Abstract
Introduction
Bilateral and simultaneous quadriceps tendon rupture is rarely observed. This case series evaluates 3 patients with bilateral ruptures of the quadriceps tendon. The purpose of this case series is to display the effectiveness of the suture anchor surgical repair technique in these patients.
Case Presentations
Three obese male patients experienced some type of traumatic injury to the knee extensor mechanism, resulting in bilateral quadriceps tendon ruptures. Each of the patients was evaluated and given operative and nonoperative treatment options, and they all elected to undergo surgical tendon repair. Two double-loaded anchors were placed into the superior pole of the patella, allowing the tendons to be reduced back to their original positioning. Postoperatively, all patients were given the same guidelines for physical therapy, and their progress was monitored periodically. Each patient returned to his normal level of physical activity. Range of motion at the knee and weight bearing were reestablished in all 3 patients.
Discussion
These quadriceps tendon ruptures occurred in patients with a predisposition to injury as a result of excessive weight bearing. When addressing bilateral quadriceps tendon ruptures in this patient population, we found that a suture anchor-based construct allows for a secure repair, early initiation of physical therapy, and a noted improvement in pain scores on the Visual Analog Scale.
Keywords: obesity, quadriceps tendon, suture anchor
INTRODUCTION
The extensor mechanism of the knee is an essential component of locomotion. The primary components of knee extension include the quadriceps muscles, quadriceps tendon, patella, and patellar tendon as well as the retinaculum.1 Quadriceps ruptures are commonly associated with corticosteroid use or systemic disease, such as hyperparathyroidism, renal failure, or connective tissue disease. These diseases compromise the patient’s blood supply and/or collagen production over time, which can lead to weakened tendons.2 This weakening of the tendons makes them more vulnerable to rupture. Aside from these risk factors, quadriceps tendon ruptures are also seen when an eccentric load is placed on the knee during flexion, such as when one is attempting to land from a jump or when falling.
Obesity has been linked to tendinopathy because of tendon overload and chronic inflammation.3,4 Tendon overload, as it relates to the tendon continuum theory, suggests that as a tendon is continuously exposed to an increased yield and load, it progressively degenerates until the damage is no longer reversible.3 Chronic inflammation is also linked to obesity. As obesity advances, there is hypertrophy of adipocytes, which leads to an increase in macrophage secretion and production of a proinflammatory environment.4 These 2 factors contribute to structural tendon damage as well as irritation and joint pain.
The rupture of a single quadriceps tendon represents a substantial percentage of extensor mechanism injuries, especially in patients older than the age of 50 years.5 However, bilateral and simultaneous quadriceps tendon rupture is rarely observed. According to Neubauer and et al6, “Only 66 cases have been reported in the English literature between the first description in 1949 and 2002.”
This case report evaluates 3 patients with bilateral ruptures of the knee extensor mechanism. Each patient did not have a history of a systemic disease that is commonly associated with quadriceps rupture but did have obesity. Although the tendon injury these patients experienced was linked to their specific trauma (sudden eccentric knee flexion), their obesity put them at a higher risk of complete rupture of the quadriceps tendon. In these difficult cases of bilateral quadriceps tendon ruptures, it is important to perform a timely repair of the extensor mechanism that allows for immediate weight bearing, early ambulation, and knee range of motion. In this case series, we review the clinical outcomes of 3 obese patients with bilateral quadriceps tendon tears treated with a suture anchor-based repair construct.
CASE PRESENTATIONS
Case 1
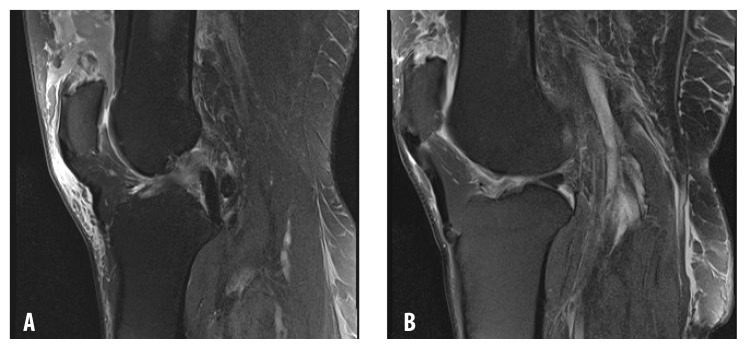
A 64-year-old man with a body mass index (BMI) of 41.8 kg/m2 (calculated from the patient’s weight just before surgery) presented with bilateral knee pain, effusion, and inability to perform a straight leg raise after sustaining a fall down the stairs 1 week earlier. He described an eccentric load that was placed on either knee during the fall. At the time of examination, he was unable to ambulate and had palpable gaps superior to the proximal pole of the patella. His Visual Analog Scale (VAS) score was 10 (on a 10-point scale). Routine radiographs were performed, which showed an effusion and osteoarthritic changes. A magnetic resonance image was obtained of each knee, which revealed full-thickness quadriceps tendon ruptures from the superior pole of the patella along with some degenerative intra-articular pathology (Figure 1).
Figure 1.
Case 1. Magnetic resonance image showing bilateral quadriceps tendon rupture (A. left knee and B. right knee).
The patient was counseled on his condition and given operative and nonoperative options of treatment. He elected to undergo bilateral quadriceps tendon repair. The surgical procedure, a suture anchor-based repair, was performed within 2 weeks of injury, as described in the Surgical Technique section after the case reports.
Postoperatively, the patient was placed in hinged knee braces and locked in extension for ambulation. Physical therapy started on postoperative day 2 to aid in recovery and strengthen his tendons. The patient was allowed to gradually increase his knee flexion in 30-degree increments every 2 weeks (Table 1).
Table 1.
Postoperative protocol after quadriceps tendon repair using suture anchors
| Time | Protocol |
|---|---|
| 0–6 wk | WBAT, with brace locked in extension at all times except therapy.
|
| 6–12 wk | Unlock brace for ambulation. Wean from brace as tolerated. May discontinue crutches when gait normalizes. Normalize ROM. Begin exercises such as minisquats, short-crank cycling, and weight shifting. |
| 3–6 mo | If gait is normal, begin WBAT without assistance. If ROM is normal, begin leg presses, running/jogging, agility exercises, and use of vertical climber fitness machine (VersaClimber, Heart Rate Inc, Santa Ana, CA). |
ROM = range of motion; WBAT = weight bearing as tolerated.
Six weeks postoperatively, the brace was unlocked for ambulation. At that time, the patient could ambulate without an assistive device, was able to achieve full knee extension with 5 of 5 quadriceps tendon strength, and had a VAS pain score of 2 of 10 (consistent with his baseline knee arthritis). By 3 months, he was allowed to discontinue wearing the brace. Now more than 2 years after surgery, the patient maintains an active lifestyle.
Case 2
A 43-year-old man presented with the chief complaint of bilateral knee pain after a fall while playing on a trampoline. During the fall, this patient sustained bilateral ankle fractures, which had previously undergone open reduction internal fixation at another health care facility. We examined the patient approximately 3 weeks after his injury. He walked with an antalgic gait, bilateral knee effusions were present, and he was unable to perform a straight leg raise. His medical history included hypertension and a BMI of 36.94 kg/m2 (calculated from the patient’s weight just before surgery).
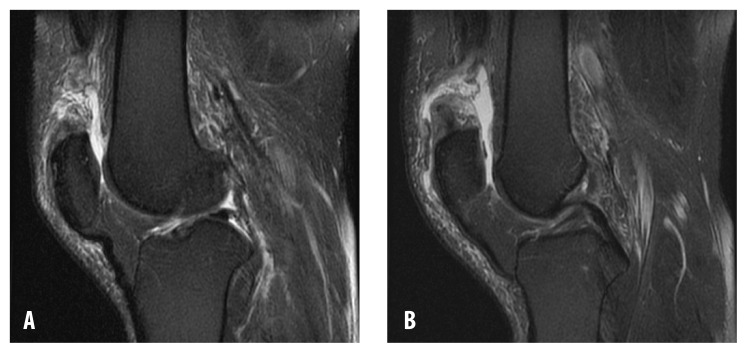
Magnetic resonance images were obtained of both knees. Results confirmed bilateral quadriceps tendon ruptures (Figure 2), which had not previously been found. When he came to our practice, there was documentation only of reported pain and swelling of the knee. After being counseled on his diagnosis and treatment options, the patient chose to undergo bilateral quadriceps tendon repair.
Figure 2.
Case 2. Magnetic resonance image showing bilateral quadriceps tendon rupture (A. left knee and B. right knee).
The surgery was performed as described in the Surgical Technique section. The patient followed the postoperative protocol described in Table 1.
At 8 weeks postoperatively, the patient had a VAS pain score of 0 of 10 and was able to perform bilateral straight leg raises without an extensor lag. Six months postoperatively, his flexion reached 120° bilaterally, and he was back to an active lifestyle. More than 1 year since surgery, he has had no knee complaints.
Case 3
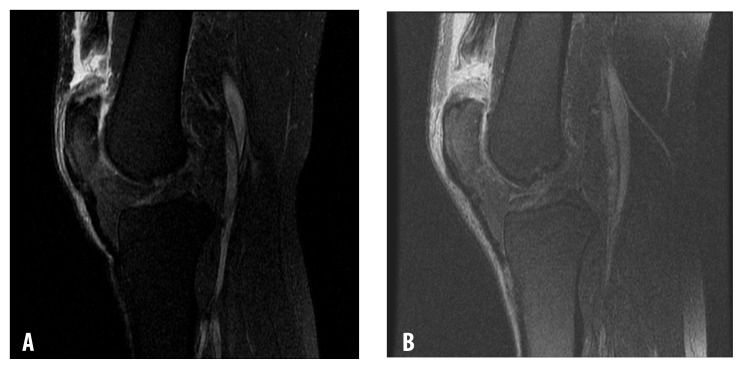
A 61-year-old man in a wheelchair came to our practice for evaluation of bilateral knee pain sustained in an injury 3 weeks earlier. Routine radiographs showed bilateral mild osteoarthritis and knee effusions. Results of magnetic resonance imaging confirmed bilateral quadriceps tendon ruptures (Figure 3). The patient’s medical history was remarkable for vitamin D deficiency, prostate cancer, and a BMI of 35.9 kg/m2 (calculated from the patient’s weight just before surgery). He was counseled on treatment options and ultimately chose to undergo quadriceps tendon repair.
Figure 3.
Case 3. Magnetic resonance image showing bilateral quadriceps tendon rupture (A. left knee and B. right knee).
The surgery was performed as described in the Surgical Technique section and was uneventful. The patient followed the postoperative protocol shown in Table 1.
By 6 months postoperatively, his tendon strength reached a plateau of a 5 of 5 on physical examination. His VAS pain score at final follow-up was 1 of 10. Now 1 year after surgery, the patient is back to full work duty. A timeline of all 3 cases appears in Table 2.
Table 2.
Timeline of cases
| Patient | Earliest recorded BMI | Ruptured tendons | Final outcome |
|---|---|---|---|
| 1 | 41.73 kg/m2 on 9/26/2005 | 2/05/2016 | Patient able to achieve full knee extension with 5/5 quadriceps tendon strength and had a VAS score of 2/10 (consistent with his baseline knee arthritis) |
| 2 | 35.63 kg/m2 on 2/22/2015 | 12/11/2017 | Patient reported a VAS pain scale of 0/10. He was able to perform the straight leg raise test |
| 3 | 35.37 kg/m2 on 10/06/2011 | 4/01/2017 | Patient reported a VAS pain scale of 1/10 and was back to working his full-time job |
BMI = body mass index; VAS = Visual Analog Scale.
SURGICAL TECHNIQUE
The same surgical technique was used on all 3 patients. In the preoperative holding area, the patient receives bilateral single-shot femoral blocks placed for regional anesthesia. The patient is brought to the operating room and placed supine on a well-padded operating table. General anesthesia is induced. Nonsterile tourniquets are placed on both thighs. The knee is cycled to be sure that the tourniquet is not constraining excursion of the quadriceps tendon. Both lower extremities are scrubbed and prepared in a standard fashion using chlorhexidine gluconate skin preparation (ChloraPrep, Becton, Dickinson and Company, Franklin Lakes, NJ).
A double drape is placed, and 1 knee is covered with an additional sterile drape while the opposite knee undergoes surgery. An Esmarch bandage is used to exsanguinate the lower extremity, and the tourniquet is inflated to 250 mmHg. A 6-cm to 8-cm midline incision is made sharply over the superior patella and quadriceps tendon. A Bovie cautery is used to dissect down to the defect, followed by evacuation of the hematoma. Blunt dissection frees up any adhesions. The superior pole of the patella and distal aspect of the quadriceps tendon are prepared using a curette and rongeur. Occasionally, a burr is used to aid in creating a bleeding surface along the superior border of the patella.
Two 2.8-mm, double-loaded, all-suture anchors (Q-FIX⋄, Smith and Nephew Inc, Cordova, TN) are placed in the superior pole of the patella (Figure 4). A modified Krackow suture configuration is placed into the quadriceps tendon with a single limb of each pair of sutures (Figure 5). The knee is placed in full extension, and the 4 pairs of sutures are sequentially tied, thus reducing the quadriceps tendon to the superior pole of the patella. The retinaculum is repaired using no. 2 or 5 nonabsorbable sutures with buried knots. The knee range of motion is checked and recorded. The knee goes through a last cycle of irrigation, and the wound is closed in layers.
Figure 4.
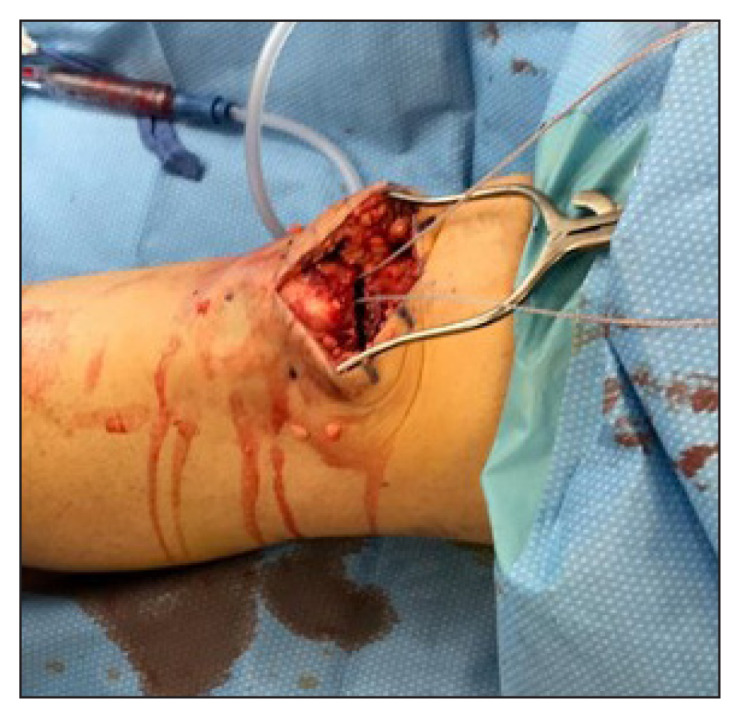
Double-loaded suture anchors in superior pole of patella.
Figure 5.
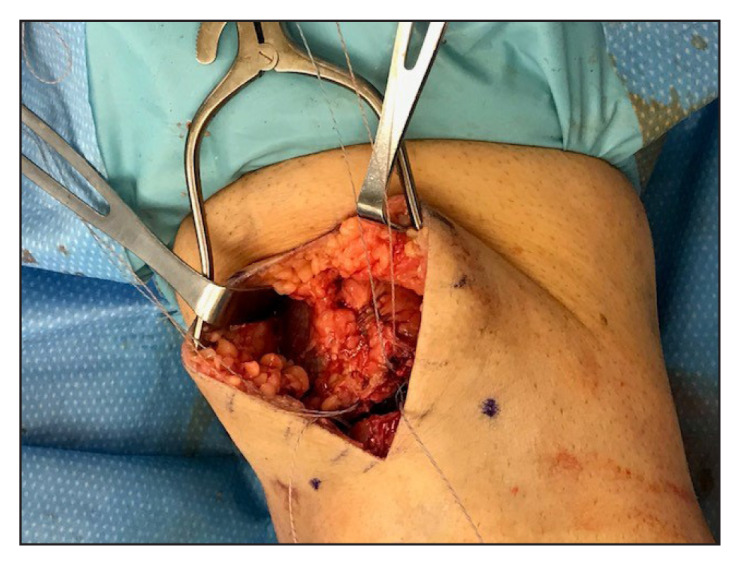
Krackow suture configuration.
The opposite knee is prepared again, and the procedure is repeated on that knee.
DISCUSSION
Knee extensor mechanism ruptures can occur either at the patellar tendon or quadriceps tendon. The literature suggests that disruption of the knee extensor mechanism in individuals over the age of 40 years typically involves the quadriceps tendon.7 In a review of 726 patients who experienced extensor mechanism injuries from 1986 to 2012, a total of 210 (28.9%) sustained quadriceps tendon ruptures. Their mean age was 61.0 years old (standard deviation = 13.1 years).2
A bilateral rupture of the quadriceps tendon is rare. There have been fewer than 100 reported cases of simultaneous bilateral quadriceps tendon ruptures in the US since 1949.8 Because of the rare occurrence of this injury, the initial diagnosis can be difficult for some physicians.9 A missed diagnosis is not uncommon and can lead to delays in patient care. A thorough history and physical examination, understanding of the mechanism of injury, knowledge of potential predisposing conditions, and imaging are critical tools to help make an accurate and timely diagnosis.10–12 Some diagnostic indicators of bilateral quadriceps tendon rupture include an inability to perform the straight leg raise test, palpation of a gap superior to the patella, and a limping or antalgic gait.
The literature on tendinopathies suggests multiple factors that increase the risk of injury to the tendon. These factors, whether they be intrinsic or extrinsic, are split into a mechanical theory and a vascular theory, signifying that they either effect the load or the perfusion of the tendon, putting it at risk of injury. Some of these factors include repetitive loading, excessive force, systemic diseases (ie, diabetes mellitus, systemic lupus erythematosus, renal failure, gout, thyroid disorders), and infection.13
Obesity has been linked to tendinopathies.14 Tendon overload combined with repetitive use can damage tendons. Tendon damage is described through a continuum in which the damage progresses from reactive tendinopathy to tendon disrepair and ultimately to degenerative tendinopathy. Once a tendon reaches the last stage of this continuum, cell death ensues, which puts the tendon at increased risk of rupture.15 Individuals with obesity tend to have an increase in adipocytes, which leads to a pro-inflammatory tendon environment. As adipocytes experience this inflammation, there is an increase in cell hypoxia, adipocyte cell death, and leptin production. These factors encourage the recruitment of macrophages, which secrete molecules such as interleukin 6 and tumor necrosis factor-α, thus promoting a proinflammatory state.16,17 The release of these cytokines triggers matrix metalloproteases, which work to further degrade tendon extracellular matrix.18 This tendon damage is often irreversible and predisposes tendons in obese individuals to rupture.
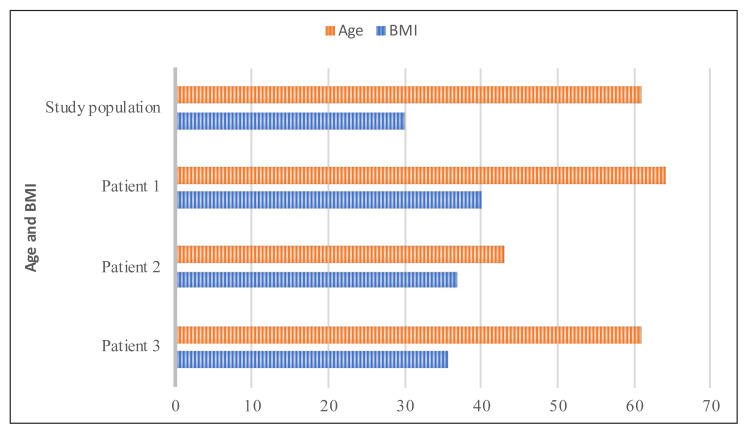
Neubauer et al6 noted a link between obesity and quadriceps tendon ruptures. In their study, 28 patients sustained bilateral quadriceps tendon ruptures, and the most frequently documented risk factor was obesity, with 6 (21.4%) of the patients being classified as obese. This finding is in agreement with what we have noted in our practice. In a review by Garner et al,2 210 patients with a quadriceps tendon rupture had an average BMI of 30.0 kg/m2 (standard deviation = 6.05 kg/m2). Findings of our case series are in line with the results of that study supporting the association between obesity and risk of quadriceps tendon ruptures (Figure 6).
Figure 6.
Comparison of age (years) and body mass index (BMI, kg/m2) of a study of 210 patients with quadriceps tendon rupture by Garner et al2 versus patients in this case report.
Quadriceps tendon repairs have historically been performed through a transosseous approach. This is traditionally done by drilling 3 transosseous holes through the patella, suturing the torn tendon in a modified Krackow fashion, passing the sutures through each hole, and tying the sutures over the inferior pole of the patella.19 New techniques have been described to repair the quadriceps tendon, including a suture anchor-based repair,20,21 the technique we chose to use.
In a biomechanics cadaver study by Sherman et al,20 the suture anchor-based repair of the quadriceps tendon was compared with the transosseous technique. The suture anchor-based construct had statistically significantly less gap formation at all forces tested in their study. Clinically, we have noted less incidence of extensor lag in patients with quadriceps tendon tears treated with a suture anchor-based repair as opposed to the transosseous approach. Although we have not formally compared both surgical techniques, we performed a transosseous technique for 5 years, and we observed more patients having an extensor lag 6 weeks postoperatively with the transosseous technique (unpublished data). Other noted benefits of a suture anchor-based approach include higher load to failure, reduced operative time, improved cosmesis, earlier initiation of range of motion and weight bearing, and less risk of penetration to the patellar articular cartilage.16,22–24
There are some contraindications as well as theoretical risks and complications with the use of our surgical approach. Some of the contraindications are as follows: Previous patellar fracture, previous knee replacement, and current infection. One surgical complication may occur while the surgeon is penetrating the cartilage; at that time, there is a theoretical threat of penetrating the patellar tendon, causing further injury. Another theoretical complication, fracturing of the patella, is possible in a patient with inadequate bone stock or osteoporosis. In our patients there were no issues with bone stock, and the tendon was easily reduced to the patella.
CONCLUSION
Bilateral quadriceps tendon ruptures are disabling injuries that are detrimental to the knee extensor mechanism. A timely repair, within 6 weeks of the tendon ruptures, is paramount. Our patients in this series all shared a comorbidity, obesity. When addressing bilateral quadriceps tendon ruptures in this patient population, we have found that a suture anchor-based construct allows for a secure repair, early initiation of physical therapy, and a noted improvement in the VAS pain scores.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications performed a primary substantive edit.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Tuong B, White J, Louis L, Cairns R, Andrews G, Forster BB. Get a kick out of this: The spectrum of knee extensor mechanism injuries. Br J Sports Med. 2011 Feb;45(2):140–6. doi: 10.1136/bjsm.2010.076695. [DOI] [PubMed] [Google Scholar]
- 2.Garner MR, Gausden E, Berkes MB, Nguyen JT, Lorich DG. Extensor mechanism injuries of the knee: Demographic characteristics and comorbidities from a review of 726 patient records. J Bone Joint Surg Am. 2015 Oct 7;97(19):1592–6. doi: 10.2106/JBJS.O.00113. [DOI] [PubMed] [Google Scholar]
- 3.Tendon pathophysiology. Physiopedia. Revised 2019 Feb 27 [originally cited 2018 Jul 27]. Available from: www.physio-pedia.com/index.php?title=Tendon_Pathophysiology&oldid=164409.
- 4.Surmi BK, Hasty AH. Macrophage infiltration into adipose tissue: Initiation, propagation and remodeling. Future Lipidol. 2008;3(5):545–56. doi: 10.2217/17460875.3.5.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abduljabbar FH, Aljurayyan A, Ghalimah B, Lincoln L. Bilateral simultaneous quadriceps tendon rupture in a 24-year-old obese patient: A case report and review of the literature. Case Rep Orthop. 2016;2016 doi: 10.1155/2016/4713137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neubauer T, Wagner M, Potschka T. Riedl M. Bilateral, simultaneous rupture of the quadriceps tendon: A diagnostic pitfall? Report of three cases and meta-analysis of the literature. Knee Surg Sports Traumatol Arthrosc. 2007 Jan 15;15(1):43–53. doi: 10.1007/s00167-006-0133-7. [DOI] [PubMed] [Google Scholar]
- 7.Rehabilitation guidelines for patellar tendon and quadriceps tendon repair [Internet] Madison, WI: University of Wisconsin Health Sports Medicine; updated 2018 Feb [cited 2018 Jun 18]. Available from: www.uwhealth.org/files/uwhealth/docs/pdf6/SM_pat_tendon_quad.pdf. [Google Scholar]
- 8.Neubauer T. Re: Simultaneous and spontaneous bilateral quadriceps tendons rupture. Am J Phys Med Rehabil. 2014 Jan;93(1):97–8. doi: 10.1097/PHM.0b013e318296e2d7. [DOI] [PubMed] [Google Scholar]
- 9.Kelly BM, Rao N, Louis SS, Kostes BT, Smith RM. Bilateral, simultaneous, spontaneous rupture of quadriceps tendons without trauma in an obese patient: A case report. Arch Phys Med Rehabil. 2001 Mar;82(3):415–8. doi: 10.1053/apmr.2001.19784. [DOI] [PubMed] [Google Scholar]
- 10.Ellanti P, Davarinos N, Morris S, Rice J. Bilateral synchronous rupture of the quadriceps tendon. Ir J Med Sci. 2012 Sep;181(3):423–5. doi: 10.1007/s11845-010-0596-x. [DOI] [PubMed] [Google Scholar]
- 11.Assiotis A, Pengas I, Vemulapalli K. Bilateral quadriceps tendon rupture in a seasoned marathon runner with patellar spurs. Grand Rounds. 2011;11(1):77–80. doi: 10.1102/1470-5206.2011.0020. [DOI] [Google Scholar]
- 12.Keogh P, Shanker S, Burke T, O’Connell R. Bilateral simultaneous rupture of the quadriceps tendons. Clin Orthop Relat Res. 1988 Sep;234:139–41. doi: 10.1097/PHM.0b013e318296e2d7. [DOI] [PubMed] [Google Scholar]
- 13.Riley G. The pathogenesis of tendinopathy. A molecular perspective. Rheumatology (Oxford) 2004 Feb;43(2):131–42. doi: 10.1093/rheumatology/keg448. [DOI] [PubMed] [Google Scholar]
- 14.Castro A, Skare TL, Nassif PAN, Sakuma AK, Barros WH. Tendinopathy and obesity. Arq Bras Cir Dig. 2016;29(Suppl 1):107–10. doi: 10.1590/0102-6720201600S10026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: What is its merit in clinical practice and research? Br J Sports Med. 2016 Oct;50(19):1187–91. doi: 10.1136/bjsports-2015-095422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Capiola D, Re L. Repair of patellar tendon rupture with suture anchors. Arthroscopy. 2007 Aug;23(8):906.e1–4. doi: 10.1016/j.arthro.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 17.Kumar V, Abbas AK, Aster JC, editors. Robbins and Cotran pathologic basis of disease. 9th ed. Philadelphia, PA: Saunders Elsevier; 2015. [Google Scholar]
- 18.Del Buono A, Oliva F, Osti L, Maffulli N. Metalloproteases and tendinopathy. Muscles Ligaments Tendons J. 2013 May 21;3(1):51–7. doi: 10.32098/mltj.01.2013.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Plesser S, Keilani M, Vekszler G, et al. Clinical outcomes after treatment of quadriceps tendon ruptures show equal results independent of suture anchor or transosseus repair technique used - A pilot study. PLoS One. 2018 Mar 19;13(3):e0194376. doi: 10.1371/journal.pone.0194376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sherman SL, Copeland ME, Milles JL, Flood DA, Pfeiffer FM. Biomechanical evaluation of suture anchor versus transosseous tunnel quadriceps tendon repair techniques. Arthroscopy. 2016 Jun;32(6):1117–24. doi: 10.1016/j.arthro.2015.11.038. [DOI] [PubMed] [Google Scholar]
- 21.Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: A biomechanical study. Am J Sports Med. 2006 Sep;34(9):1492–9. doi: 10.1177/0363546506287489. [DOI] [PubMed] [Google Scholar]
- 22.Amini MH. Quadriceps tendon repair using knotless anchors and suture tape. Arthrosc Tech. 2017 Sep 11;6(5):e1541–5. doi: 10.1016/j.eats.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richards DP, Barber FA. Repair of quadriceps tendon ruptures using suture anchors. Arthroscopy. 2002 May-Jun;18(5):556–9. doi: 10.1053/jars.2002.30729. [DOI] [PubMed] [Google Scholar]
- 24.Maniscalco P, Bertone C, Rivera F, Bocchi L. A new method of repair for quadriceps tendon ruptures. A case report. Panminerva Med. 2000 Sep;42(3):223–5. [PubMed] [Google Scholar]