗∗∗ | .159∗∗∗ |
| p | 0.112 | <.001 | <.001 | |
| Trust in Government | r | .192∗∗∗ | .215∗∗∗ | .130∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Agreeableness | r | .071∗∗∗ | .107∗∗∗ | .161∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Conscientiousness | r | .087∗∗∗ | .131∗∗∗ | .172∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Extraversion | r | −0.003 | .058∗∗∗ | .199∗∗∗ |
| p | 0.772 | <.001 | <.001 | |
| Openness | r | .054∗∗ | .095∗∗∗ | .181∗∗∗ |
| p | <.001 | <.001 | <.001 | |
| Emotional Stability | r | .000 | .028 | .068∗∗∗ |
| p | .990 | .010 | <.001 |
Note. ∗∗∗p < .001; ∗∗p < .01.
Higher belief that taking health precautions is effective (rs = 0.359-0.669, ps < .001), greater health importance (rs = 0.359-0.669, ps < .001), and stronger trust in government (rs = 0.130-0.215, p < .001) were all associated with more rule following, taking health precautions, and greater tendencies to give health advice to others. To our surprise, perceived (in)vulnerability was generally not a strong predictor of any of the behavioral outcomes (|r|s < 0.090), perhaps consistent with the finding that age was also generally unrelated to the behavioral outcomes. And belief that contracting COVID-19 would be disruptive was significantly associated with taking health precautions and greater tendencies to make health recommendations to others (rs = 0.159-0.226), but not with rule-following behavior (r = 0.017).
Regarding personality predictors, no traits predicted rule-following behavior (|r|s = 0.000-0.087); but higher agreeableness and conscientiousness predicted taking health precautions (rs = 0.107-0.131); and higher agreeableness, consciousness, extraversion, and openness all predicted higher tendencies to give health recommendations to others (rs = 0.161-0.199). Only emotional instability had virtually no associations with the health behavior outcomes (rs = 0.000-0.068).
4.1. Belief predictors of COVID-19 behaviors
To examine which beliefs were most relevant for predicting COVID-19 health behaviors, we conducted three stepwise regressions, regressing each of our three behavioral outcome variables on our five COVID-19 belief predictors in Step 1, and then controlling for age, gender, and the Big 5 subscales in Step 2. We used semipartial rs (the proportion of the variance in each health behavior uniquely explained by the individual predictor) as estimates of the predictor effect size. We again only interpreted those effects that reached a threshold of at least |semipartial r| ≥ 0.10, Cohen’s standard for a “small” effect [35].
Quite consistent patterns emerged from these three regressions. Belief that taking health procedures are effective for avoiding COVID-19 emerged as one of the strongest predictors of rule following, semipartial rs = .34-.35; taking health precautions, semipartial rs = .47; and giving health advice to others, semipartial rs = .18, with and without controls. Health importance was also consistently a fairly strong predictor of rule following, semipartial rs = .19; taking health precautions, semipartial rs = .25-.26; and giving health advice to others, semipartial rs = .26-.32. Perceived vulnerability, beliefs that getting COVID-19 would be disruptive, and government trust had very small to non-existent relationships with our three behavioral outcomes (however, there was a small trend indicating that believing that getting COVID-19 would be disruptive was associated with less rule following). Other variables, including age, gender, and personality traits, demonstrated very small to non-existent relationships with the three behavioral outcomes as well.(see Table 2 )
Table 2.
Each behavioral outcome regressed on all COVID-19 beliefs in Step 1 and controls in Step 2.
| Rule following | ||||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | F | R2 | Beta | t | p | 95% CI | Semipartial r | |
| Model (n = 8246) | 630.31 | .28 | <.001 | |||||
| Procedures Effective | .39 | 37.24 | <.001 | .52 | .58 | .35 | ||
| Health Importance | .22 | 20.33 | <.001 | .19 | .23 | .19 | ||
| Invulnerability | -.04 | −3.89 | <.001 | -.06 | -.02 | -.04 | ||
| COVID-19 disruptive | -.13 | −12.96 | <.001 | -.12 | -.09 | -.12 | ||
| Government trust |
.07 |
7.01 |
<.001 |
.04 |
.07 |
.07 |
||
| Model (n = 8246) | 272.81 | .29 | <.001 | |||||
| Procedures Effective | .39 | 36.65 | <.001 | .51 | .57 | .34 | ||
| Health Importance | .23 | 20.50 | <.001 | .20 | .24 | .19 | ||
| Invulnerabiliity | -.03 | −3.29 | .001 | -.05 | -.01 | -.03 | ||
| COVID-19 disruptive | -.13 | −12.61 | <.001 | -.12 | -.08 | -.12 | ||
| Government trust | .07 | 6.95 | <.001 | .04 | .07 | .07 | ||
| Gender | .05 | 5.24 | <.001 | .06 | .13 | .05 | ||
| Age | -.02 | −1.60 | .109 | .00 | .00 | -.02 | ||
| Agreeableness | .01 | 1.21 | .225 | -.01 | .03 | .01 | ||
| Conscientiousness | .02 | 1.57 | .117 | .00 | .03 | .02 | ||
| Extraversion | -.06 | −5.84 | <.001 | -.05 | -.03 | -.05 | ||
| Openness | .02 | 1.98 | .048 | .00 | .04 | .02 | ||
| Emotional Stability | -.03 | −3.09 | .002 | -.04 | -.01 | -.03 | ||
| Taking health precautions | ||||||||
| Predictor | F | R2 | Beta | t | p | 95% CI | Semipartial r | |
| Model (n = 8246) | 1860.84 | .53 | <.001 | |||||
| Procedures Effective | .53 | 62.34 | <.001 | .63 | .67 | .47 | ||
| Health Importance | .30 | 34.95 | <.001 | .24 | .27 | .26 | ||
| Invulnerability | -.03 | −4.07 | <.001 | -.04 | -.02 | -.03 | ||
| COVID-19 disruptive | .04 | 4.35 | <.001 | .01 | .04 | .03 | ||
| Government trust |
.03 |
3.78 |
<.001 |
.01 |
.03 |
.03 |
||
| Model (n = 8246) | 794.67 | .54 | <.001 | |||||
| Procedures Effective | .53 | 61.97 | <.001 | .63 | .67 | .47 | ||
| Health Importance | .29 | 33.29 | <.001 | .24 | .27 | .25 | ||
| Invulnerability | -.03 | −3.23 | .001 | -.04 | -.01 | -.02 | ||
| COVID-19 disruptive | .04 | 4.87 | <.001 | .02 | .04 | .04 | ||
| Government trust | .03 | 4.12 | <.001 | .01 | .03 | .03 | ||
| Gender | .06 | 8.06 | <.001 | .08 | .12 | .06 | ||
| Age | .01 | 0.71 | .480 | .00 | .00 | .01 | ||
| Agreeableness | .00 | −0.39 | .694 | -.02 | .01 | .00 | ||
| Conscientiousness | .02 | 2.53 | .011 | .00 | .03 | .02 | ||
| Extraversion | -.04 | −4.35 | <.001 | -.03 | -.01 | -.03 | ||
| Openness | .04 | 4.92 | <.001 | .02 | .05 | .04 | ||
| Emotional Stability | -.01 | −0.82 | .410 | -.01 | .01 | -.01 | ||
| Giving health advice | ||||||||
| Predictor | F | R2 | Beta | t | p | 95% CI | Semipartial r | |
| Model (n = 8246) | 516.65 | .24 | <.001 | |||||
| Procedures Effective | .20 | 18.69 | <.001 | .25 | .31 | .18 | ||
| Health Importance | .36 | 32.82 | <.001 | .33 | .37 | .32 | ||
| Invulnerability | -.02 | −2.15 | .031 | -.04 | .00 | -.02 | ||
| COVID-19 disruptive | .02 | 1.78 | .075 | .00 | .03 | .02 | ||
| Government trust | .02 | 1.91 | .056 | .00 | .03 | .02 | ||
| Model (n = 8246) | 254.95 | .27 | <.001 | |||||
| Procedures Effective | .20 | 18.77 | <.001 | .25 | .31 | .18 | ||
| Health Importance | .30 | 27.45 | <.001 | .28 | .32 | .26 | ||
| Invulnerability | -.02 | −1.54 | .123 | -.04 | .00 | -.02 | ||
| COVID-19 disruptive | .03 | 2.55 | .011 | .01 | .04 | .02 | ||
| Government trust |
.03 |
2.96 |
.003 |
.01 |
.04 |
.03 |
||
| Gender | .04 | 4.16 | <.001 | .04 | .11 | .04 | ||
| Age | .04 | 4.39 | <.001 | .00 | .01 | .04 | ||
| Agreeableness | .02 | 2.20 | .028 | .00 | .04 | .02 | ||
| Conscientiousness | .06 | 5.83 | <.001 | .03 | .06 | .06 | ||
| Extraversion | .08 | 6.98 | <.001 | .03 | .06 | .07 | ||
| Openness | .10 | 9.95 | <.001 | .08 | .12 | .09 | ||
| Emotional Stability | -.01 | −1.15 | .249 | -.02 | .01 | -.01 | ||
5. Discussion
Countries around the world are facing extraordinary challenges in implementing various measures to slow down the spread of COVID-19. Guided by international recommendations from the World Health Organization, a number of countries have implemented a series of measures to stop the spread of COVID-19. However, in order for these measures to be effective, the public must comply with these rules and recommendations. The present study examined predictors of COVID-19 health compliance behaviors during an ongoing pandemic while many governments are lifting official restrictions, thus elevating the importance of voluntary compliance. The primary objective of this study was to identify which beliefs about and attitudes toward COVID-19 predict 1) following government recommendations, 2) taking health precautions (including mask wearing, social distancing, handwashing, and staying at home), and 3) encouraging others to take health precautions.
In a large international sample, we discovered that (1) beliefs that taking health precautions are effective for avoiding COVID-19 and (2) concern for one’s own health are important predictors of voluntary compliance behaviors, including following government rules, taking various health precautions, and urging others to do the same. In contrast, age, perceived vulnerability to COVID-19, and perceived disruptiveness of catching COVID-19 were not significant predictors of health behaviors. We also found that trust in government was relatively unimportant for predicting voluntary compliance.
These findings suggest possible avenues and dead ends for interventions. Informing individuals about the efficacy of wearing masks, handwashing, social distancing, and staying at home, and perhaps also elevating the importance of general health, might increase voluntary compliance with government rules and recommendations. In contrast, warning individuals about their own vulnerability to COVID-19, providing details about the inconvenience of getting COVID-19, and targeting government trust might not.
5.1. Limitations and future directions
The present findings were based on a large international sample of Praditus application users. This sampling technique allowed us to collect a large sample that is more representative of a global population (and thus, more generalizable) than many psychological studies [32], but still is of course not representative of a true global population. Our sample was mainly from Western/European countries, relatively young, and overrepresented females. Moreover, our participants are likely to have been more tech savvy than the average global citizen, and thus more connected to media. Future research is needed to determine whether our findings are generalizable to broader populations.
Another limitation of the present work is that voluntary compliance behaviors were self-reported by participants. Rather than collecting objective measures of participants’ rule compliance and health precaution behaviors, we relied on participants to reflect on and report the extent to which they engage in these behaviors. Self-report measures vary in their correspondence to actual behaviors [36], as participants may be unable or unwilling to report accurate estimates. Future work might seek converging support for the present findings by examining actual health compliance behaviors.
Last, the HBM, in contrast to our results, might have predicted that perceived vulnerability and disruptivity (and therefore, also age) would be related to more health compliance behavior. Future research should explore why these variables appeared to be of relatively little importance for predicting COVID-19 health compliance behaviors. For example, are older and more vulnerable populations less willing to sacrifice their quality of life to take ongoing health precautions, which might cancel out the influences of age and vulnerability in predicting health compliance behaviors? Scholars might also build upon and extend our exploratory research in more detail, for example, by examining the role of perceived tradeoffs and personal risk-taking on behavior at different points during the pandemic, potentially also by changing the context and regarding employees in companies instead of citizens only.
6. Conclusion
We hope that this work will be of interest to scholars across many disciplines, including psychologists but also social scientists across various other disciplines (including those in management, public health, and public policy). This work has relevance to both research (i.e., it shines some light on the effectiveness of the HBM in predicting health compliance behaviors) and practical applications (it suggests potential avenues for interventions).
Our findings highlight the importance of belief in the efficacy of health behaviors in promoting compliance with health behavior recommendations. Although they have significance for the current pandemic, they may also be useful as a starting point for other kinds of government-led health behavior interventions regarding other public health concerns (e.g., smoking, obesity, vaccines), and particularly those that require voluntary compliance from a populace. Building trust in the efficacy of health-promoting behavior could increase willingness to engage in such practices, thus reducing the need for more intrusive government interventions, which might impel protest and backlash, particularly in democratic societies. Finding ways to encourage citizens to practice such behaviors voluntarily can save healthcare resources and, more importantly, lives.
CRediT authorship contribution statement
Cory Clark: Formal analysis, Writing - original draft. Andrés Davila: Writing - original draft. Maxime Regis: Writing - original draft.
APPENDIX. : Scale Items
BELIEF PREDICTORS.
|
Government trust (adapted from acceptance of physician authority, [26]; p. 384) |
Completely disagree | Completely agree | |||
|---|---|---|---|---|---|
| 1. Everyone should follow official recommendations. | 1 | 2 | 3 | 4 | 5 |
| 2. Government officials know best about what is good for citizens in managing COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 3. Managing COVID-19 is the government’s job. | 1 | 2 | 3 | 4 | 5 |
| Disruptivity (adapted from perceived severity: [30]; p. 225) | |||||
| 4. Having COVID 19 would be disruptive to my everyday life. | 1 | 2 | 3 | 4 | 5 |
| 5. Having COVID 19 would be disruptive to my life overall. | 1 | 2 | 3 | 4 | 5 |
| 6. Having COVID-19 would be disruptive to my physical health. | 1 | 2 | 3 | 4 | 5 |
| 7. Having COVID-19 would be disruptive to my social life. | 1 | 2 | 3 | 4 | 5 |
| Health importance (adapted from health involvement, [26]; p. 384) | |||||
| 8. I am concerned about my health and am taking action to prevent COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 9. My health is my top priority. | 1 | 2 | 3 | 4 | 5 |
| 10. Taking care of my health means a lot to me. | 1 | 2 | 3 | 4 | 5 |
| Invulnerability (adapted from perceived susceptibility, [29]; p. 277) | |||||
| 11. I am less likely than most people to get COVID-19 | 1 | 2 | 3 | 4 | 5 |
| 12. I am not at risk for getting infected with COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 13. My body could fight off COVID-19 infection. | 1 | 2 | 3 | 4 | 5 |
| 14. People like me don’t get COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 15. There is little chance that I could get or spread COVID-19 from what I do in my everyday life. | 1 | 2 | 3 | 4 | 5 |
| Effectiveness of health procedures (adapted from response efficacy: [27]; p. 296) | |||||
| 16. Avoiding crowds is an effective method for fighting COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 17. Practicing social distancing is an effective method for avoiding COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 18. Staying at home is an effective method for avoiding COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 19. Washing your hands frequently is an effective method for avoiding COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 20. Wearing a surgical mask is an effective method for avoiding COVID-19. | 1 | 2 | 3 | 4 | 5 |
| BEHAVIORAL OUTCOMES | |||||
| Rule following (adapted from therapy compliance, [26]; p. 384) | |||||
| 21. I follow the rules for sheltering in place. | 1 | 2 | 3 | 4 | 5 |
| 22. I have chosen not to visit friends and family. | 1 | 2 | 3 | 4 | 5 |
| 23. I only leave home for reasons sanctioned by the government. | 1 | 2 | 3 | 4 | 5 |
| Health precautions (adapted from intention, [27]; p. 297) | |||||
| 24. I intend to practice social distancing to avoid COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 25. I intend to stay at home to avoid COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 26. I intend to wash my hands frequently to avoid COVID-19. | 1 | 2 | 3 | 4 | 5 |
| 27. I intend to wear a surgical mask to avoid COVID-19. | 1 | 2 | 3 | 4 | 5 |
| Giving health advice (adapted from safety citizen role, [28]; p. 178) | |||||
| 28. I explain to others how to behave to stay healthy and safe. | 1 | 2 | 3 | 4 | 5 |
| 29. I express my opinions on health and safety matters even when others disagree. | 1 | 2 | 3 | 4 | 5 |
| 30. I frequently speak up and encourage others to engage in safe and healthy behavior. | 1 | 2 | 3 | 4 | 5 |
| 31. I help others take the correct actions to remain healthy and safe. | 1 | 2 | 3 | 4 | 5 |
| 32. I often make health- and safety-related recommendations about various activities. | 1 | 2 | 3 | 4 | 5 |
References
- 1.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Who . World Health Organisation; Geneva: 2020. Novel Coronavirus (2019-nCoV) SITUATION REPORT 51. [Google Scholar]
- 3.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kraus S., Clauss T., Breier M., Gast J., Zardini A., Tiberius V. The economics of COVID-19: initial empirical evidence on how family firms in five European countries cope with the corona crisis. Int. J. Enterpren. Behav. Res. 2020 doi: 10.1108/IJEBR-04-2020-0214. [DOI] [Google Scholar]
- 5.Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. 2020. https://spiral.imperial.ac.uk/handle/10044/1/77482
- 6.Kucharski A.J., Russell T.W., Diamond C., Liu Y., Edmunds J., Funk S. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Weerd W., Timmermans D.R., Beaujean D.J., Oudhoff J., van Steenbergen J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in The Netherlands. BMC Publ. Health. 2011;11:575. doi: 10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinstein N.D. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. J. Behav. Med. 1987;10(5):481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- 9.Rosenstock I.M., Strecher V.J., Becker M.H. « the health belief model and HIV risk behavior change ». In: DiClemente R.J., Peterson J.L., dirs, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. Springer US; Boston, MA: 1994. pp. 5–24. AIDS Prevention and Mental Health. [Google Scholar]
- 10.Janz N.K., Becker M.H. The health belief model: a decade later. Health Educ. Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 11.Rutter D., Quine L. Social cognition models and changing health behaviours. In: Rutter D., Quine L., editors. Changing Health Behaviour: Intervention and Research with Social Cognition Models. Open University Press; 2002. pp. 1–27. [Google Scholar]
- 12.Jones C.J., Smith H., Llewellyn C. Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review. Health Psychol. Rev. 2014;8(3):253–269. doi: 10.1080/17437199.2013.802623. [DOI] [PubMed] [Google Scholar]
- 13.Sulat J.S., Prabandari Y.S., Sanusi R., Hapsari E.D., Santoso B. The validity of health belief model variables in predicting behavioral change: a scoping review. Health Educ. 2018;118(6):499–512. [Google Scholar]
- 14.Mohammadi S., Ghajari H., Valizade R., Ghaderi N., Yousefi F., Taymoori P., Nouri B. Predictors of smoking among the secondary high school boy students based on the health belief model. Int. J. Prev. Med. 2017;8 doi: 10.4103/ijpvm.IJPVM_264_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoramabadi M., Dolatian M., Hajian S., Zamanian M., Taheripanah R., Sheikhan Z., Mahmoodi Z., Seyedi-Moghadam A. Effects of education based on health belief model on dietary behaviors of Iranian pregnant women. Global J. Health Sci. 2016;8(2):230–239. doi: 10.5539/gjhs.v8n2p230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soleymanian A., Niknami S., Hajizadeh E., Shojaeizadeh D., Montazeri A. Development and validation of a health belief model based instrument for measuring factors influencing exercise behaviors to prevent osteoporosis in pre-menopausal women (HOPE) BMC Muscoskel. Disord. 2014;15(1):61. doi: 10.1186/1471-2474-15-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villar O.A.E.-D., Montañez-Alvarado P., Gutiérrez-Vega M., Carrillo-Saucedo I.C., Gurrola-Peña G.M., Ruvalcaba-Romero N.A., García-Sánchez M.D., Ochoa-Alcaraz S.G. Factor structure and internal reliability of an exercise health belief model scale in a Mexican population. BMC Publ. Health. 2017;17(1):229. doi: 10.1186/s12889-017-4150-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao J., Song F., Ren S., Wang Y., Wang L., Liu W., Wan Y., Xu H., Zhou T., Hu T., Bazzano L., Sun Y. Predictors of condom use behaviors based on the health belief model (HBM) among female sex workers: a cross-sectional study in hubei province, China. PloS One. 2012;7:11. doi: 10.1371/journal.pone.0049542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vermandere H., Stam M.-A. van, Naanyu V., Michielsen K., Degomme O., Oort F. Uptake of the human papillomavirus vaccine in Kenya: testing the health belief model through pathway modeling on cohort data. Glob. Health. 2016;12(1):72. doi: 10.1186/s12992-016-0211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shahnazi H., Ahmadi-Livani M., Pahlavanzadeh B. 2020. Assessing Preventive Health Behaviors from COVID-19 Based on the Health Belief Model (HBM) Among People in Golestan Province: A Cross-Sectional Study in Northern Iran. (Research Square) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sarwar F., Panatik S.A., Sarwar F. Editorial: psychology of preventive behavior for COVID-19 outbreak. J. Res. Psychol. 2020;2(1):1–3. [Google Scholar]
- 22.Rosenstock I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974;2:328–335. [Google Scholar]
- 23.Champion V.L., Skinner C.S. The health belief model. Health Behav. Health Educ.: Theor. Res. Pract. 2008;4:45–65. [Google Scholar]
- 24.Bandura A. « Health promotion by social cognitive means ». Health Educ. Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 25.Vonasch A.J., Clark C.J., Lau S., Vohs K.D., Baumeister R.F. Ordinary people associate addiction with loss of free will. Addict. Behav. Rep. 2017;5:56–66. doi: 10.1016/j.abrep.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prigge J.K., Dietz B., Homburg C., Hoyer W.D., Burton J.L. Patient empowerment: a cross-disease exploration of antecedents and consequences. Int. J. Res. Market. 2015;32:375–386. [Google Scholar]
- 27.van Empelen P., Schaalma H.P., Kok G., Jansen M.W. Predicting condom use with casual and steady sex partners among drug users. Health Educ. Res. 2001;16:293–305. doi: 10.1093/her/16.3.293. [DOI] [PubMed] [Google Scholar]
- 28.Hofmann D.A., Morgeson F.P., Gerras S.J. Climate as a moderator of the relationship between leader-member exchange and content specific citizenship: safety climate as an exemplar. J. Appl. Psychol. 2003;88:170. doi: 10.1037/0021-9010.88.1.170. [DOI] [PubMed] [Google Scholar]
- 29.Rhodes S.D., Arceo R. Developing and testing measures predictive of hepatitis A vaccination in a sample of men who have sex with men. Health Educ. Res. 2004;19:272–283. doi: 10.1093/her/cyg026. [DOI] [PubMed] [Google Scholar]
- 30.Gerend M.A., Shepherd J.E., Monday K.A. Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Ann. Behav. Med. 2008;35:221–229. doi: 10.1007/s12160-008-9024-0. [DOI] [PubMed] [Google Scholar]
- 31.Asendorpf J.B., Conner M., De Fruyt F., De Houwer J., Denissen J.J., Fiedler K. Recommendations for increasing replicability in psychology. Eur. J. Pers. 2016;27:108–119. [Google Scholar]
- 32.Henrich J., Heine S.J., Norenzayan A. Most people are not WEIRD. Nature. 2010;466 doi: 10.1038/466029a. 29-29. [DOI] [PubMed] [Google Scholar]
- 33.Clark C.J., Bauman C.W., Kamble S.V., Knowles E.D. Intentional sin and accidental virtue? Cultural differences in moral systems influence perceived intentionality. Soc. Psychol. Pers. Sci. 2017;8:74–82. [Google Scholar]
- 34.John O.P., Srivastava S. The Big 5 trait taxonomy: history, measurement, and theoretical perspectives. Handb. Pers.: Theor. Res. 1999;2:102–138. [Google Scholar]
- 35.Cohen J. second ed. Lawrence Erlbaum; Lawrence Hillsdale, NJ: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 36.Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Gorber S.C., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behav. Nutr. Phys. Activ. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]


