Abstract
Background
Troponin is a crucial biomarker for the diagnosis of an acute coronary syndrome (ACS). It rises in response to myocardial injury from significant acute myocardial ischaemia caused by obstructive coronary artery disease [‘classical’ myocardial infarction (MI)]. However, raised levels have also been noted in conditions not recognized as classical ACS. This may include MI with non-obstructed coronary arteries such as takotsubo cardiomyopathy and other acute or chronic conditions such as pulmonary embolus or chronic kidney disease. This is commonly labelled as a ‘falsely elevated’ troponin although there is some myocardial strain to explain the rise, such as an increase in cardiac oxygen demand. True ‘falsely elevated’ troponin, characterized by a persistent elevation in the absence of cardiac injury does occur and thought to be secondary to an immunoglobulin-troponin complex (macrotroponin).
Case summary
A 53-year-old gentleman with a background of diabetes, hypertension, hypercholesterolaemia, and hepatitis B was admitted with chest pain and persistently elevated cardiac troponin T (cTnT) levels. Investigations revealed unobstructed coronary arteries and a structurally normal, well-functioning heart. Subsequent biochemical analysis found the persistently elevated cTnT secondary to macrotroponin T.
Discussion
Macrotroponin, an immunoglobulin-troponin bound complex should be considered as a differential diagnosis when the biochemistry is not reflective of the clinical picture. Early recognition requires effective collaboration with the biochemistry laboratory for accurate diagnosis.
Keywords: Case report, Macrotroponin, Falsely elevated troponin, Biochemistry
Learning points
A thorough review of the case is indicated when the biochemistry does not reflect the clinical picture.
Close collaboration between the clinicians and the clinical biochemistry laboratory is vital in establishing an early diagnosis of a falsely elevated troponin level.
Falsely elevated troponin levels due to an immunoglobulin-G-cardiac complex should be a differential diagnosis when the troponin levels do not reflect the clinical picture.
Introduction
The measurement of cardiac troponin as cardiac troponin T (cTnT) or cardiac troponin I (cTnI) is integral to the diagnosis of acute myocardial infarction (AMI) and is included as the cornerstone of the universal definition of AMI.1 Elevation of cardiac troponin also occurs in a large number of clinical conditions associated with acute or chronic myocardial injury but which are not classical AMI.1,2 These may include myocardial infarction (MI) with non-obstructed coronary arteries such as coronary vasospasm, pulmonary embolus, sepsis, and chronic causes such as chronic kidney disease or structural heart disease.1,2 Although these are often referred to as ‘false positive’, this is not in fact the case as there is underlying myocardial injury.1 However, a true ‘false positive’ troponin rise does occur which is characterized by a persistent elevation in the absence of myocardial injury and needs to be recognized by clinicians.
Timeline
| Day 0 | Admission to cardiology with assumed ACS diagnosis [after computed tomography (CT) aortagram] | Troponin T 1588 (ng/L) |
| Day 1 | Echocardiogram demonstrated well-functioning heart with no regional wall motion abnormalities | Troponin T 1842 (ng/L) |
|
Day 2 |
Coronary angiogram reveals unobstructed coronary arteries |
Troponin T 1690 (ng/L) |
| Day 4 | Cardiac MRI performed revealing a structurally normal heart and no evidence of scar | Troponin T 1789 (ng/L) |
| Day 5 | Biochemistry lab contacted to elucidate cause of persistently elevated troponin | Troponin T 1684 (ng/L) |
| Day 8 | Troponin I found to be normal and macrotroponin complex confirmed | Troponin T 1697 (ng/L) |
Case presentation
A 53-year-old south Asian male presented to the accident and emergency department with an extended history of chest pain and numbness in the left arm lasting more than 24 hours. His symptoms had initiated whilst driving but resolved on arrival to hospital. There were no abnormal findings on clinical examination (heart rate 65 b.p.m., blood pressure 108/76 mmHg, saturations 98% on air, respiratory rate 16 cycles per minute).
His medical background included type 2 diabetes (2013), hypertension (2014), hypercholesterolaemia (2002), non-alcoholic steatohepatitis (2002), and hepatitis B (2002). The patient had two prior admissions with cTnT positive chest pain, in 2002 (1410 ng/L) and 2015 (1540 ng/L), during which coronary angiography demonstrated unobstructed coronary anatomy and a diagnosis of probable myocarditis was given on each occasion.
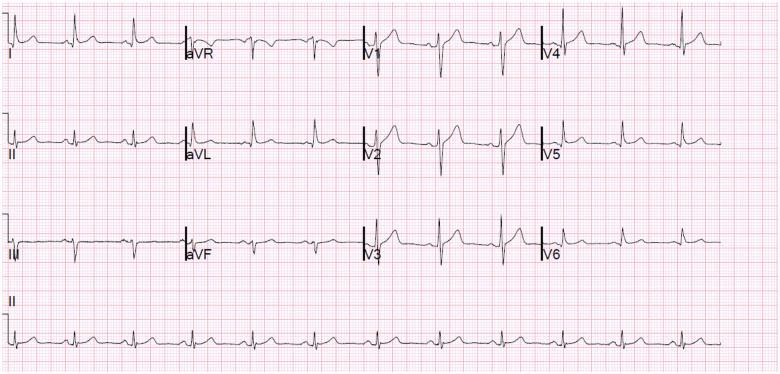
An electrocardiogram (ECG) on admission demonstrated no ischaemic changes (Figure 1). However, an initial cTnT was raised at 1588 ng/L (normal range <15 ng/L) and 1842 ng/L when repeated. This was in the context of a normal renal function [creatinine 102 (normal 62–106 μmol/L)] and a normal haemoglobin (137 g/L). Subsequent serial troponins did not drop below 1600 ng/L (timeline). Due to this stagnation, a creatine kinase level was measured and found to be only borderline raised at 338 U/L (normal 40–320 U/L). An echocardiogram was also performed which showed no regional wall motion abnormalities and a preserved left ventricular ejection fraction of 60–65%.
Figure 1.
Electrocardiogram on admission demonstrating no ischaemic changes.
Owing to the patient’s clinical picture, a CT aortagram was performed which excluded an aortic dissection and within its limits, a pulmonary embolus. Thus, a working diagnosis of acute coronary syndrome was suggested and he underwent a coronary angiogram. This showed only mild disease in the right coronary artery (Supplementary material online, Video S1) and left anterior descending (Supplementary material online, Video S2) whilst the left main stem and circumflex vessels (Supplementary material online, Video S3) were unobstructed. Subsequently a cardiac MRI with gadolinium was performed which was unremarkable and confirmed preserved bi-ventricular function (Supplementary material online, Videos S4 and S5) with no evidence of a scar, fibrosis, or oedema (Supplementary material online, Video S6). Acute myocardial injury was therefore considered unlikely. Furthermore, he remained on telemetry and despite 7 days of cardiac monitoring, no arrhythmia was documented. After extensive investigations had excluded myocardial damage and any other clinical condition as a likely cause of the troponin elevation, the biochemistry laboratory was contacted for assistance in elucidating the cause of the persistently elevated cTnT.
Initially, a measurement of cTnI was performed (Abbott diagnostics hs cTnI, LOD 2 ng/L 10% CV = 4.7 ng/L, 99th percentile URL = 26.2 ng/L) on the cTnT sample value 1674 ng/L, and was <2 ng/L, therefore excluding myocardial injury. Analytical interference causing a false-positive cTnT result was then suspected.
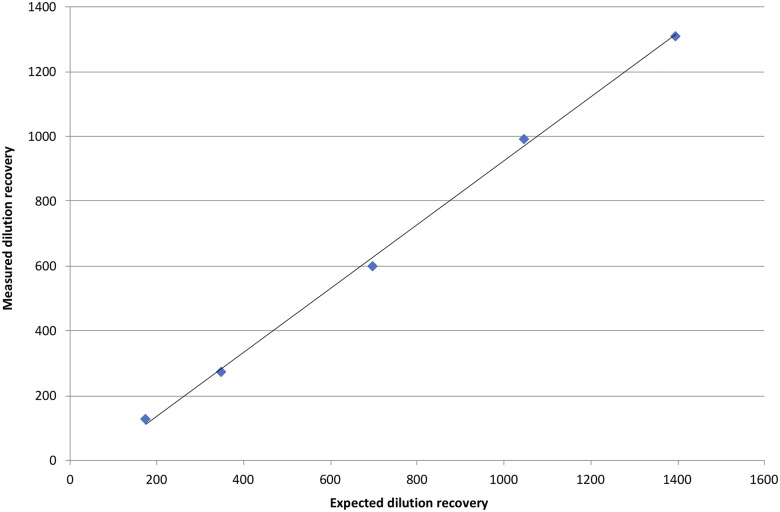
Serial dilution of the sample using troponin free diluent was linear (Figure 2) (recovery sample 73.1–94.7%, control 81.5–109.2%) although recovery at a one in 10 dilution was <100% compared with the control. This suggested that an analytical interference from an interfering antibody (anti-mouse) was unlikely. The Roche cTnT assay uses fragment antigen binding portions of 2 cTnT-specific mouse monoclonal antibodies (MAbs) directed against epitopes in the central region of human cTnT.
Figure 2.
Graph demonstrating linear dilution of the patient’s cTnT sample of 1745 ng/L in keeping with a likely macrotroponin causing an analytical interference.
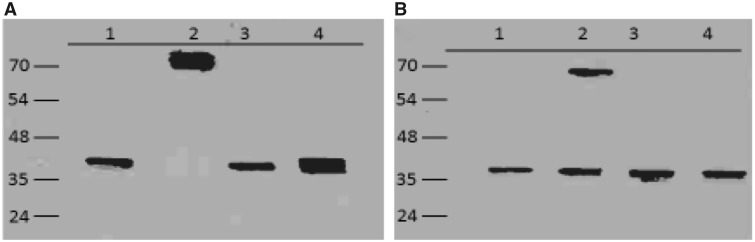
One control (Randox IA3, Randox, County Antrim), two control patients (cTnT 2091 and 1637 ng/L) and two patient samples (cTnT 1745 and 1697 ng/L) were diluted one in two with troponin free diluent and with polyethylene glycol (25% w/v). Samples were incubated at room temperature for 10 minutes and centrifuged at 14°000 g for 5 min. Troponin T was analysed in the supernatant. Recovery was 705.8/1104 (63.9%) for the control material. For two control patient’s recovery was 687/807.4 (85.1%) and 910/963.4 (94.5%). For the patient’s day 4 sample recovery was 10.8/794.4 (1.4%) and for day 5 8.7/770.3 (1.1%). The presence of a macro form of cTnT was therefore confirmed. Subsequent electrophoresis using sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and western blotting (immunofixation) with the M7 MAb anti-human cTnT (donated by Roche Diagnostics, Mannheim, Germany) against human cTnT and mouse anti-human immunoglobulin-G (IgG; IG266, Abcam, Cambridge, UK) revealed a cTnT-IgG complex (Figure 3).
Figure 3.
(A) Western blot of cTnT demonstrating intact free cTnT (lane 1) serum from index case (lane 2), serum from cTnT positive patients (lanes 3 and 4). (B) Western blot of Human IgG control (lane 1), index case (lane 2) cTnT positive patients (lanes 3 and 4).
Following this diagnosis, reassurance was given and he was discharged home with routine follow-up arranged. A subsequent outpatient 24-hour Holter demonstrated only sinus rhythm, which reaffirmed the unlikelihood of a cardiac arrhythmia and a dobutamine stress echocardiogram found no evidence of inducible ischaemia with a normal functioning heart. He was safely discharged from the cardiology services.
Discussion
Cardiac troponin is integral to the diagnosis of a myocardial infarction. Troponin rise from a MI occurs due to cardiac injury from acute cardiac ischaemia, although elevated levels are also seen in acute or chronic conditions not recognized as classical MI.1,2 This is often referred to as a ‘false positive’ rise, which is not entirely true as there is some underlying cardiac injury. The mechanism of injury may include a rise in cardiac oxygen demand, oxygen demand/supply mismatch,3 and the fourth universal definition of MI addresses this by distinguishing myocardial injury from MI.4 Interestingly, true analytical false positives do occur which are thought to be secondary to macrotroponin, an IgG complex attached to the troponin protein.5
In a clinical setting, elevation of cTnT due to macrotroponin appears to be relatively uncommon and more frequently seen with cTnI than cTnT.5 However, the overall prevalence of macrotroponins may be more common than currently reported by clinicians. For instance, cTnT autoantibodies have been found in up to 9.9% of healthy blood donors6 and similarly, cTnI autoantibodies have been found in up to 12.7%.7 This is comparable with the prevalence of thyroglobulin and thyroperoxidase antibodies, which are commonly encountered in clinical practice.7 It is therefore probable that the rise in troponin levels attributed to clinical conditions other than MI, could actually be due to macrotroponins.
This case illustrates the importance of clinical assessment of patients admitted where the laboratory findings do not match the clinical state of the patient and the importance of close collaboration with the clinical chemistry laboratory. A significantly elevated troponin in an otherwise well individual should raise the suspicion of an analytical interference. The clue in this case was the sustained elevation in the absence of any other clinical condition likely to produce an elevated troponin of this magnitude. This led to an alternative troponin being measured which was normal and subsequently, to the diagnosis of the macrotroponin.
From this experience, it could be suggested that clinicians facing a persistently elevated troponin with an atypical history and lack of evidence suggestive of cardiac injury (ECG, echocardiography), should consider measurement of an alternative troponin. Invasive investigations could be avoided unless the history is suggestive of another clinical condition causing the rise. The important thing is to recognize the lack of a dynamic change and lack of comorbidities likely to produce a significant troponin elevation.
Conclusion
This case illustrates the importance of interpreting a troponin result in the clinical context of the patient and underlines the importance of clinical assessment of the patient. It also highlights the dangers of over-reliance on uncritical acceptance of laboratory results. True false-positive elevations of cardiac troponin from macrotroponins do occur, though they are rare. Cases of macrotroponin I have been reported in the literature, however, our case is the earliest description of a falsely elevated troponin secondary to troponin T autoantibodies in a clinical setting.
Lead author biography
Zaki Akhtar graduated from St George's University of London in 2011 having completed his medical course and a bachelor's degree in Physiology from King's College London. Currently he is a research fellow at St George's Hospital, London.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;76:1383–1415.30689804 [Google Scholar]
- 2. Eggers KM, Jernberg T, Lindahl B.. Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol 2019;73:1–9. [DOI] [PubMed] [Google Scholar]
- 3. Lefort G, D'Antonio C, Caffery T.. A non-ischaemic cause of elevated troponin; BMJ. Case Rep 2014;2014:bcr2014203729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Collinson P, Lindahl B.. Type 2 myocardial infarction: the chimaera of cardiology? Heart 2015;101:1697–1703. [DOI] [PubMed] [Google Scholar]
- 5. Michielsen EC, Bisschops PG, Janssen MJ.. False positive troponin result caused by a true macrotroponin. Clin Chem Lab Med 2011;49:923–925. [DOI] [PubMed] [Google Scholar]
- 6. Adamczyk M, Brashear RJ, Mattingly PG.. Prevalence of autoantibodies to cardiac troponin T in healthy blood donors. Clin Chem 2009;55:1592–1593. [DOI] [PubMed] [Google Scholar]
- 7. Adamczyk M, Brashear RJ, Mattingly PG.. Circulating cardiac Troponin-I autoantibodies in human plasma and serum. Ann N Y Acad Sci 2009;1173:67–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.