Abstract
Background
Transcatheter aortic valve implantation operators have adapted to a less invasive technique by foregoing the use of general anaesthesia and transoesophageal echocardiography. This is known as a ‘minimalist approach’. This approach has yet to be explored in transcatheter mitral valve replacement (TMVR). Two patients with high perioperative risk underwent TMVR using only monitored conscious sedation (CS) and intracardiac echocardiography (ICE).
Case summary
The patients were symptomatic and required treatment of severe mitral regurgitation and severe mitral stenosis in a mitral valve ring and prosthetic mitral valve, respectively. With the use of an antegrade transseptal approach, the procedure was conducted under CS using ICE only. After placement of the prosthetic mitral valve, the valve was assessed by advancing the ICE catheter through the interatrial septal defect and no significant paravalvular leak occurred. In one case, ad hoc treatment of right to left shunting was successfully pursued. Valve function was excellent immediately and at 24 h after implantation and resulted in significant haemodynamic improvement.
Conclusion
With more TMVR cases being conducted, the ‘minimalist approach’ with CS and ICE may be considered in selected cases.
Keywords: Transcatheter mitralvalve-in-valve, Valve-in-ring, Intracardiac echocardiography, Minimalist approach, Case report
Learning points
Implementing a minimalist approach using only intracardiac echocardiography and conscious sedation for transcatheter mitral valve replacement is feasible.
Intracardiac echocardiography is an effective and practical tool for atrial puncture, valve deployment, and valve interrogation.
Using a minimalist approach for percutaneous mitral valve interventions allows adequate imaging, decreased invasiveness, patient safety, and operator independence.
Introduction
The ‘minimalist approach’ using monitored conscious sedation (CS) has evolved to become the strategy of choice in most experienced transcatheter aortic valve implantation (TAVI) centres.1 It is associated with improved procedural efficiency and reduced length of stay2 without compromising procedural success or clinical outcomes.3 To our knowledge, this approach has not been evaluated in patients undergoing transcatheter mitral valve replacement (TMVR). We report the first two cases and demonstrate the feasibility of this approach, while highlighting the value of intracardiac echocardiography (ICE).
Timeline
| Case 1 | |
| Six months prior to presentation | A 73-year-old woman with severe degenerative mitral valve regurgitation s/p surgical mitral valve repair w/ring c/b aortic dissection. Explorative reoperation and surgical repair with endovascular graft. |
| Upon presentation to clinic | Completed rehab but complaining of sob w/ exertion. New York Heart Association III, decompensated heart failure, and elevated BNP |
| Transthoracic echocardiography: severe recurrent m itral regurgitation | |
| Evaluation by Heart Team including work up w/CTA and transoesophageal echocardiography (TOE); decision for percutaneous transcatheter mitral valve replacement (TMVR) | |
| Operative procedure | Transcatheter mitral valve replacement, valve-in-ring; minimalist approach |
| Discharged safely in 48 h on Aspirin and Plavix | |
| 12-week post-operative | After TMVR, symptomatically free and no evidence of paravalvular leak |
| Case 2 | |
| Nine years prior to presentation | A 69-year-old woman with surgical bioprosthetic mitral valve implanted |
| Upon presentation to clinic | Subjectively, limited functional capacity, lower limb swelling, on exam diastolic murmur Grade III, volume overloaded, cardiac echo: severe mitral stenosis of bioprosthetic valve, severe pulmonary hypertension, right ventricular systolic dysfunction |
| Heart Team evaluation for severe symptomatic mitral stenosis: left right cath, TOE, CT imaging | |
| Prohibitive surgical risk due to frailty index and medical comorbidities | |
| Operative procedure | Transcatheter mitral valve replacement, valve-in-valve; minimalist approach |
| Iatrogenic ASD closure with occluder device | |
| Postoperatively | After TMVR, no evidence of paravalvular leak |
| Discharged in 48 h on Aspirin and Plavix | |
| 8-week post-operative | New York Heart Association functional Class II and reporting improved quality of life |
Case presentation
Case 1
A 73-year-old woman was referred for management of severe symptomatic relapsing mitral valve regurgitation after a failed mitral valve repair 3 months prior. She presented to the clinic with dyspnoea on exertion, significant weight loss, and mild anaemia from low-grade haemolysis. Signs of decompensated heart failure and a loud precordial holosystolic murmur were appreciated on exam. Because of a previously complicated post-operative course with ensuing frailty and worsening heart failure, she was considered for transcatheter mitral valve-in-ring (ViR). Pre-procedural transoesophageal echocardiography (TOE) assessment confirmed a large, anteriorly directed regurgitant jet from a relapsing posterior leaflet prolapse (Figure 1A;Supplementary material online, Video S1) with preserved biventricular function. Computed tomography (CT) revealed a 34-mm 3D CarboMedics Ring (Sorin SpA, Milan, Italy) with a measured inner area of 519 mm2 and a calculated neo left ventricular outflow tract (LVOT) area of 418.9 mm2.
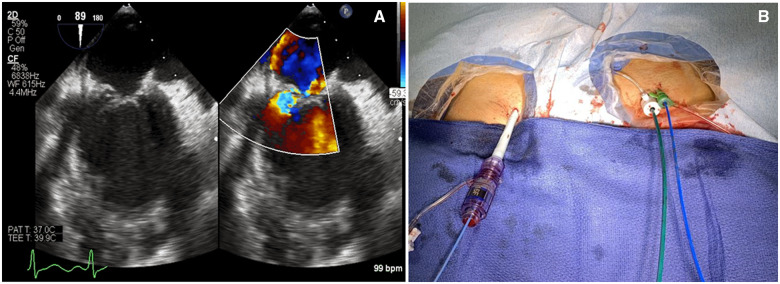
Figure 1.
(A) Transoesophageal echocardiography image showing prolapse of the posterior mitral valve leaflet resulting in severe regurgitation. (B) Demonstration of vascular access used during a ‘minimalist approach’ with a 16-Fr Edwards E-Sheath in the right femoral vein, 11-Fr St Jude sheath in the left femoral vein with 9-Fr intracardiac echocardiography catheter, and a 6-Fr sheath in the left femoral artery with 6-Fr pigtail catheter.
Intervention
The procedure was performed in the hybrid operating suite using a ‘minimalist approach’ with ICE imaging and CS. Local anaesthesia was provided prior to bilateral femoral access. Neither central line nor Foley catheter were used. Transcatheter mitral ViR was pursed through a transseptal approach using a 29-mm Edwards Sapien S3 valve (Edwards Lifesciences, Irvine, CA, USA) from the right femoral vein (Figure 1B). A 9-Fr Viewflex ICE catheter (Abbott Vascular, Santa Clara, CA, USA) was inserted into the right atria from the contralateral femoral vein to guide the transseptal puncture and TMVR. Transseptal access was performed with an 8.5-Fr Agilis catheter and standard BRK needle (St. Jude Medical; St. Paul, MN, USA) (Supplementary material online, Video S2). Atrial septostomy was performed with a 12 mm × 40 mm 0.035 ‘Mustang balloon (Marlborough, MA, USA) over a 0.035’ Medtronic Confida wire (Minneapolis, MN, USA). Right ventricular (RV) burst pacing was employed at 180 b.p.m. to allow for a steady and gradual deployment of the balloon-expandable prosthesis within the 3D Carbomedics ring. The valve delivery system was removed over a wire to maintain transseptal access. The tip of the ICE catheter was redirected into the left atrium (LA) chamber across the atrial septostomy to interrogate the bioprosthesis (Supplementary material online, Video S3). Intracardiac echocardiography examination showed clear visualization of a normal functioning mitral bioprosthesis in stable position with trivial paravalvular regurgitation (Supplementary material online, Video S4). The pressure gradient measured across the neo-LVOT was 3 mmHg. Colour Doppler interrogation of the atrial septostomy showed a small, non-clinically significant 8 mm left-to-right shunt on colour Doppler that was left untreated. The patient’s post-operative course was uneventful and characterized by prompt recovery with early discharge the next day on aspirin 81 mg and clopidogrel 75 mg daily. Remarkable clinical improvements with preserved valve function was appreciated during 12-week follow-up.
Case 2
A 69-year-old frail woman was referred for management of severe bioprosthetic mitral stenosis involving a 27-mm ThermaFix Carpentier-Edwards bovine pericardial valve implanted 9 years prior. Symptoms included progressive decline in functional capacity with dyspnoea on minimal exertion and her medical comorbidities included severe obstructive sleep apnoea and low-grade lymphoma. Physical exam was notable for moderate diastolic rumble with mechanical S1. Transthoracic echocardiography confirmed the presence of structural valve degeneration with mean transvalvular gradient of 13 mmHg. A transcatheter mitral valve-in-valve (ViV) procedure was recommended due to high frailty index, coupled with the presence of severe pulmonary hypertension with poor RV systolic function. Pre-procedural CT imaging revealed a calculated neo LVOT area of 443 mm2 and an inner bioprosthetic valve area of 462 mm2.
Intervention
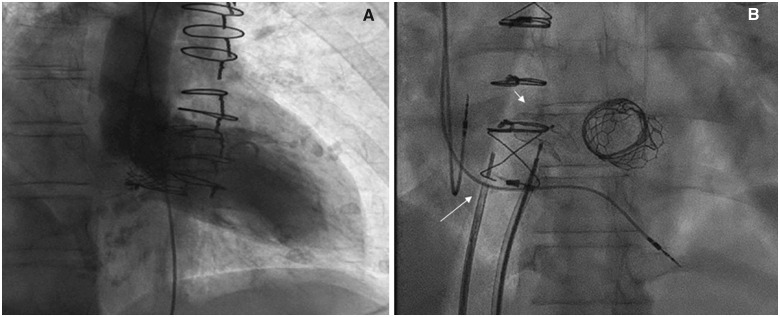
As with the previous case, a ‘minimalist approach’ was undertaken in the hybrid suite using CS and ICE imaging. Vascular access, transseptal puncture, and atrial septostomy were completed using the same technique described earlier. A transcatheter 26-mm Edwards Sapien S3 valve was deployed under rapid burst pacing at 180 b.p.m. with an additional 1 mL of saline above nominal volume to flare the skirt of the S3 prosthesis. Fluoroscopic examination revealed adequate valve position and implant height (Figure 2A). The mean mitral valve gradient decreased from 14 to 2 mmHg following TMVR. A corresponding decrease in mean LA pressure was also observed from 34 to 14 mmHg, with a final LVOT gradient of 3 mmHg. Intracardiac echocardiography examination obtained from the LA chamber revealed a stable, normal functioning ViV bioprosthesis with no evidence of residual mitral regurgitation or mitral stenosis. Noticeably, the patient experienced significant hypoxaemia soon after the valve delivery system was removed. The finding was explained by the presence of right to left atrial shunting noted during ICE examination (Supplementary material online, Video S5) in a patient with severe residual tricuspid regurgitation and pulmonary HTN. Intracardiac echocardiography-guided percutaneous closure of the atrial septostomy was pursued ad hoc with a 14-mm Amplatzer Septal Occluder (AGA Medical, Golden Valley, MN, USA). The hypoxaemia resolved immediately following septal closure (Supplementary material online, Video S6; Figure 2B). The post-operative course was characterized by an uneventful recovery and early discharge 2 days later with aspirin 81 mg and clopidogrel 75 mg daily. At 30-day follow-up, the patient reported marked improvement in functional status and quality of life.
Figure 2.
(A) Fluoroscopic exam showing left ventriculography with no evidence of mitral valvular regurgitation during left ventricular systole. (B) Fluoroscopic image showing final result: intracardiac echocardiography catheter (long arrow), Amplatz Septal Occluder (short arrow), and Edward Sapien S3 ViV.
Discussion
Transcatheter aortic valve implantation was once uniformly performed using general anaesthesia and TOE, with central line placement, and Foley catheter insertion. It took over a decade to transform the practice of TAVI using a less invasive ‘minimalist approach’ with monitored CS and local anaesthesia.1 As validated by multiple studies, this strategy has been associated with lower transfusion rates, procedural times and hospital length of stay, while reducing cost and improving procedural outcomes.1–9 The adoption of a ‘minimalist approach’ in the contemporary era of TMVR has not yet been systematically evaluated. We, herein, report the first two cases whereby a ‘minimalist approach’ was successfully employed during TMVR using ICE imaging to safely execute and complete the procedure.
In the first case, a mitral ViR was performed in a frail and debilitated patient with refractory heart failure from severe degenerative mitral regurgitation despite previous surgical repair attempt. The second case involved a mitral ViV replacement in a patient with severe degenerative bioprosthetic mitral stenosis with concomitant RV systolic dysfunction, severe tricuspid regurgitation, and pulmonary HTN. Both patients were deemed high risk and poor surgical candidates for redo-surgery. Additionally, general anaesthesia with TOE was felt to add greater risk and concerns for prolonged recovery and post-operative complication. In both, the ‘minimalist approach’ (Figure 1B) resulted in prompt and uneventful recovery with early discharge within 48 h.
The feasibility of ICE-guided TMVR is also exemplified. In both cases, ICE imaging resulted in clear visualization of the interatrial septum during transseptal puncture, while providing an ad hoc solution for mitral valve assessment following TMVR. Furthermore, ICE provides clear visualization of the atrial septostomy post-TMVR and for percutaneous septal closure when clinically warranted as illustrated in Case 2. Although one may argue that TOE may be performed under conscious sedation, it is often cumbersome and therefore avoided in prolonged complex procedures. This too explains why in the contemporary era, ICE has evolved to become a resourceful tool for structural heart procedures such as atrial septal defect, patent foramen ovale, and LA appendage closure.10,11 In these cases ICE has been proven safe and effective,12,13 while evading the need for general anaesthesia, and reducing radiation exposure, contrast use, decreasing hospital length of stay and increasing operator independence.11,14,15
Among the main limitations of ICE includes far-field interrogation of cardiac structures. This explains why, as in our case, transseptal access is required to interrogate the mitral valve or other left-sided structures. In the case of a TMVR, it is recommended that the distal ICE catheter tip be advanced into the LA through the atrial septostomy (Supplementary material online, Video S3). Finally, although not specific to TMVR, a few studies have reported similar value to ICE and CS in patients undergoing Mitraclip or mitral balloon valvuloplasty.11,14,16 Until recently ICE imaging was only available in two-dimensional form, however, as three-dimensional ICE imaging becomes more available, it is likely that we will see a surge in its applicability. It is important to acknowledge that ICE imaging requires operator proficiency and technical expertise. Formal training is therefore encouraged to master the technique and assure its safety and applicability.
The present case series supports the strategy of a ‘minimalist approach’ using ICE imaging during TMVR and resulting in decreased invasiveness, adequate imaging, operator independence and early hospital discharge. Until further evaluation, this strategy should not replace the existing standard of care of general anaesthesia and TOE for TMVR. To our knowledge, however, this represents the first cases of mitral ViR and ViV performed using this approach—demonstrating its potential safety and feasibility.
Lead author biography
Robert J. Cubeddu, MD is a section head of structural heart disease, Chairman of Cardiology Heart and Vascular Institute Cleveland Clinic Florida. Post-graduate training in Interventional Cardiology and SHD at MGH, Harvard Medical School with vast experience in SHD interventions. National proctor for TAVR, Mitraclip, and Amplatz-related products. Principal site investigator for several multicentre RCTs. Multiple publications in peer review journals. Member of the editorial board—Journal of CCI and Journal of SHD. Member of the national SHD council for SCAI. Interest in clinical research and innovations.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Durand E, Borz B, Godin M, Tron C, Litzler P-Y, Bessou J-P, , Bejar K, Fraccaro C, Sanchez-Giron C, Dacher JN, Bauer F, Cribier A, Eltchaninoff H. Transfemoral aortic valve replacement with the Edwards SAPIEN and Edwards SAPIEN XT prosthesis using exclusively local anesthesia and fluoroscopic guidance: feasibility and 30-day outcomes. JACC Cardiovasc Interv 2012;5:461–467. [DOI] [PubMed] [Google Scholar]
- 2. Barbanti M, Capranzano P, Ohno Y, Attizzani GF, Gulino S, Imme S, Cannata S, Aruta P, Bottari V, Patanè M, Tamburino C, Di Stefano D, Deste W, Giannazzo D, Gargiulo G, Caruso G, Sgroi C, Todaro D, di Simone E, Capodanno D, Tamburino C. Early discharge after transfemoral transcatheter aortic valve implantation. Heart 2015;101:1485–1490. [DOI] [PubMed] [Google Scholar]
- 3. Hosoba S, Yamamoto M, Shioda K, Sago M, Koyama Y, Shimura T, Kagase A, Tada N, Naganuma T, Araki M, Yamanaka F, Shirai S, Watanabe Y, Hayashida K Safety and efficacy of minimalist approach in transfemoral transcatheter aortic valve replacement: insights from the Optimized transCathEter vAlvular interventioN–Transcatheter Aortic Valve Implantation (OCEAN-TAVI) registry. Interact Cardiovasc Thorac Surg 2017;26:420–424. [DOI] [PubMed] [Google Scholar]
- 4. Motloch LJ, Rottlaender D, Reda S, Larbig R, Bruns M, Müller-Ehmsen J, Strauch J, Madershahian N, Erdmann E, Wahlers T, Hoppe UC.. Local versus general anesthesia for transfemoral aortic valve implantation. Clin Res Cardiol 2012;101:45–53. [DOI] [PubMed] [Google Scholar]
- 5. Yamamoto M, Meguro K, Mouillet G, Bergoend E, Monin J-L, Lim P, Dubois-Rande J-L, Teiger E.. Effect of local anesthetic management with conscious sedation in patients undergoing transcatheter aortic valve implantation. Am J Cardiol 2013;111:94–99. [DOI] [PubMed] [Google Scholar]
- 6. Frohlich GM, Lansky AJ, Webb J, Roffi M, Toggweiler S, Reinthaler M, Wang D, Hutchinson N, Wendler O, Hildick-Smith D, Meier P.Local versus general anesthesia for transcatheter aortic valve implantation (TAVR)—systematic review and meta-analysis. BMC Med 2014;12:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Durand E, Eltchaninoff H, Canville A, Bouhzam N, Godin M, Tron C, Rodriguez C, Litzler P-Y, Bauer F, Cribier A.. Feasibility and safety of early discharge after transfemoral transcatheter aortic valve implantation with the Edwards SAPIEN-XT prosthesis. Am J Cardiol 2015;115:1116–1122. [DOI] [PubMed] [Google Scholar]
- 8.Giri J. Moderate vs. general anesthesia for transcatheter aortic valve replacement: an STS/ACC transcatheter valve therapy registry analysis. SCAI 2016; Orlando, FL 2016.
- 9. Villablanca Pedro A, Nikolic K, Vucicevic D, Maldonato Y, Augoustides John G, Ramakrishna H.. Abstract 15166: Comparison of general versus local anesthesia in patients undergoing transcatheter aortic valve replacement (TAVR): a meta-analysis. Circulation 2016;134:A15166–A. [Google Scholar]
- 10. Alqahtani F, Bhirud A, Aljohani S, Mills J, Kawsara A, Runkana A, Alkhouli M.. Intracardiac versus transesophageal echocardiography to guide transcatheter closure of interatrial communications: Nationwide trend and comparative analysis. J Interven Cardiol 2017;30:234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alkhouli M, Hijazi ZM, Holmes DR Jr, Rihal CS, Wiegers SE.. Intracardiac echocardiography in structural heart disease interventions. JACC Cardiovasc Interv 2018;11:2133–2147. [DOI] [PubMed] [Google Scholar]
- 12. Frangieh AH, Alibegovic J, Templin C, Gaemperli O, Obeid S, Manka R, Holy EW, Maier W, Lüscher TF, Binder RK.. Intracardiac versus transesophageal echocardiography for left atrial appendage occlusion with watchman. Catheter Cardiovasc Interv 2017;90:331–338. [DOI] [PubMed] [Google Scholar]
- 13. Berti S, Paradossi U, Meucci F, Trianni G, Tzikas A, Rezzaghi M, Stolkova M, Palmieri C, Mori F, Santoro G. Periprocedural intracardiac echocardiography for left atrial appendage closure: a dual-center experience. JACC Cardiovasc Interv 2014;7:1036–1044. [DOI] [PubMed] [Google Scholar]
- 14. Enriquez A, Saenz LC, Rosso R, Silvestry FE, Callans D, Marchlinski FE, Garcia F.. Use of intracardiac echocardiography in interventional cardiology. Circulation 2018;137:2278–2294. [DOI] [PubMed] [Google Scholar]
- 15. Bartel T, Bonaros N, Edlinger M, Velik-Salchner C, Feuchtner G, Rudnicki M, Müller S. Intracardiac echo and reduced radiocontrast requirements during TAVR. JACC Cardiovasc Imaging 2014;7:319–320. [DOI] [PubMed] [Google Scholar]
- 16. Patzelt J, Ulrich M, Magunia H, Sauter R, Droppa M, Jorbenadze R, Becker AS, Walker T, von Bardeleben RS, Grasshoff C, Rosenberger P, Gawaz M, Seizer P, Langer HF.. Comparison of deep sedation with general anesthesia in patients undergoing percutaneous mitral valve repair. J Am Heart Assoc 2017;6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779052/. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.