Introduction
With more than 2.6 million cases diagnosed and 128,000 deaths to date in the United States (US) (Coronavirus Disease, 2019, 2020), the pandemic novel coronavirus COVID-19 has necessitated coordinated global action to slow the transmission of infection to avoid overwhelming health services. At the same time, there is increasing evidence that rates of infection, morbidity and mortality from COVID-19 are not evenly distributed in the population, with demographic and clinical risk factors clearly associated with risk of complications and death from the disease. Statistics from the U.S. Centers for Disease Control and Prevention (CDC) indicate that people 65 years of age and older represented 8 out of 10 deaths reported in the US, with individuals living in nursing homes or long-term care facilities also at elevated risk (CDC, 2020). Additionally, individuals with underlying medical conditions including heart disease, chronic lung disease, moderate to severe asthma, severe obesity, diabetes, chronic kidney disease, liver disease, and the immunocompromised are at increased risk (CDC, 2020). Other trends in risk factors beyond age and chronic disease have been emerging. For example, data from the CDC indicate a significantly higher case fatality in male versus female patients and African Americans compared to other racial groups (Provisional death counts, 2020).
One approach to characterizing and quantifying the underlying factors that make some communities or populations more or less susceptible to a particular health hazards is a vulnerability index. For example, The CDC's Social Vulnerability Index is widely used in health research, particularly in the fields of medical emergencies and evacuation planning (Flanagan et al., 2018). The Pampalon index is a deprivation index developed in Canada that aims to quantify health inequalities and wellness both in terms and social and material deprivation (Pampalon et al., 2009). Multiple indices of vulnerability to COVID-19 and its impacts in the US are emerging online and in rapid reports. These vulnerability indices have been largely based on different a priori selections of sociodemographic variables and chronic disease prevalence estimates within administrative areas, often at the county level (Surgo Foundation; RS21, 2020; Davis, 2020). One study applied the CDC's Social Vulnerability Index to COVID-19 mortality (Nayak et al., 2020) while others have used non-COVID disease statistics to drive the selection of index components (DeCaprio et al., 2020).
In this article, we demonstrate an empirical approach to developing a small-area COVID-19 vulnerability index using statistics on diagnoses in two counties from Washington State, USA, along with sociodemographic, occupational, and population health data.
Methods
Data
The COVID-19 diagnosis rates for the two most populous counties in Washington State were obtained from the King and Spokane County Departments of Health (COVID-19 data dashboard, Spokane County COVID-19 Case Data). Socio-demographic characteristics of ZIP codes were obtained from the 2018 American Community Survey 5-year estimates (United States Census, 2018). Registered deaths for the state were obtained from the Washington State Department of Health, Center for Health Statistics for the years 2011–2017 (Washington State Department of Health, 2018). Use of de-identified publicly available data did not warrant a review by an Institutional Review Board.
Measures
The outcome was COVID-19 diagnosis rates. King and Spokane County have made these data available to the public via data dashboards that list the number and rates of COVID-19 across ZIP codes. Data on diagnoses were obtained in mid April and updated June 10, 2020. Census data were used to calculate percent of nonwhite population, including African Americans, American Indian or Alaska Natives, Asians or other Pacific Islanders, multiracial, and Hispanics. Percent of population in transportation, protective service (firefighting and prevention, and other protective service workers including supervisors and Law enforcement workers including supervisors), healthcare support, and practitioners and technical occupations. Percent of population below federal poverty line, and population density. We used logarithmic transformation of population density in analyses.
The burden of comorbidities that have been linked to greater vulnerabilithy to COVID-19 was operationalized as mortality due to diabetes, heart disease, and chronic lower respiratory disease. For each ZIP code, rates of mortality from these conditions were calculated among people 65 years and above. We used decedents’ address, their underlying causes of death, and the associated International Classification of Diseases (ICD-10) codes as described previouslly. Residential locations with address matching accuracy of 80% or above were included in the analyses.
Statistical analysis
Unadjusted and adjusted multilevel modeling were performed to examine factors associated with COVID-19 diagnosis rates. We treated COVID-19 diagnosis rates across ZIP codes at level-1 nested within level-2 counties. Inclusion of random intercept in the multilevel models accommodated the likelihood of COVID-19 diagnosis rates to vary across the two counties. The data were analyzed using the lmer package in R. The significance level was set at 0.05 (two-tailed).
Results
One hundred and sixteen ZIP codes with a total of 8,773 COVID-19 diagnoses were included in the analyses (81 in King County and 35 in Spokane County). Four ZIP codes had missing COVID-19 diagnosis rates and were excluded. COVID-19 diagnosis rates varied from 0 to 362 per 100,000 people. Percent of non-white population ranged from one to 72%, percent of service occupations from zero to 30%, percent of population below federal poverty line from zero to 38%, mortality rates from zero to 3523 per 100,000 people, and population density from 0.18 to 18,990 per square miles.
Table 1 shows the results of unadjusted and adjusted multilevel models. In both the unadjusted and adjusted models, all index components were positively and significantly associated covid-19 diagnosis rates across WA state ZIP codes. In the adjusted model, percent of non-white population (B = 0.46), chronic disease burden (B = 0.27), percent of population in service occupations (B = 0.26), percent of population below poverty (B = 0.19), and higher population density (B = 0.18) remained significantly associated with diagnosis rates, with most of the coefficients increasing in amplitude compared to the bivariate models.
Table 1.
Unadjusted and adjusted multilevel analyses of factors associated with COVID-19 diagnosis rates in Washington State ZIP codes(n = 116; 81 in King County and 35 in Spokane County). Rates are based on 8,773 diagnosed cases.
| Predictors | Unadjusted Estimates, B (SE) | Adjusted Estimates, B (SE) |
||||
|---|---|---|---|---|---|---|
| % non-white | 0.68 (0.07)*** | 0.46 (0.07)*** | ||||
| Mortality from chronic disease | 0.27 (0.08)** | 0.27 (0.06)*** | ||||
| % population in service occupations | 0.26 (0.09)** | 0.26 (0.06)*** | ||||
| % population below poverty | 0.5 (0.07)*** | 0.19 (0.06)** | ||||
| Population density (log) |
0.34 (0.08)*** |
0.18 (0.06)** |
||||
| Random Effects | ||||||
| σ2 | 18470 | 27184 | 27930 | 20223 | 26112 | 11712 |
| τ00 | 1271 C | 33195 C | 42756 C | 41443 C | 13309 C | 18671 |
| ICC | 0.06 | 0.55 | 0.60 | 0.67 | 0.34 | 0.61 |
| Marginal R2/Conditional R2 | 0.489/0.522 | 0.045/0.570 | 0.038/0.620 | 0.143/0.719 | 0.110/0.410 | 0.381/0.761 |
NOTES: ***p < 0.001, **p < 0.01, *p < 0.05, C-County.
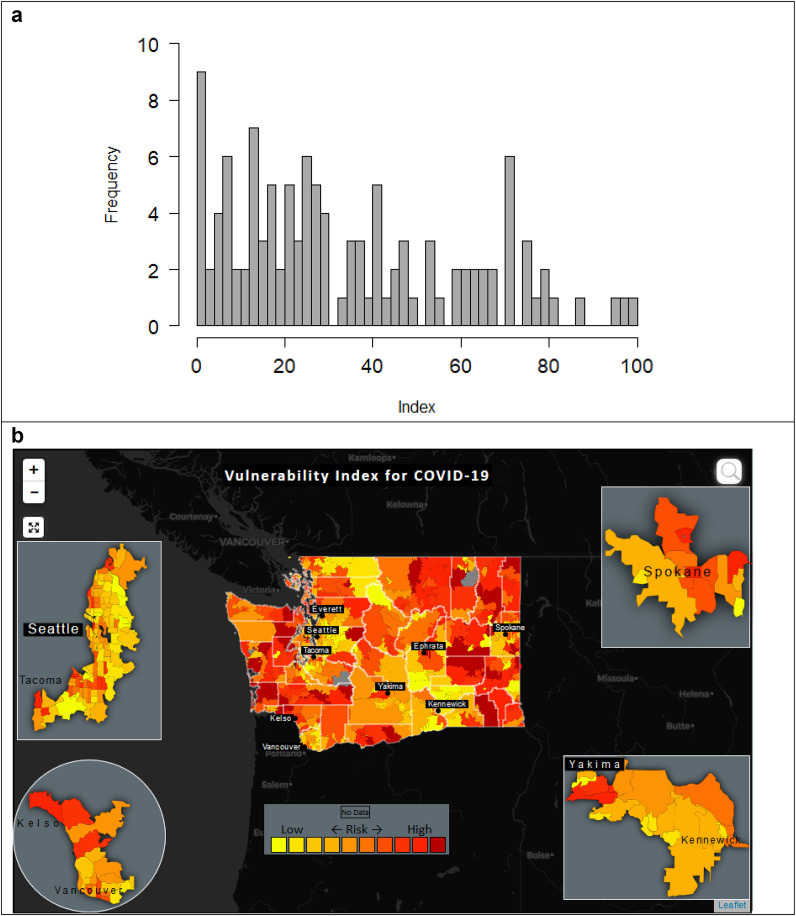
We used the standardized coefficients from the adjusted model to create an index that reflected risk of COVID-19 diagnosis for ZIP codes across Washington State. The median value for index was 31.9 with an interquartile of 13.7–45.8. The distribution of index values are shown in Fig. 1 a and an illustration of the variation in index values across ZIP codes in Washington are shown in Fig. 1b. An interactive version of the map is available at https://chaselab.net/VurnailityIndex/Index.htm.
Fig. 1.
Distribution of vulnerability index values (panel a) and a screen capture of an interactive choropleth map for Washington State illustrating variability in index for the state and select population centers (panel b). Analysis based on 8,773 dignosed cases within 116 ZIP codes. An interactive version of this map is available at https://chaselab.net/VurnailityIndex/Index.htm
Discussion
The COVID-19 vulnerability index presented here is driven by indicators of both social determinants and chronic disease burden. Our indicator of chronic disease burden, ZIP code-level mortality rates from diabetes, heart disease, and chronic lower respiratory disease, were strongly associated with ZIP code-level COVID-19 cases in Washington State. Social determinant indicators related to race (percentage of nonwhites) and socioeconomic factors (percentage of population in service occupations and poverty) were also strongly associated COVID-19 cases. Finally, population density was also positively associated with cases of COVID-19, as individuals in these environments tend to have higher likelihood of social contact, which results in an increase of COVID-19 transmission rates.
The demographic and socioeconomic indicators percentage of nonwhites, percentage of population below poverty, and percentage of population in service occupations. These indicators were significant both in bivariate models and in the multivariable adjusted model, concordant with recent reports, which indicate that Black, Hispanic, and poorer populations are more likely to be exposed to and impacted by COVID-19. There are several hypotheses attempting to explain this phenomenon. The first is that non-white populations are less likely to have jobs that can be performed from home. A recent published report by US Bureau of Statistics showed that only 19% of Black and 16.2% of Hispanic can Telework compared to 29.9% of white and 37% of Asian respectively. (Job flexibilities, 2019) Indeed, the percentage of the resident population in each ZIP code engaged in service occupations was strongly and significantly associated with infection. Secondly, these populations are more likely to have other underlying health conditions and less likely to have medical coverage and therefore less likely to access health services if they are experiencing symptoms of COVID-19 (Monsivais, 2019; Schmitt-Grohé et al., 2020), ultimately leading to an increase in transmission rates.
Our vulnerability index has several strengths. First, the index components (predictors) were selected based on the emerging literature, and the index was tested using actual COVID-19 cases at a ZIP code level, which are relatively small geographic areas. In addition, the primary data used in this index are widely available to local health authorities across the United States. Mortality data are routinely collected by the local departments of health across the nation, and in some states, are also available to researchers. The sociodemographic data, which makes up most of the indicators in the model, can be downloaded freely from the US census data website.
Relation to other indices
Several others have developed indices aiming to identify population at risk of COVID-19. For example, Researchers have applied the CDC's Social Vulnerability Index (Flanagan et al., 2018) to COVID-19 statistics in U.S. counties, finding that higher social vulnerability was associated with a higher case fatality rate (Nayak et al., 2020). The CV19 model was developed using an individual's near-term risk of severe complication from pneumonia, influenza, acute bronchitis, and other specified upper respiratory infections (DeCaprio et al., 2020). The Social Progress Initiative developed a vulnerability tool to map and rank the US's 500 largest cities at the census-tract level based on underlying health issues, population demographics, and health infrastructure (Davis, 2020). Similarly, RS21 has created the Urban Health Vulnerability Index (UHVI) to identify urban populations at high risk for COVID-19 by focusing on older adults and people with serious medical conditions (RS21, 2020). The COVID-19 Community Vulnerability Index (CCVI) from the Surgo Foundation maps anticipated negative impacts of coronavirus outbreaks utilizing COVID-19 indicators and the CDC's Social Vulnerability Index (SVI) at the US census tract, county and state level. (Surgo Foundation) However, the model presented here is the first to be validated using actual COVID-19 cases.
Limitations
A limitation of this index is that we only used ZIP code level COVID-19 cases from two counties in Washington State to assess its validity. The limited availability of data on COVID-19 cases and related deaths will need to be addressed before more insight on the impact of this disease on the population can be gleaned. We also tested only a limited range of sociodemographic and occupational risk factors, though these were selected based on clinical reports and observed patterns emerging from public health surveillance.
Policy implications and conclusions
This COVID-19 vulnerability index is based on ZIP code level and publicly-available data on demographic, socioeconomic, and medical risk factors can be used to understand population- and community-level variation in susceptibility to COVID-19 across Washington State. Making this and similar indices available to the scientific community, public health experts, and local governments will lead to a better understanding of where outbreaks may occur and which populations need more support than others. This could facilitate more effective resource allocation to communities with limited ability to manage transmission of COVID-19. Targeted interventions such as social distancing, the deployment of personal protective equipment for essential workers, and educational and training programs could help curtail the worst possible outcomes of this pandemic. However, there is a need to improve access to data on where and when COVID-19 cases and deaths occur.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2020.102377. Link for an online version of the vulnerability index map:https://chaselab.net/VurnailityIndex/Index.htm
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Coronavirus Disease 2019 (COVID-19): Cases in the U.S. 3 july 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html accessed 28 Apr2020. [Google Scholar]
- COVID-19 data dashboard. https://www.kingcounty.gov/depts/health/covid-19/data.aspx accessed 28 Apr2020.
- Davis D. 2020. Covid-19 Vulnerability Mapping for the US's 500 Largest Cities.https://socialprogress.blog/2020/04/03/covid-19-vulnerability-mapping-for-the-uss-500-largest-cities/ accessed 28 Apr2020. [Google Scholar]
- DeCaprio D., Gartner J., Burgess T., Kothari S., Sayed S. 2020. Building a COVID-19 Vulnerability Index. arXiv Prepr arXiv200307347. [Google Scholar]
- Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease Control and prevention's social vulnerability index. J. Environ. Health. 2018;80:34. [PMC free article] [PubMed] [Google Scholar]
- Job flexibilities and work schedules -- 2017-2018: Data from the american time use survey. 2019. https://www.bls.gov/news.release/flex2.nr0.htm Washington, D.C. [Google Scholar]
- Monsivais P., Amiri S., Denney J.T., Amram O. Area deprivation amplifies racial inequities in premature mortality: Analysis of 242,667 deaths in Washington State, USA 2011-15. Health & Place. 2019:102261. doi: 10.1016/j.healthplace.2019.102261. [DOI] [PubMed] [Google Scholar]
- Nayak A., Islam S.J., Mehta A., Ko Y.-A., Patel S.A., Goyal A., et al. 2020. Impact of Social Vulnerability on COVID-19 Incidence and Outcomes in the United States. medRxiv. [Google Scholar]
- Pampalon R., Hamel D., Gamache P., Raymond G. A deprivation index for health planning in Canada. Chron. Dis. Can. 2009;29(4):178–191. [PubMed] [Google Scholar]
- People Who Are at Higher Risk for Severe Illness. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html accessed 28 Apr2020. [Google Scholar]
- Provisional Death Counts for Coronavirus Disease (Covid-19) 2020. [Google Scholar]
- Rs21 . 2020. Urban Health Vulnerability Index.https://covid.rs21.io/ accessed 28 Apr2020. [Google Scholar]
- Schmitt-Grohé S., Teoh K., Uribe M. National Bureau of Economic Research; 2020. Covid-19: Testing Inequality in New York City. [Google Scholar]
- Spokane county COVID-19 case data. https://srhd.org/covid19cases accessed 28 Apr2020.
- Surgo Foundation The COVID-19 community vulnerability index map. https://precisionforcovid.org/ccvi
- United States Census . 2018. American Community Survey 5-year Estimates.https://www2.census.gov/programs-surveys/acs/summary_file/2018/data/?# accessed 28 Apr2020. [Google Scholar]
- Washington state department of health services center for health statistics: death data. https://www.doh.wa.gov/DataandStatisticalReports/HealthStatistics/Death accessed 12 Jun2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.