Abstract
Patient: Female, 36-year-old
Final Diagnosis: Pancreatitis
Symptoms: Abdominal and back pain
Medication:—
Clinical Procedure: Laparoscopic pancreatic surgery
Specialty: Gastroenterology and Hepatology • General and Internal Medicine • Surgery
Objective:
Unusual clinical course
Background:
Chronic pancreatitis is a slowly progressive inflammatory disease, affecting patients’ quality of life due to chronic pain as well as endocrine and exocrine pancreatic insufficiency. Patients often choose surgery if medical and endoscopic interventions fail. Surgical approaches for chronic pancreatitis can be categorized as follows: resection of the diseased gland, diversion and drainage of the dilated pancreatic duct, or a combination of these approaches. Frey’s procedure, which involves resection and drainage by longitudinal pancreaticojejunostomy and coring out of the pancreatic head, is reserved for patients with debilitating pain. Although laparoscopic surgery is gaining popularity in recent years due to its noninvasiveness and cosmetic benefit, few reports describe performing Frey’s procedure laparoscopically.
Case Report:
A 36-year-old Japanese female with chronic pancreatitis complained of back pain and pain in the left upper quadrant abdomen. Plain computed tomography of her abdomen revealed a dilated main pancreatic duct containing diffuse calculi extending to the pancreatic parenchyma. Laboratory findings, including amylase level, were within normal ranges. She was diagnosed with chronic pancreatitis, and subsequently underwent a laparoscopic Frey’s procedure. To our knowledge, we are the first to improve operative field visibility by using a Penrose drain to move the stomach from the line of sight. Postoperatively, the patient did well and was discharged 10 days after surgery. She remained symptom-free without medications for 80 months.
Conclusions:
Due to its noninvasive nature and cosmetic advantages, laparoscopic Frey’s procedure may be an attractive therapeutic option for chronic pancreatitis.
MeSH Keywords: Abdominal Pain; Laparoscopy; Pancreatitis, Chronic
Background
Chronic pancreatitis is an inflammatory disease that reduces patients’ quality of life due to chronic pain as well as endocrine and exocrine pancreatic insufficiency [1–3]. Patients often choose surgery if medical and endoscopic interventions fail. Frey’s procedure for chronic pancreatitis, involving longitudinal pancreaticojejunostomy and coring out of the pancreatic head, is reserved for patients with debilitating pain [1–3]. Recently, laparoscopic pancreatic surgery has become increasingly preferred because of its noninvasiveness [4–6]. However, limited reports of Frey’s procedure performed laparoscopically exist [7–9]. To our knowledge, we present the first case of chronic pancreatitis successfully treated by laparoscopic Frey’s procedure in a Japanese patient.
Case Report
A 36-year-old Japanese female with a history of alcohol abuse was referred to our hospital primarily complaining of left upper quadrant abdominal and back pain. Plain computed tomography of her abdomen revealed a dilated main pancreatic duct containing diffuse calculi (particularly in the pancreatic head) extending to the pancreatic parenchyma (Figure 1). Laboratory findings, including amylase, were within normal ranges. She was diagnosed with chronic pancreatitis, and we deemed calculus removal necessary to relieve her pain. To abate her symptoms, surgically coring out the pancreatic head was preferable over endoscopic treatment, which would, to a certain extent, remove the calculus in the main pancreatic duct but neglect those in the parenchyma of the pancreatic head. Considering her long-term prognosis, we opted to preserve pancreatic function, deeming it necessary to remove the calculus surgically. Since it was possible to conduct Frey’s procedure laparoscopically, we performed this treatment after obtaining the patient’s informed consent.
Figure 1.
Plain computed tomography of the abdomen revealed diffuse calculi in a dilated main pancreatic duct and parenchyma, particularly in the pancreatic head.
Under general anesthesia, we placed the patient in the lithotomy position. The operating surgeon stood on the patient’s right side, the assistant surgeon stood on the left, and the laparoscope assistant was between the patient’s legs. We inserted a trocar for the laparoscope through an incision in the umbilicus. Two trocars (5 mm) were inserted bilaterally at the subcostal pararectal area, with another two (12 mm) at the flanks beside the umbilicus.
We divided the gastrocolic omentum using an ultrasonic dissector to open the bursa omentalis and exposed the whole pancreas by dissecting its surrounding inflammatory adhesions. The stomach was percutaneously suspended at the epigastrium using an 8 mm Penrose drain with 3 tied threads (at both ends and the center) through two 5 mm trocars (Figure 2). After mobilizing the pancreatic head and duodenum, we first exposed the gastroduodenal artery, followed by the gastrocolic trunk. Then, we cut the connecting branches of the gastrocolic trunk to the pancreatic head. We located the dilated main pancreatic duct with a linear laparoscopic ultrasound device, which was longitudinally cut open with an ultrasonic dissector at the ventral side of the pancreas. We extracted the ductal stones while distally and proximally opening the pancreatic duct (Figure 3). While preserving the anterior superior pancreaticoduodenal and gastroduodenal arteries, we excavated the parenchyma of the pancreatic head with an ultrasonic dissector to the posterior wall of the pancreatic duct, being careful to identify and preserve the biliary duct in the pancreatic parenchyma by employing a linear laparoscopic ultrasound device. We avoided excessive excavation of the pancreatic head parenchyma while prioritizing main pancreatic duct drainage (Figure 4). We also preserved the uncinate process with a few calculi. Laproscopically, we removed all identified stones in the main pancreatic duct and parenchyma of the pancreatic head (Figure 5).
Figure 2.

An 8 mm Penrose drain (black arrowheads) with 3 tied threads through two 5-mm trocars, and the epigastric abdominal wall was used to draw the stomach (black arrows) out of the field of view. White arrowheads indicate the omentum, and white arrows indicate the pancreas.
Figure 3.

The main pancreatic duct was cut open longitudinally at the ventral side of the pancreas with an ultrasonic dissector. Ductal stones (black arrow) were extracted while opening the pancreatic duct distally and proximally.
Figure 4.

We excavated the parenchyma of the pancreatic head (black arrows) with an ultrasonic dissector to the posterior wall of the pancreatic duct, being careful to identify and preserve the biliary duct in the pancreatic parenchyma with a linear laparoscopic ultrasound device.
Figure 5.
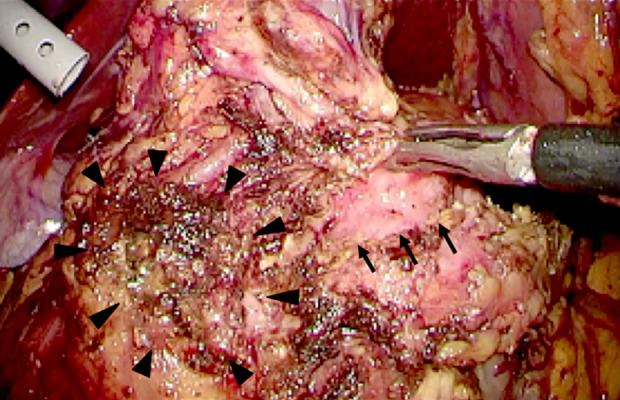
Laparoscopically identified stones in the main pancreatic duct (black arrows) and parenchyma of the pancreatic head (black arrowheads) was removed.
Then, we adopted a retrocolic approach to performing Roux-en-Y reconstruction by lifting the transverse colon upward and cutting the jejunum 35 cm from the proximal end with an endo linear cutter. The Roux jejunum was (without tension) positioned longitudinally along the opened main pancreatic duct, then we placed stay sutures between them at both ends. Having opened the Roux jejunum longitudinally, we performed a single-layer, side-to-side pancreaticojejunostomy using absorbable threads with running sutures (Figure 6). Using an endo linear cutter, we performed a side-to-side jejunojejunostomy 40 cm distal to the pancreaticojejunostomy.
Figure 6.

Single-layer side-to-side pancreaticojejunostomy consisted of running sutures using absorbable threads. Black arrows indicate the main pancreatic duct that was cut open, and black arrowheads indicate the jejunum.
Postoperatively, the patient did well and was discharged 10 days after surgery. We performed laboratory examinations every 6 months and plain computed tomography every year. She remained symptom-free without medications for 80 months. Laboratory findings, including amylase, were within normal ranges, and plain computed tomography revealed no pancreatitis relapse.
Discussion
Frey’s procedure for chronic pancreatitis, involving a combination of pancreatic head resection with drainage of the remnant pancreases, is reserved for patients with debilitating pain, with the laparoscopic equivalent gaining popularity in recent years due to its noninvasiveness and cosmetic benefit [1–6]. Tan et al. described the successful treatment of 7 out of 9 patients who underwent laparoscopic Frey’s procedure for chronic pancreatitis, showing the comparable outcome of laparoscopic Frey’s procedure to that of open surgery [8]. Despite positive outcomes, there remain few publications of laparoscopic Frey’s procedure [7–10]. Kilburn et al. described the importance of appropriate patient selection, remarking that some patients are poor candidates for laparoscopic Frey’s procedure, with technical difficulties commonly manifested in patients with a history of extensive abdominal surgery or obesity [10]. Our patient was suitable for the procedure since they had a body mass index (BMI) of 21, which is within the normal range by Asia-Pacific standards. We added our unique techniques in laparoscopic Frey’s procedure. For example, we had excellent laparoscopic visualization by removing the stomach from the field of view by using an 8 mm Penrose drain with tied threads through two 5 mm trocars on the epigastric abdominal wall. Soft coagulation also contributed to our success, having provided sufficient hemostasis for bleeding in the intrapancreatic artery and venous branches. Furthermore, we spared pancreatic function by avoiding coring out of the pancreatic head excessively, while achieving sufficient removal of the stones. Using these techniques, we avoided postoperative disability and reduced the length of hospital stay.
Conclusions
Laparoscopic Frey’s procedure may be an attractive alternative to treat chronic pancreatitis with calculus due to its noninvasiveness and cosmetic benefit. Although evaluating more cases is necessary, the accumulation of reports regarding laparoscopic Frey’s procedure for chronic pancreatitis is vital to widen our existing knowledge of pancreatic surgery.
Acknowledgments
We would like to thank Editage by CACTUS for providing proofreading our manuscript.
Footnotes
Conflicts of interest
None.
References:
- 1.Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2(6):701–7. doi: 10.1097/00006676-198711000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Roch AM, Brachet D, Lermite E, et al. Frey procedure in patients with chronic pancreatitis: Short and long-term outcomes from a prospective study. J Gastrointest Surg. 2012;16(7):1362–69. doi: 10.1007/s11605-012-1904-8. [DOI] [PubMed] [Google Scholar]
- 3.Ueda J, Miyasaka Y, Ohtsuka T, et al. Short- and long-term results of the Frey procedure for chronic pancreatitis. J Hepatobiliary Pancreat Sci. 2015;22(3):211–16. doi: 10.1002/jhbp.176. [DOI] [PubMed] [Google Scholar]
- 4.Mabrut JY, Fernandez-Cruz L, Azaqra JS, et al. Laparoscopic pancreatic re-section: Results of a multicenter European study of 127 patients. Surgery. 2005;137(6):597–605. doi: 10.1016/j.surg.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Kooby DA, Hawkins WG, Schmidt CM, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: Is laparoscopic resection appropriate? J Am Coll Surg. 2010;210(5):779–87. doi: 10.1016/j.jamcollsurg.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 6.Justin V, Fingerhut A, Khatkov I, Uranues S. Laparoscopic pancreatic resection – a review. Transl Gastroenterol Hepatol. 2016;1:36. doi: 10.21037/tgh.2016.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper MA, Datta TS, Makary MA. Laparoscopic Frey procedure for chronic pancreatitis. Surg Laparosc Endosc Percutan Tech. 2014;24(1):16–20. doi: 10.1097/SLE.0b013e31828f6edf. [DOI] [PubMed] [Google Scholar]
- 8.Tan CL, Zhang H, Li KZ. Single center experience in selecting the laparoscopic Frey procedure for chronic pancreatitis. World J Gastroenterol. 2015;21(44):12644–52. doi: 10.3748/wjg.v21.i44.12644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saravanan J, Sukumar R, Jeswanth S, Ravichandran P. Therapeutic angioembolization of bleeding pancreaticoduodenal artery pseudoaneurysm following laparoscopy assisted Frey’s procedure. Int J Case Rep Imag. 2013;4(5):275–78. [Google Scholar]
- 10.Kilburn DJ, Chiow AKH, Leung U, et al. Early experience with laparoscopic Frey’s procedure for chronic pancreatitis: A case series and review of literature. J Gastrointest Surg. 2017;21(5):904–9. doi: 10.1007/s11605-016-3343-4. [DOI] [PubMed] [Google Scholar]



