Abstract
Direct contact with devices such as elevator buttons, beepers, telephones, computer mice and keyboards can contribute to spread viral diseases. Here, we report our experience in designing, producing and dispatching three 3D-printed objected intending to lower the risks of COVID-19 contamination by limiting direct contacts: (1) fixed hand-free door openers, (2) door hooks and (3) button pushers. These devices were produced in industrial quantities and made available for free for Greater Paris University Hospitals and various state institutions as part of the 3D COVID project. In this short technical note, we describe the sequential organisation of the design and production and highlight the advantages of additive manufacturing in dealing with specific aspects of sanitary crises.
Keywords: COVID-19, Pandemic, Door opener, Virus, Infection control, Contamination
1. Introduction
In December 2019, Coronavirus Disease 2019 (COVID-19) first appeared in Wuhan, Hubei, China before spreading worldwide. To limit the progression of this deadly pandemic, personal protective equipment and various devices designed to avoid contacts with contaminated surfaces were quickly produced and dispatched within affected populations, and more specifically within hospitals [1].
Additive manufacturing was central in this effort to promptly obtain a large array of devices with different geometries. In fact, current 3D printers such as fused deposition modelling (FDM), stereolithography (SLA) and polyjet technologies allow both fast prototyping and reliable production [2], [3], [4], [5]. Here we report the design, production and dispatch processes of three 3D-printed objects:
-
•
fixed hands-free door openers;
-
•
door hooks;
-
•
button pushers,PASSER A LA LIGNE ICImade available for the trust of Greater Paris University Hospitals (Assistance Publique–Hôpitaux de Paris, AP–HP), the largest healthcare cluster in Europe, and the University of Paris, as part of the 3D COVID project, an innovative approach to emergency health device production based on additive manufacturing.
We decided to focus on these three devices based on recent studies assessing viral contamination of various surfaces within hospitals. In fact, viral contamination has been screened in different sites of a Chinese hospital, such as desktops, door handles, elevator buttons telephones or telephones: virus was found on buttons and phones, among others, but not on handles [6]. Nevertheless, the virus is known to survive 72 hours on plastic and stainless steel surfaces [7]. We thus identified buttons and doors as two potential contamination zones and produced three objects designed to limit disease spread when opening doors and pressing call buttons.
2. Technical note
2.1. 3D COVID initiative
To anticipate various shortages in personal protective equipment and medical devices during the wave of COVID-19 in the Greater Paris region, AP–HP and University of Paris settled an emergency additive manufacturing platform including 60 FDM machines (44 F120, 13 F170 and 3 F370 from Stratasys, Eden Prairie, MN, USA). Within 4 days, starting 30th of March 2020, the printers were ordered, delivered, and settled in the XVIIth century Port-Royal Abbey in the centre of Paris (Fig. 1 ). Five full-time engineers from a Parisian start-up specialised in 3D design and 3D printing (Bone3D, Paris, France) were hired for four months with conception and maintenance duties. The needs of health professionals were centralised via a website (Covid3D.org) and analysed with the help of pharmacists from the Agence Générale des Équipements et des Produits de Santé (AGEPS), specialised in medical device regulations. Black and white Acrylonitrile Butadiene Styrene (ABS) was used as the main raw material for the FDM printers and sufficient supplies for 24/7 production during a period of 4 months were included into the budget of the 3D COVID initiative. The entirety of the project was funded by private charity money (Kering Group, Paris, France). The designs were made available open-source on the website of the project in STL format. Five Form 2 SLA printers (Formlabs, Somerville, Mass, USA), one J735 and one J750 (both from Stratasys, Eden Prairie, MN, USA), previously owned by Bone3D and APHP, were also included into the initiative to benefit from various types of additive manufacturing processes beyond FDM if required.
Fig. 1.
The 3D COVID initiative: 60 3D-printers within a XVIIth century abbey in the centre of Paris, producing protection devices and medical devices in response to the COVID-19 pandemic.
2.2. Design and production of hand-free door openers
Hands-free door openers were defined as devices fixed to door handles and activated using the forearm or the elbow. This device had to be easy to install, easy to clean and fast to produce. Despite the great variety of door handles in hospitals, schools and state buildings, several shapes were redundant, such as cylindrical bent extrusions. The design of the device had to allow the door handle to rotate to release the latch, and to allow the user open and close the door.
Based on these prerequisites, we designed two types of door openers:
-
•
opener fixed using clips (Fig. 2 a and b) adapted to straight handles with circular sections;
-
•
opener fixed using three cable ties running into grooves designed to be printed without support (Fig. 2c–f), adapted to straight handles with circular sections, and to curved handles with/without circular sections.
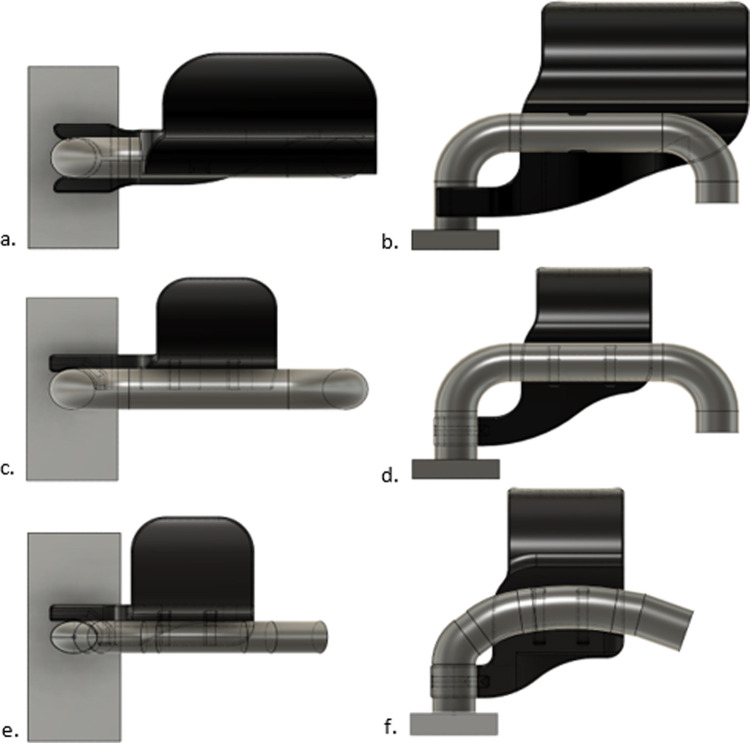
Fig. 2.
Hands-free door openers. (a,b): device using clips on a straight handle with circular section; (c,d): device using cable ties on a straight handle with circular section; (e,f): device using cable ties on a curved handle with elliptical section.
For handles with circular cross sections (Fig. 2a–d), contact surfaces were a quarter cylinder with a circular base and a radius equal to the handle radius. Three cross-section diameters were produced based on the needs: 18, 19 and 20 mm.
For handles with curved cross-sections (Fig. 2e and f), contact surfaces were spline curves adapted to each specific case. To date, two different handles with a curved profile have been produced.
Door openers were printed using FDM devices (J120, J170 and J370). Layer thickness was 0.33 mm, with a filling density of 43% and a wall thickness of 2 mm (Fig. 3 ). The support angle was calibrated to 30° to avoid excessive amount of material. On average, 5 pairs of door openers (left and right) were printed in 22 h for the design with clips and in 17 hours for the design with cable ties; printing position was optimised in order to obtain good surface quality [8] (Fig. 4 ). On the 15th of May 2020, after 45 days of activity, around 750 clipped door handles had been dispatched to three AP–HP hospitals – 150 for Pitié-Salpêtriere University Hospital, Paris, 200 for Necker–Enfants Malades University Hospital, Paris and 400 for Beaujon University Hospital, Clichy. Over 1600 devices with cable ties had also been dispatched in various hospitals, schools, and research institutions – 900 for Imagine Institute, Paris, 165 for École Élémentaire de l’Arbalète, Paris, 65 for École Élémentaire publique Saint-Jacques (two state elementary schools), 400 for AGEPS and 80 for University of Paris (Fig. 5 ).
Fig. 3.
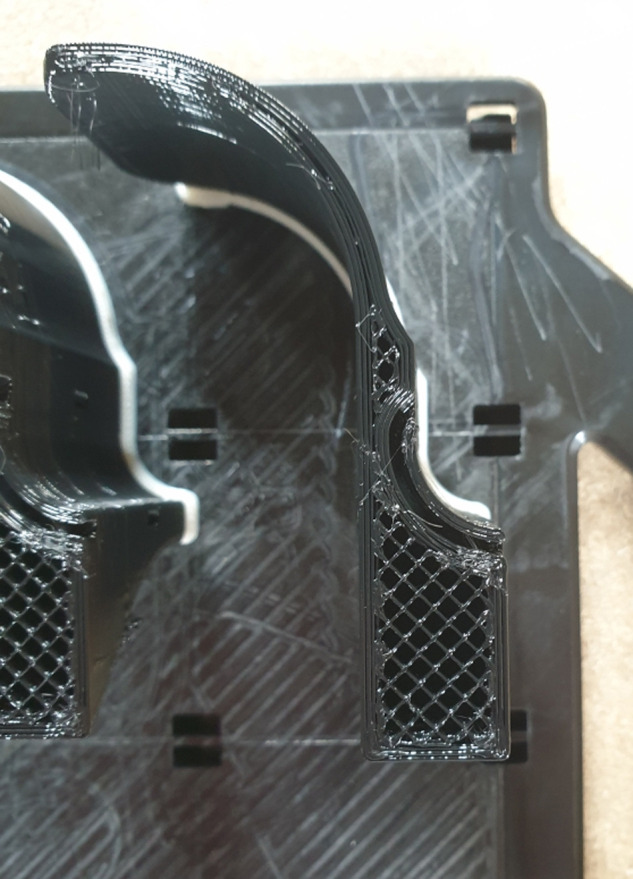
Printing characteristics on a J120 device: layer thickness = 0.33 mm, filling density = 43%, wall thickness = 2 mm; the use of support was optimised in order to decrease post-treatment time.
Fig. 4.
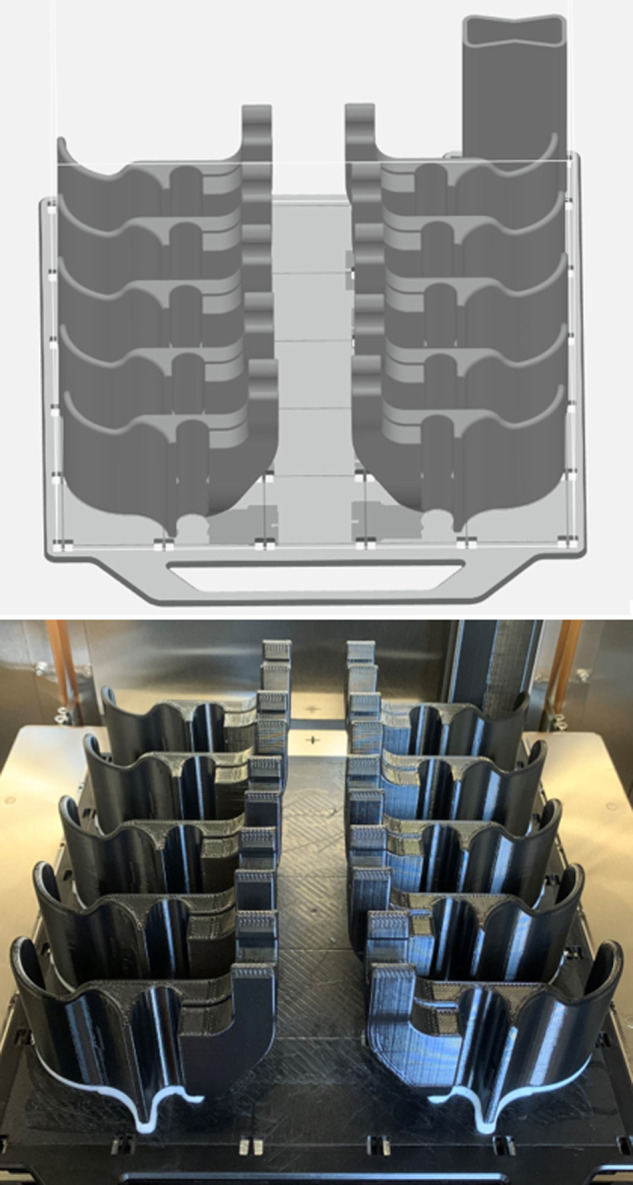
Ten clipping door openers in a J120 device: planification using Grab Cad Print (Stratasys, Eden Prairie, MN, USA) and actual result.
Fig. 5.
Hands-free door openers using cable ties on two types of door handles.
During the production process, the length of the blade was reduced from 150 mm to 100 mm to reduce the amount of material used without any functional consequences.
2.3. Door hook
Some door handles have a geometry that does not allow the design of an obvious fixed door opener. As a solution to this issue, a hook protected by an easily retractable sheath was developed in ABS (Fig. 6 ).
Fig. 6.
Door hook in closed (left) and open (right) positions.
The filling density was 100% for both the hook and its sheath and printing time using F120, F170 or F370 FDM printers was 90 minutes. The length of the hook was 80 mm with a 5 mm thickness. The hook and the scabbard are printed separately and easily combined once produced. On the 15th of May 2020, 20 hooks had been produced for two elementary schools after discussing the difficulties of producing fixed door handles.
2.4. Button pusher
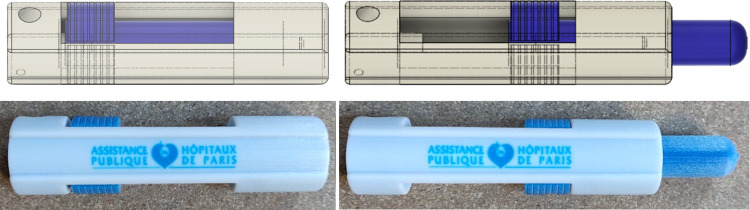
A button pusher formed by a cylindrical tube containing a retractable tip that could be blocked by a pressure pin was designed (Fig. 7 ). FDM was not suitable for this device, as a gap was needed between the tube and the retractable tip. Polyjet J735 and J750 printers were thus used to produce this device, with VeroWhite and VeroBlue resins (Stratasys, Eden Prairie, MN, USA). Button pushers were printed already assembled, and thus required post-treatment using a waterjet to remove support material. A second phase of cleaning, using a solvent, was necessary before dispatching. On the 15th of June 2020, 850 button pushers had been produced for Pitié-Salpêtrière University Hospital.
Fig. 7.
Button pusher in closed (left) and open (right) positions. On the first row, the CAO and on the second one, the device once produced.
3. Discussion and conclusion
Additive manufacturing was specifically adapted to the production of important quantities (several thousands of pieces) of devices with a common overall shape but with specific minor differences – such as door openers adapted to several door handles. In this context, 3D printing could ensure both prototyping and production. For devices with a unique shape needed in large quantities – such as door hooks and button pushers – plastic injection moulding was the ideal long-term solution and 3D printing was used as an intermediate technique in a context of sanitary crisis.
A recent study [7] demonstrated that SARS-CoV-2 did not survive over 4 hours on a copper-coated surface – as opposed to a survival time of 72 hours on a plastic surface. In fact, in March 2020, the Ministry of Science and Technology of Taiwan coated the doorknobs and the elevator buttons of its buildings with copper foils1 . Further studies are required to assess the efficiency of this procedure, as well as the contamination patterns of the three devices reported here.
3D printing allowed the design and dispatch of large quantities of protection devices in response to a sanitary crisis thanks to the installation of a production centre within a large hospital, in close connection with medical and engineering teams. The 3D COVID initiative was the first example of a large-scale emergency medical 3D-printing production platform and raised numerous questions, including the production of medical devices. With the development of affordable and reliable 3D-printing technologies, the scope of additive manufacturing in crisis situations will expand and new regulatory frameworks will have to be developed to control in house production in critic conditions such as the current pandemic, combining high demand in medical material and supply chain issues.
Funding
The 3D COVID projet has been fully funded by Kering (Paris, France) and the printers now belong to Assistance Publique–Hôpitaux de Paris.
Disclosure of interest
P.M. François, J. Kosior and J. Adam work for BONE3D, the company commissioned by AP–HP to designing and producing protection devices in response to the pandemic, as part of the 3D COVID initiative led by RH Khonsari.
Footnotes
Coating doorknobs with copper foil as COVID-19 prevention: MOST – Focus Taiwan. (n.d.). Retrieved May 23, 2020, from https://focustaiwan.tw/society/202003260010.<Normal>
References
- 1.Tino R., Moore R., Antoline S., Ravi P., Wake V., Ionita C.N., et al. COVID-19 and the role of 3D printing in medicine. 3D Print Med. 2020;6:11. doi: 10.1186/s41205-020-00064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amin D., Nguyen N., Roser S.M., Abramowicz S. 3D Printing of face shields during COVID-19 pandemic: a technical note. J Oral Maxillofac Surg. 2020 doi: 10.1016/j.joms.2020.04.040. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erickson M.M., Richardson E.S., Hernandez N.M., Bobbert D.W., Gall K., Fearis P. Helmet modification to PPE with 3D printing during the COVID-19 pandemic at Duke University Medical Centre: a novel technique. J Arthroplasty. 2020 doi: 10.1016/j.arth.2020.04.035. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flanagan S.T., Ballard D.H. 3D printed face shields: a community response to the COVID-19 global pandemic. Acad Radiol. 2020 doi: 10.1016/j.acra.2020.04.020. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ms D.P., Rao Y.J., Mitic K., Obaid S.N., Pierce D., Huckenpahler J., et al. 2020. Rapid prototyping of reusable 3D-printed N95 equivalent respirators at the George Washington University. [in press] [DOI] [Google Scholar]
- 6.Nuñez P.J., Rivas A., García-Plaza E., Beamud E., Sanz-Lobera A. Dimensional and surface texture characterization in fused deposition modelling (FDM) with ABS plus. Procedia Eng. 2015;132:856–863. doi: 10.1016/j.proeng.2015.12.570. [DOI] [Google Scholar]
- 7.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl J Med. 2020 doi: 10.1056/NEJMc2004973. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu S., Wang Y., Jin X., Tian J., Liu J., Mao Y. Environmental contamination by SARS-CoV-2 in a designated hospital for Coronavirus Disease 2019. Am J Infect Control. 2020 doi: 10.1016/j.ajic.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]