Abstract
Background
Acquired coronary cameral fistula is an extremely rare condition that involves an abnormal communication between a coronary artery and a cardiac chamber. It usually occurs after chest trauma or cardiovascular interventions, such as percutaneous coronary intervention (PCI) and is associated with various outcomes, ranging from a stable status to haemodynamic instability. Acquired coronary cameral fistula frequently arises from the right coronary artery and drains generally into the right ventricle.
Case summary
We report the unusual case of a 56-year-old male patient referred to an invasive cardiology centre for a suspected left anterior descending (LAD) coronary–left ventricular (LV) fistula resulting from a primary PCI for an anterior ST-elevation myocardial infarction. Here, the confirmed LAD–LV fistula was successfully treated by retrograde PCI with covered stent implantation. Clinical and angiographic outcomes were favourable at 1-month follow-up.
Discussion
Coronary cameral fistula can be a severe complication of primary PCI. Various treatment strategies can be considered based on haemodynamic status and anatomical features. In the case described herein, the use of a retrograde approach led to permanent fistula closure and complete revascularization.
Keywords: Case report, Coronary cameral fistula, Percutaneous coronary interventions, Retrograde approach
Learning points
Coronary cameral fistulae are unusual complications of percutaneous interventions.
They consist in an abnormal communication between a coronary artery and a cardiac cavity potentially caused by guidewire-induced perforation, overexpansion of a coronary segment or inappropriate wire-tracking.
Retrograde approach can be helpful for fistula closure when it is necessary to cross a stent implanted towards the fistulized branch.
Introduction
Coronary cameral fistula was first described by Cayla in 1885. It consists in an abnormal communication between one or several coronary arteries and a cardiac cavity (generally the right ventricle). This condition is mainly congenital but it can also result from chest trauma or invasive cardiac procedures.1 This report describes the case of a patient treated with primary percutaneous coronary intervention (PCI) during which procedural complications resulted in a left anterior descending (LAD)–left ventricular (LV) fistula. The patient was then transferred to an invasive cardiology centre where successful management of the fistula was obtained by the retrograde implantation of a covered stent on the mid-LAD artery—the origin of the fistulized septal branch.
Timeline
| Initial procedure | Anterior ST-elevation myocardial infarction with percutaneous coronary intervention (PCI) failure complicated by coronary cameral fistula. Patient haemodynamically stable transferred to an invasive centre with on-site cardiac surgery. |
| 6 h post-procedure | Angiographic control showing a large septal branch fistula spraying in the left ventricle and an occluded mid-left anterior descending (LAD). |
| Day 1 post- procedure | Successful PCI with LAD retrograde crossing and covered stent placement at the origin of the fistulized septal branch. |
| Day 4 post- procedure | Discharged from the hospital. |
| 1 month after procedure | Follow-up with no angina symptoms, preserved ejection fraction and good angiographic result. |
Case presentation
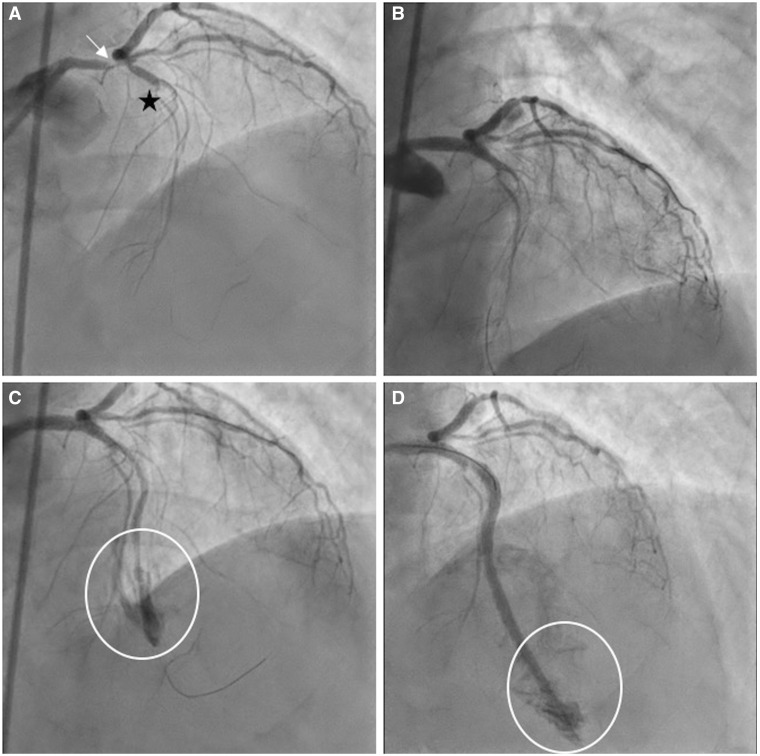
A 56-year-old male patient was admitted to the cathlab for an anterior ST-elevation myocardial infarction (STEMI) after presenting ventricular fibrillation treated by external defibrillation during ambulance transport. His medical history was limited to moderate hyperlipidaemia without medication. On admission, the patient was afebrile with a heart rate of 65 b.p.m. and blood pressure of 135/60 mmHg. Physical examination revealed a Killip Class II with bilateral basal lung crackles without further abnormalities. The electrocardiogram recorded a significant ST-segment elevation in antero-lateral leads and a ST-segment depression in inferior leads. An emergency coronary angiography showed a severe stenosis of the distal left main coronary artery and an occlusion of the mid-LAD (Figure 1A, Supplementary material online, Video S1). A PCI was initially performed in the left main and ostial LAD (Figure 1B, Supplementary material online, Video S2). Then, a distal balloon inflation induced a contrast extravasation (Figure 1C, Supplementary material online, Video S3), treated with the bailout implantation of two covered stents and a drug-eluting stent (DES). The final angiographic control showed a potential coronary cameral fistula (Figure 1D, Supplementary material online, Video S4). The patient was haemodynamically stable, with no pericardial effusion or arrhythmia. He was thus referred to a high-volume centre with on-site cardiac surgery facilities.
Figure 1.
Primary emergency coronary angiography. (A) Severe stenosis of the distal left main coronary artery (white arrow) and occlusion of the mid left anterior descending (black asterisk). (B) Result of the left main percutaneous coronary intervention. (C) Contrast extravasation following balloon inflation (circle shows the contrast extravasation). (D) Final result with suspected coronary cameral fistula (circle shows the contrast extravasation into a heart cavity).
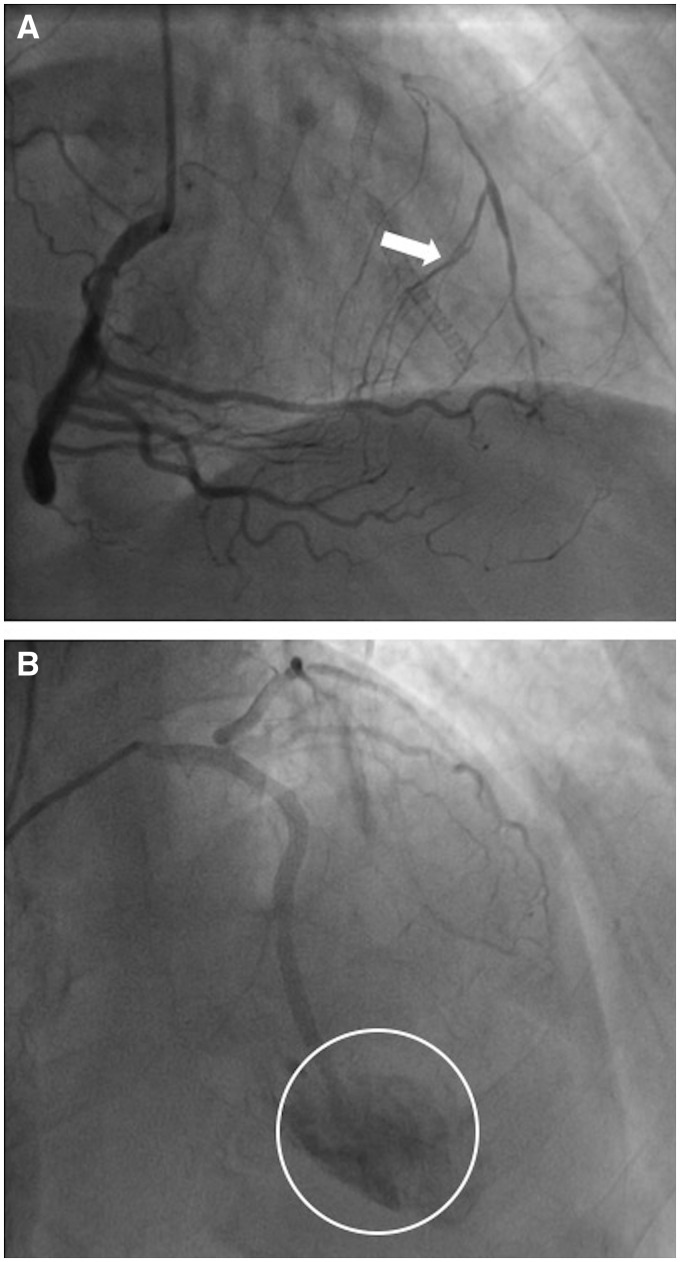
At admission, the patient remained asymptomatic. The electrocardiogram showed no Q waves, and displayed negative T waves in the lateral leads (Supplementary material online, Figure S1). A control coronary angiography revealed a luminal narrowing of the ostial segment of the left main coronary artery, a patent stent extending from the left main to the proximal LAD, multiple stents in a septal branch with an iatrogenic LAD–LV fistula and an occluded mid-LAD supplied by collaterals arising from the right coronary artery (RCA) (Figure 2A and B, Supplementary material online, Videos S5–S7). This confirmed that balloon inflation and bailout PCI performed during the first procedure were carried out erroneously in the main septal branch. The Heart Team strategy was thus to attempt a percutaneous myocardial revascularization of the LAD, and a fistula closure.
Figure 2.
Control coronary angiography after transfer to an invasive centre. (A) Mid left anterior descending occlusion supplied by septal collaterals channels from right coronary artery (large white arrow). (B) Selective left coronary angiography showing leakage of contrast into the left ventricle, confirming the diagnosis of left anterior descending–left ventricular fistula (circle shows the contrast leakage).
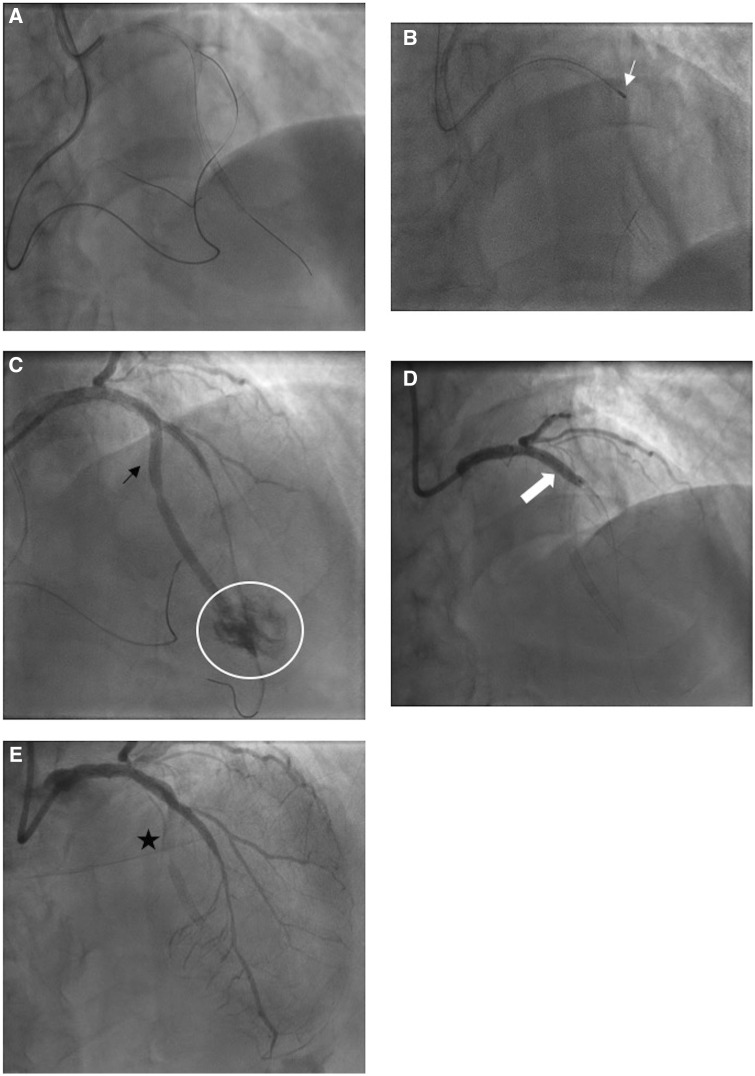
First, a bilateral radial approach was performed with 6 Fr guiding catheters, allowing a retrograde crossing through a septal collateral with a Caravel™ (Asahi Intecc, Aichi, Japan) microcatheter and a Gaïa second™ (Asahi Intecc, Aichi, Japan) guidewire (Figure 3A). Then, an antegrade rotational atherectomy was performed with the Rotablator™ system (Boston SC, Natick, MA, USA) and a 1.25 mm burr in order to ablate the stent struts and to perform a balloon inflation, followed by a DES implantation in the mid-LAD (Figure 3B).
Figure 3.
Percutaneous revascularization and fistula closure at Day 1 following ST-elevation myocardial infarction. (A) Retrograde wiring through a septal collateral from the right coronary artery. (B) Rotational atherectomy with a 1.25 mm burr through the stent struts (white arrow shows the burr). (C) Heavy blood flow through the septal-left ventricular fistula decreasing significantly the flow through the left anterior descending (black arrow shows a persistent flow through the septal and circle shows the leakage into the left ventricle). (D) Covered stent implantation at the origin of the fistulized septal branch (large white arrow shows the inflated covered stent). (E) Final result demonstrating a successful percutaneous coronary intervention of the mid-left anterior descending and an occluded coronary cameral fistula (black asterisk).
Angiographic views showed a successful opening of the LAD but a persistent competitive flow through the iatrogenic septal LAD–LV fistula, which could induce a coronary steal and a stent thrombosis in the LAD (Figure 3C). The decision was thus made to attempt a closure of the fistula. The initial attempt at vascular plug delivery in the fistula failed, and the significant competitive flow was successfully occluded by the insertion of a PK Papyrus™ (Biotronik, Berlin, Germany) covered stent (Figure 3D). Final angiographic views showed an excellent management of the LAD lesion and a thrombolysis in myocardial infarction (TIMI) III flow (Figure 3E).
The patient was still asymptomatic, with normalization of T-waves inversion on the electrocardiogram (Supplementary material online, Figure S2) and normal renal function. T Troponin reached a peak of 3140 ng/L (N < 14). Transthoracic echocardiography showed a preserved LV ejection fraction at 55%, with an anterolateral hypokinesis (Supplementary material online, Video S8). The patient was discharged three days later, on dual antiplatelet therapy with aspirin and ticagrelor as well as statin, beta-blockers, and angiotensin-converting enzyme inhibitors.
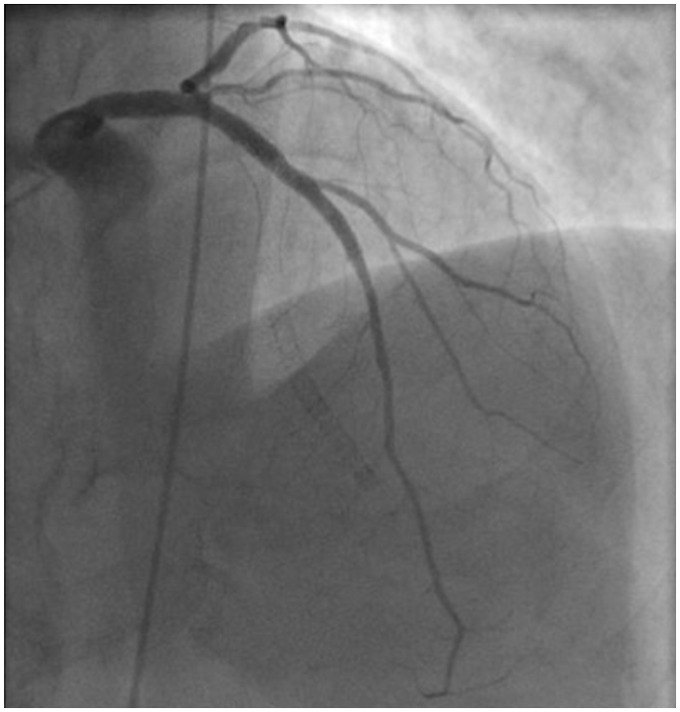
At 1-month follow-up, he remained asymptomatic. A control angiography showed patent stents on the left main and LAD coronary artery, with a totally occluded coronary cameral fistula (Figure 4, Supplementary material online, Video S9).
Figure 4.
Control coronary angiography performed at 1-month follow-up, showing a persistent occlusion of the fistula and a successful revascularization of the left anterior descending.
Discussion
Acquired coronary cameral fistula (ACCF) is an extremely rare complication of PCI. Potential causes of ACCF include guidewire-induced perforation, overexpansion of a coronary segment, and improper wire-tracking.2 Considering the rarity of ACCF, no clear consensus about the management of this condition has been reached to date. It is a case-based decision depending on the underlying aetiology and its severity. Some of these fistulae tend to close spontaneously. Regarding larger ACCF, which can lead to coronary steal syndrome, closure management procedures include a prolonged balloon inflation, coil or vascular plug embolization, and surgery.3
Various management strategies were described in the literature.4 Most of the cases described in past reports concern the surgical correction of primary coronary cameral fistula of congenital aetiology.5,6 More recently, Yu et al.7 described the spontaneous closure of a secondary RCA–RV fistula, and Mertens et al.8 reported the case of an acquired LAD–RV fistula treated with coil embolization. The case presented herein is the first report of an iatrogenic LAD–LV fistula successfully occluded by retrograde wiring and covered-stent angioplasty.
Our case shows how the initial mispositioning of the guidewire can lead to a severe complication. Indeed, during the initial procedure, the first septal branch was confused with the LAD and the first balloon inflation probably provoked the dissection and/or rupture of the septal branch that was treated with the implantation of three stents. This procedure eventually led to the perforation of the septal branch into the LV chamber. In order to confirm the proper positioning of the guidewire—and thus, avoid the complication described here—two options could have been considered: the use of different angiographic projections, including lateral views, and the use of a tip injection from a microcatheter or a thrombo-aspiration catheter.
Here, a retrograde approach was preferred, considering the presence of interventional collaterals and in order to allow a safe crossing of the stent implanted towards the first septal. Indeed, an antegrade approach would have required to use stiffer guidewires, with an increased risk of LAD perforation or dissection.
Conclusion
Acquired coronary cameral fistula is an unusual but potentially severe complication of PCI, particularly in the setting of STEMI. Since no recommendations are available concerning the management of ACCF, the appropriate treatment should be determined on an individual basis, based on haemodynamic status and anatomical features. This report describes the first case of an iatrogenic LAD–LV fistula resulting from the complications of a primary PCI procedure that was successfully occluded by retrograde wiring with placement of a covered stent.
Lead author biography
Dr Paul Ohayon is an interventional cardiologist who specializes in complex and high-risk coronary interventions. He received his MD from Toulouse Paul Sabatier University, France. He completed his cardiovascular medicine residency and interventional cardiology fellowships in Toulouse University Hospital. He is currently participating in a dedicated training at Montreal Heart Institute in complex and high-risk interventional procedures. He also holds a MS in Cardiovascular Physiology from Toulouse Paul Sabatier University with a research interest focused on novel therapeutics in interventional cardiology.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: N.B. is proctor in CTO‐PCI for BIOTRONIK. All other authors have no conflict of interest to declare.
Supplementary Material
References
- 1. Serratto M, Kezdi P.. Congenital coronary artery-right ventricular fistula corrected surgically. Br Heart J 1965;27:781–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oh SW, Kim YJ, Lim JG, Choi WG.. An iatrogenic coronary arteriovenous fistula caused by guidewire trauma during percutaneous coronary intervention. Korean J Med 2012;82:337. [Google Scholar]
- 3. Javaid A, Buch AN, Satler LF, Kent KM, Suddath WO, Lindsay J, Pichard AD, Waksman R.. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2006;98:911–914. [DOI] [PubMed] [Google Scholar]
- 4. Park S-H, Rha S-W, Cho A-R, Lee H-G, Choi C-U, Oh D-J.. Successful management of iatrogenic coronary arteriovenous fistula developed during chronic total occlusion intervention. J Cardiol Cases 2012;6:e96–e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abrams LD, Evans DW, Howarth FH.. Coronary artery–right ventricular fistula treated surgically. Br Heart J 1967;29:132–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morgan JR, Forker AD, O'Sullivan MJ, Fosburg RG.. Coronary arterial fistulas: seven cases with unusual features. Am J Cardiol 1972;30:432–436. [DOI] [PubMed] [Google Scholar]
- 7. Yu X, Wang X, Zhang R, Xu F, Ji F.. Spontaneous closure of an iatrogenic coronary artery fistula during recanalization of a chronic total occlusion lesion: A case report. Medicine 2019;98:e14068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mertens A, Dalal P, Ashbrook M, Hanson I.. Coil embolization of coronary-cameral fistula complicating revascularization of chronic total occlusion. Case Rep Cardiol 2018;2018:6857318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.