Abstract
Objective
The aim of this cross‐sectional study was to compare the masticatory performance and oral health‐related quality of life (OHRQoL) of edentulous maxillectomy patients with and without implant‐supported obturator prostheses.
Material and methods
Nineteen edentulous maxillectomy patients with completed prosthetic obturator treatment in the upper jaw participated in this study. In nine patients, the obturator prosthesis was supported by implants in the remaining bone of the midface and/or skull base to improve retention. Masticatory performance was measured objectively by the mixing ability test (MAT) and subjectively by three OHRQoL questionnaires: (a) the Oral Health Impact Profile for EDENTulous people (OHIP‐EDENT), (b) the Obturator Function Scale (OFS), and (c) the Dutch Liverpool Oral Rehabilitation Questionnaire version 3 (LORQv3‐NL). The independent t test and the Mann–Whitney U test were used to test for differences in outcomes of patients with and without implant‐retention of their obturator prostheses.
Results
Patients with implant‐supported obturator prostheses had significantly better masticatory and oral function, reported fewer chewing difficulties, and had less discomfort during food intake than did patients with a conventional obturator.
Conclusion
Supporting prosthetic obturators after maxillectomy with implants improve oral functioning, chewing, and eating comfort. This treatment modality is a viable technique to improve the functionality of prosthetic rehabilitation in patients who have undergone maxillectomy.
Keywords: dental implant, mastication, maxillary defect, maxillofacial reconstruction, midfacial defect, obturator, quality of life
1. INTRODUCTION
Maxillary defects due to trauma, infections, or tumour resections can result in tremendous limitations in daily life, depending on the size and anatomical location of the defect (Umino, Masuda, Ono, & Fujita, 1998; Vero et al., 2015). Surgical reconstruction of these defects remains challenging and controversial due to the complex three‐dimensional anatomy of the maxilla and midface (Brown, Schache, & Butterworth, 2016; Mertens, Freudlsperger, et al., 2016; Santamaria & Cordeiro, 2006). Preserving the oronasal separation and a clear nasal airway is important for optimal mastication, deglutition, and phonetics (Santamaria & Cordeiro, 2006). These oral functions are essential for the total rehabilitation of the patient and, therefore, directly related to quality of life issues (Depprich et al., 2011; Kornblith et al., 1996). Microsurgical repair is regarded as the standard option in reconstructive surgery of the face, depending on the defect size and the indication (Brown et al., 2016; Lethaus, Lie, et al., 2010). However, excellent facial contour, function, and acceptable aesthetics can seldom be achieved with a single‐stage procedure (Lethaus, Kessler, Boeckman, Poort, & Tolba, 2010). A considerable number of these patients will consequently remain deprived of dental rehabilitation and will not return to normal food intake (Triana et al., 2000). Nonetheless, prosthetic obturation appears to be the preferred treatment modality for many patients, which generally leads to an improvement of masticatory performance (Andrades, Militsakh, Hanasono, Rieger, & Rosenthal, 2011; Sharma & Beumer, 2005; Vero et al., 2015). However, prosthodontic treatment is challenging due to technical limitations, such as poor retention, instability of the obturator prosthesis, and oronasal incompetence (Andrades et al., 2011). Retention of the obturator prosthesis is very difficult to achieve, especially in edentulous patients. Nevertheless, implants have been placed successfully in the residual maxillary alveolar process, the pterygoid, and zygomatic bone for maxillary prosthetic rehabilitation (Goiato et al., 2014; Huang et al., 2014). To the best of our knowledge, the literature lacks objective masticatory performance testing that is combined with patient‐reported oral health‐related quality of life (OHRQoL) after prosthetic obturation of edentulous maxillectomy patients (Chen, Ren, Gao, et al., 2016; Chen, Ren, Huang, et al., 2016; Landes, 2005; Mertens, de San Jose Gonzalez, et al., 2016; Seignemartin, Miranda, Luz, & Teixeira, 2015; Wang et al., 2017). Therefore, the aim of this study was to compare the masticatory performance and OHRQoL of edentulous maxillectomy patients with and without implant‐supported obturator prostheses.
2. MATERIALS AND METHODS
2.1. Patients
All patients that were referred to the Department of Cranio‐Maxillofacial Surgery at Maastricht University Medical Centre (MUMC+) for surgical and prosthetic rehabilitation in the maxilla/midface between 2005 and 2015 were asked to participate in this comparative cross‐sectional study. We compared patients with implant‐supported obturator prostheses (Group 1) with patients wearing conventional obturator prostheses (Group 2). Patients with maxillary/midface defects in edentulous upper jaws were included when the prosthetic obturator treatment was completed. Brown's classification was used to determine the defect size in the maxilla/midface (Brown & Shaw, 2010). The study was approved by the Ethics Committee of the MUMC+ (METC 15‐4‐123). Informed consent was obtained from all participating patients.
2.2. Procedure
Patients with a status eligible for implants after partial or total maxillectomy or partial or total loss of the maxilla/midface were treated according to the “surgical and prosthetic reconsiderations in patients with maxillectomy protocol” as defined by Lethaus, Lie, et al. (2010). Implants were not placed if it was expected that there would be sufficient prosthetic options for a conventional obturator. Furthermore, some patients refused implant treatment. The decision of using implants was not based on the prognosis of the patient. Imaging for digital planning was based on computerized tomography (CT) scans acquired by multi‐slice CT (Siemens) or cone‐beam CT (ICAT, Hatfield). Implant sites in the remaining facial skeleton or skull base were planned based on the CT‐data with the Simplant 3D® program (Dentsply Sirona, Wals bei Salzburg). When standard abutments did not comply with the required distances or angulations of our protocol, individual abutments were designed by hand or by using the Cinema 4D® planning program (Design Express). If possible, a bar construction was made on the dental implants to support the obturator. Magnet abutments were used as an alternative retention method when the space between two implants was too wide (Figures 1 and 2).
Figure 1.
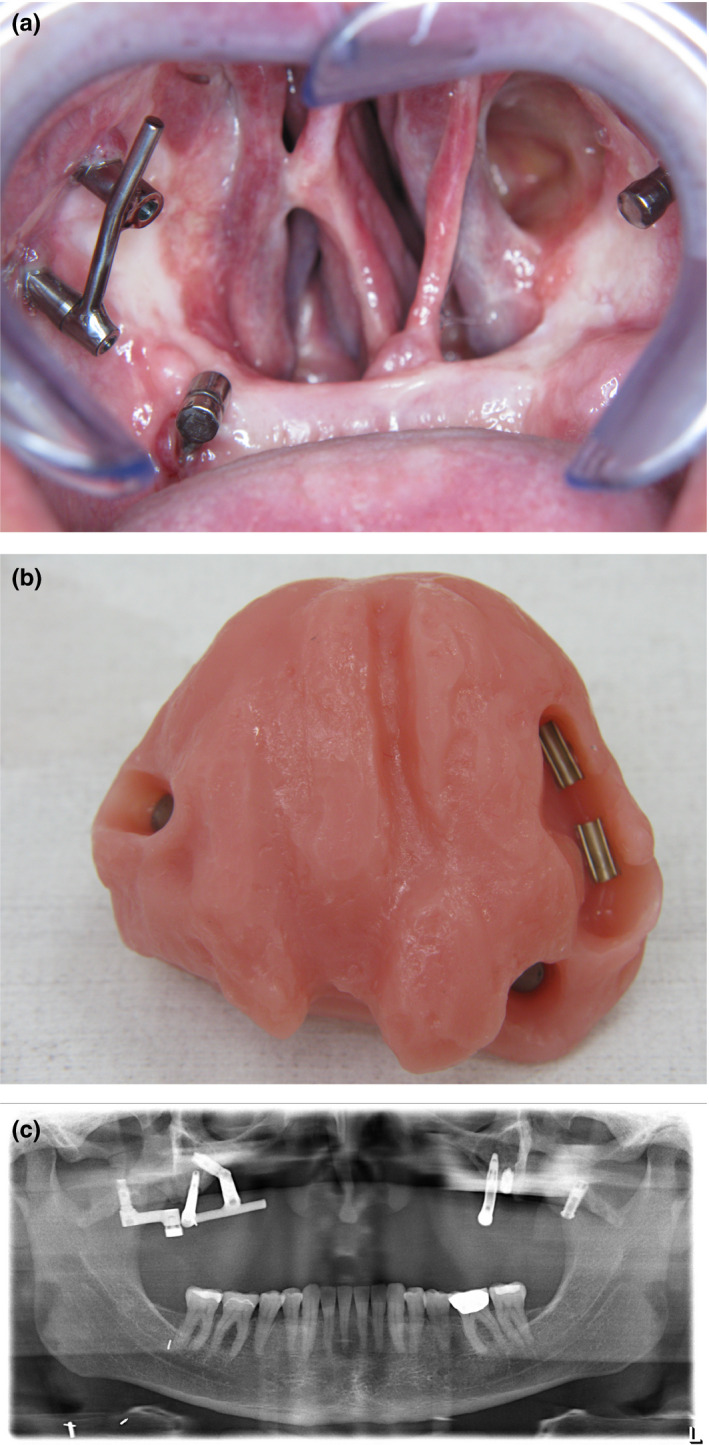
A patient presented with a Brown class IId defect (Brown & Shaw, 2010) after avascular necrosis after Le Fort I osteotomy. (a) Bar construction was made on the dental implants to support the obturator, where the space was too large between two implants, magnet abutments were used as alternative retention method. (b) Retentive parts in the obturator prosthesis. (c) Panoramic radiography showed the position of dental implants in remaining bony parts of the midface or skull base
Figure 2.
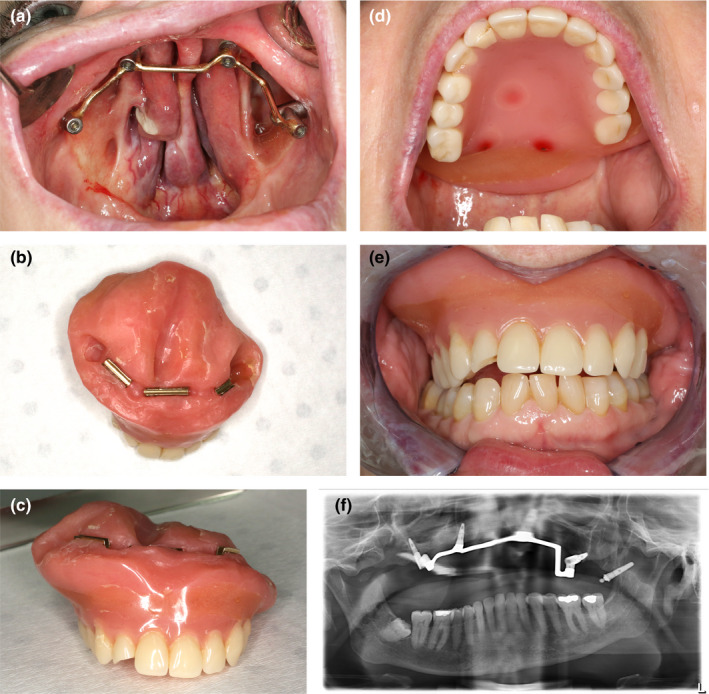
A patient presented with a Brown class IId defect (Brown & Shaw, 2010) after treatment of ameloblastoma. (a) Bar construction was made on the dental implants to support the obturator. (b) Retentive parts in the obturator prosthesis. (c) Frontal view of the obturator. (d) Palatal view of the final prosthesis. (e) Frontal view many years (>8) after implant‐supported obturator delivery. (f) Panoramic radiography showed the position of dental implants in remaining bony parts of the midface or skull base
2.3. Data acquisition
The mixing ability test (MAT) was used to measure the masticatory performance objectively (van der Bilt, Speksnijder, de Liz Pocztaruk, & Abbink, 2012; Speksnijder, Abbink, van der Glas, Janssen, & van der Bilt, 2009). Subjective aspects were measured with three OHRQoL questionnaires: (a) the Oral Health Impact Profile for EDENTulous people (OHIP‐EDENT) (Allen & Locker, 2002), (b) the Obturator Functioning Scale (OFS) (Kornblith et al., 1996), (c) and the Dutch Liverpool Oral Rehabilitation Questionnaire version 3 (LORQv3‐NL) (Engelen, Buurman, Bronkhorst, & van Heumen, 2017; Pace‐Balzan, Butterworth, Dawson, Lowe, & Rogers, 2008; Pace‐Balzan, Butterworth, Lowe, & Rogers, 2009; Pace‐Balzan, Cawood, Howell, Lowe, & Rogers, 2004).
2.4. Masticatory performance
The MAT measures how well a subject can mix a two‐coloured wax tablet by chewing on it. The tablet has a diameter of 20 mm and consists of two 3 mm layers of red and blue wax. The test‐wax is a soft material (Plasticine modelling wax, non‐toxic DIN EN‐71) that forms a compact bolus during chewing and was offered at room temperature (20°C). After chewing, the wax is flattened between foils to a thickness of 2.0 mm to avoid shadows. Then, the test‐wax is illuminated by a scanner lamp and photographed on both sides using a high‐quality scanner (Epson V750). The images of the wax were analysed and processed using a commercially available program for image analysis (Adobe Photoshop CS3). Intermediate colour intensities appear, and the spreads of the intensities for red and blue decrease. A lower mixing ability index (MAI) score implies a better‐mixed tablet and, hence, better masticatory performance (van der Bilt et al., 2012; Speksnijder et al., 2009).
2.5. Oral health impact profile for EDENTulous people
The OHIP‐EDENT is based on the original 49 items of OHIP and adapted for edentulous patients. The internal consistency of the OHIP‐EDENT has a Cronbach's alpha of .86–.97 (He & Wang, 2015; Sato, Kaiba, Yamaga, & Minakuchi, 2012; Souza, Patrocinio, Pero, Marra, & Compagnoni, 2007). The test‐retest reliability has an intraclass correlation (ICC) of .57–.76 (He & Wang, 2015; Souza et al., 2007). The aim of the OHIP‐EDENT is to detect OHRQoL changes, as influenced by the clinical aspects of edentulism and its treatment. The in total 19 items are defined to measure seven domains: (1) functional limitation (3 items), (2) pain (4 items), (3) psychological discomfort (2 items), (4) physical disability (3 items), (5) psychological disability (2 items), (6) social disability (3 items), and (7) handicap (2 items). Each item is scored on a Likert scale from 1 (‘Never’) to 5 (‘Very often’). The outcomes of the OHIP‐EDENT can have a range from 19 to 95. A score of 19 means that dental problems do not affect daily life at all, whereas a score of 95 means that dental problems affect daily life very often.
2.6. Obturator Functioning Scale
The OFS assesses patients' satisfaction and the quality of their obturator prosthesis (Kornblith et al., 1996). The total scale of the questionnaire has an excellent internal consistency, and the eating and speech sub‐scales have a Cronbach's alpha of .86, .82, and .87, respectively (Kornblith et al., 1996). This questionnaire consists of 15 items in total and three subcategories: (a) eating problems (3 items), (b) speech problems (5 items), and (c) other problems (7 items). Each item is scored on a Likert scale from 1 (‘Not at all a problem’) to 5 (‘Always a problem’).
2.7. Dutch liverpool oral rehabilitation questionnaire version 3
The LORQv3‐NL evaluates the impact of oral rehabilitation on OHRQoL in patients treated for oral cancer. The LORQv3‐NL is divided into four sections and consists of (a) oral function, oral‐facial appearance and social interaction (17 items), (b) patient satisfaction of prostheses (4 items), (c) patient satisfaction upper dentures (6 items), and (d) patient satisfaction of lower dentures (6 items). The internal consistency of these sections has a Cronbach's alpha of .89, .83, .75, and .81, respectively (Engelen et al., 2017). All items are rated on a 1 to 4 Likert scale from 1 (‘Never’) to 4 (‘Always’) and refer to recent symptoms or problems experienced during the previous week.
2.8. Statistics
The presentation of results is primarily descriptive with means, standard deviations (SD), and medians. Fisher's exact test, the Chi‐square‐test, and Independent t tests were used to assess whether there are differences in demographic and clinical data. Values of the implant‐retained group versus the conventional group of the MAI score (continued data) were compared with Independent t tests when data were normally distributed; otherwise, the Mann–Whitney U test was applied. Normal distribution was verified by using the Shapiro–Wilk test. The Mann–Witney U Test was used to compare the outcome of the OHIP‐EDENT, OFS, and LORQv3‐NL questionnaires (ordinal data) for the two patient groups. Statistical analyses were regarded as significant if the p‐value was equal to or lower than .05. Data were evaluated using SPSS (IBM version 24 for Mac).
A post hoc power analysis was performed on the primary outcome MAI score by G*Power (Faul, Erdfelder, Buchner, & Lang, 2009; Faul, Erdfelder, Lang, & Buchner, 2007).
3. RESULTS
3.1. Clinical features of patients
Twenty‐two patients with substantial loss of maxillary/midfacial substance and edentulism in the remaining maxillae were eligible to participate in this cross‐sectional study. Nineteen patients agreed to participate, two patients rejected the invitation, and one patient did not respond. The medical history and demographic data of the 11 men (57.9%) and eight women (42.1%) are shown in Table 1. Regarding sex, age, reason for maxillectomy, adjuvant radiotherapy, and dental status in the lower jaw, no significant differences were found between the two patient groups. According to Brown's classification, the maxillary defects ranged from Ia to IId. Two patients only had a defect of the soft palate (SP), which is not included in Brown's classification. The defects in the group of patients with an implant‐supported obturator prosthesis were significantly larger and more ventral than the defects in the group with conventional obturator prostheses, making prosthetic rehabilitation more challenging (see also Table 1). On average, the patients with implant‐supported obturating prostheses were interviewed 3.8 years after prosthetic rehabilitation (range: 1 month–7.4 years), and 4.8 years (range: 4 months–8.7 years) in the conventional obturator group. Thirteen patients, five with implant‐supported prostheses and nine with conventional obturator prostheses, had a history of adjuvant radiotherapy (56–70 Gy) due to cancer treatment.
Table 1.
Demographic and clinical characteristics of patients with implant‐supported obturators and patients with conventional obturators
| Patient characteristics |
Implant‐supported obturators n = 9 |
Conventional obturators n = 10 |
p‐value |
|---|---|---|---|
| Gender (%) | |||
| Male | 7 (78%) | 4 (40%) | .170c |
| Female | 2 (22%) | 6 (60%) | |
| Age | |||
| 40–49 | 2 | 0 | |
| 50–59 | 2 | 1 | |
| 60–69 | 2 | 3 | .327a |
| 70–79 | 3 | 4 | |
| 80–89 | 0 | 2 | |
| Follow‐up time ( Mean ± SD) | 45.38 ± 34.67 | 57.09 ± 31.46 | .453b |
| Origin of maxillectomy | |||
| Gingival squamous cell carcinoma | 5 | 6 | |
| Polymorf lowgrade adenocarcinoma | 0 | 2 | |
| Adenoidcystic carcinoma | 1 | 1 | |
| Muco‐epidermoid carcinoma | 0 | 1 | .417a |
| Ameloblastoma | 1 | 0 | |
| Avascular necrosis after Le Fort I osteotomy | 1 | 0 | |
| Traumata | 1 | 0 | |
| Radiotherapy | 5 (56%) | 8 (80%) | .350c |
| Brown‐classification | |||
| Ia | 1 | 0 | |
| IIa | 0 | 3 | |
| IIb | 2 | 5 | .021a, * |
| IIc | 1 | 0 | |
| IId | 5 | 0 | |
| soft palate | 0 | 2 | |
| Dental status mandibular | |||
| Natural dentition | 3 | 1 | |
| Implant‐supported lower denture | 4 | 3 | .091 a |
| Conventional lower denture | 2 | 6 | |
Brown vertical classification. I: maxillectomy not causing an oronasal fistula; II: not involving the orbit. Brown horizontal classification. a: palatal defect only. not involving the dental alveolus; b: less than or equal to 1/2 unilateral; c: less than or equal to 1/2 bilateral or transverse anterior; d: greater than 1/2 maxillectomy. Soft palate not part of Browns classification with only a defect in the soft palate.
χ2‐test.
t Test.
Fisher's exact test.
p < .05.
In Group 1 (nine patients), the mean age was 64 years (range 47–78). Four of these patients received implants in the remaining parts of the maxilla; one patient received implants after bone‐augmentation. In the remaining five cases, no viable maxillary structure was left for implant placement. These patients received implants in the remaining bone structures useful for implantation, such as the pterygoid bone, the zygomatic bone, or the paranasal pillars of the nasal aperture. In total, 42 implants were placed to support the obturator prostheses, of which four were lost in a total of three patients. Three implants were lost before loading due to lack of osseointegration; the fourth showed good osseointegration but was lost 3 years after loading. These patients had undergone radiation treatment: two after implant placement, and one before implant placement. In three patients of Group 1, the natural dentition in the lower jaw was preserved. In four of the remaining six patients, the lower jaw dentures were implant‐retained.
Ten patients with a mean age of 71 years (range 59–85) were treated with conventional obturator prostheses (Group 2). A partial natural dentition was preserved in the lower jaw in only one patient of Group 2. In three of the remaining nine patients, the lower jaw dentures were implant‐retained.
3.2. Quality of life related to masticatory performance
The Shapiro–Wilk test showed a non‐normal distribution of the MAT outcomes; therefore, the Mann–Whitney U test was used.
Patients with an implant‐supported obturator prosthesis had a significantly better MAI score (18.66 ± 1.37) than patients with conventional prostheses (22.36 ± 3.16; p = .015). Thereby, the subdomain of ‘chewing difficulty’ showed better results in patients with an implant‐supported obturator in both the OHIP‐EDENT (p = .001; Table 2) and OFS (p = .007; Table 3). The subdomain of ‘eating comfort’ of the OHIP‐EDENT also showed a significantly better eating comfort in patients with an implant‐supported prosthesis (p = .026). Likewise, the domain of ‘oral functioning’ of the LORQv3‐NL was better in patients with an implant‐supported obturator prosthesis (p = .030; Table 4). The difficulties in swallowing solids are noteworthy. The results were worse in patients wearing conventional obturator prostheses in comparison to those with implant‐supported devices (LORQv3‐NL; p = .000). Voice modifications were more obvious in patients of Group 2 (OFS; p = .034).
Table 2.
OHIP‐EDENT scores of patients with implant‐supported obturators and patients with conventional obturators
| Item No | Description | Implant‐supported obturators | Conventional obturators | p‐value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | |||
| Functional limitation | ||||||
| 1 | Difficulty chewing | 2.00 ± 0.71 | 2.00 | 3.40 ± 0.70 | 3.00 | .001** |
| 2 | Food catching | 3.44 ± 1.33 | 4.00 | 3.40 ± 1.17 | 3.00 | .799 |
| 3 | Dentures not fitting | 1.78 ± 0.83 | 2.00 | 2.00 ± 0.94 | 2.00 | .601 |
| Subtotal | 7.22 ± 2.17 | 7.00 | 8.80 ± 1.93 | 9.00 | .115 | |
| Physical pain | ||||||
| 4 | Painful aching | 2.22 ± 1.48 | 2.00 | 2.45 ± 1.26 | 2.25 | .612 |
| 5 | Uncomfortable to eat | 2.11 ± 1.17 | 2.00 | 3.40 ± 0.97 | 3.50 | .026* |
| 6 | Sore spots | 2.22 ± 1.30 | 2.00 | 1.70 ± 1.06 | 1.00 | .295 |
| 7 | Uncomfortable dentures | 1.44 ± 0.53 | 1.00 | 1.40 ± 0.52 | 1.00 | .849 |
| Subtotal | 8.00 ± 3.57 | 8.00 | 8.95 ± 2.71 | 9.50 | .412 | |
| Psychological discomfort | ||||||
| 8 | Worried | 1.44 ± 0.73 | 1.00 | 1.50 ± 0.85 | 1.00 | 1.000 |
| 9 | Self‐conscious | 2.22 ± 1.64 | 2.00 | 2.60 ± 1.27 | 3.00 | .473 |
| Subtotal | 3.67 ± 2.24 | 3.00 | 4.10 ± 1.52 | 4.00 | .297 | |
| Physical disability | ||||||
| 10 | Avoid eating | 3.00 ± 1.12 | 3.00 | 3.60 ± 1.17 | 4.00 | .247 |
| 11 | Unable to eat | 1.67 ± 1.00 | 1.00 | 1.80 ± 0.79 | 2.00 | .534 |
| 12 | Interrupt meals | 1.33 ± 0.71 | 1.00 | 1.70 ± 0.82 | 1.50 | .254 |
| Subtotal | 6.00 ± 2.45 | 6.00 | 7.10 ± 2.13 | 7.50 | .233 | |
| Psychological disability | ||||||
| 13 | Upset | 1.78 ± 1.30 | 1.00 | 1.80 ± 1.23 | 1.00 | .927 |
| 14 | Been embarrassed | 1.89 ± 1.36 | 1.00 | 1.80 ± 1.14 | 1.00 | .927 |
| Subtotal | 3.67 ± 2.60 | 3.00 | 3.60 ± 2.01 | 3.00 | .931 | |
| Social disability | ||||||
| 15 | Avoid going out | 1.44 ± 0.73 | 1.00 | 2.10 ± 1.37 | 1.50 | .314 |
| 16 | Less tolerant of others | 1.67 ± 1.12 | 1.00 | 1.30 ± 0.68 | 1.00 | .460 |
| 17 | Irritable with others | 1.67 ± 1.12 | 1.00 | 1.80 ± 0.92 | 1.50 | .614 |
| Subtotal | 4.78 ± 2.77 | 3.00 | 5.20 ± 1.75 | 5.00 | .293 | |
| Handicap | ||||||
| 18 | Unable to enjoy company | 1.56 ± 0.88 | 1.00 | 1.90 ± 1.20 | 1.00 | .567 |
| 19 | Life unsatisfying | 1.56 ± 1.33 | 1.00 | 1.70 ± 0.82 | 1.50 | .296 |
| Subtotal | 3.11 ± 2.03 | 2.00 | 3.60 ± 1.84 | 3.00 | .376 | |
| Total | 36.44 ± 13.79 | 31.00 | 41.35 ± 9.16 | 43.25 | .253 | |
p < .05.
p < .01.
Table 3.
OFS‐scores of patients with implant‐supported obturators and patients with conventional obturators
| Item No | Description | Implant‐supported obturators | Conventional obturators | p | ||
|---|---|---|---|---|---|---|
| Mean | Median | Mean | Median | |||
| Eating problems | ||||||
| 1 | Difficulty in chewing food | 1.67 ± 0.87 | 1.00 | 3.00 ± 0.82 | 3.00 | .007** |
| 2 | Leakage when swallowing liquids | 3.11 ± 1.36 | 3.00 | 3.60 ± 1.08 | 4.00 | .446 |
| 3 | Leakage when swallowing food | 2.44 ± 1.24 | 3.00 | 2.10 ± 1.37 | 2.00 | .497 |
| Subtotal | 7.22 ± 2.68 | 8.00 | 8.70 ± 2.41 | 9.00 | .323 | |
| Speech problems | ||||||
| 4 | Voice different from before surgery | 1.89 ± 1.76 | 1.00 | 2.70 ± 0.82 | 2.50 | .034* |
| 5 | Difficulty in talking in public | 1.78 ± 1.56 | 1.00 | 2.20 ± 1.40 | 2.00 | .236 |
| 6 | Speech is nasal | 2.22 ± 1.48 | 2.00 | 2.60 ± 1.35 | 2.00 | .367 |
| 7 | Difficulty in pronouncing words | 1.89 ± 1.27 | 1.00 | 2.30 ± 1.25 | 2.00 | .367 |
| 8 | Speech is difficult to understand | 2.00 ± 1.50 | 1.00 | 1.80 ± 0.79 | 2.00 | .790 |
| Subtotal | 9.78 ± 6.55 | 6.00 | 11.60 ± 4.30 | 10.50 | .174 | |
| 9 | Mouth feels dry | 2.67 ± 1.58 | 2.00 | 1.90 ± 1.10 | 1.50 | .250 |
| 10 | Dissatisfaction with looks | 2.11 ± 1.54 | 1.00 | 1.50 ± 1.08 | 1.00 | .276 |
| 11 | Clasps on front teeth are noticeable | 2.11 ± 1.45 | 2.00 | 1.70 ± 0.95 | 1.00 | .563 |
| 12 | Upper lip feels numb | 1.56 ± 0.73 | 1.00 | 1.70 ± 1.25 | 1.00 | .899 |
| 13 | Avoidance of family/social events | 1.56 ± 1.13 | 1.00 | 1.40 ± 0.84 | 1.00 | .818 |
| 14 | Difficulty inserting obturator | 1.11 ± 0.33 | 1.00 | 1.50 ± 0.97 | 1.00 | .301 |
| 15 | Upper lip looks funny | 2.00 ± 1.41 | 1.00 | 1.30 ± 0.95 | 1.00 | .126 |
| Total | 30.11 ± 13.52 | 26.0 | 31.30 ± 6.40 | 30.0 | .413 | |
p < .05.
p < .01.
Table 4.
LORQv3‐NL scores of patients with implant‐supported obturators and patients with conventional obturators
| Item No | Description | Implant‐supported obturators | Conventional obturators | p‐value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | |||
| Chewing | ||||||
| 1 | Did you experience difficulty with chewing? | 1.67 ± 1.00 | 1.00 | 2.00 ± 0.67 | 2.00 | .183 |
| 2 | Did you have pain when you chew? | 1.33 ± 0.71 | 1.00 | 1.30 ± 0.48 | 1.00 | .832 |
| 16 | Did your chewing ability influence your choice of foods? | 1.78 ± 0.97 | 2.00 | 2.50 ± 1.18 | 2.00 | .153 |
| Subtotal | 4.78 ± 2.05 | 4.00 | 5.80 ± 1.81 | 6.00 | .199 | |
| Swallowing | ||||||
| 3 | Did you experience difficulty with swallowing solids? | 1.00 ± 0.00 | 1.00 | 2.30 ± 0.68 | 2.00 | .000*** |
| 4 | Did you experience difficulty with swallowing liquids? | 1.44 ± 0.73 | 1.00 | 1.70 ± 0.82 | 1.50 | .461 |
| Subtotal | 2.44 ± 0.73 | 2.00 | 4.00 ± 0.94 | 4.00 | .002** | |
| Salivation | ||||||
| 5 | Did food particles collect under your tongue? | 1.33 ± 0.50 | 1.00 | 2.00 ± 1.16 | 1.50 | .216 |
| 6 | Did food particles stick to your palate? | 1.56 ± 0.53 | 2.00 | 1.70 ± 0.68 | 2.00 | .678 |
| 7 | Did food particles stick inside your cheeks? | 1.78 ± 0.83 | 2.00 | 2.10 ± 1.37 | 1.50 | .793 |
| 8 | Did you have mouth dryness? | 2.33 ± 0.87 | 2.00 | 2.30 ± 0.95 | 2.00 | .965 |
| 9 | Did you have problems with drooling? | 1.56 ± 0.73 | 1.00 | 2.00 ± 1.33 | 1.00 | .648 |
| Subtotal | 8.56 ± 1.81 | 8.00 | 10.10 ± 2.85 | 9.50 | .282 | |
| 10 | Did you experience problems with speech? | 1.44 ± 1.01 | 1.00 | 2.00 ± 1.16 | 1.50 | .237 |
| 17 | Did you experience difficulty with opening your mouth? | 1.56 ± 1.01 | 1.00 | 2.30 ± 1.34 | 2.00 | .196 |
| Subtotal Oral function (1–10, 16, 17) | 18.78 ± 4.35 | 19.00 | 24.20 ± 5.25 | 22.50 | .030* | |
| Orofacial appearance | ||||||
| 11 | Were you upset by your facial appearance? | 1.44 ± 1.01 | 1.00 | 1.10 ± 0.32 | 1.00 | .440 |
| 12 | Were you upset by the appearance of your mouth? | 1.56 ± 1.01 | 1.00 | 1.20 ± 0.42 | 1.00 | .458 |
| 13 | Were you upset by the appearance of your lips? | 1.44 ± 1.01 | 1.00 | 1.00 ± 0.00 | 1.00 | .126 |
| 14 | Were you upset by the appearance of your teeth? | 1.33 ± 0.71 | 1.00 | 1.00 ± 0.00 | 1.00 | .126 |
| Subtotal | 5.78 ± 3.56 | 4.00 | 4.30 ± 0.68 | 4.00 | .215 | |
| Social interaction | ||||||
| 15 | Did your chewing ability affect your social life? | 1.33 ± 1.00 | 1.00 | 2.00 ± 1.05 | 2.00 | .065 |
| Total (1–17) | 25.89 ± 8.37 | 25.00 | 30.50 ± 5.91 | 29.0 | .078 | |
| Patient satisfaction | ||||||
| 20 | Were you embarrassed about conversing because of your dentures/implant‐retained teeth? | 1.33 ± 0.71 | 1.00 | 1.20 ± 0.63 | 1.00 | .530 |
| 21 | Did you refuse dinner invitations because of embarrassment about your dentures/implant‐retained teeth? |
1.22 ± 0.67 | 1.00 | 1.70 ± 1.06 | 1.00 | .187 |
| 22 | Did you feel loss of self‐confidence because of embarrassment about your dentures/implant‐retained teeth? | 1.44 ± 1.01 | 1.00 | 1.20 ± 0.42 | 1.00 | .818 |
| 23 | Did you find it difficult to open your mouth because of your dentures/implant‐retained teeth? | 1.11 ± 0.33 | 1.00 | 2.20 ± 1.23 | 2.00 | .023* |
| Subtotal | 5.11 ± 2.32 | 4.00 | 6.30 ± 1.57 | 7.00 | .049* | |
| Maxillary prosthetic satisfaction | ||||||
| 26 | Were you dissatisfied with your upper denture/implant‐retained teeth? | 1.33 ± 1.00 | 1.00 | 1.10 ± 0.32 | 1.00 | .878 |
| 27 | Did you upper denture/implant‐retained teeth cause soreness or ulceration of the gum? | 1.11 ± 0.33 | 1.00 | 1.40 ± 0.52 | 1.00 | .165 |
| 28 | Did you find food particles collecting under your upper denture/implant‐retained teeth? | 2.33 ± 0.87 | 2.00 | 1.70 ± 0.68 | 2.00 | .098 |
| 29 | Did you take out your upper denture/implant‐retained teeth for eating? | 1.00 ± 0.00 | 1.00 | 1.00 ± 0.00 | 1.00 | 1.000 |
| 30 | Did you feel insecure with your upper denture/implant‐retained teeth? | 1.44 ± 1.01 | 1.00 | 1.10 ± 0.32 | 1.00 | .440 |
| 31 | Were you worried that your upper denture/implant‐retained teeth might fall out? | 1.22 ± 0.67 | 1.00 | 1.20 ± 0.42 | 1.00 | .699 |
| Subtotal | 8.44 ± 2.65 | 8.00 | 7.50 ± 0.97 | 7.00 | .493 | |
| Mandibular prosthetic satisfaction | ||||||
| 34 | Were you dissatisfied with your lower denture/implant‐retained teeth? | 1.17 ± 0.41 | 1.00 | 1.11 ± 0.33 | 1.00 | .765 |
| 35 | Did your lower denture/implant‐retained teeth cause soreness or ulceration of the gum? | 1.17 ± 0.41 | 1.00 | 1.22 ± 0.44 | 1.00 | .799 |
| 36 | Did you find food particles collecting under your lower denture/implant‐retained teeth? | 1.50 ± 0.55 | 1.50 | 2.00 ± 0.87 | 2.00 | .255 |
| 37 | Did you take out your lower denture/implant‐retained teeth for eating? | 1.17 ± 0.41 | 1.00 | 1.67 ± 1.32 | 1.00 | .673 |
| 38 | Did you feel insecure with your lower denture/implant‐retained teeth? | 1.00 ± 0.00 | 1.00 | 1.44 ± 1.01 | 1.00 | .232 |
| 39 | Were you worried that your lower denture/implant‐retained teeth might fall out? | 1.00 ± 0.00 | 1.00 | 1.56 ± 1.01 | 1.00 | .129 |
| Subtotal | 7.00 ± 0.89 | 7.00 | 9.00 ± 4.06 | 8.00 | .276 | |
p < .05.
p < .01.
p < .001.
3.3. Post hoc power calculation
We computed the sample size given α = .05, power = 0.8, and the expected effect size for two independent means (matched pairs) with the MAI score outcomes of this study. The mean MAI score was 18.66 (±3.16) for the patients with implant‐supported obturator prostheses and 22.36 (±1.37) for the patients with conventional obturators. Therefore, the required sample size was estimated at 16 subjects (eight per group).
4. DISCUSSION
In this cross‐sectional comparative study, we explored whether implant‐supported obturator prostheses in maxillectomy patients improved masticatory performance and OHRQoL. Therefore, we evaluated both objective outcomes from the MAT and subjective outcomes from the OHRQoL questionnaires, as objective information of oral functioning may be different from personal experiences. The MAT evaluates the ability to mix a bi‐coloured wax tablet and results in the MAI score. It has proven to be a valid and reliable in test candidates with compromised masticatory performance (Remijn, Vermaire, Nijhuis‐van de Sanden, Groen, & Speksnijder, 2018; Speksnijder et al., 2009).
The study indicates that implant‐supported obturator prostheses are useful in the oral functional rehabilitation of maxillectomy patients. The results show a significantly better MAI score outcome in patients of Group 1, notwithstanding the larger and more ventral defects. The patients with implant‐supported obturator prostheses show similar MAI score results (18.66 ± 1.37) compared with dentate obturator patients (18.4 ± 4.2) despite severely compromised oral function due to the maxillectomy. Likewise, healthy edentulous non‐maxillectomy individuals with conventional maxillary dentures and implant‐supported mandibular overdentures (MAI 18.5 ± 3.1) have shown similar results. The mean MAI score of Group 2 patients (22.36 ± 3.16) was comparable to healthy full denture patients (21.2 ± 3.6) and other edentulous obturator patients (25.1 ± 5.3) (Kreeft et al., 2012; Speksnijder et al., 2009).
The added value of dental implants in prosthetic rehabilitation of patients after maxillectomy has been reported previously, both in patients receiving obturator prostheses, as well as in surgically reconstructed patients. The use of zygomatic implants increases reconstructive treatment options, especially for maxillectomy patients. To date, functional differences have not been established between the obturator and surgically reconstructed patients (Breeze et al., 2016; Landes et al., 2009; Wang et al., 2017).
We reached an overall implant survival of 90.5%, with four out of 42 implants lost in patients in Group 1. Since the four lost implants have failed in irradiated bone, our overall implant survival in non‐irradiated bone of 100% is comparable with the results published by Huang et al. (2014). In their study, implant survival in irradiated patients was 82.6%. Other studies have reported similar results; however, these studies did not refer to dental implant survival in extra‐maxillary bony structures of the midface or skull base (Chambrone, Mandia, Shibli, Romito, & Abrahao, 2013; Schiegnitz, Al‐Nawas, Kammerer, & Grotz, 2014; Shugaa‐Addin, Al‐Shamiri, Al‐Maweri, & Tarakji, 2016). Moreover, current literature does not explicitly reveal information about the radiation doses at the specific implant sites. Instead, studies have reported whether the patient was irradiated or not. In our study, the implant sites of the lost implants had been irradiated with more than 50 Gy. Nevertheless, the patients could continue to wear their prosthetic obturators despite singular implant loss, which we considered a successful overall result of functional rehabilitation.
In addition to objective results such as MAI scores, functional aspects must be assessed subjectively using the OHRQoL. The OHIP‐EDENT is a modified shorted version of the OHIP‐49 questionnaire which, in contrast to the more commonly used OHIP‐14, includes items related to chewing and denture problems (Allen & Locker, 2002). The OHIP‐EDENT showed significantly better results after implant‐retained prosthetic rehabilitation in a study on five edentulous hemi‐maxillectomy patients (Mertens, de San Jose Gonzalez, et al., 2016).
The Memorial Sloan Kettering Cancer Centre Obturator Functioning Scale (OFS) has proven to be a viable questionnaire to assess self‐reported obturator functioning and to predict quality of life in maxillectomy patients (Irish et al., 2009; Kornblith et al., 1996; Riaz & Warriach, 2010). It has shown the negative impact of (adjuvant) radiotherapy (Chen, Ren, Gao, et al., 2016; Chen, Ren, Huang, et al., 2016; Chigurupati, Aloor, Salas, & Schmidt, 2013; Riaz & Warriach, 2010) and defect size on obturator functioning (Chen, Ren, Huang, et al., 2016; Kreeft et al., 2012).
The LORQv3 is a health‐related questionnaire assessing the impact of oral rehabilitation on patients' OHRQoL (Pace‐Balzan et al., 2008, 2009, 2004). It has recently been translated and validated into the Dutch language, resulting in the LORQv3‐NL (Engelen et al., 2017). This questionnaire has shown the added value of prosthetic rehabilitation in improving HRQoL of patients treated for head and neck cancer, including maxillectomy patients rehabilitated with obturator prostheses (Dholam, Chouksey, & Dugad, 2016; Dholam, Dugad, & Sadashiva, 2017; Peker et al., 2014).
Our OHIP‐EDENT, OFS, and LORQv3‐NL results did not disclose significant differences in summary scales between the two patient groups. This is probably due to the long‐time interval between prosthetic rehabilitation and data acquisition (range: 1 month–7.4 years). Patients tend to adapt over time and under‐report deficits, also called response shifts (Rogers, Lowe, McNally, Brown, & Vaughan, 2003).
On the subscale level, the ‘Oral function’ subscale and the ‘Patient Satisfaction’ subscale of the LORQv3‐NL showed that implant retainment has an added value for the obturator prostheses. Although these benefits are underlined in response choices by all three questionnaires, the small patient groups should be considered. The same carefully interpretation should be applied for the promising results in the speaking and swallowing domains, which have proven to be important for quality of life (Irish et al., 2009; Kornblith et al., 1996).
There are benefits for microsurgical reconstruction of extended maxillary and midface defects. Patients requiring adjuvant radiotherapy will take advantage of reconstructive surgery, as the risk of post‐radiogenic changes in the irradiated tissues will be less pronounced. Tissue atrophy, fibrosis, and the most feared risk of osteoradionecrosis can be prevented by vascularized tissue transfer into the defect site. Moreover, surgical defect repair can lead to aesthetic benefits, and implant‐retained fixed dentures can be applied. However, risks, as well as costs of reconstructive surgery, should not be underestimated. For class IIb and smaller defects, very good results can be achieved by either prosthetic obturation or surgical reconstruction (Brown & Shaw, 2010). Our results endorse the previously mentioned advantages of implant‐supported prosthetic rehabilitation, especially in (a) preventing donor site morbidity, (b) surgical risks, and (c) longer hospitalization needed for a vascularized flap transfer (Boyes‐Varley, Howes, Davidge‐Pitts, Branemark, & McAlpine, 2007). The overall treatment time until adequate prosthetic rehabilitation is achieved is much shorter in prosthetic obturation. In oncologic cases, the inspection of the resection defect offers advantages during the follow‐up.
4.1. Strengths and limitations
To our knowledge, this is the first study to objectively examine masticatory performance in patients rehabilitated with implant‐supported obturator prostheses in comparison to conventional prosthetic devices. Moreover, patient‐reported OHRQoL‐results appear to support the objective results of this study. The inclusion of only edentulous maxillectomy patients has the advantage of eliminating the bias of residual dentition, which has proven to be beneficial for masticatory performance (Chen, Ren, Gao, et al., 2016; Kreeft et al., 2012; Matsuyama, Tsukiyama, Tomioka, & Koyano, 2006; Vero et al., 2015; Wedel, Yontchev, Carlsson, & Ow, 1994).
Limitations are the cross‐sectional study design, the small population, the inhomogeneous anamnesis, and the wide time span between prosthetic rehabilitation and data acquisition. Although patients in Group 1 had a mean follow‐up time of 4.8 years, only four out of these nine patients had a follow‐up of more than 5 years. Quality of life 1 year after surgery has been shown to be a good indicator of long‐term quality of life (Rogers, Hannah, Lowe, & Magennis, 1999). Implant survival rates, however, ask for a minimum of 5 years, and preferably 10 years, of follow‐up (Huang et al., 2014; Korfage et al., 2010; Schiegnitz et al., 2014; Wetzels et al., 2017).
4.2. Future research
Long‐term longitudinal prospective research with a larger number of participants is required, as well as objective measurements of speech and swallowing. Comparison of functional outcomes and HRQoL after prosthetic obturation, preferably implant‐supported, with surgical reconstruction would give support in the individual decision making for maxillectomy patients.
4.3. Conclusion
Implant‐supported prosthetic obturation after maxillectomy appears to improve chewing ability, oral functioning, and patient satisfaction. More research is needed to confirm the advantages in speech and swallowing after implant‐supported prosthetic obturation. This treatment modality is a viable alternative to surgical reconstruction after maxillectomy, especially in medically compromised and older patients. If implant placement is possible in maxillectomy patients, implant‐retained obturator prostheses should be preferred.
AUTHOR CONTRIBUTIONS
DB, BE and PK conceived the ideas; BE collected the data; DB and CS analysed the data; and DB, CS and PK led the writing.
Supporting information
Buurman DJM, Speksnijder CM, Engelen BHBT, Kessler P. Masticatory performance and oral health‐related quality of life in edentulous maxillectomy patients: A cross‐sectional study to compare implant‐supported obturators and conventional obturators. Clin Oral Impl Res. 2020;31:405–416. 10.1111/clr.13577
REFERENCES
- Allen, F. , & Locker, D. (2002). A modified short version of the oral health impact profile for assessing health‐related quality of life in edentulous adults. The International Journal of Prosthodontics, 15(5), 446–450. [PubMed] [Google Scholar]
- Andrades, P. , Militsakh, O. , Hanasono, M. M. , Rieger, J. , & Rosenthal, E. L. (2011). Current strategies in reconstruction of maxillectomy defects. Archives of Otolaryngology ‐ Head and Neck Surgery, 137(8), 806–812. 10.1001/archoto.2011.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyes‐Varley, J. G. , Howes, D. G. , Davidge‐Pitts, K. D. , Branemark, I. , & McAlpine, J. A. (2007). A protocol for maxillary reconstruction following oncology resection using zygomatic implants. The International Journal of Prosthodontics, 20(5), 521–531. [PubMed] [Google Scholar]
- Breeze, J. , Rennie, A. , Morrison, A. , Dawson, D. , Tipper, J. , Rehman, K. , … Pigadas, N. (2016). Health‐related quality of life after maxillectomy: Obturator rehabilitation compared with flap reconstruction. British Journal of Oral and Maxillofacial Surgery, 54(8), 857–862. 10.1016/j.bjoms.2016.05.024 [DOI] [PubMed] [Google Scholar]
- Brown, J. , Schache, A. , & Butterworth, C. (2016). Liverpool opinion on unfavorable results in microsurgical head and neck reconstruction: Lessons learned. Clinics in Plastic Surgery, 43(4), 707–718. 10.1016/j.cps.2016.05.007 [DOI] [PubMed] [Google Scholar]
- Brown, J. S. , & Shaw, R. J. (2010). Reconstruction of the maxilla and midface: Introducing a new classification. The Lancet Oncology, 11(10), 1001–1008. 10.1016/S1470-2045(10)70113-3 [DOI] [PubMed] [Google Scholar]
- Chambrone, L. , Mandia Jr, J. , Shibli, J. A. , Romito, G. A. , & Abrahao, M. (2013). Dental implants installed in irradiated jaws: A systematic review. Journal of Dental Research, 92(12. Suppl), 119S–130S. 10.1177/0022034513504947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, C. , Ren, W. , Gao, L. , Cheng, Z. , Zhang, L. , Li, S. , & Zhi, P. K. (2016). Function of obturator prosthesis after maxillectomy and prosthetic obturator rehabilitation. Brazilian Journal of Otorhinolaryngology, 82(2), 177–183. 10.1016/j.bjorl.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, C. , Ren, W.‐H. , Huang, R.‐Z. , Gao, L. , Hu, Z.‐P. , Zhang, L.‐M. , … Zhi, K.‐Q. (2016). Quality of life in patients after maxillectomy and placement of prosthetic obturator. The International Journal of Prosthodontics, 29(4), 363–368. 10.11607/ijp.4608 [DOI] [PubMed] [Google Scholar]
- Chigurupati, R. , Aloor, N. , Salas, R. , & Schmidt, B. L. (2013). Quality of life after maxillectomy and prosthetic obturator rehabilitation. Journal of Oral and Maxillofacial Surgery, 71(8), 1471–1478. 10.1016/j.joms.2013.02.002 [DOI] [PubMed] [Google Scholar]
- Depprich, R. , Naujoks, C. , Lind, D. , Ommerborn, M. , Meyer, U. , Kubler, N. R. , & Handschel, J. (2011). Evaluation of the quality of life of patients with maxillofacial defects after prosthodontic therapy with obturator prostheses. International Journal of Oral and Maxillofacial Surgery, 40(1), 71–79. 10.1016/j.ijom.2010.09.019 [DOI] [PubMed] [Google Scholar]
- Dholam, K. P. , Chouksey, G. C. , & Dugad, J. (2016). Oral health‐related quality of life after prosthetic rehabilitation in patients with oral cancer: A longitudinal study with the liverpool oral rehabilitation questionnaire version 3 and oral health impact profile‐14 questionnaire. Indian Journal of Cancer, 53(2), 256–260. 10.4103/0019-509X.197716 [DOI] [PubMed] [Google Scholar]
- Dholam, K. P. , Dugad, J. A. , & Sadashiva, K. M. (2017). Impact of oral rehabilitation on patients with head and neck cancer: A study using the liverpool oral rehabilitation questionnaire and the oral health impact profile‐14. Journal of Prosthetic Dentistry, 117(4), 559–562. 10.1016/j.prosdent.2016.06.019 [DOI] [PubMed] [Google Scholar]
- Engelen, M. , Buurman, D. J. M. , Bronkhorst, E. M. , & van Heumen, C. C. M. (2017). Translation, cross‐cultural adaptation, and validation of the liverpool oral rehabilitation questionnaire (LORQ) into the Dutch language. Journal of Prosthetic Dentistry, 10.1016/j.prosdent.2017.03.023 [DOI] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Buchner, A. , & Lang, A. G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Lang, A. G. , & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Goiato, M. C. , Pellizzer, E. P. , Moreno, A. , Gennari‐Filho, H. , dos Santos, D. M. , Santiago Jr, J. F. , & dos Santos, E. G. (2014). Implants in the zygomatic bone for maxillary prosthetic rehabilitation: A systematic review. International Journal of Oral and Maxillofacial Surgery, 43(6), 748–757. 10.1016/j.ijom.2014.01.004 [DOI] [PubMed] [Google Scholar]
- He, S. L. , & Wang, J. H. (2015). Reliability and validity of a Chinese version of the oral health impact profile for edentulous subjects. Quality of Life Research, 24(4), 1011–1016. 10.1007/s11136-014-0822-5 [DOI] [PubMed] [Google Scholar]
- Huang, W. , Wu, Y. , Zou, D. , Zhang, Z. , Zhang, C. , Sun, J. , … Zhang, Z. (2014). Long‐term results for maxillary rehabilitation with dental implants after tumor resection. Clinical Implant Dentistry and Related Research, 16(2), 282–291. 10.1111/j.1708-8208.2012.00481.x [DOI] [PubMed] [Google Scholar]
- Irish, J. , Sandhu, N. , Simpson, C. , Wood, R. , Gilbert, R. , Gullane, P. , … Barker, E. (2009). Quality of life in patients with maxillectomy prostheses. Head and Neck, 31(6), 813–821. 10.1002/hed.21042 [DOI] [PubMed] [Google Scholar]
- Korfage, A. , Schoen, P. J. , Raghoebar, G. M. , Roodenburg, J. L. , Vissink, A. , & Reintsema, H. (2010). Benefits of dental implants installed during ablative tumour surgery in oral cancer patients: A prospective 5‐year clinical trial. Clinical Oral Implants Research, 21(9), 971–979. 10.1111/j.1600-0501.2010.01930.x [DOI] [PubMed] [Google Scholar]
- Kornblith, A. B. , Zlotolow, I. M. , Gooen, J. , Huryn, J. M. , Lerner, T. , Strong, E. W. , … Holland, J. C. (1996). Quality of life of maxillectomy patients using an obturator prosthesis. Head and Neck, 18(4), 323–334. [DOI] [PubMed] [Google Scholar]
- Kreeft, A. M. , Krap, M. , Wismeijer, D. , Speksnijder, C. M. , Smeele, L. E. , Bosch, S. D. , … Balm, A. J. (2012). Oral function after maxillectomy and reconstruction with an obturator. International Journal of Oral and Maxillofacial Surgery, 41(11), 1387–1392. 10.1016/j.ijom.2012.07.014 [DOI] [PubMed] [Google Scholar]
- Landes, C. A. (2005). Zygoma implant‐supported midfacial prosthetic rehabilitation: A 4‐year follow‐up study including assessment of quality of life. Clinical Oral Implants Research, 16(3), 313–325. 10.1111/j.1600-0501.2005.01096.x [DOI] [PubMed] [Google Scholar]
- Landes, C. A. , Paffrath, C. , Koehler, C. , Thai, V. D. , Stubinger, S. , Sader, R. , … Piwowarczyk, A. (2009). Zygoma implants for midfacial prosthetic rehabilitation using telescopes: 9‐year follow‐up. The International Journal of Prosthodontics, 22(1), 20–32. [PubMed] [Google Scholar]
- Lethaus, B. , Kessler, P. , Boeckman, R. , Poort, L. J. , & Tolba, R. (2010). Reconstruction of a maxillary defect with a fibula graft and titanium mesh using CAD/CAM techniques. Head & Face Medicine, 6(1), 16 10.1186/1746-160X-6-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lethaus, B. , Lie, N. , de Beer, F. , Kessler, P. , de Baat, C. , & Verdonck, H. W. (2010). Surgical and prosthetic reconsiderations in patients with maxillectomy. Journal of Oral Rehabilitation, 37(2), 138–142. 10.1111/j.1365-2842.2009.02031.x [DOI] [PubMed] [Google Scholar]
- Matsuyama, M. , Tsukiyama, Y. , Tomioka, M. , & Koyano, K. (2006). Clinical assessment of chewing function of obturator prosthesis wearers by objective measurement of masticatory performance and maximum occlusal force. The International Journal of Prosthodontics, 19(3), 253–257. [PubMed] [Google Scholar]
- Mertens, C. , de San Jose Gonzalez, J. , Freudlsperger, C. , Bodem, J. , Krisam, J. , Hoffmann, J. , & Engel, M. (2016). Implant‐prosthetic rehabilitation of hemimaxillectomy defects with CAD/CAM suprastructures. Journal of Cranio‐Maxillo‐Facial Surgery, 44(11), 1812–1818. 10.1016/j.jcms.2016.08.009 [DOI] [PubMed] [Google Scholar]
- Mertens, C. , Freudlsperger, C. , Bodem, J. , Engel, M. , Hoffmann, J. , & Freier, K. (2016). Reconstruction of the maxilla following hemimaxillectomy defects with scapular tip grafts and dental implants. Journal of Cranio‐Maxillo‐Facial Surgery, 44(11), 1806–1811. 10.1016/j.jcms.2016.08.010 [DOI] [PubMed] [Google Scholar]
- Pace‐Balzan, A. , Butterworth, C. J. , Dawson, L. J. , Lowe, D. , & Rogers, S. N. (2008). The further development and validation of the Liverpool Oral Rehabilitation Questionnaire (LORQ) version 3: A cross‐sectional survey of patients referred to a dental hospital for removable prostheses replacement. Journal of Prosthetic Dentistry, 99(3), 233–242. 10.1016/S0022-3913(08)60048-7 [DOI] [PubMed] [Google Scholar]
- Pace‐Balzan, A. , Butterworth, C. , Lowe, D. , & Rogers, S. N. (2009). The responsiveness of the liverpool oral rehabilitation questionnaire (LORQ): A pilot study. The International Journal of Prosthodontics, 22(5), 456–458. [PubMed] [Google Scholar]
- Pace‐Balzan, A. , Cawood, J. I. , Howell, R. , Lowe, D. , & Rogers, S. N. (2004). The liverpool oral rehabilitation questionnaire: A pilot study. Journal of Oral Rehabilitation, 31(6), 609–617. 10.1111/j.1365-2842.2004.01279.x [DOI] [PubMed] [Google Scholar]
- Peker, K. , Ozdemir‐Karatas, M. , Balik, A. , Kurklu, E. , Uysal, O. , & Rogers, S. N. (2014). Validation of the Turkish version of the Liverpool Oral Rehabilitation Questionnaire version 3 (LORQv3) in prosthetically rehabilitated patients with head and neck cancer. BMC Oral Health, 14, 129 10.1186/1472-6831-14-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remijn, L. , Vermaire, J. A. , Nijhuis‐van de Sanden, M. W. G. , Groen, B. E. , & Speksnijder, C. M. (2018). Validity and reliability of the mixing ability test as masticatory performance outcome in children with spastic cerebral palsy and children with typical development: A pilot study. Journal of Oral Rehabilitation, 45(10), 790–797. 10.1111/joor.12690 [DOI] [PubMed] [Google Scholar]
- Riaz, N. , & Warriach, R. A. (2010). Quality of life in patients with obturator prostheses. Journal of Ayub Medical College, Abbottabad, 22(2), 121–125. [PubMed] [Google Scholar]
- Rogers, S. N. , Hannah, L. , Lowe, D. , & Magennis, P. (1999). Quality of life 5–10 years after primary surgery for oral and oro‐pharyngeal cancer. Journal of Cranio‐Maxillo‐Facial Surgery, 27(3), 187–191. 10.1016/S1010-5182(99)80049-3 [DOI] [PubMed] [Google Scholar]
- Rogers, S. N. , Lowe, D. , McNally, D. , Brown, J. S. , & Vaughan, E. D. (2003). Health‐related quality of life after maxillectomy: A comparison between prosthetic obturation and free flap. Journal of Oral and Maxillofacial Surgery, 61(2), 174–181. 10.1053/joms.2003.50044 [DOI] [PubMed] [Google Scholar]
- Santamaria, E. , & Cordeiro, P. G. (2006). Reconstruction of maxillectomy and midfacial defects with free tissue transfer. Journal of Surgical Oncology, 94(6), 522–531. 10.1002/jso.20490 [DOI] [PubMed] [Google Scholar]
- Sato, Y. , Kaiba, Y. , Yamaga, E. , & Minakuchi, S. (2012). Reliability and validity of a Japanese version of the oral health impact profile for edentulous subjects. Gerodontology, 29(2), e1033–1037. 10.1111/j.1741-2358.2011.00606.x [DOI] [PubMed] [Google Scholar]
- Schiegnitz, E. , Al‐Nawas, B. , Kammerer, P. W. , & Grotz, K. A. (2014). Oral rehabilitation with dental implants in irradiated patients: A meta‐analysis on implant survival. Clinical Oral Investigations, 18(3), 687–698. 10.1007/s00784-013-1134-9 [DOI] [PubMed] [Google Scholar]
- Seignemartin, C. P. , Miranda, M. E. , Luz, J. G. , & Teixeira, R. G. (2015). Understandability of speech predicts quality of life among maxillectomy patients restored with obturator prosthesis. Journal of Oral and Maxillofacial Surgery, 73(10), 2040–2048. 10.1016/j.joms.2015.04.031 [DOI] [PubMed] [Google Scholar]
- Sharma, A. B. , & Beumer, J. 3rd (2005). Reconstruction of maxillary defects: The case for prosthetic rehabilitation. Journal of Oral and Maxillofacial Surgery, 63(12), 1770–1773. 10.1016/j.joms.2005.08.013 [DOI] [PubMed] [Google Scholar]
- Shugaa‐Addin, B. , Al‐Shamiri, H. M. , Al‐Maweri, S. , & Tarakji, B. (2016). The effect of radiotherapy on survival of dental implants in head and neck cancer patients. Journal of Clinical and Experimental Dentistry, 8(2), e194–e200. 10.4317/jced.52346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza, R. F. , Patrocinio, L. , Pero, A. C. , Marra, J. , & Compagnoni, M. A. (2007). Reliability and validation of a Brazilian version of the oral health impact profile for assessing edentulous subjects. Journal of Oral Rehabilitation, 34(11), 821–826. 10.1111/j.1365-2842.2007.01749.x [DOI] [PubMed] [Google Scholar]
- Speksnijder, C. M. , Abbink, J. H. , van der Glas, H. W. , Janssen, N. G. , & van der Bilt, A. (2009). Mixing ability test compared with a comminution test in persons with normal and compromised masticatory performance. European Journal of Oral Sciences, 117(5), 580–586. 10.1111/j.1600-0722.2009.00675.x [DOI] [PubMed] [Google Scholar]
- Triana Jr, R. J. , Uglesic, V. , Virag, M. , Varga, S. G. , Knezevic, P. , Milenovic, A. , … Futran, N. D. (2000). Microvascular free flap reconstructive options in patients with partial and total maxillectomy defects. Archives of Facial Plastic Surgery, 2(2), 91–101. 10.1001/archfaci.2.2.91 [DOI] [PubMed] [Google Scholar]
- Umino, S. , Masuda, G. , Ono, S. , & Fujita, K. (1998). Speech intelligibility following maxillectomy with and without a prosthesis: An analysis of 54 cases. Journal of Oral Rehabilitation, 25(2), 153–158. 10.1046/j.1365-2842.1998.00238.x [DOI] [PubMed] [Google Scholar]
- van der Bilt, A. , Speksnijder, C. M. , de Liz Pocztaruk, R. , & Abbink, J. H. (2012). Digital image processing versus visual assessment of chewed two‐colour wax in mixing ability tests. Journal of Oral Rehabilitation, 39(1), 11–17. 10.1111/j.1365-2842.2011.02229.x [DOI] [PubMed] [Google Scholar]
- Vero, N. , Mishra, N. , Singh, B. P. , Singh, K. , Jurel, S. K. , & Kumar, V. (2015). Assessment of swallowing and masticatory performance in obturator wearers: A clinical study. The Journal of Advanced Prosthodontics, 7(1), 8–14. 10.4047/jap.2015.7.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, F. , Huang, W. , Zhang, C. , Sun, J. , Qu, X. , & Wu, Y. (2017). Functional outcome and quality of life after a maxillectomy: A comparison between an implant supported obturator and implant supported fixed prostheses in a free vascularized flap. Clinical Oral Implants Research, 28(2), 137–143. 10.1111/clr.12771 [DOI] [PubMed] [Google Scholar]
- Wedel, A. , Yontchev, E. , Carlsson, G. E. , & Ow, R. (1994). Masticatory function in patients with congenital and acquired maxillofacial defects. Journal of Prosthetic Dentistry, 72(3), 303–308. 10.1016/0022-3913(94)90344-1 [DOI] [PubMed] [Google Scholar]
- Wetzels, J. G. H. , Meijer, G. J. , Koole, R. , Adang, E. M. , Merkx, M. A. W. , & Speksnijder, C. M. (2017). Costs and clinical outcomes of implant placement during ablative surgery and postponed implant placement in curative oral oncology: A five‐year retrospective cohort study. Clinical Oral Implants Research, 28(11), 1433–1442. 10.1111/clr.13008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


