Abstract
Background
There are increasing reports of corrosion between the femoral head and trunnion in primary conventional THA, resulting in metal particulate release often termed trunnionosis. There may be heightened awareness of this condition because of severe soft-tissue reactions initially thought to be solely attributable to prostheses with a metal-on-metal (MoM) bearing surface. It is unclear what percentage of revisions for THA with non-MoM bearing surfaces can be attributed to trunnionosis and to what extent adverse reaction to metal debris (ARMD) seen with MoM bearings may also be seen with other bearing surfaces in THA.
Questions/purposes
We analyzed data from a large national registry to ask: (1) What is the revision risk for the indication of ARMD in patients with conventional THA and modern non-MoM bearing surfaces such as metal or ceramic-on-cross-linked polyethylene (XLPE) or ceramic-on-ceramic? (2) What prosthesis factors are associated with an increased risk of such revision? (3) What is the relative revision risk for ARMD in THAs with large-head MoM bearings, small-head MoM bearings, and non-MoM modern bearing surfaces?
Methods
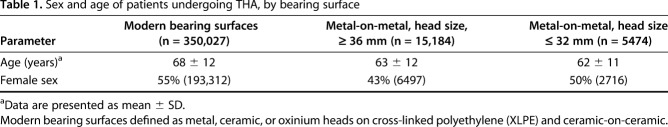
The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) longitudinally maintains data on all primary and revision joint arthroplasties, with nearly 100% capture. The study population included all THAs using modern bearing surfaces (defined as metal or ceramic heads-on-XLPE and ceramic-on-ceramic bearing couples) revised because of ARMD between September 1999 and December 2018. Prostheses with modular necks were excluded. The cumulative percent revision (CPR) because of ARMD was determined. The study group consisted of 350,027 THAs with a modern bearing surface, 15,184 THAs with a large-head MoM bearing (≥ 36 mm), and 5474 THAs with a small head MoM bearing (≤ 32 mm). The patients in the group who received the modern bearing surfaces were slightly older than the patients in the groups who received the large- and small-head bearing surfaces, with a mean age 68 years (SD 12) versus a mean age 63 years (SD 12), and a mean age 62 years (SD 11), respectively. There was a higher proportion of women in the modern bearing surface group; 55% (193,312 of 350,027), compared with 43% (6497 of 15,184) in the large-head MoM group and 50% (2716 of 5474) in the small-head MoM group. The outcome measure was the CPR, which was defined using Kaplan-Meier estimates of survivorship to describe the time to the first revision for ARMD at 17 years. Hazard ratios (HR) from Cox proportional hazards models, adjusting for age and sex, were performed to compare the revision rates among groups. The registry defines a revision as a reoperation of a previous hip arthroplasty in which one or more of the prosthetic components is replaced or removed, or one or more components is added.
Results
The CPR for ARMD for patients with a modern bearing surface at 17 years was 0.1% (95% confidence interval 0.0 to 0.1). After controlling for age and sex, we found that cobalt chrome heads, two specific prostheses (Accolade® I and M/L Taper), and head sizes ≥ 36 mm were associated with an increased risk of revision for ARMD. Metal-on-XLPE had a higher risk of revision for ARMD than ceramic-on-ceramic or ceramic-on-XLPE (HR 3.4 [95% CI 1.9 to 6.0]; p < 0.001). The Accolade 1 and the M/L Taper stems had a higher risk of revision than all other stems (HR, 8.3 [95% CI 4.7 to 14.7]; p < 0.001 and HR 14.4 [95% CI 6.0 to 34.6]; p < 0.001, respectively). Femoral stems with head sizes ≥ 36 mm had a higher rate of revision for ARMD than stems with head sizes ≤ 32 mm (HR 3.2 [95% CI 1.9 to 5.3]; p < 0.001).
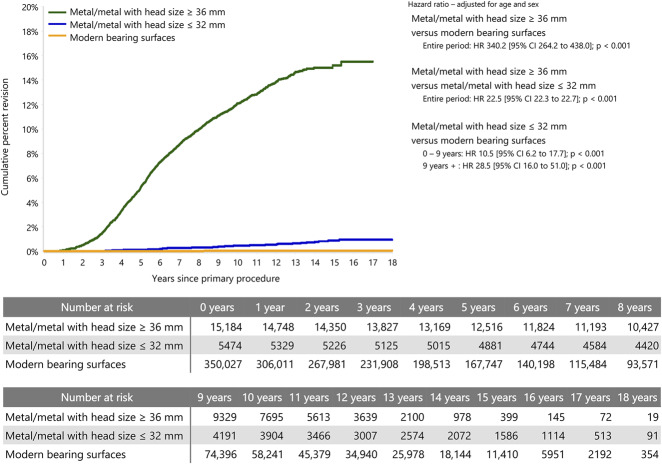
Large-head MoM bearings had a greater increase in revision for ARMD compared with modern bearing surfaces. The CPR for patients with a large-head MoM bearing at 17 years for ARMD was 15.5% (95% CI 14.5 to 16.6) and it was 0.1% for modern bearing surfaces (HR 340 [95% CI 264.2 to 438.0]; p < 0.001). Modern bearing surfaces likewise had a lower HR for revision for ARMD than did THAs with small-head MoM bearings, which had a 0.9% (95% CI 0.7 to 1.4) CPR compared with modern bearings from 0 to 9 years (HR 10.5 [95% CI 6.2 to 17.7]; p < 0.001).
Conclusions
The revision risk for ARMD with modern bearing surfaces in THA is low. The Accolade 1 and the M/L Taper stem have a higher risk of revision for ARMD and cobalt-chrome heads, and head sizes ≥ 36 mm have a higher rate of revision than ≤ 32 mm head sizes. ARMD is a rare failure mode for THA with non-MoM bearings, but in patients presenting with unexplained pain with no other obvious cause, this diagnosis should be considered and investigated further.
Level of Evidence
Level III, therapeutic study.
Introduction
The reintroduction and widespread acceptance of THA with metal-on-metal (MoM) bearing surfaces has led to higher-than-expected revision rates [3]. The reaction to metal particles results in soft-tissue damage, variously described as aseptic lymphocytic vasculitis-associated lesions [53], adverse local tissue reaction [16], pseudotumor [42], metal-related pathology [1] and adverse reaction to metal debris (ARMD) [27, 40]. Concerns about ARMD in THA were first raised in the 1970s, with regards to the McKee-Farrer hip, which was a monoblock stem [25]. More recently, studies have demonstrated higher rates of revision and higher serum levels of chrome and cobalt in conventional THA with large-head MoM bearings than with hip resurfacing arthroplasty, leading to the understanding that reactions to metal debris are not just confined to MoM bearing surfaces [5, 18]. Prostheses with a modular neck have two taper junctions that may contribute to the release of metal particles and have been reported to have a high rate of revision, regardless of the bearing surface used [23]. The idea that corrosion could occur at the head/neck taper of a THA prosthesis was first described shortly after the introduction of modularity for THA in the 1980s [33]. Modularity was rapidly adopted by the orthopaedic community. Recently, more attention has been directed to the taper or trunnion junction, with modular femoral heads as a source of metal particles. The pathologic process that releases metal ions at the taper junction has been described as mechanically assisted crevice corrosion, a combination of fretting and crevice corrosion. This produces soluble and particulate debris that may migrate locally or systemically [19, 22, 37].
There is, however, widespread variation in the reported revision incidence for ARMD with non-MoM bearings. This may be due to many of the published studies reporting small case series without knowledge of the denominator in the numbers reported. These studies come from institutions that may use a higher proportion of specific prostheses [4, 10, 21, 32, 34, 44, 46, 49, 50]. Irrespective of such case reports, considering the large number of THAs performed worldwide since the introduction of modular heads, the prevalence of revision for any metal-related cause is likely to be small. The National Joint Registry (NJR) for England, Wales, Northern Island, and the Isle of Man reported on 3340 revisions for ARMD with a revision risk of 0.032% in patients with non-MoM bearings compared with 3.7% in those with MoM bearings [35]. All types of bearings were included in this study, some of which now have little use. The aim of this study was therefore to further investigate ARMD as a cause of revision in a study population of primary THA performed with modern non-MoM bearing surfaces.
Using data from the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR), we sought to answer the following questions: (1) What is the revision risk for the indication of ARMD in patients with conventional THA and modern non-MoM bearing surfaces such as metal or ceramic-on-cross-linked polyethylene (XLPE) or ceramic-on-ceramic? (2) What prosthesis factors are associated with an increased risk of such revision? (3) What is the relative revision risk for ARMD in THAs with large-head MoM bearings, small-head MoM bearings, and non-MoM modern bearing surfaces?
Patients and Methods
The AOANJRR began data collection on September 1, 1999, with complete nationwide data collection commencing in 2002 for almost 100% of the arthroplasty procedures performed in Australia [3]. Registry data are validated against data provided by state and territory health departments in Australia with the use of a sequential multilevel matching process. A matching program is run monthly to search for all primary and revision arthroplasty procedures recorded in the registry that involve the same side and joint of the same patient, thus enabling each revision to be linked to the primary procedure. Data are also matched biannually with the Australian Government Department of Health and Ageing’s National Death Index to obtain information on the date of death. The registry cannot account for revision procedures performed on Australian emigrants, but for the population likely to undergo THA, this number is extremely small, and we believe it is unlikely to alter our results. The registry defines a revision as a reoperation of a previous hip arthroplasty in which one or more of the prosthetic components is replaced or removed, or one or more components is added. The registry does not record reoperations where a component was not added or removed.
The study population included all primary THAs for all diagnoses recorded by the registry up to December 31, 2018. This population included patients with osteoarthritis, femoral neck fractures, osteonecrosis, developmental dysplasia and rheumatoid arthritis, as well as a small number of other diagnoses. The primary aim of the study was to determine revision for ARMD with the use of modern bearing surfaces, which we defined as metal, ceramic, or oxinium head-on-XLPE and ceramic-on-ceramic. These bearing surfaces combined represent most of what is currently used in Australia (97% in 2018). We defined a number of exclusion criteria, so this study more accurately represents current surgical practice. Patients with non-highly cross-linked polyethylene were excluded because only 5.2% of patients have had this bearing couple in the past 10 years when polyethylene has been used [2]. We also could not be certain whether a diagnosis of ARMD might have been associated with catastrophic conventional polyethylene wear, with the potential for the femoral head to articulate with the acetabular shell to produce metal debris. Patients with a modular neck were excluded because they have a higher revision rate [23], are infrequently used currently [2] and have two taper junctions that may contribute to metal particle release. Ceramic-on-metal and metal-on-ceramic bearings have been used rarely in Australia and were not included in the study. We also performed a comparative analysis on patients who received a MoM bearing surface (small head, defined as ≤ 32 mm and large head defined as ≥ 36 mm) and underwent revision for the same diagnosis.
The registry records all reasons for revision. The common reasons are listed in a check box with available space for any other comments, and these reasons are recorded. We performed a search for all patients whose reason for revision recorded on their registry form included any of the following words: metal, metallosis, trunnion, taper, ALVAL (aseptic lymphocyte-dominated vasculitis-associated lesion), and pseudotumor. The acronym ARMD is not in widespread use in Australia. The registry has complete data on all prostheses revised because of ARMD. Prosthesis factors such as the type of stem and acetabular component, head size and composition and taper type, were extracted, along with patient age and sex, date of the primary procedure, and time to the first revision for ARMD. We also examined exactly what was performed at the time of the first revision.
The study group consisted of 350,027 THA procedures with a modern bearing surface, 15,184 patients with a large-head MoM bearing, and 5474 patients with a small head MoM bearing (Table 1). The group that received the modern bearing surfaces was slightly older than the groups that received the large- and small-head bearing surfaces; mean age 68 years (SD 12), versus mean age 63 years (SD 12), and mean age 62 years (SD 11), respectively. There was a higher proportion of women in the modern bearing surface group; 55% (193,312 of 350,027), compared with 43% (6497 of 15,184) in the large-head MoM and 50% (2716 of 5474) in the small-head MoM group (Table 1).
Table 1.
Sex and age of patients undergoing THA, by bearing surface
We censored eight patients with ceramic-on-ceramic bearings who had revisions for a number of causes, including dislocation and squeaking, where the words “metal stripe wear” had been written on the form. In a previous report, the authors felt this was not a true revision for ARMD [39].
Statistical Analysis
We used the cumulative percent revision (CPR), defined as the complement of the Kaplan-Meier estimates of survivorship, to describe the revision rate of an arthroplasty for ARMD. An accompanying 95% confidence interval was calculated using unadjusted pointwise Greenwood estimates. Patients were censored at the time of death, revision for reasons other than ARMD, or closure of the database at the end of the study period. Because the overall proportion of patients who died during the study period was sufficiently low, we used Kaplan-Meier estimates rather than competing risk estimates [7, 20]. We used hazard ratios from Cox proportional hazards models, adjusting for age and sex, to compare the revision rates among the three groups and, for the non MoM group, to compare the three most common femoral stems involved in revision for ARMD to all other stems, to compare revisions between cobalt-chrome and ceramic head sizes ≤ 32 mm and ≥ 36 mm, and femoral stem V40™ tapers and all others.
We checked the assumption of proportional hazards analytically for each model. If the interaction between the predictor and the log of time was statistically significant in the standard Cox model, we then performed estimates using a time-varying model. We iteratively chose points until the assumption of proportionality was met, and then we calculated the HRs for each selected period. All tests were two tailed at the 5% level of significance. The analysis was performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA).
For the comparative analysis, we compared the rates of revision until 17 years because this was the longest follow-up duration available with sufficient numbers of patients who underwent revision for the diagnosis of ARMD.
Results
There were 0.02% (63 of 350,027) of procedures with a primary THA and a modern bearing surface with a revision recorded for ARMD. The CPR for ARMD for patients with modern bearing surfaces at 17 years was 0.1% (95% CI 0.0 to 0.1). The mean time to revision for ARMD was 6 years (SD 3).
After controlling for age and sex, we found that cobalt chrome heads, two prostheses, the Accolade® I (Stryker, Fort Lauderdale, FL, USA) and M/L Taper (Zimmer Biomet, Warsaw, IN, USA) and head sizes ≥ 36 mm were associated with an increased risk of revision for ARMD.
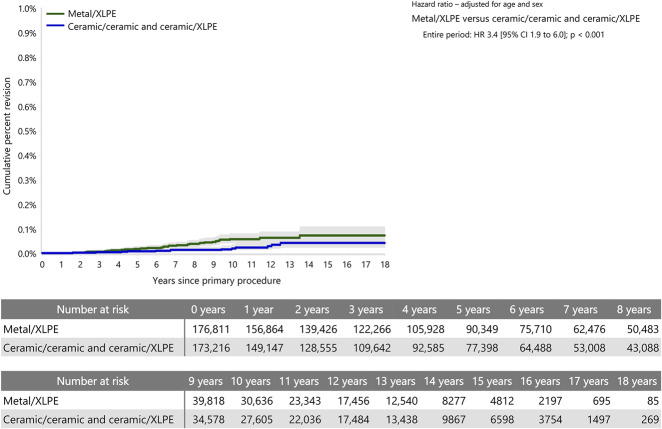
Of the 63 revisions which surgeons had recorded as being due to ARMD, 71% (45 of 63) had a cobalt-chrome head and 29% (18 of 63) had a ceramic head. Metal-on-XLPE had a higher risk of revision for ARMD than ceramic-on-ceramic or ceramic-on-XLPE (HR 3.4 [95% CI 1.9 to 6.0]; p < 0.001) (Fig. 1).
Fig. 1.
This graph shows the cumulative percent revision of primary conventional THA by metal/XLPE compared with ceramic/ceramic and ceramic/XLPE (all primary diagnoses, revision for ARMD).
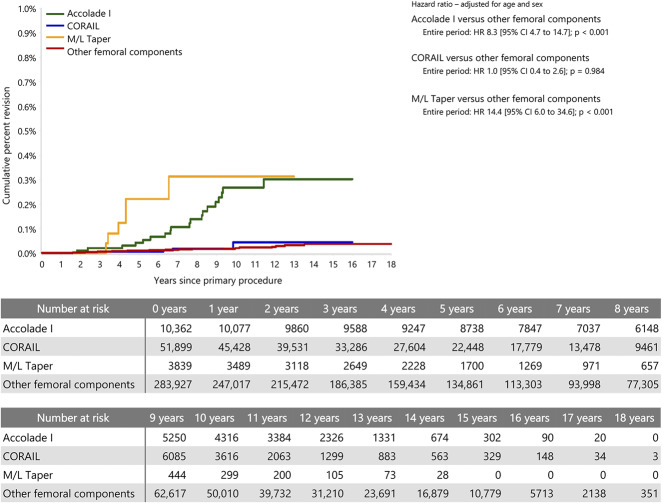
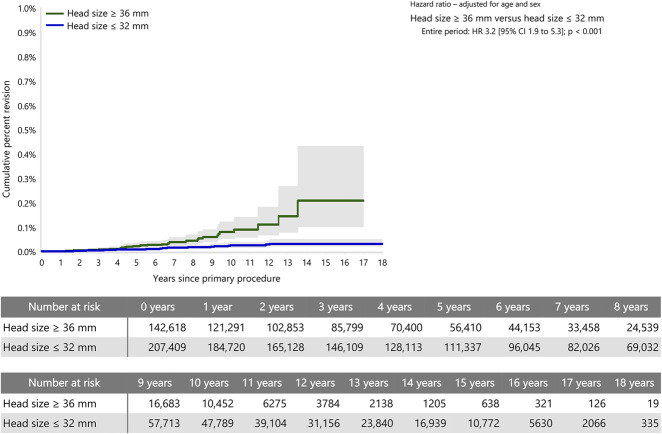
The stem/cup combination with the highest number of revisions for ARMD was the Accolade 1/Trident shell with a metal-on-XLPE bearing surface, which comprised 1.2% (4200 of 350,027) of all procedures in the study population. We performed a sub-analysis of the three stems most commonly involved in revisions for ARMD. The Accolade 1 stem comprised 30% (19 of 63) of revisions for ARMD, the M/L Taper 10% (six of 63), and the Corail® (DePuy, Leeds, UK) 8% (five of 63). With respect to the overall numbers of these procedures performed in Australia, the Accolade 1 stem had 0.2% (19 of 10,362) revised for ARMD, the M/L Taper had 0.2% (six of 3839), and the Corail had 0.01% (five of 51,899). The CPR for ARMD of the Accolade 1 stem and the M/L Taper stem at 13 years was 0.3% (95% CI 0.2 to 0.5) and (95% CI 0.1 to 0.7), respectively, and for the Corail stem it was 0.0% (95% CI 0.0 to 0.1). Both the Accolade 1 and the M/L Taper stem had a higher risk of revision than all other stems (HR 8.3 [95% CI 4.7 to 14.7]; p < 0.001 and HR 14.4 [95% CI 6.0 to 34.6]; p < 0.001, respectively), but the Corail did not have a greater risk of revision (Fig. 2). The V40™ taper (Stryker, Fort Lauderdale, FL, USA) was involved in 40% (25 of 63) of revisions in this study but there was no difference in the risk of revision of the V40 taper compared with all other tapers (HR 0.7 [95% CI 0.4 to 1.1]; p = 0.113. Femoral stems with a head size ≥ 36 mm comprised 41% (142,618 of 350,027) of the study population and 59% (207,409 of 350,027) had a head size of ≤ 32 mm. Femoral stems with a head size ≥ 36 mm had a higher rate of revision for ARMD than stems with a head size ≤ 32 mm (HR 3.2 [95% CI 1.9 to 5.3]; p < 0.001) (Fig. 3).
Fig. 2.
This graph shows the cumulative percent revision of primary conventional THA by the three most common femoral components compared with all others (all primary diagnoses, revision for ARMD).
Fig. 3.
This graph shows the cumulative percent revision of primary conventional THA for head sizes ≤ 32 mm and ≥ 36 mm (all primary diagnoses, revision for ARMD).
Large-head MoM bearings were associated with a larger increase in revision for ARMD compared with modern bearing surfaces. The CPR for ARMD for patients with a large-head MoM bearing at 17 years was 15.5% (95% CI 14.5 to 16.6), which was greater than that seen in THAs with modern bearing surfaces (HR 340.2 [95% CI 264.2 to 438.0]; p < 0.001). Modern bearing surfaces likewise had a lower HR for revision for ARMD than did THAs with small-head MoM bearings, which had a 0.9% (95% CI 0.7 to 1.4) CPR compared with modern bearings from 0 to 9 years (HR 10.5 [95% CI 6.2 to 17.7]; p < 0.001) and from 9 to 17 years (HR 28.5 [95% CI 15.9 to 51.0]; p < 0.001) (Fig. 4).
Fig. 4.
This graph shows the cumulative percent revision of primary conventional THA by bearing surface (all primary diagnoses, revision for ARMD).
Discussion
Surgeons currently have the option of several bearing surfaces for use with primary THA, apart from large-head MoM, which has been removed from the market place due to high revision rates [54]. Although there are increasing reports of ARMD associated with primary THA with non-MoM bearings, these findings have provided imprecise estimates of the actual risk [11, 44, 50]. We sought to identify the revision risk in a national population undergoing THA with modern bearing surfaces and found that it was very low. There are also certain prosthetic factors that are associated with a higher risk of revision for ARMD. These include cobalt-chrome heads, head sizes ≥ 36 mm and the use of the Accolade 1 and M/L Taper prostheses. We also demonstrated that primary THA with both large- and small-head MoM bearing surfaces had a larger risk of revision for ARMD compared with THA with modern bearing surfaces.
There are several limitations to this study. We specifically addressed the issue of revisions for ARMD only in patients who had THA with modern bearing surfaces and only those with femoral stem/head modularity. Procedures using either non-XLPE, zirconia, or alumina ceramics were excluded, as were THAs using modular necks, since the focus of the analysis was to report on contemporary practice. In Australia, the use of non-XLPE, zirconia, and alumina has almost ceased, and the use of modular neck prostheses remains very limited. In addition, the AOANJRR has previously reported on a higher risk of revision of modular neck prostheses [23].
The registry only records revision of procedures, and there may be patients who are symptomatic but have not had a revision procedure for a variety of reasons. Reactions to metal debris may also present as other possible causes of revision such as aseptic loosening, osteolysis, or even sepsis with fluid and necrosis in the periprosthetic joint tissues but no evidence of bacterial growth. Surgeons may have been unaware of the presentation of ARMD, especially early in the study period, and we believe that our data may thus underestimate the true incidence during the 17-year period. However, from 2009 onwards, “trunnionosis” or “metal related pathology” has been clearly written as the first diagnosis on most forms suggesting that surgeons are now more aware of the diagnosis. Although our study may be a conservative estimate of the true revision for ARMD, we believe that revisions for ARMD are still likely to be low.
The registry also does not record radiographic information that may influence the presentation of ARMD, as has been noted with large-head MoM THAs [8, 11]. However, a study by Whitehouse et al. [52] did not demonstrate abnormal prostheses orientation on pre-revision radiographs in patients who underwent a revision procedure for ARMD with metal-on-polyethylene bearings. The registry also did not record patient height and weight until 2015, so we do not have enough data to include in the analysis to determine if weight had an effect [14, 36]. Although it is known that increased BMI is associated with an increased risk of reoperation and revision, this is largely due to infection [41, 45]. Inadequate drying of the taper at the time of femoral head placement and incorrect insertion have also been suggested as factors that may lead to ARMD [30, 43], but it is not possible to assess the impact of these factors using registry data. Finally, the registry also does not have access to pathology and histology reports or any metal ion levels taken at the time of revision to confirm the diagnosis, so this was based on surgeons’ observations at the time of revision [6, 51].
Our study, with longer follow-up, found a slightly lower percentage of revisions for non-MoM bearings than in a report by Matharu et al. [35] using data from the NJR (0.032%). We reported on modern bearing surfaces only and this may explain the lower percentage of all revisions for ARMD in patients with non-MoM bearing surfaces in our study than in the NJR (4% compared with 8%), as their study included all non-MoM bearing surfaces [35]. The implantation time for revision for ARMD in non-MoM hips recorded in the NJR was a mean of 4 years (SD 3). This was slightly shorter than our mean time of 6 years (SD 3) and may be as a result of greater postoperative surveillance and earlier diagnosis. The percentage of revisions, which was between 1% and 3%, was lower than what has been reported in systematic reviews [6, 17, 48]. These systematic reviews relied mainly on reports from single institutions of the incidence of revision and, therefore, are subject to the implants that were used. This may not reflect broad community use but implant-specific problems or the use of certain implants at a hospital level.
After controlling for age and sex, we found that two types of femoral stems (the Accolade 1 and the M/L Taper), cobalt-chrome heads, and larger head sizes had a higher revision risk. Our findings are in accordance with many of the case series published [4, 9, 32, 34, 44, 46, 50] with the Accolade 1 being the most commonly reported stem involved in revisions for ARMD in both case series and in our registry. The Accolade 1, which is made of titanium-molybdenum-zirconium-iron (TMZF) alloy [9, 22, 46] has been demonstrated in mechanical studies to have a higher flexural rigidity than other materials and this may contribute to ARMD. Specific prostheses were not listed in the study from the NJR [35].
Cobalt-chrome heads had a higher revision rate than ceramic heads and mixed metal combinations are more susceptible to taper corrosion [6]. This is generally in the form of mechanically-assisted crevice corrosion, which results in material loss from both the trunnion and the femoral taper [24]. We also recorded several ARMD revisions in ceramic-on-ceramic bearing surfaces, especially those with larger heads. Although fretting can occur with ceramic-on-titanium trunnions, the volumetric material loss is an order of magnitude less than with cobalt-chrome femoral heads. Kurtz et al. [26] have suggested that using ceramic heads can reduce, but not eliminate, fretting from modular THA head/stem junctions. Although there is no cobalt-chrome in ceramic heads, metal wear could be derived from titanium or stainless steel debris as a result of impingement between the stem and acetabular rim [47].
We reported a higher revision risk for ARMD for both metal and ceramic large femoral heads (≥ 36 mm). Larger head sizes place greater stresses on the head-trunnion interface [31] and may cause more corrosion [15]. Larger heads were also shown to have a higher revision for ARMD than those ≤ 32 mm in metal-on-polyethylene bearings in the NJR [35].
The V40 taper was the most common taper involved, but this was used with the Accolade 1 stem and was not found to be a risk factor in and of itself. The V40 taper is most commonly used in Australia with the Exeter cemented stem and it is likely that the combination of the V40 Taper and the TMZF material in the Accolade 1 contributes to the increased revision for ARMD. However, a trend toward shorter trunnions has been associated with an increase in taper junction failure in larger-diameter MoM bearings [28]. Although a detailed discussion of all the mechanisms associated with ARMD is beyond the scope of this study, there are multiple reviews on this subject [6, 13, 38, 51] and our registry findings correlate with these clinical, retrieval, and bioengineering studies.
This study also demonstrated a substantially higher rate of revision for ARMD with large and small-head MoM bearings compared with non-MoM modern bearing surfaces. This has been previously reported for overall revisions [12]. This clinical outcome is consistent with a prior report of a retrieval study of femoral heads with metal-on-polyethylene articulations, which demonstrated five times less trunnion wear than MoM articulations for femoral stems with a 12/14 taper manufactured by the same company [29].
Conclusions
The risk of revision for ARMD with the use of modern bearing surfaces in THA is quite low and surgeons can reassure their patients in this regard. The Accolade 1 and the M/L Taper stems have a higher revision risk for ARMD and cobalt-chrome heads and head sizes ≥ 36 mm have a higher rate of revision than ≤ 32 mm head sizes. Even though ARMD is a rare failure mode for THA with modern non-MoM bearings, surgeons should consider this mechanism in patients presenting with unexplained pain and investigate further.
Acknowledgments
We thank the Australian Orthopaedic Association National Joint Replacement Registry and the hospitals, orthopaedic surgeons, and patients whose data made this work possible.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Australian Orthopaedic Association National Joint Replacement Registry, based at the South Australian Health and Medical Research Institute, Adelaide, South Australia.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2013. 2013. AOA; Available at: https://aoanjrr.sahmri.com/annual-reports-2013. Accessed February 5, 2020. [Google Scholar]
- 2.Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee and Shoulder Arthroplasty: Annual Report 2018. 2018. Adelaide, Australia, AOA; Available at: https://aoanjrr.sahmri.com/annual-reports-2018. Accessed February 5, 2020. [Google Scholar]
- 3.Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee and Shoulder Arthroplasty: Annual Report 2019. 2019. Adelaide, Australia, AOA; Available at: https://aoanjrr.sahmri.com/annual-reports-2019. Accessed February 5, 2020. [Google Scholar]
- 4.Banerjee S, Cherian JJ, Bono JV, Kurtz SM, Geesink R, Meneghini RM, Delanois RE, Mont MA. Gross trunnion failure after primary total hip arthroplasty. J Arthroplasty. 2015;30:641-648. [DOI] [PubMed] [Google Scholar]
- 5.Beaule PE, Kim PR, Hamdi A, Fazekas A. A prospective metal ion study of large-head metal-on-metal bearing: a matched-pair analysis of hip resurfacing versus total hip replacement. Orthop Clin North Am. 2011;42:251-257. [DOI] [PubMed] [Google Scholar]
- 6.Berstock JR, Whitehouse MR, Duncan CP. Trunnion corrosion: what surgeons need to know in 2018. Bone Joint J. 2018;100:44-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biau DJ, Latouche A, Porcher R. Competing events influence estimated survival probability: when is Kaplan-Meier analysis appropriate? Clin Orthop Relat Res. 2007;462:229-233. [DOI] [PubMed] [Google Scholar]
- 8.Bolland BJ, Culliford DJ, Langton DJ, Millington JP, Arden NK, Latham JM. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg Br. 2011;93:608-615. [DOI] [PubMed] [Google Scholar]
- 9.Cook RB, Bolland BJ, Wharton JA, Tilley S, Latham JM, Wood RJ. Pseudotumour formation due to tribocorrosion at the taper interface of large diameter metal on polymer modular total hip replacements. J Arthroplasty. 2013;28:1430-1436. [DOI] [PubMed] [Google Scholar]
- 10.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655-1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291-1297. [DOI] [PubMed] [Google Scholar]
- 12.de Steiger R, Peng A, Lewis P, Graves S. What Is the Long-term Survival for Primary THA With Small-head Metal-on-metal Bearings? Clin Orthop Relat Res. 2018;476:1231-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Del Balso C, Teeter MG, Tan SC, Lanting BA, Howard JL. Taperosis: Does head length affect fretting and corrosion in total hip arthroplasty? Bone Joint J. 2015;97:911-916. [DOI] [PubMed] [Google Scholar]
- 14.Donaldson FE, Coburn JC, Siegel KL. Total hip arthroplasty head-neck contact mechanics: a stochastic investigation of key parameters. J Biomech. 2014;47:1634-1641. [DOI] [PubMed] [Google Scholar]
- 15.Dyrkacz RM, Brandt JM, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty. 2013;28:1036-1040. [DOI] [PubMed] [Google Scholar]
- 16.Engh CA, Jr., Ho H, Engh CA. Metal-on-metal hip arthroplasty: does early clinical outcome justify the chance of an adverse local tissue reaction? Clin Orthop Relat Res. 2010;468:406-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Esposito CI, Wright TM, Goodman SB, Berry DJ, Clinical B, Bioengineering Study Groups from Carl TBW. What is the trouble with trunnions? Clin Orthop Relat Res. 2014;472:3652-3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award: Metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2010;468:318-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res. 1993;27:1533-1544. [DOI] [PubMed] [Google Scholar]
- 20.Gillam MH, Ryan P, Graves SE, Miller LN, de Steiger RN, Salter A. Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry. Acta Orthop. 2010;81:548-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gkagkalis G, Mettraux P, Omoumi P, Mischler S, Rudiger HA. Adverse tissue reaction to corrosion at the neck-stem junction after modular primary total hip arthroplasty. Orthop Traumatol Surg Res. 2015;101:123-126. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, Leurgans S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002:149-161. [DOI] [PubMed] [Google Scholar]
- 23.Graves SE, de Steiger R, Davidson D, Donnelly W, Rainbird S, Lorimer MF, Cashman KS, Vial RJ. The use of femoral stems with exchangeable necks in primary total hip arthroplasty increases the rate of revision. Bone Joint J. 2017;99:766-773. [DOI] [PubMed] [Google Scholar]
- 24.Hussey DK, McGrory BJ. Ten-Year Cross-Sectional Study of Mechanically Assisted Crevice Corrosion in 1352 Consecutive Patients With Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty. 2017;32:2546-2551. [DOI] [PubMed] [Google Scholar]
- 25.Jones DA, Lucas HK, O'Driscoll M, Price CH, Wibberley B. Cobalt toxicity after McKee hip arthroplasty. J Bone Joint Surg Br. 1975;57:289-296. [PubMed] [Google Scholar]
- 26.Kurtz SM, Kocagoz SB, Hanzlik JA, Underwood RJ, Gilbert JL, MacDonald DW, Lee GC, Mont MA, Kraay MJ, Klein GR, Parvizi J, Rimnac CM. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471:3270-3282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg Br. 2010;92:38-46. [DOI] [PubMed] [Google Scholar]
- 28.Langton DJ, Sidaginamale R, Lord JK, Nargol AV, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res. 2012;1:56-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lanting BA, Teeter MG, Howard JL, MacDonald SJ, Van Citters DW. Metal-on-Metal Compared With Metal-on-Polyethylene: The Effect on Trunnion Corrosion in Total Hip Arthroplasty. J Arthroplasty. 2017;32:2574-2579. [DOI] [PubMed] [Google Scholar]
- 30.Lavernia CJ, Baerga L, Barrack RL, Tozakoglou E, Cook SD, Lata L, Rossi MD. The effects of blood and fat on Morse taper disassembly forces. Am J Orthop (Belle Mead NJ). 2009;38:187-190. [PubMed] [Google Scholar]
- 31.Lavernia CJ, Iacobelli DA, Villa JM, Jones K, Gonzalez JL, Jones WK. Trunnion-Head Stresses in THA: Are Big Heads Trouble? J Arthroplasty. 2015;30:1085-1088. [DOI] [PubMed] [Google Scholar]
- 32.JU Lindgren, Brismar BH, Wikstrom AC. Adverse reaction to metal release from a modular metal-on-polyethylene hip prosthesis. J Bone Joint Surg Br. 2011;93:1427-1430. [DOI] [PubMed] [Google Scholar]
- 33.Lucas LC, Buchanan RA, Lemons JE. Investigations on the galvanic corrosion of multialloy total hip prostheses. J Biomed Mater Res. 1981;15:731-747. [DOI] [PubMed] [Google Scholar]
- 34.Mao X, Tay GH, Godbolt DB, Crawford RW. Pseudotumor in a well-fixed metal-on-polyethylene uncemented hip arthroplasty. J Arthroplasty. 2012;27:493 e413-497. [DOI] [PubMed] [Google Scholar]
- 35.Matharu GS, Pandit HG, Murray DW, Judge A. Adverse reactions to metal debris occur with all types of hip replacement not just metal-on-metal hips: a retrospective observational study of 3340 revisions for adverse reactions to metal debris from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. BMC Musculoskelet Disord. 2016;17:495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matsen Ko L, Chen AF, Deirmengian GK, Hozack WJ, Sharkey PF. Catastrophic Femoral Head-Stem Trunnion Dissociation Secondary to Corrosion. J Bone Joint Surg Am. 2016;98:1400-1404. [DOI] [PubMed] [Google Scholar]
- 37.Matusiewicz H. Potential release of in vivo trace metals from metallic medical implants in the human body: from ions to nanoparticles--a systematic analytical review. Acta Biomater. 2014;10:2379-2403. [DOI] [PubMed] [Google Scholar]
- 38.Mistry JB, Chughtai M, Elmallah RK, Diedrich A, Le S, Thomas M, Mont MA. Trunnionosis in total hip arthroplasty: a review. J Orthop Traumatol. 2016;17:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Molloy DO, Munir S, Jack CM, Cross MB, Walter WL, Walter WK, Sr Fretting and corrosion in modular-neck total hip arthroplasty femoral stems. J Bone Joint Surg Am. 2014;96:488-493. [DOI] [PubMed] [Google Scholar]
- 40.National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 6th Annual Report 2009. 2009. Hemel Hempstead, NJR: Available at: http://www.njrcentre.org.uk/njrcentre/Portals/0/Sixth%20annual%20NJR%20report.pdf. Accessed February 5, 2020. [Google Scholar]
- 41.Onggo JR, Onggo JD, de Steiger R, Hau R. Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: a meta-analysis and systematic review. Osteoarthritis Cartilage. 2020;28:31-44. [DOI] [PubMed] [Google Scholar]
- 42.Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847-851. [DOI] [PubMed] [Google Scholar]
- 43.Pennock AT, Schmidt AH, Bourgeault CA. Morse-type tapers: factors that may influence taper strength during total hip arthroplasty. J Arthroplasty. 2002;17:773-778. [DOI] [PubMed] [Google Scholar]
- 44.Raju S, Chinnakkannu K, Puttaswamy MK, Phillips MJ. Trunnion Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty: A Case Series. J Am Acad Orthop Surg. 2017;25:133-139. [DOI] [PubMed] [Google Scholar]
- 45.Sayed-Noor AS, Mukka S, Mohaddes M, Karrholm J, Rolfson O. Body mass index is associated with risk of reoperation and revision after primary total hip arthroplasty: a study of the Swedish Hip Arthroplasty Register including 83,146 patients. Acta Orthop. 2019;90:220-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shamshoon S, Thornley P, de Beer J. Profound Trunnion Wear Resulting in Femoral Head-Neck Dissociation in Total Hip Arthroplasty. Case Rep Orthop. 2018;2018:1534572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steinhoff A, Hakim V, Walker RH, Colwell CW, Jr., Copp SN. Ceramic liner fracture and impingement in total hip arthroplasty. HSS J. 2015;11:50-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sultan AA, Cantrell WA, Khlopas A, Berger RJ, Sodhi N, Molloy RM, Krebs VE, Mont MA. Evidence-Based Management of Trunnionosis in Metal-on-Polyethylene Total Hip Arthroplasty: A Systematic Review. J Arthroplasty. 2018;33:3343-3353. [DOI] [PubMed] [Google Scholar]
- 49.Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J Bone Joint Surg Am. 1988;70:1238-1242. [PubMed] [Google Scholar]
- 50.Urish KL, Hamlin BR, Plakseychuk AY, Levison TJ, Higgs GB, Kurtz SM, DiGioia AM. Trunnion Failure of the Recalled Low Friction Ion Treatment Cobalt Chromium Alloy Femoral Head. J Arthroplasty. 2017;32:2857-2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weiser MC, Lavernia CJ. Trunnionosis in Total Hip Arthroplasty. J Bone Joint Surg Am. 2017;99:1489-1501. [DOI] [PubMed] [Google Scholar]
- 52.Whitehouse MR, Endo M, Zachara S, Nielsen TO, Greidanus NV, Masri BA, Garbuz DS, Duncan CP. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J. 2015;97-B:1024-1030. [DOI] [PubMed] [Google Scholar]
- 53.Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28-36. [DOI] [PubMed] [Google Scholar]
- 54.Zagra L, Gallazzi E. Bearing surfaces in primary total hip arthroplasty. EFORT Open Rev. 2018;3:217-224. [DOI] [PMC free article] [PubMed] [Google Scholar]