Abstract
Patient: Female, 46-year-old
Final Diagnosis: Bowel perforation
Symptoms: Decreased level of consciousness
Medication: —
Clinical Procedure: Central venous catheterization
Specialty: Critical Care Medicine
Objective:
Unusual clinical course
Background:
Central venous catheter (CVC) insertion is commonly performed in the emergency department. The femoral vein is often chosen for insertion of CVCs due to its lower risk for complication. We present a rare complication of bowel puncture during insertion of a femoral CVC in the emergency department in a 46-year-old female.
Case Report:
A 46-year-old female with a history of partial gastrectomy and colostomy was transported to the emergency department after being found unconscious. Despite multiple attempts, intravenous access could not be obtained. The emergency physician proceeded to insert a left femoral CVC to obtain venous access. Ultrasound was not used due to perceived urgency, as well as a bedside assessment that the patient’s anatomy was straight forward. Stool-like material was aspirated upon inserting the introducer needle, which was quickly removed. An upright x-ray showed no free air, but due to the patient history, an exploratory laparotomy was performed. A single-side perforation in the mid-sigmoid with a small hematoma along the antimesenteric wall was found. The puncture was over sewn, and the patient recovered well; the patient’s initial presentation was ultimately considered to be due to medication misuse.
Conclusions:
This case highlights the importance of using caution in blind attempts at femoral CVC in patients with prior abdominal surgery. It is also important to note the need to avoid insertion of CVCs without the use of ultra-sound or when in a rush. If venous access is needed quickly, peripheral or intraosseous venous access can be obtained much more quickly and safely.
MeSH Keywords: Central Venous Catheters, Intestinal Perforation, Ultrasonography
Background
The insertion of central venous catheters (CVC) is a common procedure, with an estimated 5 million CVCs inserted annually in the United States [1]. CVCs are inserted in a variety of clinical settings, including in the emergency department during the care of critically ill patients. Common indications for insertion of CVCs in the emergency department include poor venous access, the requirement for infusions such as vasopressors that are not intended for prolonged peripheral administration, or the need for advanced therapies such as dialysis or cardiac pacing [2].
CVCs can be inserted in femoral, subclavian, or internal jugular veins, with each site having its own benefits and risks [3]. The femoral vein is often chosen as the site for insertion of CVCs in the emergency department due to its perceived benefits in emergency situations – benefits such as the ability to apply direct pressure to the insertion site in cases of coagulopathy or complication, relative ease of insertion in uncooperative patients compared to other sites, the ability to insert femoral lines without placing the patient in Trendelenburg position (which may be potentially harmful in patients with severe traumatic brain injury), or the ability to insert without interrupting cardiopulmonary resuscitation [4].
Despite the possible benefits of femoral CVCs in emergency situations, complications at the time of insertion, as well as after insertion may occur [5]. Vascular injuries, thrombosis, and infections are the most commonly cited complications of femoral CVCs. We report a case of bowel puncture during attempted insertion of femoral CVC in the emergency department that was recognized after aspiration of feces. The objective of this case report is to describe a rare complication of femoral CVC insertion, and outline possible risk factors and prevention strategies for this complication.
Case Report
A 46-year-old female was found by family members unconscious on her couch at home in the morning hours; she had been well the prior night. The patient was known to have a history of chronic obstructive pulmonary disease, fibromyalgia, celiac disease, migraines, depression, peptic ulcer disease, partial gastrectomy, and past colostomy that had since been reversed.
An ambulance was called, and on its arrival, paramedics found the patient to be unresponsive with a Glasgow Coma Scale (GCS) of 3. Additionally, the patient was found to have an oxygen saturation (SpO2) of 68% on room air, blood pressure 72/30 mmHg, heart rate (HR) of 88 beats per minute (bpm), respiratory rate 10 breaths per minute, and glucose 10.5 mmol/L. An 18-gauge intravenous (IV) needle was inserted in the left antecubital fossa and oxygen administered via 100% nonrebreather (NRB). Oxygen saturation improved only marginally to 78% with the 100% NRB, so the patient was intubated in the prehospital setting by paramedics with the administration of 5 mg of diazepam IV.
Upon arrival to the emergency department, the patient’s condition had improved with vital signs now showing a temperature 35.6°C, HR of 100 bpm BP 100/70 mmHg, and SpO2 of 100% with an FiO2 of 100%. The patient was placed on a ventilator with a volume control mode delivering a respiratory rate of 12 breaths per minute and tidal volume of 500 mL. Several attempts to obtain bloodwork and additional IV access were unsuccessful, so the decision was made to insert a femoral CVC to facilitate blood draws and medication administration.
Ultrasound was not used to guide CVC insertion due to the perceived sense of urgency to insert the line, and a feeling that the patient’s body habitus was conducive to easy insertion. The procedure was performed by a senior emergency physician. On insertion of the introducer needle stool-like material was aspirated. Due to concern regarding bowel puncture and possible perforation during femoral vein cannulation, the needle was quickly removed, and general surgery was consulted. An upright x-ray performed immediately after the CVC attempt showed no signs of free air (Figure 1).
Figure 1.
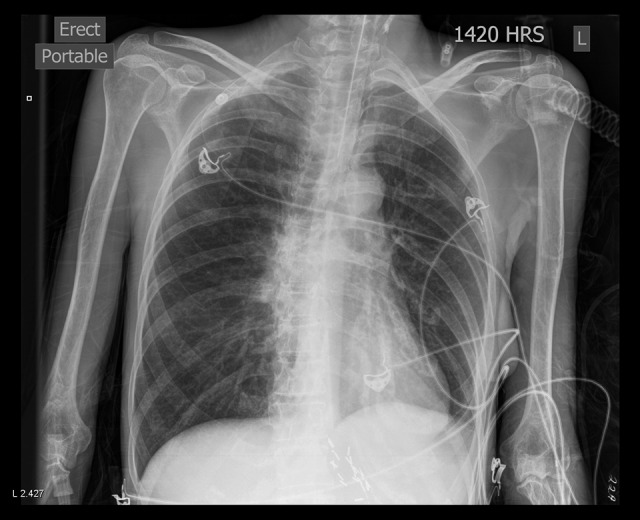
Upright x-ray performed after possible bowel puncture showing no signs of free air. Multiple surgical clips in the left upper quadrant are noted from prior gastrectomy.
General surgery opted to perform an exploratory laparotomy without further imaging given the patient’s instability and the possibility that there may have been a perforation prior to the CVC attempt accounting for both the patient’s presentation and the bowel contents in the needle. Intraoperatively, a single side perforation was observed in the mid-sigmoid with an associated small hematoma along the antimesenteric wall. The puncture site was over sewn with 3 interrupted Lembert sutures of 3-0 Vicryl. No other abnormal intra-abdominal pathology was found.
The patient was transferred to the intensive care unit (ICU) post-operatively where she recuperated well. After further history was obtained, medication misuse was identified as the most likely cause of the patient’s initial presentation.
Discussion
CVC is widely used in the emergency department for quick and sustained access to the bloodstream. In emergency situations, the femoral vein is often selected as the site for CVC insertion due to its ease of access and lower risk of vascular and mechanical complications.
This case report highlights a rare complication of bowel puncture resulting from CVC insertion in the femoral site in the emergency department. Several factors may have contributed to this complication that practitioners should be aware of and consider in their own patients.
The patient in this case had a history of prior abdominal surgeries likely resulting in abdominal adhesions. When abdominal adhesions result in the bowel being fixed to the peritoneum and abdominal wall, this leaves the bowel more susceptible to injury from surrounding procedures. While needle insertion should always occur distal to the inguinal ligament to avoid bowel injury, in patients with prior abdominal surgery, it is likely safer to start even more distal to the inguinal ligament than usual. Such an approach would also prove useful in the rare cases when a femoral hernia is present but undiagnosed (though that was not the case here).
This case report also highlights the importance of the use of ultrasound during CVC insertion. Use of ultrasound allows for the visualization of target vessels and surrounding structures, and has been shown to reduce complications and increase success [6]. In the reported case, forgoing the ultrasound in the interest of time resulted in severe morbidity. This demonstrates the necessity of ultrasound guidance for all patients, as high-risk features may still be present in those with a perceived ease of cannulation.
Most importantly, the case demonstrates the associated risks of rushing CVC insertion before exploring other modalities. Peripheral IV or intraosseous infusion is a safer and quicker approach for resuscitation. For instance, evidence supports the safety of peripheral delivery of caustic medications (i.e., vasopressors) for short periods of time. In this case, the physician’s hurried decision increased the risk for complications to ultimately result in bowel puncture and morbidity.
Conclusions
A case of bowel puncture during emergent femoral CVC insertion of a patient presenting normal anatomy (i.e., no femoral hernia) is presented. Several important lessons can be taken from this case report. First, this case emphasizes the importance of not inserting CVCs in a hurried manner. When venous access is needed urgently, peripheral IV access or IO approaches are faster and safer. Second, the importance of using ultrasound to identify the location of vessels and guide needle insertion for CVC insertion is demonstrated as abnormal anatomy may occur even in patients with no external signs of difficulty. Third, in patients with past abdominal surgeries, extra care should be taken as abdominal contents may be adhered to the abdominal wall making them more at risk for injury from surrounding procedures.
Acknowledgments
We would like to acknowledge the support of Joanna Giddens for their assistance in editing and writing the manuscript.
Footnotes
Conflicts of interest
None.
References:
- 1.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):1123–33. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 2.Freel AC, Shiloach M, Weigelt JA, et al. American College of Surgeons. American College of Surgeons Guidelines Program: A process for using existing guidelines to generate best practice recommendations for central venous access. J Am Coll Surg. 2008;207(5):676–82. doi: 10.1016/j.jamcollsurg.2008.06.340. [DOI] [PubMed] [Google Scholar]
- 3.Parienti JJ, Mongardon N, Mégarbane B, et al. 3SITES Study Group: Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373(13):1220–29. doi: 10.1056/NEJMoa1500964. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn GJ, White BC, Swetnam RE, et al. Peripheral vs. central circulation times during CPR: A pilot study. Ann Emerg Med. 1981;10(8):417–19. doi: 10.1016/s0196-0644(81)80308-3. [DOI] [PubMed] [Google Scholar]
- 5.Graham AS, Ozment C, Tegtmeyer K, et al. Central venous catheterization. N Engl J Med. 2007;356(21):e21. doi: 10.1056/NEJMvcm055053. [DOI] [PubMed] [Google Scholar]
- 6.Saugel B, Scheeren TWL, Teboul JL. Ultrasound-guided central venous catheter placement: A structured review and recommendations for clinical practice. Crit Care. 2017;21(1):225. doi: 10.1186/s13054-017-1814-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


