In the UK, more than 279 392 cases of COVID-19 had been documented by June 3, 2020, and more than 39 500 patients had died with the disease, according to the COVID-19 web-based dashboard at Johns Hopkins University.1 Data derived from the UK Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme Database show that, for the first 8062 patients admitted to the ICU across the UK with documented outcomes, by May 29, 2020, about 72% received advanced mechanical ventilation and the mortality rate was around 53%. This mortality far exceeds that of typical severe acute respiratory distress syndrome (ARDS).2 The significant surge in the number of patients requiring ventilatory support has presented the UK National Health Service with unprecedented challenges, including pressures on critical care capacity, resources, and supplies, concerns about staff protection, as well as ethical issues associated with triage and resource allocation.3 Debates about the way in which different modalities of ventilatory support should be provided to the largest number of patients, while controlling the number of critical care admissions and protecting staff, have at times generated adversarial positions at the extremes of the debate. The motivations behind these arguments are undoubtedly positive, but they do not necessarily help frontline clinicians who are caring for individuals with COVID-19.
To design triage systems and pathways of care, it is important to operate cautiously within models that best reflect evolving understanding of the pathophysiology and natural history of this new disease. COVID-19 pneumonia leads to hypoxaemic respiratory failure, initially due to the coexistence of interstitial oedema and altered pulmonary perfusion, in the absence of a significant loss of lung volume and compliance.4 Although, on average, patients present with an oxygenation deficit5 similar to that of moderate-to-severe ARDS (median PaO2/FiO2 of 20 kPa),2 the cause of this deficit seems to be unlike that of classic ARDS, and the response to positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP) in terms of alveolar recruitment is not substantial in patients with COVID-19.6
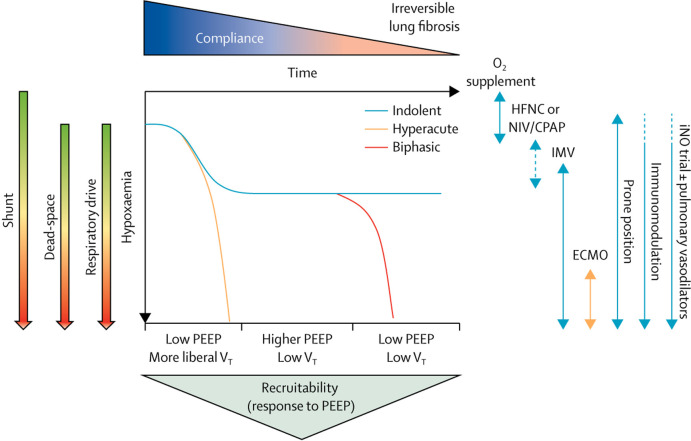
Multiple mechanisms of dysregulation in the pulmonary perfusion exist in COVID-19: the abolition of hypoxic pulmonary vasoconstriction, causing an increase in venous admixture; excessive pulmonary vasoconstriction; and microthrombosis or macrothrombosis, leading to increased dead-space.7 Patients with COVID-19 and hypoxaemia predominantly due to shunt have a variable work of breathing, might respond to CPAP, and could be considered for awake prone positioning.8 As dead-space ventilation increases, patients typically have greater respiratory drive and work of breathing, and greater minute ventilation at the expense of higher transpulmonary pressures. These patients are at higher risk of self-induced lung injury, are prone to further deterioration with non-invasive ventilation (NIV), which might be associated with worse outcomes,9 and might benefit from prompt invasive ventilation. In patients with COVID-19, increased dead-space can be due to vasoconstriction or prevalent microthrombosis or macrothrombosis, so they are likely to benefit from pulmonary vasodilators or systemic anticoagulation. Furthermore, the hyperinflammatory and hypermetabolic state might determine a further significant increase in respiratory drive, and transpulmonary stress and strain. The consequent lung oedema, lung weight, and worsening consolidation can contribute to disease progression.10 At this stage, patients with COVID-19 often present with features resembling more typical ARDS—including a variable degree of lung recruitability—and might respond to treatments generally used in this condition. Finally, on the basis of radiological and pathological findings from our institution (unpublished), COVID-19 seems to be associated with early and extensive fibroproliferation. Therefore, patients in the later stages of severe and progressive disease might lose recruitability as the lung oedema is replaced by dense consolidation and fibrosis, with failure to respond to conventional treatment, prone positioning, or pulmonary vasodilators.
On the basis of our experience, patients can present to hospital with any of these phenotypes, and the clinical course tends to follow one of three main patterns: a hyperacute course, with severe hypoxaemia and breathlessness leading to immediate intubation; an indolent course, in which patients have a moderate or severe hypoxaemia but only moderate work of breathing; and a biphasic course, in which patients have an initial indolent course followed—typically after 5–7 days—by an acute deterioration with hyperinflammation, fever, and worsening respiratory failure with bilateral infiltrates and consolidation. It seems logical that triage and ventilatory strategies should reflect these factors in addition to resource and ethical considerations. Proposed approaches are presented in the accompanying schematic (figure ), but further studies of the course of COVID-19 will be needed to describe and validate phenotypes of the disease.
Figure.
Pathophysiological trajectory in COVID-19 and proposed implications for respiratory support
The schematic is based on our observations in a large centre for the management of patients with severe respiratory failure, part of a UK severe respiratory failure/ECMO network. CPAP=continuous positive airway pressure. ECMO=extracorporeal membrane oxygenation. HFNC=high-flow nasal cannula. IMV=invasive mechanical ventilation. iNO=inhaled nitric oxide. NIV=non-invasive ventilation. PEEP=positive end-expiratory pressure. VT=tidal volume.
A one-size-fits-all approach will not lead to improved outcomes in patients with COVID-19. Importantly, we argue that consideration for extracorporeal support should be given to patients who become refractory to conventional management strategies—particularly those with a hyperacute course—before they develop overt and diffuse fibrosis. The selection of patients likely to benefit from extracorporeal membrane oxygenation (ECMO) is extremely difficult, given the large number of potential candidates, the limited resources available, and lack of evidence for the effectiveness of ECMO above and beyond conventional strategies.3
We propose that ventilation strategy should be integrated with the observed phases and physiological patterns of the disease. This might prove to be useful in addressing ongoing controversies about the use of NIV versus invasive mechanical ventilation, as well as intubation timing and criteria. Future research should aim to clarify the best ventilation strategy for individual patients (eg, phenotypes and response to PEEP), to describe disease mechanisms associated with the pathophysiological patterns and clinical course of COVID-19 (eg, early vs late presentation; vascular vs parenchymal), to identify biomarkers (eg, cytokines, ferritin, D-dimer, or procalcitonin) that could help to guide management, and to establish the efficacy and optimum timing of promising therapeutics. In the meantime, in an era of big data and large databases, it would be worth using machine learning and other approaches to try to identify the link between observed patterns of physiology, interventions, and outcomes before clinical trials have been completed.
Acknowledgments
We declare no competing interests.
References
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellani G, Laffey JG, Pham T. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 3.Phua J, Weng L, Ling L. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gattinoni L, Chiumello D, Caironi P. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020 doi: 10.1007/s00134-020-06033-2. published online April 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G, Zangrillo A, Zanella A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan C, Chen L, Lu C. Lung recruitability in COVID-19-associated acute respiratory distress syndrome: a single-center observational study. Am J Respir Crit Care Med. 2020;201:1294–1297. doi: 10.1164/rccm.202003-0527LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020 doi: 10.1016/S2665-9913(20)30121-1. published online May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elharrar X, Trigui Y, Dols AM. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020 doi: 10.1001/jama.2020.8255. published online May 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellani G, Laffey JG, Pham T. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 10.Tonelli R, Fantini R, Tabbi L. Inspiratory effort assessment by esophageal manometry early predicts noninvasive ventilation outcome in de novo respiratory failure: a pilot study. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.201912-2512OC. published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]