Abstract
Background
In kinematic alignment in TKA, the aim is to match the implant’s position to the pre-arthritic anatomy of an individual patient, in contrast to the traditional goal of neutral mechanical alignment. However, there are limited mid-term, comparative data for survivorship and functional outcomes for these two techniques.
Questions/purposes
In the setting of a randomized, controlled trial at 5 years, is there a difference between kinematic alignment and mechanical alignment in TKA in terms of (1) patient-reported outcome measures, (2) survivorship free from revision or reoperation, and (3) the incidence of radiographic aseptic loosening?
Methods
In the initial study, 99 primary TKAs for osteoarthritis were randomized to either the mechanical alignment (n = 50) or kinematic alignment (n = 49) group. Computer navigation was used in the mechanical alignment group, and patient-specific cutting blocks were used in the kinematic alignment group. At 5 years, 95% (48 of 50) of mechanical alignment and 96% (47 of 49) of kinematic alignment TKAs were available for follow-up. Knee function was assessed using the Knee Society Score (KSS), VAS, Oxford Knee Score (OKS), WOMAC, Forgotten Joint Score (FJS) and EuroQol 5D. Survivorship free from reoperation (any reason) and revision (change or addition of any component) was determined via Kaplan-Meier analysis. Radiographs were assessed for signs of aseptic loosening (as defined by the presence of progressive radiolucent lines in two or more zones) by a single blinded observer.
Results
At 5 years, there were no differences in any patient-reported outcome measure between the two groups. For example, the mean OKS did not differ between the two groups (kinematic alignment: 41.4 ± 7.2 versus mechanical alignment: 41.7 ± 6.3; difference -0.3 [95% confidence interval - 3.2 to 2.5]; p = 0.99). At 5 years, survivorship free from reoperation was 92.2 (95% CI 80.4 to 97.0) for mechanical alignment and 89.7 (95% CI 77.0 to 95.6) for kinematic alignment (log rank test; p = 0.674), survivorship free from revision was 94.1 (95% CI 82.9 to 98.1) for mechanical alignment and 95.9 (95% CI 84.5 to 99.0) for kinematic alignment (log rank test; p = 0.681). At 5 years, one patient demonstrated radiographic aseptic loosening for the mechanical alignment group; no cases were identified for the kinematic alignment group.
Conclusions
We found no mid-term functional or radiographic differences between TKAs with mechanical alignment or kinematic alignment. The anticipated improvements in patient-reported outcomes with kinematic alignment were not realized. Because kinematic alignment results in a high proportion of patients whose tibial components are inserted in varus, loosening remains a potential long-term concern. Given the unknown impact on long-term survivorship of the substantial alignment alterations with kinematic alignment, our findings do not support the routine use of kinematic alignment outside of a research setting.
Level of Evidence
Level I, therapeutic study.
Introduction
Mechanical alignment in TKA aims to position femoral and tibial components perpendicular to the mechanical axis of each bone, aligning the hip-knee-ankle angle of the limb to neutral under static weightbearing conditions. Conventional TKA instrumentation is based around this principle, and computer navigation was introduced to aid accuracy in achieving the goal of a neutral mechanical axis. However, this situation differs from the native knee, in which the articular surface of the tibia averages 3° varus and that of the femur 2° to 3° of valgus relative to the mechanical axis [2]. Additionally, there is wide individual variation in limb alignment. If patients with variants of alignment undergo TKA using mechanical alignment principles, medial soft tissue releases are likely to be required. In contrast, the kinematic alignment technique attempts to match the implant position to recreate the anatomy of the pre-arthritic articular surface for the individual patient.
Currently, there is debate over the relative merits of kinematic alignment versus mechanical alignment in TKA. Dissatisfaction after mechanical alignment in TKA remains between 10% and 20%, with residual symptoms reported in 33% to 54% of patients [4, 24]. Advocates of kinematic alignment suggest a more individualized “kinematic” alignment will offer advantages over the mechanical alignment technique in terms of pain and function. However, there is concern that kinematic alignment may align the components in outlier categories, thereby increasing the risk of loosening or failure [18]. Although many surgeons see kinematic alignment as having potential to improve patient outcomes, early published results of randomized controlled trials (RCTs) comparing kinematic alignment with mechanical alignment in TKA have been mixed [28]. We previously published the 2-year results of an RCT [29] showing no difference in clinical or radiologic outcomes between kinematic alignment and mechanical alignment. Likewise, a meta-analysis in which raw data were combined was unable to definitely establish a benefit of kinematic alignment compared with mechanical alignment in TKA, nor was it able to recommend specific patients who may be more likely to benefit from kinematic alignment [28].
Although kinematic alignment appears to demonstrate early functional results comparable to mechanical alignment, the long-term function and survivorship of kinematic alignment remains unknown. We, therefore, asked the following, using our previous patient groups: Is there a difference between kinematic alignment and mechanical alignment in TKA at 5 years follow-up in terms of (1) patient-reported outcome measures, (2) survivorship free from revision or reoperation, and (3) the incidence of radiographic “aseptic” loosening?
Patients and Methods
This RCT presents follow-up on our published 2-year study in which the detailed methodology was described previously [29]. The extension to 5-year follow-up was approved by the national ethical review board, and the trial and protocol were reported in the ClinicalTrials.Gov register (Identifier: NCT02527148).
In the initial study [29] a research nurse enrolled 110 patients (114 TKAs) between August 2011 and August 2013. Computer-generated randomization to the kinematic alignment group (n = 57) or mechanical alignment group (n = 57) was performed with numbered, opaque, sealed envelopes. Eight patients in the kinematic alignment group and seven patients in the mechanical alignment group did not receive their allocated intervention, and 49 patients in the kinematic alignment group and 50 in the mechanical alignment group were available for postoperative follow-up. The sample size was set at a minimum of 45 patients per treatment arm based on a 5-point improvement in the mean Oxford Knee Score (OKS; the previously reported minimum clinically significant difference for the OKS in TKA), 80% power, a significance level of 5% and accounting for 10% loss of follow up [29]. At 5 years, we achieved excellent follow-up with reference to the original power. Only two patients in the kinematic alignment group had withdrawn, while in the mechanical alignment group, one patient underwent revision and another was lost to follow-up (Fig. 1).
Fig. 1.

This flow diagram shows the patients who were included in the study.
Patient-reported outcomes were assessed using the OKS (with 0 to 48 representing worst to best) [23], the reduced WOMAC score (with 0 to 100 representing worst to best) [27], the pain and function components of the Knee Society Score (KSS) (with 0 to 100 representing worst to best) [16], the Forgotten Joint Score (FJS) (with 0 to 100 representing worst to best) [3, 21], EuroQol 5D [5], and a VAS, which measures pain at rest and when mobilizing (with 0 to 10 representing none to worst). Scores were measured preoperatively and at 6 weeks, 6 months, 12 months, 2 years (initial study) and at exactly 5 years postoperatively (extension study).
The frequency and type of reoperations, as well as postoperative complications, were recorded. Radiographic assessment was performed by a blinded assessor (NS) at 5 years postoperatively using a system described by Meneghini et al. [22]—the Modern Knee Society Radiographic Evaluation System. We assessed the postoperative, 2-year, and 5-year short-leg AP, lateral, and skyline radiographs for signs of implant loosening in zones (Fig. 2). Lines were described as static or progressive with reference to both the postoperative and 2-year radiographs. If there was apparent progression between postoperative and 2 years but no progression between 2 years and 5 years, the lines were classified as static. Radiographic aseptic loosening was defined as the presence of progressive radiolucent lines in two or more zones.
Fig. 2.

These (A) AP and (B) lateral radiographs show radiographic zones around tibial and femoral components (zones translated from Meneghini et al. [22]).
Statistical Analysis
All data and graphical representations were evaluated using the GraphPad Prism V7.0 statistical package (GraphPad Prism, La Jolla, CA, USA) and IBM SPSS version 25 (IBM Corp, Armonk, NY, USA). The results are summarized using the mean and SD for continuous variables and frequencies and percentages for categorical variables for both the mechanical alignment and kinematic alignment patient groups. We applied repeat ANOVA measures to assess the differences between treatment groups at 5-year follow-up with respect to previously published outcomes at 2-year follow-up. A Bonferroni correction was applied to correct for multiple testing with adjusted p value for each comparison. Data was adjusted to ensure pair-wise matching in the 5-year analysis. We analyzed the patient-reported outcome measures within each treatment group from the 2-year time point to 5-year time point using the Mann-Whitney U test to account for patients who withdrew or were lost to follow-up. Differences were considered significant when p < 0.05.
We analyzed survivorship at 5 years on Kaplan-Meier curves with reoperation (any reason) and revision (change or addition of any component) defined as the primary endpoints. We compared survivorship on the log-rank test, differences were considered significant when p was < 0.05.
Results
Clinical Outcome Measures
At 5 years postoperatively, there was no difference in the mean scores for any of the patient-reported outcome measures (Table 1). As an example, the mean OKS did not differ between the two groups (kinematic alignment: 41.4 ± 7.2 versus mechanical alignment: 41.7 ± 6.3; difference -0.3 [95% CI - 3.2 to 2.5]; p = 0.99). Similarly the median scores at 2 years versus 5 years showed no differences for the mechanical alignment group (Table 2) or the kinematic alignment group (Table 3), apart from the EuroQol-5D index score (0.75 at 2 years versus 0.70 at 5 years; p < 0.01) in the mechanical alignment group.
Table 1.
5-year outcomes: kinematic alignment versus mechanical alignment
Table 2.
Mechanical alignment from 2-year to 5-year scores
Table 3.
Kinematic alignment from 2-year to 5-year score
Survivorship Free from Reoperation or Revision
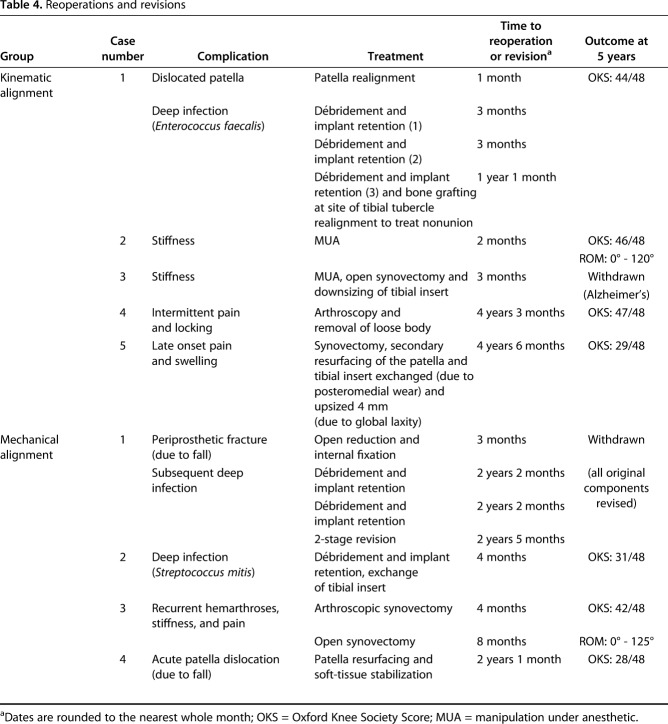
In the kinematic alignment group, five patients underwent further surgery (nine procedures), with no revisions of the femoral or tibial components. In the mechanical alignment group, four patients underwent further procedures (nine procedures), with one full revision of all components (Table 4).
Table 4.
Reoperations and revisions
The 5-year Kaplan-Meier survivorship was 92.2 (95% CI 80.4 to 97.0) for mechanical alignment and 89.7 (95% CI 77.0 to 95.6) for kinematic alignment with reoperation (any cause) as the primary endpoint; no difference was demonstrated between groups (log rank test; p = 0.674) (Fig. 3). With revision (change or addition of any component) as the primary endpoint, the 5-year Kaplan-Meier survivorship was 94.1 (95% CI 82.9 to 98.1) for mechanical alignment and 95.9 (95% CI 84.5 to 99.0) for kinematic alignment; no difference was demonstrated between groups (log rank test; p = 0.681) (Fig. 4).
Fig. 3.
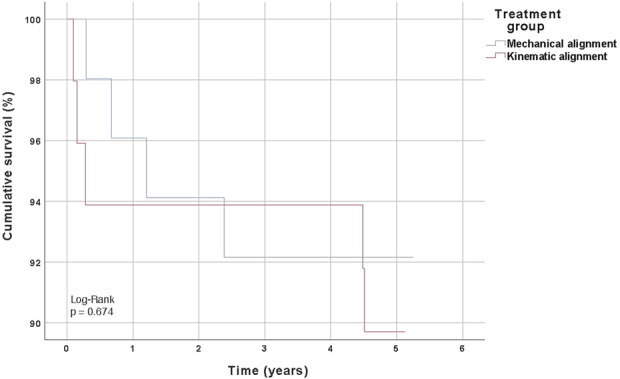
This graph shows Kaplan-Meier survivorship free from reoperation (any cause) as the primary endpoint.
Fig. 4.

This graph shows Kapan-Meier survivorship with revision (change or addition of any component) as the primary endpoint.
Radiographic Aseptic Loosening
At 5 years, one patient in the mechanical alignment group demonstrated possible radiographic aseptic loosening; the patient showed progressive radiolucent lines in two contiguous zones of the femur. The patient remains asymptomatic with high functional scores. There was no evidence of radiographic loosening in the kinematic alignment group.
Discussion
The aim of traditional mechanical alignment in TKA is to balance the load distribution by aligning the hip, knee, and ankle (Fig.5) angle to neutral to prevent polyethylene wear and minimize the risk of aseptic loosening. In contrast, the aim of kinematic alignment is to reduce pain and improve knee function and soft-tissue balance by implanting components in an alignment that more closely matches the patient’s pre-arthritic anatomy (Fig.5). In this randomized controlled trial, we found no differences in functional outcomes, survivorship free from reoperation and revision, or radiographic signs of aseptic loosening between patients whose TKAs were implanted using kinematic alignment or mechanical alignment at 5 years of follow-up.
Fig. 5.
These radiographs show (A and B) mechanical and (C and D) kinematic alignment at 5 years postoperatively in patients who underwent TKA.
There are a number of limitations to this study [29]. First, the kinematic alignment technique we used relied on patient-specific instrumentation and proprietary software for analyzing preoperative MRI data. This particular system is no longer available; however, the system is identical to those used in several previous studies [9, 10, 12, 14, 24, 25] and its accuracy was validated in a clinical trial [8]. Although alternative methods of kinematic alignment are described, image-derived instrumentation (IDI) represents a reproducible method of kinematic alignment that would be potentially generalizable were there any clinical benefit seen. Second, we did not control for patella resurfacing. There were, however, clearly defined indications for resurfacing, and the proportion of resurfaced procedures did not differ between the kinematic alignment and mechanical alignment groups. Third, these results at 5 years are suitable for evaluating early implant failures, but the long-term outcome of kinematic alignment remains unknown. Although we found similar rates of aseptic loosening between kinematic alignment and mechanical alignment, the original goal of mechanical alignment was to minimize the risk of this complication and differences may develop with longer term follow-up. Further, we note that early loosening is an uncommon event. Achieving a sample size of adequate statistical power is difficult in this setting, and our groups may simply be too small to demonstrate a true difference. In addition, there may be subtle loosening, as with any implant, that is not detectable with standard imaging. Finally, although the primary goal of this study was to compare the outcomes of kinematic alignment versus mechanical alignment component positioning, differing surgical techniques in the form of IDI in the kinematic alignment group and computer navigation in the mechanical alignment group were used. There may be varying levels of surgical proficiency as a consequence, favoring one or the other approach. However, we do not believe this alters the interpretation of our findings, as both computer navigation and IDI simply represent methods to enhance surgical accuracy when achieving alignment targets.
We found no differences in the mean scores for any of the patient-reported outcome measures recorded. To date, four RCTs have compared functional outcomes between mechanical alignment and kinematic alignment using this patient-specific implant system, with mixed findings. Our study supports those of Waterson et al. [26] who also found no difference in patient-reported outcomes between mechanical alignment and kinematic alignment. These findings suggest that altering alignment with kinematic alignment to more closely match patient native anatomy and kinematics does not lead to a measurable improvement in function. In contrast, Dossett et al. [10] and Calliess et al. [6] reported some improvements in clinical outcomes for kinematic alignment compared with mechanical alignment. Several factors may contribute to the difference in results. First, variation in the follow-up duration may be a contributing factor, although our cohort showed no differences in outcomes at 1, 2, and 5 years after surgery. Second, in Dossett et al.’s study [10], the patient group mostly consisted of men who were veterans (90%), which may affect the generalizability of the results. Third, different surgical methods were used in the mechanical alignment group, with some studies using conventional instrumentation for mechanical alignment versus a patient-specific implant for kinematic alignment, whereas our study used computer-navigation for mechanical alignment versus patient-specific implants for kinematic alignment.
There was no difference between the groups in terms of survivorship free from reoperation or revision 5 years after TKA. With a definition of revision as any change of a component or addition of a component (for example, secondary patella resurfacing), our groups showed no difference at 5 years postoperatively (two revisions in the kinematic alignment group versus three in the mechanical alignment group). In particular, our patellofemoral complication rate remains consistent with other series using kinematic alignment [9, 10, 12, 13, 14]. In a varus knee, kinematic alignment tends to internally rotate the femoral component compared with traditional mechanical alignment, which could be expected to adversely affect patella tracking. Calliess et al. [6] reported that two patients in their kinematic alignment group had “severe multidirectional instability” and underwent revision within the first year, compared with one patient in the mechanical alignment group who underwent revision for instability. Because the number of events is low, it is difficult to compare between studies; however, our complication rate is similar to that reported previously [1, 19].
Using the Modern Knee Society Radiographic Evaluation System to evaluate 5-year radiographs, we found no difference in the incidence of radiographic loosening [7, 11]. This remains a concern with kinematic alignment technique, as more than 30% of tibias in our study were implanted in more than 5° of varus (see Appendix, Supplemental Digital Content, http://links.lww.com/CORR/A294) and 5-year follow up is likely too short to detect clinical signs of aseptic loosening. The only published longer-term kinematic alignment data is from a design center, with Howell et al. [15] reporting no increased early failure rate with the kinematic alignment technique at 10 years in a noncomparative series. Biomechanical evidence suggests varus tibial alignment increases contact stresses and bone-implant loads [17, 20], and surgeons must remain cautious until independent longer-term kinematic alignment follow-up is available. We note one patient in the kinematic alignment group, with an initially well-functioning TKA, who developed late pain and swelling after mild trauma. The overall CT-measured coronal limb alignment was 2° valgus, with the femoral component in 5° valgus and the tibial component in 3° varus. The patient underwent secondary patella resurfacing; during this procedure considerable posteromedial wear of the tibial insert was seen and the liner exchanged and upsized. The significance of these findings in a single patient is unclear.
In conclusion, at 5 years postoperatively, we found no difference in clinical or radiographic signs of loosening and no differences in survivorship. We found no mid-term functional or radiographic differences between TKAs with mechanical alignment or kinematic alignment. The anticipated improvements in patient-reported outcomes with kinematic alignment were not realized. Because kinematic alignment results in a high proportion of patients whose tibial components are inserted in varus, loosening remains a potential long-term concern. Given the unknown impact on long-term survivorship of the substantial alignment alterations with kinematic alignment, our findings do not support the routine use of kinematic alignment outside of a research setting.
Acknowledgments
We thank Mr. Tony Danesh-Clough FRACS, Mr. Dean Schluter FRACS, and Mr. Rob Sharp FRCS Tr&Orth, consultant orthopaedic surgeons at North Shore Hospital Auckland, for acting as co-investigators on this study.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The institution of one or more of the authors (SWY, MLW, AB, BF, SH) has received, during the study period, funding from Stryker (Kalamazoo, MI, USA). One or more of the authors (AB, MLW, BF, SWY) or a member of his or her immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Stryker in the form of grants and/or consultancy fees. The remaining authors (NPTS, SH) certify that they have no commercial associations that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery at North Shore Hospital, Auckland, New Zealand and Waitakere Hospital, Waitakere, New Zealand.
References
- 1.Bannister G, Ahmed M, Bannister M, Bray R, Dillon P, Eastaugh-Waring S. Early complications of total hip and knee replacement: a comparison of outcomes in a regional orthopaedic hospital and two independent treatment centres. Ann R Coll Surg Engl. 2010;92:610-614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat Award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. Arthroplasty. 2012;27:430-436.e1. [DOI] [PubMed] [Google Scholar]
- 4.Blackburn J, Qureshi A, Amirfeyz R, Bannister G. Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee. 2012;19:522-524. [DOI] [PubMed] [Google Scholar]
- 5.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53-72. [DOI] [PubMed] [Google Scholar]
- 6.Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1743-1748. [DOI] [PubMed] [Google Scholar]
- 7.Chockalingam S, Scott G. The outcome of cemented vs. cementless fixation of a femoral component in total knee replacement (TKR) with the identification of radiological signs for the prediction of failure. Knee. 2000;7:233-238. [DOI] [PubMed] [Google Scholar]
- 8.Clark G, Leong A, McEwen P, Steele R, Tran T, Trivett A. Intraoperative reliability of ShapeMatch cutting guide placement in total knee arthroplasty. Comput Aided Surg. 2013;18:159-165. [DOI] [PubMed] [Google Scholar]
- 9.Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J. 2014;96:907-913. [DOI] [PubMed] [Google Scholar]
- 10.Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics. 2012;35:e160-e169. [DOI] [PubMed] [Google Scholar]
- 11.Ecker ML, Lotke PA, Windsor RE, Cella JP. Long-term results after total condylar knee arthroplasty. Significance of radiolucent lines. Clin Orthop Relat Res. 1987:151-158. [PubMed] [Google Scholar]
- 12.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471:1000-1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. 2015;39:2117-2124. [DOI] [PubMed] [Google Scholar]
- 14.Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013;21:2271-2280. [DOI] [PubMed] [Google Scholar]
- 15.Howell SM, Shelton TJ, Hull ML. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty. 2018; 33:3678-3684. [DOI] [PubMed] [Google Scholar]
- 16.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13-14. [PubMed] [Google Scholar]
- 17.Ishikawa M, Kuriyama S, Ito H, Furu M, Nakamura S, Matsuda S. Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee. 2015;22:206-212. [DOI] [PubMed] [Google Scholar]
- 18.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. Journal of Arthroplasty. 2008;23:26–29. [DOI] [PubMed] [Google Scholar]
- 19.Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293-297. [DOI] [PubMed] [Google Scholar]
- 20.Li Z, Esposito CI, Koch CN, Lee YY, Padgett DE, Wright TM. Polyethylene damage increases with varus implant alignment in posterior-stabilized and constrained condylar knee arthroplasty. Clin Orthop Relat Res. 2017;475:2981-2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H, Yuasa T, Behrend H, Kaneko K. Validation study of the Forgotten Joint Score-12 as a universal patient-reported outcome measure. Eur J Orthop Surg Traumatol. 2015;25:1141-1145. [DOI] [PubMed] [Google Scholar]
- 22.Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR. Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty. 2015;30:2311-2314. [DOI] [PubMed] [Google Scholar]
- 23.Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89:1010-1014. [DOI] [PubMed] [Google Scholar]
- 24.Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014;96:96-100. [DOI] [PubMed] [Google Scholar]
- 25.Nogler M, Hozack W, Collopy D, Mayr E, Deirmengian G, Sekyra K. Alignment for total knee replacement: a comparison of kinematic axis versus mechanical axis techniques. A cadaver study. Int Orthop. 2012;36:2249-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Joint J. 2016;98:1360-1368. [DOI] [PubMed] [Google Scholar]
- 27.Whitehouse SL, Lingard EA, Katz JN, Learmonth ID. Development and testing of a reduced WOMAC function scale. J Bone Joint Surg Br. 2003;85:706-711. [PubMed] [Google Scholar]
- 28.Woon JT, Zeng IS, Calliess T, Windhagen H, Ettinger M, Waterson HB, Toms AD, Young SW. Outcome of kinematic alignment using patient-specific instrumentation versus mechanical alignment in TKA: a meta-analysis and subgroup analysis of randomised trials. Arch Orthop Trauma Surg. 2018;138:1293-1303. [DOI] [PubMed] [Google Scholar]
- 29.Young SW, Walker ML, Bayan A, Briant-Evans T, Pavlou P, Farrington B. The Chitranjan S. Ranawat Award: No difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res. 2017;475:9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]