Abstract
Background
Anchored transosseous equivalent suture-bridge technique (TOE) is widely used for arthroscopic rotator cuff repair. It is unknown how patient outcomes scores, ROM, and integrity of the rotator cuff after repair using this anchored technique compare with those after repair using an anchorless transosseous technique (TO).
Questions/purposes
(1) What are the differences in patient-reported outcomes (American Shoulder and Elbow Surgeons [ASES] score) and shoulder ROM between TO and TOE rotator cuff repair techniques at 1 and 2 years after surgery? (2) What is the difference in repair integrity as measured by the re-tear rate, assessed ultrasonographically at 1 year, between these two techniques? (3) What is the difference in procedure duration between the two techniques when performed by a surgeon familiar with each?
Methods
We reviewed 331 arthroscopic rotator cuff repairs performed by one surgeon from December 2011 to July 2016 in this retrospective, matched-pair study. Of these patients, 63% (208 of 331) underwent repair with standard anchored technique (anchors placed in a double-row, TOE manner) and 37% (123 of 331) underwent anchorless TO repair, with the same indications for surgery between groups. Forty-four percent (91 of 208) of patients in the TOE group and 61% (75 of 123) of patients in the TO group met the inclusion criteria. Eighty percent (73 of 91) of patients in the TOE group and 88% (66 of 75) in the TO group had minimum 2-year follow-up. We matched each group to a cohort of 50 patients by sex, age, smoking status, and tear size (by Cofield classification: small, < 1 cm; medium, 1-3 cm; large, > 3-5 cm; or massive, > 5 cm). The resulting cohorts did not differ in mean age (TO, 62 years [range 53-65 years]; TOE, 58 years [range 53-65 years]; p = 0.79), mean BMI value (TO, 30 [range 27-33]; TOE, 29 [range 27-35]; p = 0.97), or dominant arm involvement (TO, 80%; TOE, 78%; p = 0.81). The cohorts were followed for at least 2 years (median, 3.2 years [interquartile range (IQR) 2.2-4.3] for TO and 2.9 years [IQR 2.0-3.5 years] for TOE). ASES scores and ROM were evaluated before surgery and at follow-up visits and were recorded in a longitudinally maintained institutional database. Repair integrity was assessed using ultrasonography at 1 year, as is standard in our practice. For each tear-size group, we calculated the proportion of intact tendon repairs versus the proportion of re-tears. Duration of surgery was recorded for each patient.
Results
At 1 year, we observed no difference in median ASES scores (90 [IQR 92-98] for TO and 88 [IQR 72-98] for TOE; p = 0.44); external rotation (50° [IQR 45°-60°) for TO and 50° [IQR: 40°-60°] for TOE; p = 0.58); forward flexion (165° [IQR 160°-170°] for both groups; p = 0.91); or abduction (100° [IQR 90°-100°] for TO and 90° [IQR 90°-100°] for TOE; p = 0.06). Fourteen percent of shoulders (seven of 50) in each treatment group had evidence of re-tear at 1 year (p > 0.99): 0 of 2 small tears in each group, 0 of 7 medium tears in each group, five of 32 large tears in each group, and two of 9 massive tears in each group (all, p > 0.99). At 2 years, we found no differences in median ASES scores (92 [IQR 74-98)] for TO and 90 [IQR 80-100] for TOE; p = 0.84); external rotation (60° [IQR 50°-60°] for both groups; p = 0.74); forward flexion (170° [IQR 160°-170°] for both groups; p = 0.69); or abduction (100° [IQR 90°-100°] for both groups; p = 0.95). We found no differences between groups in mean ± SD procedure time, which was 103 ± 20 minutes for TO repair and 99 ± 20 minutes for TOE repair (p = 0.45).
Conclusions
TO and TOE techniques for arthroscopic rotator cuff repair results in no differences in ROM, ASES scores, re-tear rates, and surgical time. Randomized control trials are needed to confirm these similarities or determine a superior method of repair. Future cost analyses may also help to determine the relative value of each technique.
Level of Evidence
Level III, therapeutic study.
Introduction
The original approach to rotator cuff repair was via open surgery, in which the cuff was repaired with transosseous sutures [8, 16]. During the past 20 years, arthroscopic techniques have allowed for less-invasive procedures, less deltoid muscle morbidity, and comparable likelihood of healing to those of open repair [16, 28]. Several new anchor and suture configurations have been developed to mimic the biomechanics of open repair and improve initial repair strength and healing rates. The current arthroscopic approach is often the suture-bridge technique, also known as a transosseous-equivalent construct (TOE) [17, 24, 27, 29]. Recently, arthroscopic anchorless transosseous techniques (TO) have been developed, which combine the advantages of open repair with those of an arthroscopic approach [6, 14, 22, 31, 34, 35]. Studies have described high healing rates and good patient-reported outcome scores after arthroscopic repair using the TO technique [3, 13, 22] but have not included TOE cohorts for comparison.
Much of the available data on arthroscopic TO repair are from biomechanical studies, which report conflicting information about the superiority of TOE versus TO repair [1, 21, 26, 29]. Some suggested inferior performance of the TO approach [21, 29], whereas others noted potential benefits, including greater vascularity at the insertion site [1, 2, 19, 20, 26]. Recently, a clinical study by Seidl et al. [30] compared TO and TOE repairs and found no substantial difference in pain or patient-reported outcomes at 1 year of follow-up. Their study’s statistical power was limited, however, with only 21 patients in each group, making it possible that clinically important differences between the treatments might have been present but might have gone undetected. In addition, anchorless repairs have other potential advantages, in that they leave less foreign material in the greater tuberosity than anchored repairs, and they reduce implant costs [22, 29]. Revision of failed TOE repairs may also be simpler than revision of failed TO repairs because TOE constructs are more likely to experience Type 1 failure (tendon pulling off bone) [29] than Type 2 failure (which occurs at the musculotendinous junction). If patient-reported outcomes and healing rates are equivalent between repair techniques, these benefits would be welcomed; however, any such considerations would be more than offset if TO repairs prove to be less effective or durable than TOE repairs. Also concerning is whether one technique may be more difficult to perform than the other, leading to longer operative times.
Therefore, we asked: (1) What are the differences in patient-reported outcomes (American Shoulder and Elbow Surgeons [ASES] score) and shoulder ROM between TO and TOE rotator cuff repair techniques at 1 and 2 years after surgery? (2) What is the difference in repair integrity as measured by the re-tear rate, assessed ultrasonographically at 1 year, between these two techniques? (3) What is the difference in procedure duration between the two techniques when performed by a surgeon familiar with each?
Patients and Methods
Patient Selection, Matching, and Indications
After receiving institutional review board approval to perform this study, we reviewed the medical records of 331 patients who underwent arthroscopic rotator cuff repair by one fellowship-trained shoulder surgeon (US) at our institution from December 2011 to July 2016. This surgeon was trained in both TO and TOE techniques during fellowship, has completed more than 100 cases of each approach, and trains residents and fellows in both techniques. Because the TO technique requires greater experience with suture management, training begins with the TOE approach and, after competency is achieved, we transition to a TO approach for a given trainee. Although patients were not randomized between the two techniques, we do not believe there was systematic bias in selection of the repair technique according to intraoperative factors. In this consecutive series, there were no instances in these cohorts in which we planned to perform TOE repair and converted to TO repair during the procedure, and likewise no patients were converted from TO repair to TOE repair. Patients were counseled that either anchors or tunnels would be used to secure the sutures used in the repair because we believed in their equipoise. No patient insisted on a particular technique. We excluded patients who had isolated partial-thickness tears, subscapularis tears, Grade 3 or Grade 4 osteoarthrosis, revision repairs, or repairs associated with distal clavicle excision, capsular release, calcific deposit removal, chondroplasty or microfracture, suprascapular nerve release, SLAP (superior labrum anterior and posterior) repair, or teres minor repair. We also excluded patients who did not complete the 2-year follow-up. Fifty of the remaining patients from each group were successfully matched by age (within 6 years), sex, tear size category (by Cofield classification), and smoking status. The remaining patients (16 TO, 23 TOE) could not be matched by these criteria to corresponding patients and were therefore excluded. Matching was performed by an author (EGH) who was blinded to cuff integrity results at the time of matching. The number of smokers was very small, precluding matching; therefore, smokers were excluded from both cohorts. This resulted in 50 matched patients in each cohort (Fig. 1).
Fig. 1.

The patient selection flowchart is shown here; AC = acromioclavicular; OA = osteoarthritis; TO = transosseous; TOE = transosseous equivalent; SLAP = superior labrum anterior and posterior.
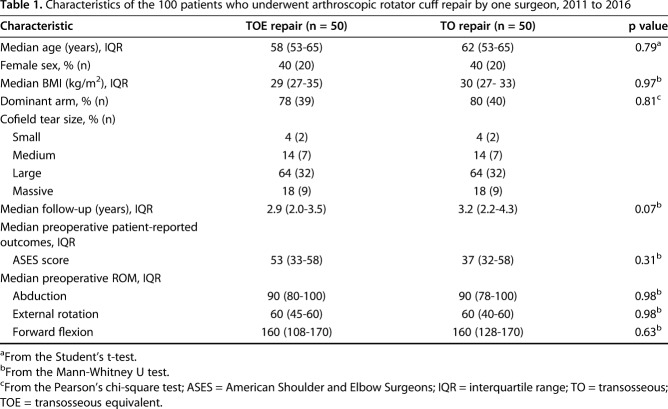
Demographic characteristics, including age, sex, and body mass index value, did not differ substantially between the TO and TOE groups (Table 1).
Table 1.
Characteristics of the 100 patients who underwent arthroscopic rotator cuff repair by one surgeon, 2011 to 2016
Data Collection
Data were collected from a longitudinally maintained database. Before surgery, all patients underwent a physical examination (including ROM testing of external rotation with the arm at the side, forward flexion, and abduction), radiography, and MRI. The size of each rotator cuff tear was determined using the Cofield classification [7] (small, < 1 cm; medium, 1-3 cm; large, > 3-5 cm; or massive, > 5 cm). In each group, there were two small, seven medium, 32 large, and nine massive rotator cuff tears. Other shoulder disorders, such as biceps tendon degeneration, were recorded and treated routinely with subpectoral biceps tenodesis. If the biceps tendon was already torn, tenodesis was not attempted. Duration of the surgical procedure was recorded for each.
Shoulder-specific, patient-reported outcomes were measured using the ASES score. At 3 months, 6 months, 1 year, 2 years, and latest follow-up, we assessed the ASES score and performed physical examinations of each patient. At a minimum of 1 year after surgery, patients underwent ultrasonography of the rotator cuff by the treating surgeon, as is routine for all patients after rotator cuff repair in our practice. A board-certified radiologist (AU) blinded to the treatment group independently assessed the rotator cuff’s integrity by reviewing the ultrasound images. In our evaluation of structural integrity, we exclusively used the radiologist’s interpretations. Median length of follow-up was 3.2 years (interquartile range [IQR] 2.2-4.3 years) for the TO group and 2.9 years (IQR 2.0-3.5 years) for the TOE group.
Surgical Technique
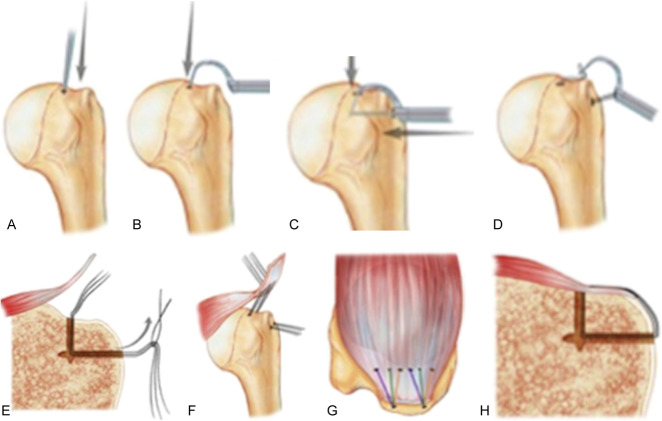
One surgeon (US), who is fellowship trained in shoulder surgery and incorporates both techniques into his practice regularly, performed all procedures. All patients underwent rotator cuff repair in the “beach chair” position. For the TO group, small tears were repaired using a single transosseous tunnel with two or three number-2 braided sutures in the tunnel; medium-sized to large tears were repaired using two tunnels with three number-2 braided sutures in each tunnel; and massive tears were repaired using two or three tunnels each with three number-2 braided sutures. The TransOs Tunneler system (Tensor Surgical, Chattanooga, TN, USA) or ArthroTunneler system (Tornier, Bloomington, MN, USA) was used to create the transosseous tunnels. Each of the sutures was passed separately through the rotator cuff and tied down in a simple fashion (Fig. 2A-H).
Fig. 2A-H These images illustrate the surgical steps of the typical anchorless transosseous approach to repair of a torn rotator cuff. (A) A bone punch was used at the desired anchor site in the greater tuberosity (arrow), (B) and a tunneling device was inserted into the pilot hole (arrow). (C) An awl was passed through the lateral cortex using the tunneling device (long arrow) after a capture device was inserted into the pilot hole (short arrow). (D) The tunneling device was removed and a passing suture was captured by the tunneling device and passed through the tunnel. (E) Repair sutures were passed through the passing loop as shown by the arrow. (F) The sutures were passed through the torn rotator cuff tendon. (G) The sutures were then tied together over the top of the cuff. (H) This image is a coronal cross-section of the tunneled transosseous cuff repair. Illustration: Tim Phelps, MS, FAMI, © (2016) JHU AAM Department of Art as Applied to Medicine, The Johns Hopkins University School of Medicine.
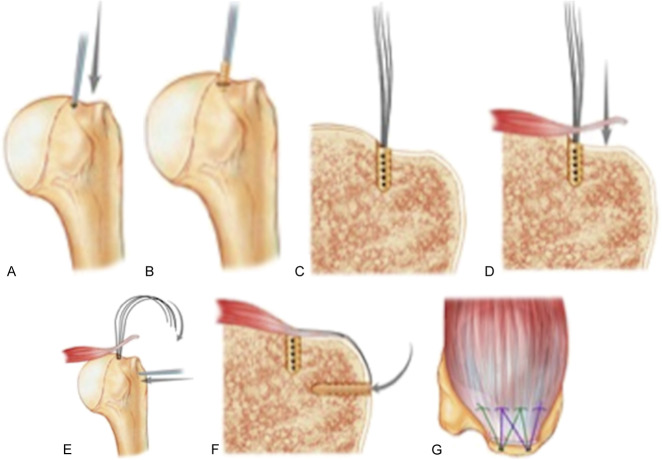
For the TOE approach, small tears were repaired using one medial and one lateral anchor; medium-sized to large tears were repaired using two medial anchors connected to one or two lateral anchors, as determined by the tear pattern, for a suture-bridge configuration with medially tied sutures; and massive tears were repaired using two or three medial anchors and two lateral anchors. We used 4.5-mm Healicoil PK medial row anchors (Smith & Nephew, Andover, MA, USA) and 4.5-mm Footprint Ultra PK lateral row anchors (Smith & Nephew) (Fig. 3A-G). After surgery, patients underwent identical pain control regimens and rehabilitation programs [4].
Fig. 3A-G These images illustrate the surgical steps of the typical anchored (transosseous equivalent) approach to repair of a torn rotator cuff. (A) A bone punch was used at the desired anchor site in the greater tuberosity (arrow), and (B) an anchor was inserted into the pilot hole. (C) This image is a coronal cross-section of the anchor in the tuberosity. (D) These images show a coronal cross-section of cuff reduction in the greater tuberosity (arrow), and (E) a bone punch used to insert a lateral anchor in the greater tuberosity (straight arrow shows direction of punch, and curved arrow shows direction of suture passage). (F) This image is a coronal cross-section of the anchored transosseous equivalent cuff repair after a lateral row anchor was placed (arrow). (G) This image is a superior view of anchored transosseous equivalent cuff repair. Illustration: Tim Phelps, MS, FAMI, © (2016) JHU AAM Department of Art as Applied to Medicine, The Johns Hopkins University School of Medicine.
Statistical Analysis
Data were analyzed using SPSS software, version 25 (IBM Corp, Armonk, NY, USA). The Shapiro-Wilk test and frequency histograms were used to determine the normality of distribution for each continuous dataset. Patient age and duration of procedure followed normal distributions and were compared between groups using t-tests. All other continuous datasets showed nonparametric distribution; therefore, comparisons between groups were performed using Mann-Whitney U tests. Within-group comparisons were performed using Wilcoxon signed-rank tests. The distributions of patient sex and Cofield classification were identical between groups because of the matched nature of the cohorts. Arm dominance and overall cuff integrity were compared using Pearson’s chi-square tests. Re-tear rates, stratified by Cofield classification, were compared using Fisher exact tests.
Sample Size Justification
An a priori power analysis was performed to determine the necessary sample size using G*Power, version 3.1, software [12]. Reported values for the minimal clinically important difference for the ASES score (primary outcome) vary. One report based on various diagnoses, including some postoperative patients, suggested a minimal clinically important difference of 6.4 points [25]. Another study of only nonoperative treatment of rotator cuff disease reported minimal clinically important difference values ranging from 12 to 17 points [33]. The required sample size was 45 patients per group to detect a 12-point difference in the ASES score as a function of the significance level (α = 0.05), effect size (0.6), and power level (1 – β = 0.80).
Results
Clinical Outcome Measures
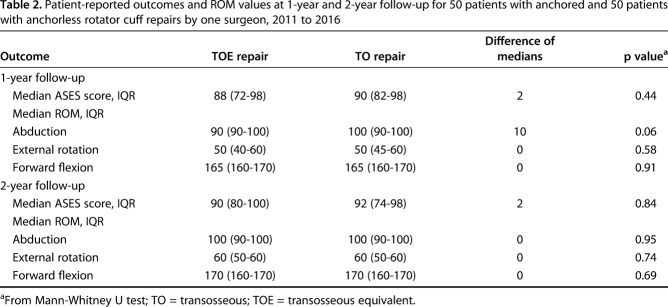
At 1 year, we found no differences in median ASES scores, which were 90 (IQR 82-98) for TO and 88 (IQR 72-98) for TOE (p = 0.44) (Table 2). We also found no differences at 1 year in median external rotation (50° [IQR 45°-60°] for TO and 50° [IQR 40°-60°] for TOE; p = 0.58); median forward flexion (165° [IQR 160°-170°] for both groups; p = 0.91); or median abduction (100° [IQR 90°-100°] for TO and 90° [IQR 90°-100°] for TOE; p = 0.06). The same held true at 2 years, with median ASES scores of 92 (IQR 74-98) for TO and 90 (IQR 80-100) for TOE (p = 0.84); median external rotation of 60° (IQR 50°-60°) for both groups (p = 0.74); median forward flexion of 170° (IQR 160°-170°) for both groups (p = 0.69); and median abduction of 100° (IQR 90°-100°) for both groups (p = 0.95).
Table 2.
Patient-reported outcomes and ROM values at 1-year and 2-year follow-up for 50 patients with anchored and 50 patients with anchorless rotator cuff repairs by one surgeon, 2011 to 2016
At 1 year postoperatively, the improvement in ASES score (compared with preoperative score) was greater in the TO group (median 42; IQR 29-62) than in the TOE group (median 32; IQR 19-43; p = 0.03). This difference was not seen at 2 years postoperatively, when median ASES scores were 42 (IQR 21-62) in the TO group and 40 (IQR 25-50) in the TOE group (p = 0.75).
At 1 year postoperatively, the changes in ROM were similar between groups; for external rotation, median, -10° [IQR -10°-0°] for TO and 0° (IQR -10°-14°) for TOE (p = 0.16); for forward flexion, median, 10° (IQR 0°-13°) for TO and 10° (IQR 10°-40°) for TOE (p = 0.46); and for abduction, median, 0° (IQR 0°-10°) for TO and 0° (IQR -10°-15°) for TOE (p = 0.43). These similarities persisted at 2 years postoperatively, when changes in ROM were similar between groups; for external rotation, median, 0° (IQR -10°-20°) for TO and 0° (IQR 0°-10°) for TOE (p = 0.91); for forward flexion, median 10° (IQR 0°-35°) for TO and 10° (IQR 10°-50°) for TOE (p = 0.88); and for abduction, median 0° (IQR 0°-20°) for TO and 0° (IQR 0°-10°) for TOE (p = 0.63).
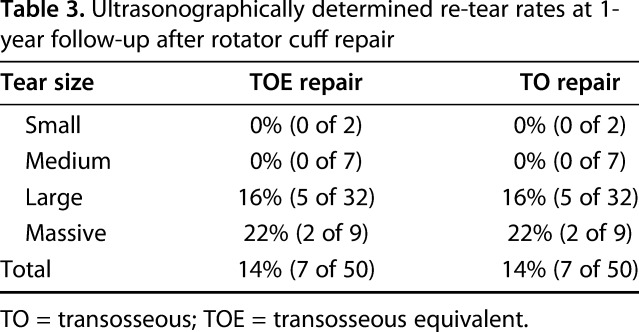
Repair Integrity
Overall repair integrity was the same between groups, with 86% (43 of 50) of repairs intact on ultrasound imaging (p > 0.99; Table 3). When stratified by Cofield classification, the rates of re-tear were identical between the two repair types: 0% (0 of 2) for small tears; 0% (0 of 7) for medium tears; 16% (5 of 32) for large tears; and 22% (2 of 9) for massive tears) (p > 0.99).
Table 3.
Ultrasonographically determined re-tear rates at 1-year follow-up after rotator cuff repair
Procedure Duration
We found no difference between groups in the mean ± SD procedure time, which was 103 ± 20 minutes for TO repair and 99 ± 20 minutes for TOE repair (p = 0.45).
Discussion
Many options for arthroscopic rotator cuff repair are available, with some techniques aiming to reproduce the biomechanics of a TO repair [17, 24, 27, 29]. Biomechanical data have been used to support the notion that anchored repair is superior because of higher ultimate failure load [19], but these differences in fixation strength may be overcome by adjusting other technical parameters, including the number of sutures placed through the tendon [18] and the suture configuration (mattress versus simple) [11]. In addition to biomechanical data, we need clinical support for our chosen technique, including subjective patient-reported outcome scores and objective measures such as repair integrity and ROM. We compared the outcomes of anchorless TO repair with that of a TOE construct. Our findings suggest that the TO method may provide effective repair with no difference in patient-reported outcome scores compared with TOE repair.
The limitations of this retrospective study include lack of randomization of technique, which may lead to selection bias that has not been identified. Our matching may not fully account for this potential bias. In an attempt to minimize the differences between groups, we matched patients by age, sex, tear size category, and smoking status. The investigator who performed the matching was blinded from cuff integrity results, but differences may be present that were not evaluated, such as Goutallier classification of fatty atrophy, activity level, and medical comorbidities. If the groups differed in terms of atrophy of the cuff musculature, the healing rates may be less similar than they seem. The authors were not blinded to technique while performing follow-up examinations, including measurement of ROM. Ultrasonography to evaluate cuff integrity was performed by the treating surgeon, who was not blinded to the technique used; however, the radiologist was blinded when reviewing the results. As with many studies, some patients were lost to follow-up. Proportions of loss were similar between the TO group (12%) and the TOE group (20%) but a higher follow-up rate may have allowed for additional matching and a larger sample. Restricting the study to patients treated by one surgeon at one institution may result in limited external validity. The surgeon was a fellowship-trained shoulder surgeon at an academic medical center that serves patients from urban and suburban areas. The surgeon was experienced with both approaches, having performed more than 100 cases using each technique. Results may differ according to the surgeon’s experience with these approaches. We have found that trainees obtain a basic level of mastery with TO repair, after learning TOE repair, by performing approximately 10 procedures.
ASES scores and ROM at 1 and 2 years after surgery were no different between the TO and TOE groups. This finding is consistent with those of Seidl et al. [30], who found no differences in patient-reported outcomes at 1 year after surgery in a smaller study. Other studies have reported good functional outcomes after arthroscopic TO rotator cuff repair, but they did not include a control group [3, 13, 22].
The risk of re-tear after anchorless TO repair was no different than that of a matched cohort that underwent TOE repair. Kuroda et al. [22] reported a 6% re-tear rate after TO repair, which is lower than the 14% seen in our study; however, their study did not include any massive tears, which failed at the highest rate of any tear size category in our study (22%). This finding is consistent with other modes of fixation, in which larger tears are associated with higher failure rates [9, 10, 15, 23, 32].
In a biomechanical study, Kilcoyne et al. [19] found that when failure occurred, the primary modes were Type 2 tendon tear after TOE repair (seven of 10 patients) and Type 1 tendon tear after TO repair (six of 10 patients). Type 2 tears occur at the muscle-tendon junction with the residual tendon attached to the greater tuberosity [5], which can make surgical revision difficult. In contrast, Type 1 tears, in which the tendon re-tears from the greater tuberosity, leave more tendon and bone available for repair, simplifying revision [16, 20, 29].
Finally, we found no difference in the operative time between the TO and TOE groups. This finding agrees with that of Seidl et al. [30], who showed no difference between the techniques. It is important to note that the surgeon in this study was experienced with both techniques, and a learning curve may be seen early during the implementation of a new technique.
Our results suggest that TO and TOE rotator cuff repair techniques result in no differences in patient-reported outcomes, shoulder ROM, and structural integrity in a matched cohort study that was adequately powered to detect the minimal clinically important difference for the ASES score. Operative time did not differ between techniques. These findings support the continued use of both techniques, as well as further investigation into each. Future randomized controlled trials can reduce potential biases to confirm equivalence of the two techniques or determine whether one is superior in the outcomes it produces. A cost-effectiveness analysis could further determine the relative value of each approach.
Acknowledgments
We thank Arvinder Uppal MD, for her imaging review and Kerry Kennedy BA, and Rachel Box MS, for editing the manuscript.
Footnotes
One of the authors certifies that he (US), or a member of his immediate family, has received or may receive payments or benefits, during the study period, in an amount of USD < 10,000 from Smith & Nephew (Andover, MA, USA) and between USD 10,000-100,000 from Orthospace Inc. (Caesarea, Hefa, Israel), between USD 10,000-100,000 from Conventus (Maples Grove, MN, USA), between USD 10,000-100,000 from Wright Medical (Memphis, TN, USA), between USD 10,000-100,000 from Arthrex (Naples, FL, USA), between USD 10,000-100,000 from DePuy Synthes (Warsaw, IN, USA), between USD 10,000-100,000 from Omega Medical Grants Association (Rosemont, IL, USA), all outside the submitted work. One author (US) reports that he has a patent pending for an augmentable anchor.
Each of the remaining authors certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Apreleva M, Ozbaydar M, Fitzgibbons PG, Warner JJ. Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519-526. [DOI] [PubMed] [Google Scholar]
- 2.Behrens SB, Bruce B, Zonno AJ, Paller D, Green A. Initial fixation strength of transosseous-equivalent suture bridge rotator cuff repair is comparable with transosseous repair. Am. J. Sports Med. 2012;40:133-140. [DOI] [PubMed] [Google Scholar]
- 3.Black EM, Lin A, Srikumaran U, Jain N, Freehill MT. Arthroscopic transosseous rotator cuff repair: technical note, outcomes, and complications. Orthopedics. 2015;38:e352-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brigham and Women's Hospital. Arthroscopic Rotator Cuff Repair Frequently Asked Questions. Available at: https://www.brighamandwomens.org/assets/BWH/patients-and-families/rehabilitation-services/pdfs/shoulder-arthroscopic-rct-repair-protocol-hybrid-patient-therapist.pdf. Accessed on November 26. 2016.
- 5.Cho NS, Yi JW, Lee BG, Rhee YG. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38:664-671. [DOI] [PubMed] [Google Scholar]
- 6.Cicak N, Klobucar H, Bicanic G, Trsek D. Arthroscopic transosseous suture anchor technique for rotator cuff repairs. Arthroscopy. 2006;22:565 e561-566. [DOI] [PubMed] [Google Scholar]
- 7.Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982;154:667-672. [PubMed] [Google Scholar]
- 8.Cole BJ, ElAttrache NS, Anbari A. Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy. 2007;23:662-669. [DOI] [PubMed] [Google Scholar]
- 9.DeHaan AM, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med. 2012;40:1176-1185. [DOI] [PubMed] [Google Scholar]
- 10.Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835-841. [DOI] [PubMed] [Google Scholar]
- 11.Esquivel AO, Duncan DD, Dobrasevic N, Marsh SM, Lemos SE. Load to failure and stiffness: anchor placement and suture pattern effects on load to failure in rotator cuff repairs. Orthop J Sports Med. 2015;3:2325967115579052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191. [DOI] [PubMed] [Google Scholar]
- 13.Flanagin BA, Garofalo R, Lo EY, Feher L, Castagna A, Qin H, Krishnan SG. Midterm clinical outcomes following arthroscopic transosseous rotator cuff repair. Int J Shoulder Surg. 2016;10:3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleega BA. Arthroscopic transhumeral rotator cuff repair: Giant needle technique. Arthroscopy. 2002;18:218-223. [DOI] [PubMed] [Google Scholar]
- 15.Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254-1260. [DOI] [PubMed] [Google Scholar]
- 16.Garofalo R, Castagna A, Borroni M, Krishnan SG. Arthroscopic transosseous (anchorless) rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2012;20:1031-1035. [DOI] [PubMed] [Google Scholar]
- 17.Hapa O, Barber FA, Sunbuloglu E, Kocabey Y, Sarkalkan N, Baysal G. Tendon-grasping strength of various suture configurations for rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011;19:1749-1754. [DOI] [PubMed] [Google Scholar]
- 18.Jost PW, Khair MM, Chen DX, Wright TM, Kelly AM, Rodeo SA. Suture number determines strength of rotator cuff repair. J Bone Joint Surg Am. 2012;94:e100. [DOI] [PubMed] [Google Scholar]
- 19.Kilcoyne KG, Guillaume SG, Hannan CV, Langdale ER, Belkoff SM, Srikumaran U. Anchored transosseous-equivalent versus anchorless transosseous rotator cuff repair: A biomechanical analysis in a cadaveric model. Am J Sports Med. 2017;45:2364-2371. [DOI] [PubMed] [Google Scholar]
- 20.Kim SH, Kim J, Choi YE, Lee HR. Healing disturbance with suture bridge configuration repair in rabbit rotator cuff tear. J Shoulder Elbow Surg. 2016;25:478-486. [DOI] [PubMed] [Google Scholar]
- 21.Kummer FJ, Hahn M, Day M, Meislin RJ, Jazrawi LM. A laboratory comparison of a new arthroscopic transosseous rotator cuff repair to a double row transosseous equivalent rotator cuff repair using suture anchors. Bull Hosp Jt Dis (2013). 2013;71:128-131. [PubMed] [Google Scholar]
- 22.Kuroda S, Ishige N, Mikasa M. Advantages of arthroscopic transosseous suture repair of the rotator cuff without the use of anchors. Clin Orthop Relat Res. 2013;471:3514-3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533-1541. [DOI] [PubMed] [Google Scholar]
- 24.Longo UG, Franceschi F, Spiezia F, Marinozzi A, Maffulli N, Denaro V. The low-profile Roman bridge technique for knotless double-row repair of the rotator cuff. Arch Orthop Trauma Surg. 2011;131:357-361. [DOI] [PubMed] [Google Scholar]
- 25.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587-594. [DOI] [PubMed] [Google Scholar]
- 26.Park MC, Cadet ER, Levine WN, Bigliani LU, Ahmad CS. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154-1159. [DOI] [PubMed] [Google Scholar]
- 27.Park MC, Jun BJ, Park CJ, Oh JH, Lee TQ. Biomechanical analysis of a knotless transtendon interimplant mattress repair for partial-thickness articular-sided rotator cuff tears. Am J Sports Med. 2009;37:2427-2434. [DOI] [PubMed] [Google Scholar]
- 28.Post M, Silver R, Singh M. Rotator cuff tear. Diagnosis and treatment. Clin Orthop Relat Res. 1983:78-91. [PubMed] [Google Scholar]
- 29.Salata MJ, Sherman SL, Lin EC, Sershon RA, Gupta A, Shewman E, Wang VM, Cole BJ, Romeo AA, Verma NN. Biomechanical evaluation of transosseous rotator cuff repair: do anchors really matter? Am J Sports Med. 2013;41:283-290. [DOI] [PubMed] [Google Scholar]
- 30.Seidl AJ, Lombardi NJ, Lazarus MD, Black EM, Maltenfort MG, Pepe MD, Austin LS. Arthroscopic Transosseous and Transosseous-Equivalent Rotator Cuff Repair: An Analysis of Cost, Operative Time, and Clinical Outcomes. Am J Orthop (Belle Mead NJ). 2016;45:E415-E420. [PubMed] [Google Scholar]
- 31.Shea KP, Jennings JE. Arthroscopic rotator cuff repair using a transhumeral approach to fixation. Arthroscopy. 1998;14:118-122. [DOI] [PubMed] [Google Scholar]
- 32.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953-960. [DOI] [PubMed] [Google Scholar]
- 33.Tashjian RZ, Deloach J, Green A, Porucznik CA, Powell AP. Minimal clinically important differences in ASES and simple shoulder test scores after nonoperative treatment of rotator cuff disease. J Bone Joint Surg Am. 2010;92:296-303. [DOI] [PubMed] [Google Scholar]
- 34.Tauber M, Hoffelner T, Penzkofer R, Koller H, Zenner J, Hitzl W, Moroder P, Resch H. Arthroscopic rotator cuff repair: a biomechanical comparison of the suture-bridge technique vs. a new transosseous technique using SutureButtons. Clin Biomech (Bristol, Avon). 2011;26:910-916. [DOI] [PubMed] [Google Scholar]
- 35.Tauber M, Koller H, Resch H. Transosseous arthroscopic repair of partial articular-surface supraspinatus tendon tears. Knee Surg Sports Traumatol Arthrosc. 2008;16:608-613. [DOI] [PubMed] [Google Scholar]