Abstract
Background
During an ongoing outbreak of COVID-19, unsuspected cases may be housed outside of dedicated isolation wards.
Aim
At a Singaporean tertiary hospital, individuals with clinical syndromes compatible with COVID-19 but no epidemiologic risk were placed in cohorted general wards for COVID-19 testing. To mitigate risk, an infection control bundle was implemented comprising infrastructural enhancements, improved personal protective equipment, and social distancing. We assessed the impact on environmental contamination and transmission.
Methods
Upon detection of a case of COVID-19 in the dedicated general ward, patients and health care workers (HCWs) contacts were identified. All patient and staff close-contacts were placed on 14-day phone surveillance and followed up for 28 days; symptomatic contacts were tested. Environmental samples were also obtained.
Findings
Over a 3-month period, 28 unsuspected cases of COVID-19 were contained in the dedicated general ward. In 5 of the 28 cases, sampling of the patient's environment yielded SARS-CoV-2; index cases who required supplemental oxygen had higher odds of environmental contamination (P = .01). A total of 253 staff close-contacts and 45 patient close-contacts were identified; only 3 HCWs (1.2%, 3/253) required quarantine. On 28-day follow-up, no patient-to-HCW transmission was documented; only 1 symptomatic patient close-contact tested positive.
Conclusions
Our institution successfully implemented an intervention bundle to mitigate COVID-19 transmission in a multibedded cohorted general ward setting.
Key Words: Containment, Coronavirus, SARS-CoV-2, Cohort, Nosocomial, Open ward
Abbreviations: AIIR, airborne infection isolation rooms; AGP, aerosol-generating procedure; ARD, acute respiratory disease; COVID-19, novel coronavirus disease-2019; CT, cycle threshold; HCW, health care workers; IPE, infection prevention and epidemiology; IW, isolation ward; PCR, polymerase chain reaction; PPE, personal protective equipment; RSW, respiratory surveillance ward
In the current COVID-19 pandemic, health care-associated transmission has been a major concern, with almost one-third of patients comprising health care workers (HCWs) and hospitalized inpatients.1 To reduce health care-associated spread, standard recommendation is that single-person rooms with dedicated toilets be used to isolate suspected COVID-19 cases, and negative-pressure airborne infection isolation rooms (AIIR) be used for cases in which aerosol-generating procedures (AGPs) may be required.2 However, during an outbreak of COVID-19 with ongoing local transmission, distinguishing COVID-19 from ordinary viral respiratory tract infection becomes challenging, as the symptoms of COVID-19 are nonspecific.3 Admitting all patients with acute respiratory disease (ARD) into dedicated isolation wards (IW) during a COVID-19 outbreak poses a logistical challenge, especially in hospitals with limited resources. Cases of COVID-19 may thus be housed outside the IW prior to detection; with potential for onward spread. Delayed detection of cases of COVID-19 can result in the inadvertent unprotected exposure of significant numbers of HCWs and patients, leading to the quarantine of large numbers of HCWs4 and lockdown of wards.5 Furthermore, health care-associated outbreaks of COVID-19 have been linked to infected patients in the general ward setting in whom COVID-19 was unsuspected; with devastating consequences for HCWs and patients.6, 7, 8 During ongoing community transmission of COVID-19, infection control strategies for the general ward setting are required in order to mitigate the potential of health care-associated transmission from unsuspected cases of COVID-19.
In Singapore, a globalized Asian city-state, local transmission of COVID-19 has been ongoing since early February 2020.9 Our institution's IW was reserved for cases meeting official criteria for confirmed/suspected COVID-19. However, rising numbers of locally transmitted cases meant that all patients presenting with ARD, even without suspicious contact or travel history, were potentially at risk of having unsuspected COVID-19 infection. After documentation of local community transmission, in order to mitigate the potential for health care-associated transmission from undetected cases of COVID-19, our institution placed individuals with clinical syndromes compatible with COVID-19 (eg, ARD, or undifferentiated viral fever) who did not have epidemiologic risk (eg, no history of contact with COVID-19 cases or clusters) in dedicated general wards segregated from the rest of the hospital. These general wards comprised a mixture of single rooms and cohorted cubicles with shared toilets. In these general wards, termed as respiratory surveillance wards (RSWs), an infection control bundle was implemented comprising infrastructural enhancements, improved personal protective equipment (PPE), and social distancing between patients, in order to mitigate the risk of a potential COVID-19 case initially admitted outside of an AIIR. We examined the impact of an infection control bundle on environmental contamination and transmission in a cohorted general ward setting, when unsuspected cases of COVID-19 were detected, focusing on the impact of such a strategy in mitigating health care-associated transmission.
Methodology
Institutional setting and study period
Singapore General Hospital is the largest public acute tertiary care hospital in Singapore, with 1,785 beds. Over a 3-month period from February 7 to May 7, 2020, we evaluated our institution's experience with managing unsuspected COVID-19 infection in cohorted RSWs, using a cross-sectional study design.
Respiratory surveillance ward: Admission criteria and ward layout
On February 5, 2020, immediately after the first reported case of local transmission,9 our institution adopted a containment strategy to place individuals without epidemiologic risk, but who presented with clinical syndromes compatible with COVID-19 (eg, ARD, or undifferentiated viral fever) in the RSWs for enhanced surveillance. Patients could only be transferred out of the RSW if oropharyngeal swabs for SARS-CoV-2 PCR were negative on 2 consecutive occasions, done 24 hours apart.10 , 11 High-risk suspect patients fulfilling official criteria for suspected COVID-19 (based on suspicious epidemiology or travel history) were admitted to the IW instead. While high-risk COVID-19 suspects were housed in AIIRs in the IW (single-occupancy rooms with ≥12 air changes-per-hour, controlled direction of air flow with negative differential pressure more negative than −2.5 Pascal, and anterooms designed to provide an “air-lock” between the adjacent area and the AIIR), the RSW was a modified normal-pressure general ward containing a mixture of normal-pressure single rooms and cohorted cubicles. Single rooms had their own attached toilet, whereas cohorted cubicles utilized a shared toilet. Each cohorted cubicle and single room had its own ventilation system, and air was not recirculated between cubicles or rooms.
Infection control bundle in respiratory surveillance ward
In the RSW, an infection control bundle was implemented comprising infrastructural enhancements, improved PPE, and social distancing between patients. Infrastructural enhancements involved the reduction of bed density in cohorted cubicles and improved distancing between beds, with the construction of partitions between beds. In the cohorted cubicles of the RSW, the average number of beds was reduced to 3 beds per cubicle, to ensure that beds were spaced at least 2 m apart; as compared to an average of 5-6 patients per cohorted cubicle in the typical general ward.12 Primary physicians in the RSW prioritized patients who required supplemental oxygen, noninvasive ventilation, or clinical features suspicious of viral pneumonia (eg, normal procalcitonin, lymphopenia) for admission to single rooms, though this was not always feasible due to the large number of admissions. Within the RSWs, cleaning and disinfection with 1,000 ppm sodium hypochlorite were stepped up, with the wards and toilets being cleaned 3 times a day. A risk-stratified approach was adopted with regards to PPE. Initially, HCWs in these wards used N95 respirators as PPE during routine care, with full PPE (N95 respirators, eye protection, gown, and gloves) reserved for instances where AGPs needed to be performed. However, from mid-March 2020, given the rising number of COVID-19 case being picked up in the RSW, HCWs used full PPE when caring for these patients. Compliance with usage of PPE in the RSW was audited by infection control nurses from the Department of Infection Prevention and Epidemiology. Finally, social distancing was encouraged within the RSW.12 Patients were advised to wear surgical masks, to remain within their room or cohorted cubicle at all times, and to avoid mingling with each other (if they were housed in a cohort cubicle). Surgical masks were provided for all patients, and patients were advised to only remove their masks during meals. Partitions between patient beds also minimized mingling. There was a strict no-visitors rule while patients were warded in the RSW.
Epidemiology investigations
Upon detection of a confirmed case of COVID-19 in the RSW, the affected room or cohorted cubicle was temporarily locked down that is, no new admissions to and no transfers out of the cubicle. Both the confirmed cases, as well as patient close-contacts, were transferred to the IW. Patient close-contacts were defined as a patient who had stayed in the same cohort cubicle with the index case5; given potential contamination of the shared air and surface environment from droplet and fomite spread.13 Simultaneously, contact tracing was done to identify HCWs who had come into contact with the confirmed case, and risk stratification was done based on the duration of contact, nature of activity (eg, AGPs), and type of PPE worn at the time of contact. Staff close-contacts were defined as HCWs who had contact within 2 m of the index case for a cumulative time of ≥15 minutes, or who had performed AGPs without appropriate PPE. Appropriate PPE was defined as at least an N95 mask for routine care and full PPE for AGPs. All patient close-contacts and staff close-contacts were monitored via phone surveillance for symptoms such as cough, dyspnea, and myalgia, and twice-daily temperature measurements, over a 14-day period from the date of exposure. If patient close-contacts or staff close-contacts developed symptoms, respiratory specimens were obtained, and swabs sent for COVID-19 testing. It was standard protocol to repeat the COVID-19 test 24 hours apart from the first in symptomatic close-contacts, if the first test was negative. All patient close-contacts and staff close-contacts were followed up for a 28-day period from the date of exposure, to determine if they tested positive for COVID-19 within this window; however, testing was only performed if contacts became symptomatic. All patient close-contacts, as well as staff close-contacts who had not utilized appropriate PPE, were placed under a 14-day quarantine based on our local Ministry of Health's guidelines. Patient close-contacts who had unresolved medical issues served out the full duration of their quarantine period in the isolation ward, even if they may have had a negative COVID-19 test during the quarantine period, whereas patient close-contacts who were medically fit for discharge were discharged to serve out their quarantine at home.
Environmental contamination: Sampling protocol upon detection of a COVID-19 case
Upon detection of a confirmed case of COVID-19 in the RSW, environmental sampling was done in the rooms to test for SARS-CoV-2 prior to terminal cleaning with sodium hypochlorite 1,000 ppm. Per protocol,13 areas that were sampled routinely included: high-touch areas in the patient's immediate vicinity, including the patient's call bell, foot and cot-side of the bed, and bedside table; as well as toilet facilities, namely the toilet bowl as well as the bathroom drain. Staff wearing full PPE used sterile premoistened swab sticks to swab high-touch areas for 2-3 minutes over a large surface. Repeat swabs were done post-terminal cleaning, using the same procedure. Investigation for SARS-CoV-2 RNA was done by qualitative real-time reverse transcription PCR (rRT-PCR) targeting E gene and ORF1b-nsp1414 , 15 on respiratory tract samples and environmental surveillance samples.
Ethics approval
As this was a descriptive study based on data collected by the hospital's Infection Prevention and Epidemiology Department as part of an outbreak investigation, ethics approval was not required under our hospital's Institutional Review Board guidelines; and application for waiver was formally obtained (CIRB 2020/2369).
Results
Case detection
Over the study period, a total of 4,621 patients were admitted to the RSW, of which 28 were confirmed cases of COVID-19 (0.61%, 28/4,621). Over the same period, a total of 845 cases of COVID-19 were picked up among the 2,681 patients admitted to the IW (31.5%, 845/2,681). Our institution used a broader set of case criteria for identifying suspect cases of COVID-19 compared to the official criteria, accounting for the higher pickup in IW.16 The RSW accounted for 3.2% (28/873) of COVID-19 cases admitted to our institution. Only 1 case of COVID-19 was initially admitted to the general ward instead of the RSW/IW during the 3-month study period, due to mild respiratory symptoms which were not apparent on initial triage in the emergency department.12
Epidemiological investigations
The details of COVID-19 patients detected in the RSW, as well as the numbers of patient and staff close-contacts, are provided in Table 1 . For index patients, the median duration of stay in the RSW prior to confirmation of COVID-19 and transfer to IW was 15.5 hours. Among index cases, the median duration of detectable viral shedding on rt-PCR of respiratory specimens was 5 days. The majority of index cases (71.4%, 20/28) presented with pneumonia; 5 presented with upper respiratory tract symptoms alone, and 3 presented with undifferentiated viral fever. Two patients had concurrent diarrhea together with respiratory symptoms. Four of the index cases required supplemental oxygen delivered through nasal cannula while in the RSW. Six of the index cases required intubation and mechanical ventilation, but all intubations occurred after IW transfer. A total of 253 staff close-contacts were identified; only 3 HCW (1.2%, 3/253) required quarantine due to significant unprotected exposure. A total of 45 patient close-contacts were identified; the median duration of overlap was 14 hours.
Table 1.
Demographics of confirmed COVID-19 cases isolated in dedicated general ward over a 3-month period (N = 28) and number of patient and staff close-contacts
 |
Environmental sampling
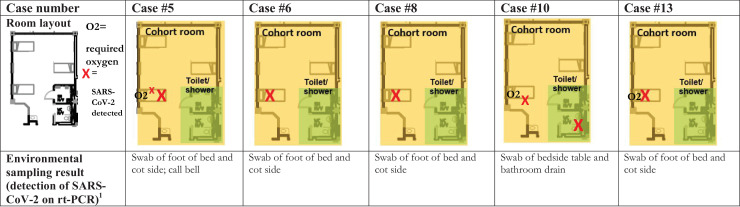
Around one-fifth of the index cases (17.9%, 5/28) had environmental surveillance samples taken from the immediate environment that returned positive for SARS-CoV-2 on rt-PCR, prior to terminal cleaning (Fig 1 ). The majority of the index cases with positive environmental surveillance samples (80.0%, 4/5) returned positive samples from high-touch areas in the immediate vicinity of the patient (eg, call bell, foot of bed, and cot-side); only in 1 instance did a swab from the bathroom drain of the shared bathroom return positive, with a cycle threshold value of 32.69 on rt-PCR for SARS-CoV-2 RNA. Of note, the index case had presented with a history of nonresolving diarrhea for 1 week, together with respiratory symptoms. The majority of positive environmental surveillance samples came from patients who were on supplemental oxygen. Of the 4 index cases who required supplemental oxygen in the general ward, 75.0% (3/4) had positive environmental surveillance samples for SARS-CoV-2, compared with 8.2% (2/24) among those not on supplemental oxygen (P = .01, Fisher's exact test). Repeat swabs taken from the immediate environment postcleaning returned negative.
Fig 1.
Location of positive environmental sampling results for SARS-CoV-2 in multibedded general ward cohort rooms prior to terminal cleaning.
1A total of 445 samples were taken; only 2.2% (10/445) returned positive.
Transmission dynamics
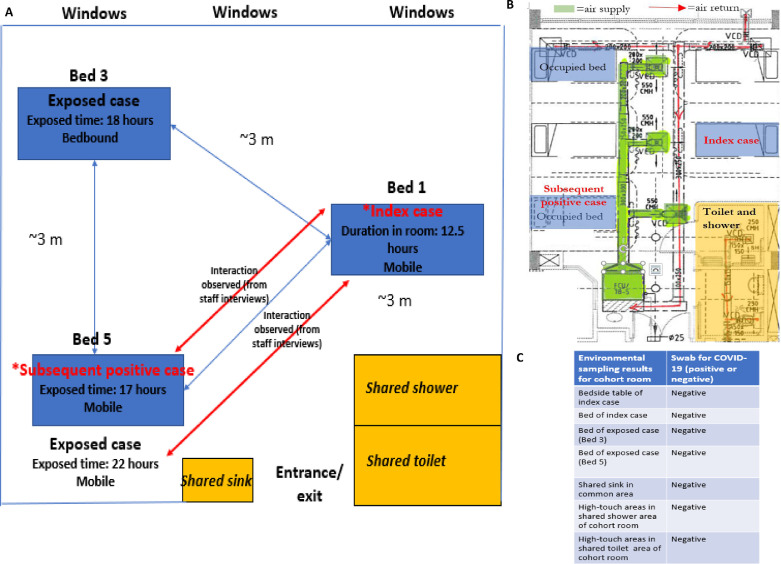
No staff close-contacts went on to develop COVID-19 postexposure despite intensive surveillance. However, among the 45 exposed patients, a total of 24 patients developed symptoms within the 14-day observation period while on phone surveillance and were subsequently tested for COVID-19. Only 1 patient close-contact who developed symptoms subsequently tested positive (2.2%, 1/45). Although the alternative possibility that this particular patient could have been exposed to an asymptomatic contact just prior to admission and was still within the incubation period17 at the point of admission could not be fully excluded, detailed epidemiological investigations were conducted for this case (Fig 2 ). Of note, the index case (Case #2) had the longest duration of stay in the RSW, at 49.5 hours. The patient close-contact that subsequently developed COVID-19 was an elderly male with a past medical history of chronic obstructive pulmonary disease. He had been admitted to another hospital 12 days prior to the current admission; during the previous admission, COVID-19 testing was negative. He shared a cohorted cubicle with Case #2 for 17 hours and had been discharged prior to the confirmation of COVID-19 in Case #2. During his admission, he had 2 negative swabs for SARS-CoV-2, 24 hours apart. He was placed on home quarantine, but subsequently developed symptoms 5 days postexposure and tests were positive for SARS-CoV-2 on re-admission. Environmental sampling of high-touch areas in the shared common areas prior to cleaning was negative for SARS-CoV-2. Of the 2 other exposed patients, 1 was bedbound and nonconversant, while the other was ambulatory. Staff had previously observed social mingling between the ambulatory patients in the cubicle, without wearing surgical masks. While the duration of overlap for the exposed patient that subsequently developed COVID-19 was the shortest, it also corresponded with the period during which the index patient was still well and able to interact socially. The index patient deteriorated subsequently over the course of the day and 4 hours after transfer to IW in the evening, required intubation and mechanical ventilation for respiratory failure. He eventually demised at day 30 of admission; respiratory samples prior to demise remained positive for SARS-CoV-2.
Fig 2.
Layout of cohort room in dedicated general ward and key findings of epidemiologic investigation for cluster of COVID-19 cases
A: Layout of cohort room and epidemiologic investigations for cluster of positive cases
B: Airflow diagram in cohort room (self-contained)
C: Results of environmental sampling in cohort room after confirmation of index case, prior to terminal cleaning (all negative)
Discussion
The main finding of our study was that an infection control bundle comprising infrastructural enhancements, improved PPE and social distancing mitigated the risk of environmental contamination and transmission in a cohorted general ward setting. In our institution, the concept of a designated RSW for patients with clinical syndromes that were compatible with COVID-19 ensured that the large majority of COVID-19 cases diagnosed outside of the IW were still managed in areas where appropriate PPE, infrastructural enhancements and proper infection prevention practices (hand hygiene, environment, and equipment hygiene) were in place to reduce health care-associated spread. Via early testing and detection, the duration of exposure in the cohorted RSW was kept relatively short (∼15 hours on average), compared to the median duration of viral shedding over the clinical course.18 Additionally, as peak viral shedding is thought to occur earlier in the clinical course during the first week of symptoms, early detection can potentially mitigate transmission risk during peak infectivity.18 Early detection in the clinical course prior to deterioration also helped to minimize the number of AGPs performed outside of the IW setting. Indeed, although almost one-fifth of the index cases subsequently deteriorated and required intubation, this occurred after the patients had been already transferred into the IW. This was important given the increased potential of health care-associated transmission during aerosolization caused by AGPs. For instance, delayed detection in a single patient that required intubation and mechanical ventilation prior to the diagnosis of COVID-19 pneumonia resulted in the quarantine of 41 HCWs for 2 weeks, due to a prolonged duration in the general ward prior to detection.4 In the cluster of COVID-19 cases reported in this study, there were several risk factors: the duration of the index patient's stay in the RSW was the longest (>48 hours) and staff had previously observed social mingling between the unmasked patients in the cubicle. Though health care-associated transmission could not be definitively proven, these findings reinforce the importance of a bundle of interventions in reducing risk of COVID-19 transmission: social distancing in high-risk areas, early detection to minimize exposure duration; and usage of appropriate PPE in higher-risk areas to minimize HCW exposure.
A short duration of stay in the dedicated general ward, reduction of the number of beds in cohorted cubicles, and usage of full PPE minimized the total numbers of patient and HCW exposures. Indeed, although a total of 28 hitherto unsuspected cases of COVID-19 were picked up in the RSW, there were only 45 patient close-contacts. In comparison, delayed detection of a single case of COVID-19 in the setting of a multibedded cohorted general ward resulted in the exposure of as many as 71 patients, with all occupants of a cohort cubicle deemed to be in close-contact and requiring quarantine.5 In our institution itself, a single case of COVID-19 in the nonmodified general ward resulted in the potential exposure of 18 patients.12 As patient close-contacts require quarantine in suitable isolation facilities within hospital if medically unfit for discharge,5 minimizing the number of patient close-contacts is crucial in relieving additional strain on hospital resources during an ongoing outbreak.
Persistence of SARS-CoV-2 in the environment, in aerosols and on surfaces,19 , 20 provides a potential vector for transmission. Multiple studies report extensive environmental contamination of inanimate surfaces in the immediate environment of COVID-19 cases (patients’ rooms and toilets) prior to cleaning.13 . 21 However, the bulk of these studies are conducted in AIIRs; the applicability of these studies to the general ward setting may potentially be confounded by differences in ventilation, airflow and room layout (such as the presence of anterooms to segregate the patient's immediate environment from common areas).22 A small study that tested environmental samples from 2 cohorted 4-bed cubicles on a general ward detected SARS-CoV-2 in 13.6% of samples collected, generally from near-patient environments; however, the COVID-19 patients placed in these cohorted cubicles were no longer symptomatic at the point of sampling.23 Uniquely, our study provided the opportunity to investigate the extent of environmental contamination in COVID-19 patients housed in a general ward setting, early on at the point of initial admission; although this was modified by the effects of our infection control bundle. The rate of environmental contamination reported in our study was low; less than 5% of environmental samples tested positive, compared to other studies which reported rates of 15%-50%, mainly from AIIRs.21, 22, 23, 24, 25 This could potentially be attributed to the effect of the infection control bundle comprising infrastructural enhancements and social distancing that was introduced in our designated wards; though the precise contribution of each component of the bundle could not be assessed.
Notably, though, in our study the majority of positive environmental surveillance samples came from patients who were on supplemental oxygen in the RSW. This may be related to increased risk of droplet dispersion in patients on supplemental oxygen26 , 27 or the inability to comply with mandatory usage of face masks.28
Our study had several limitations. Only patient and HCW contacts with fever or respiratory symptoms were tested with rt-PCR, hence the possibility of asymptomatic infection among the exposed patients and HCWs cannot be entirely excluded. As the diagnostic yield of PCR testing for SARS-CoV-2 is likely dependent on the quality of sampling,29 cases may have been missed due to sampling issues; however, all symptomatic close-contacts were tested at least twice, 24 hours apart. The follow-up of potentially exposed patients and HCWs to test for seroconversion, when such tests are developed, would be useful. For environmental sampling, we were unable to perform viral culture; hence the viability of the virus found from environmental samples could not be ascertained. We were also unable to perform air sampling for index cases, as upon confirmation of COVID-19, cases were immediately moved to the IW to reduce risk of transmission.
Conclusions
In conclusion, over a 3-month period, our institution implemented a bundle of interventions to reduce risk of intra-hospital transmission of COVID-19 in a multibedded cohorted general ward setting, through the implementation of an infection control bundle comprising infrastructural enhancements, improved PPE, and social distancing between patients. Routine testing for patients presenting with clinical syndromes compatible with COVID-19 allowed for early detection and early isolation, reducing the duration of exposure in the general ward setting and further mitigating the risk of health care-associated transmission.
Footnotes
Conflict of interest: None to report.
References
- 1.Huang CL, Wang YM, Li XW, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centres for Disease Control and Prevention, USA. Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. Available at:https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html. Accessed March 16, 2020.
- 3.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng KQ, Poon BH, Puar THK, et al. COVID-19 and the risk to healthcare workers: a case report. Ann Intern Med. 2020;172:766–767. doi: 10.7326/L20-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong SC-Y, Kwong RT-S, Wu TC, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119–127. doi: 10.1016/j.jhin.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility—King County, Washington. MMWR Morb Mortal Wkly Rep. 2020;69:339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li YK, Peng S, Li LQ, et al. Clinical and transmission characteristics of Covid-19 - a retrospective study of 25 cases from a single thoracic surgery department. Curr Med Sci. 2020;40:295–300. doi: 10.1007/s11596-020-2176-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adrait A, Benoist F, Castel-Kremer E, et al. Fast nosocomial spread of SARS-CoV2 in a French geriatric unit [e-pub ahead of print] Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.99. Accessed July 20, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore-current experience: critical global issues that require attention and action [e-pub ahead of print] JAMA. 2020 doi: 10.1001/jama.2020.2467. Accessed July 20, 2020. [DOI] [PubMed] [Google Scholar]
- 10.Wee LE, Hsieh JYC, Phua GC, et al. Respiratory surveillance wards as a strategy to reduce nosocomial transmission of COVID-19 through early detection: the experience of a tertiary-care hospital in Singapore [e-pub ahead of print] Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.207. Accessed July 20, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tay JY, Lim PL, Marimuthu K, et al. De-isolating COVID-19 suspect cases: a continuing challenge. Clin Infect Dis. 2020;71:883–884. doi: 10.1093/cid/ciaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wee LE, Conceicao EP, Sim XYJ, et al. Minimising intra-hospital transmission of COVID-19: the role of social distancing. J Hosp Infect. 2020;105:113–115. doi: 10.1016/j.jhin.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chu DKW, Pan Y, Cheng SMS, et al. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin Chem. 2020;66:549–555. doi: 10.1093/clinchem/hvaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wee LE, Fua TP, Chua YY, et al. Containing COVID-19 in the emergency room: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27:379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 19.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kampf G, Todt D, Pfaender S, et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yung CF, Kam KQ, Wong MSY, et al. Environment and personal protective equipment tests for SARS-CoV-2 in the isolation room of an infant with infection. Ann Intern Med. 2020;173:240–242. doi: 10.7326/M20-0942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Colaneri M, Seminari E, Piralla A, et al. Lack of SARS-CoV-2 RNA environmental contamination in a tertiary referral hospital for infectious diseases in Northern Italy. J Hosp Infect. 2020;105:474–476. doi: 10.1016/j.jhin.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryu BH, Cho Y, Cho OH, Hong SI, Kim S, Lee S. Environmental contamination of SARS-CoV-2 during the COVID-19 outbreak in South Korea. Am J Infect Control. 2020;48:875–879. doi: 10.1016/j.ajic.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu S, Wang Y, Jin X, Tian J, Liu J, Mao Y. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. Am J Infect Control. 2020;48:910–914. doi: 10.1016/j.ajic.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chia PY, Coleman KK, Tan YK, et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat Commun. 2020;11:2800. doi: 10.1038/s41467-020-16670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simonds AK, Hanak A, Chatwin M, et al. Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne infections. Health Technol Assess. 2010;14:131–172. doi: 10.3310/hta14460-02. [DOI] [PubMed] [Google Scholar]
- 27.Hui DS, Chan MT, Chow B. Aerosol dispersion during various respiratory therapies: a risk assessment model of nosocomial infection to health care workers. Hong Kong Med J. 2014;20(Suppl 4):9–13. [PubMed] [Google Scholar]
- 28.Liu X, Zhang S. COVID-19: Face masks and human-to-human transmission. Influenza Other Respir Viruses. 2020;14:472–473. doi: 10.1111/irv.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mackay IM, Arden KE. MERS coronavirus: diagnostics, epidemiology and transmission. Virol J. 2015;12:222–243. doi: 10.1186/s12985-015-0439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]