Abstract
Background:
Adolescents and young adult (AYA) cancer survivors have high risks of late effects. Little is known about AYA late effect information needs early in treatment or their role in treatment decision-making. We evaluated the importance, quality, and implications of information about late effects in AYAs recently diagnosed with cancer.
Methods:
We surveyed 201 AYAs with cancer age 15–29 years, treated at Dana-Farber Cancer Institute, Boston, MA. Patients were approached within 6 weeks of diagnosis and asked about their late effect and infertility information needs, treatment decision-making, and communication outcomes.
Results:
45% of participants were female; 88% were white. Most AYAs (87%, 174/201) considered information about the risks of late effects to be extremely or very important; 80%(159/201) valued information about infertility. Many were distressed by information about late effects (53%, 105/201) and infertility (45%, 90/201); those who considered late effects information distressing were more likely to value this information (P<0.0001). Consideration of late effects (41%, 82/202) and infertility (36%, 72/202) greatly influenced many patients’ treatment decision-making. Whereas 92% (184/199) of patients reported receiving high-quality information about diagnosis, 57%(113/199, P<0.0001) felt they received high-quality information about late effects, and 65%(130/199, P<0.0001) about infertility.
Conclusions:
Most AYAs with cancer value early information about risks of late effects and infertility, yet many patients felt they did not receive high-quality information about these topics. Development of age-appropriate late effect communication strategies that recognize high AYA distress may help address the gap between desired information and perceived information quality.
Keywords: Adolescent/Young Adult (AYA), Cancer, Late effects, Health-care communication, Infertility
Precis:
Most AYAs with cancer in the current study value early information about risks of late effects and infertility, in part as they find it important to their treatment decision-making. Yet, many patients are distressed by information about the long-term risks of cancer treatment and report receiving sub-optimal information about these topics.
Introduction:
More than 70,000 adolescents and young adults (AYAs) are diagnosed with cancer annually in the United States, and over 80% of AYAs with cancer become long-term survivors.1 However, cancer and its treatments can cause many late effects that may impair quality of life after completion of therapy. Approximately 60% of childhood and adolescent cancer survivors experience at least one late effect of treatment, and over a quarter of survivors experience a severe or life-threatening chronic health condition.2 AYAs with cancer may even be at greater risk of particular late effects, such as cardiac toxicity and second malignancies, compared with childhood cancer survivors.3 Risks of late effects are typically briefly reviewed in initial informed consent discussions,4 but the majority of late effects counseling occurs at the completion of therapy and in survivorship.5 AYA early information needs and preferences about the potential long-term implications of cancer and its treatments are not well known.
AYAs with cancer are a particularly vulnerable population. Consistent with their stage in human development, they have variable abilities to see long term implications of present actions, understand health risk, and make complex decisions.6 These variabilities have profound implications for their decision-making at the overwhelming time of a new cancer diagnosis. Most AYA patients with cancer desire information about their prognosis and what to expect for their life after cancer therapy,7,8 and many children and adolescents with cancer want to be involved in treatment decision-making.9,10 Yet, AYAs with cancer have substantial unmet information needs regarding possible late effects of cancer treatment and infertility within the first two years after diagnosis.11 Furthermore, many AYA cancer survivors are unaware of their risks of late effects,12 and many report unmet information needs about late effects of cancer which may impact their engagement in survivorship screening and care, as well as their long term quality of life and psychosocial well-being.13–15
We surveyed AYA patients, 15 to 29 years of age, who were newly diagnosed with cancer at a large academic cancer center to evaluate the role and value of information about risks of late effects and infertility early in treatment. In prior work evaluating late effect information preferences and experiences of parents of children with cancer, we found that many parents find this information distressing but valuable.16 We applied similar measures to evaluate AYA late effect information needs. We hypothesized that AYAs with cancer would consider late effects information important, though distressing to learn about. Despite the importance of this information, we hypothesized that late effects might have a limited role in treatment decision-making as AYAs may be more focused on the present treatment than their future survivorship.
Materials and Methods:
We surveyed AYA patients with cancer ages 15–29 years at diagnosis at Dana-Farber Cancer Institute (DFCI), Boston, Massachusetts, between April 2014 and November 2018. Eligible patients were identified sequentially from pediatric and medical oncology clinics using clinic and medical records. Permission to approach a patient was sought from the patient’s primary oncologist, and oncologists completed a question on the patient’s prognosis when providing permission. Patients were approached about participation 1 to 6 weeks after diagnosis, and only baseline surveys returned within 12 weeks of diagnosis were included.8,17
Eligible participants were approached in person during clinic visits or by mail, with a letter describing participation, the questionnaire, and a postage-paid opt-out postcard. Participants who did not respond initially were approached up to two more times in person or by mail. Surveys were offered in paper or electronic format via tablet or remotely via a secure link. Participants who completed the baseline questionnaire were invited to complete follow-up questionnaires at 4 and 12 months after diagnosis. Participating patients received a $50 gift card as an incentive to participate. Patient assent and parent/guardian signed informed consent were obtained for patients <18. Documentation of informed consent was waived for patients >18. The DFCI institutional review board approved this study.
Questionnaires mostly consisted of previously developed items.8,18,19 Limited new items were developed based on literature review, patient interviews, and prior work; new items underwent pilot-testing for conceptual, face, and content validity with 11 AYA patients.8 We assessed infertility separately from other late effects because AYAs may have distinct concerns about fertility as compared with other health effects, and because patients often have options for pre-treatment fertility preservation.20,21 Surveys took 30–40 minutes to complete.
Study Outcomes:
The primary outcomes for this analysis were the importance of knowing about the likelihood of late effects generally, and of infertility specifically, which were assessed using previously utilized items.16,22 Participants were asked the importance of knowing “how likely it is that cancer or its treatment may cause health problems in the future, other than your fertility” and the importance of knowing “how likely it is that cancer or its treatment may affect your fertility (ability to have children)” with response options “extremely,” “very,” “somewhat,” “a little,” and “not at all” important.
Secondary outcomes included the quality of information received about late effects and infertility, and the influence of these factors on decision-making. Quality of information was assessed about diagnosis, treatment, prognosis, late effects, infertility, and information overall with response categories “excellent,” “good,” “satisfactory,” “fair,” “poor,” and “did not receive information.”18,23 Participants were asked how much the chance of cure, minimizing acute side effects of treatment, minimizing late effects of treatment, and minimizing the risk of infertility influenced their treatment decisions with response options “a great deal,” “somewhat,” “a little,” and “did not influence at all.” They were similarly asked, “what aspects of treatment were most important to you” when making treatment decisions about the same 4 aspects of treatment with response options “extremely,” “very,” “somewhat,” “a little,” and “not at all” important.
Explanatory factors:
We assessed the following factors we hypothesized may be associated with considering information about late effects and infertility to be important:
Prognosis: Perception of prognosis was evaluated using a previously utilized item which asked “how likely you think it is that you will be cured of cancer,” with response categories: “extremely likely (>90% chance of cure)”; “very likely (75–90%)”; “moderately likely (50–74%)”; “somewhat likely (25–49%)”; “unlikely (10–24%)”; “very unlikely (<10%)”; or “no chance of cure”.18,24,25 Responses were dichotomized as “favorable” (>75% chance of cure), or “less favorable” (<75% chance of cure) to approximate median survival estimates of AYAs with cancer.
Psychological factors: Distress associated with information about late effects and infertility was assessed with items that asked how upsetting it was “to know how likely it is that cancer or its treatment may cause health problems in the future, other than your fertility,” and “may affect your fertility (ability to have children) in the future” with response options of extremely, very, somewhat, a little, and not at all upsetting16,19. The Hospital Anxiety and Depression Scale (HADS) evaluated depression and anxiety.26
Patient characteristics: Patients were asked to report gender, race/ethnicity, educational attainment, current school/employment status, with whom they lived before diagnosis, level of financial dependence on their parent/guardian before diagnosis, and with whom they were living at the time of survey completion. Age and diagnosis were determined using medical records.
Statistical Methods:
Participant characteristics and responses to items about importance of information, information quality, and influence on decision-making were summarized descriptively. The importance of knowledge about the likelihood of late effects and infertility were dichotomized as extremely/very important vs. somewhat/a little/not at all. Information quality was similarly dichotomized as excellent/good vs. all other categories, and influence of factors on treatment decision-making was dichotomized as “a great deal” vs. all other categories. Explanatory factors were dichotomized for analysis consistent with previous work, with cutoffs specified a priori as described in tables and text.
McNemar’s test of symmetry was used to compare patient perspectives on general late effects vs. infertility with regards to importance of information, distress associated with information, and influence of factors on treatment decision-making. McNemar’s test was similarly used to compare patient perceived information quality about diagnosis versus treatment, prognosis, late effects, infertility and information overall. Bivariable logistic regression was used to investigate factors associated with valuing information about risk of late effects and infertility respectively. Statistical analyses were conducted using SAS version 9.4 (SAS Institute, NC).
Results:
Of 303 eligible patients, 275 were approached, and 203 completed the baseline survey within 12 weeks of diagnosis (67%; 203/303). Two surveys were excluded from the present analysis as the participants did not respond to the primary outcome. Of the 203 patients who completed the baseline survey, 177 completed the 4-month survey and 154 completed all 3 time-point assessments; 10 died between the baseline and 12-month surveys. One quarter of participants were 15–17 years of age (51/201), 21% were ages 18–21 (42/201), and approximately half of the participants were 22 years old or greater (108/201, 54%) [Table 1]. Many participants were living with their parents or financially dependent on their parents at the time of diagnosis (58%, 116/201), though 42% were partially or fully independent.
Table 1.
Characteristics of participating patients (N= 201)
| N(%) | |
|---|---|
| Age (years) | |
| 15–17 | 51(25) |
| 18–21 | 42(21) |
| 22–29 | 108(54) |
| Gender | |
| Female | 91(45) |
| Male | 110(55) |
| Race* | |
| White | 175(88) |
| Black/African American | 6(3) |
| Asian/Pacific Islander | 10(5) |
| Native American or Other | 12(6) |
| Ethnicity | |
| Non-Hispanic | 182(91) |
| Hispanic | 17(9) |
| Cancer Diagnosis | |
| Lymphoma | 64(32) |
| Sarcoma | 32(16) |
| Genitourinary | 29(14) |
| Leukemia | 27(13) |
| Breast | 20(10) |
| Other Extracranial Solid Tumor | 19(9) |
| Brain | 10(5) |
| Treatment Location | |
| Pediatric oncology | 73(36) |
| Medical oncology | 128(64) |
| Education | |
| Some high school | 52(26) |
| High school grad/equiv | 30(15) |
| Some college or tech | 36(18) |
| College graduate | 62(31) |
| Graduate/prof school | 21(10) |
| Financial & Living Independence (prior to dx) | |
| Living with parents or financially dependent | 116(58) |
| Living independently or partially financial independent | 85(42) |
| Patient is a parent | |
| Yes | 15(8) |
| No | 184(92) |
| Current work/school* | |
| Work full-time | 66(33) |
| Work part-time | 29(14) |
| School full-time | 59(29) |
| School part-time | 22(11) |
| No work or school outside the home | 46(23) |
| Physician-rated prognosis | |
| Favorable (≥75% chance of cure) | 111(61) |
| Unfavorable (<75% chance of cure) | 72(39) |
categories are not mutually exclusive
Missing data: race/ethnicity, N=3; physician-rated prognosis, N=18; children, N=1.
Eighty-seven percent (174/201) of patients considered information about the risks of late effects to be extremely or very important, and 80% (159/201) considered information about the risk of infertility to be important (Table 2; p=0.03 relative to information about general late effects). The importance of information about late effects and infertility did not change over the year after diagnosis. Eighty-five percent (123/144) of participants considered late effects information important at 4 months post-diagnosis (P=0.89 relative to baseline), and 82% (118/144) considered late effects information important a year after diagnosis (P= 0.94 relative to baseline). Seventy-two percent (102/142) of patients considered information about the risk of infertility important 4 months post-diagnosis (p=0.47 relative to baseline), and 73% (104/142) considered this information important at 12 months (p=0.39 relative to baseline).
Table 2.
Value of information about late effects and infertility secondary to cancer treatment and its role in treatment decision-making. *McNemar test of symmetry comparing perspectives on general late effects to those on infertility.
| General Late Effects N(%) | Infertility N(%) | P* | |
|---|---|---|---|
| Extremely/Very Important to know likelihood | 173(87%) | 159(80%) | .03 |
| Extremely/Very Upsetting to know likelihood | 105(53%) | 90(45%) | .03 |
| Influenced treatment decision-making a great deal | 82(41%) | 72(36%) | .17 |
Most AYAs considered information about the risk of late effects to be extremely or very important when making treatment decisions (78%, 155/200), and 59% (118/200) felt risk of infertility was extremely/very important to their treatment decision-making. Many AYAs reported that consideration of late effects and infertility influenced their treatment decision-making a great deal (late effects 41%, 82/202; infertility 36%, 72/202) [Table 2].
More than half (53%, 105/201) of AYAs found information about late effects to be extremely/very upsetting. Those who were distressed by information about late effects were more likely to consider this information important (p<0.0001) [Table 3]. Compared with distress about late effects information, participants were less likely to be upset by information about infertility (45%, 90/201; p=0.03). Those who were upset by information about infertility were more likely to consider this information important (p=0.0001). Distress associated with information about late effects and infertility did not vary over time.
Table 3.
Value of information and distress related to information about late effects and infertility.
| Distress related to information about late effects | |||
|---|---|---|---|
| Extremely/very N(%) | Somewhat/a little/not at all N(%) | Total | |
| Importance of information about late effects | |||
| Extremely/Very | 101(51) | 72(36) | 173(87) |
| Somewhat/a little/not at all | 4(2) | 23(12) | 27(14) |
| P<0.0001 | |||
| Distress related to information about infertility | |||
| Extremely/very | Somewhat/a little/not at all | Total | |
| Importance of information about infertility | |||
| Extremely/Very | 88(44) | 71(36) | 159(80) |
| Somewhat/a little/not at all | 1(1) | 40(20) | 41(21) |
| P<0.0001 | |||
Bivariable analyses of factors associated with considering information about late effects and infertility important are shown in Table 4. Age, sex, and prognostic understanding were not associated with differences in considering information about late effects to be important. Patients who felt they had a favorable prognosis had higher odds of considering information about infertility important relative to those with less favorable prognoses (OR 2.67, p=0.04). Older patients, those who were financially independent, and those treated by medical oncologists, were more likely to consider information about infertility important relative to younger patients (Age 22–29 relative to <18; OR 3.94, P=0.02), those who were financially dependent (Financially independent OR 2.33, P=0.03), and those treated by pediatric oncologists (Pediatric oncology OR 0.41, P=0.01).
Table 4.
Bivariable analysis of factors associated with considering information about late effects or infertility to be “extremely” or “very” important.
| Late effects information extremely/very important | Fertility information extremely/very important | |||||
|---|---|---|---|---|---|---|
| % | OR(95% CI) | P | % | OR(95% CI) | P | |
| Age (years) | ||||||
| 15–17 | 75 | Ref | 63 | Ref | ||
| 18–21 | 95 | 6.84(1.45–32.35) | .06 | 81 | 2.52(.97–6.57) | .59 |
| 22–29 | 89 | 2.74(1.15–6.53) | .93 | 87 | 3.94(1.78–8.77) | .02 |
| Sex: | ||||||
| Female | 91 | 2.17(.90–5.21) | .08 | 83 | 1.55(.76–3.14) | .23 |
| Male | 83 | Ref | 76 | Ref | ||
| Cancer Diagnosis | ||||||
| Hematologic malignancy | 86 | Ref | 86 | Ref | ||
| Solid tumor | 87 | 1.12(.49–2.55) | .88 | 87 | 1.04(.52–2.11) | .98 |
| Brain tumor | 90 | 1.50(.18–12.84) | .74 | 90 | 1.06(.21–5.39) | .97 |
| Race/Ethnicity | ||||||
| White | 87 | Ref | 80 | Ref | ||
| Non-white or Hispanic | 87 | 1.03(.36–2.92) | .96 | 76 | .76(.33–1.77) | .52 |
| Financial & Living Independence | ||||||
| Living with parents or financially dependent | 84 | Ref | 74 | Ref | ||
| Living independently/at least partial financial independence | 89 | 1.54(.66–3.7) | .31 | 87 | 2.33(1.09–5) | .03 |
| Anxiety | ||||||
| Normal | 83 | Ref | 78 | Ref | ||
| Suggestive of Anxiety | 93 | 3.01(.99–9.11) | .05 | 82 | 1.25(.58–2.72) | .57 |
| Depression | ||||||
| Normal | 85 | Ref | 80 | Ref | ||
| Suggestive of Depression | 90 | 1.54(.50–4.74) | .46 | 78 | .86(.37–2.00) | .73 |
| Patient Perceived Prognosis | ||||||
| Favorable (>75% chance of cure) | 86 | .64(.14–2.92) | .56 | 81 | 2.67(1.02–6.96) | .04 |
| Less favorable | 90 | Ref | 62 | Ref | ||
| Treatment Location | ||||||
| Medical oncology | 88 | Ref | 85 | Ref | ||
| Pediatric oncology | 84 | .68(.30–1.53) | .35 | 70 | .41(.20–.82) | .01 |
Participants reported receiving lower quality information about the risks of late effects and infertility as compared with the information they received about their diagnosis [Figure 1]. Patients reported receiving excellent or good information about their diagnosis (92%, 184/199), treatment (89%, 177/199), prognosis (87%, 173/199) and about their cancer overall (86%, 171/199). However, relative to high-quality information about diagnosis, only 57% (113/199) felt they received high-quality information about their likelihood of experiencing late effects (P<0.0001), and 65% (130/199) of participants felt they received high-quality information about their chance of infertility (P<0.0001). Nine percent (18/200) reported receiving no information about the risks of late effects of therapy, and 6% (12/200) did not recall receiving information about potential infertility.
Figure 1.
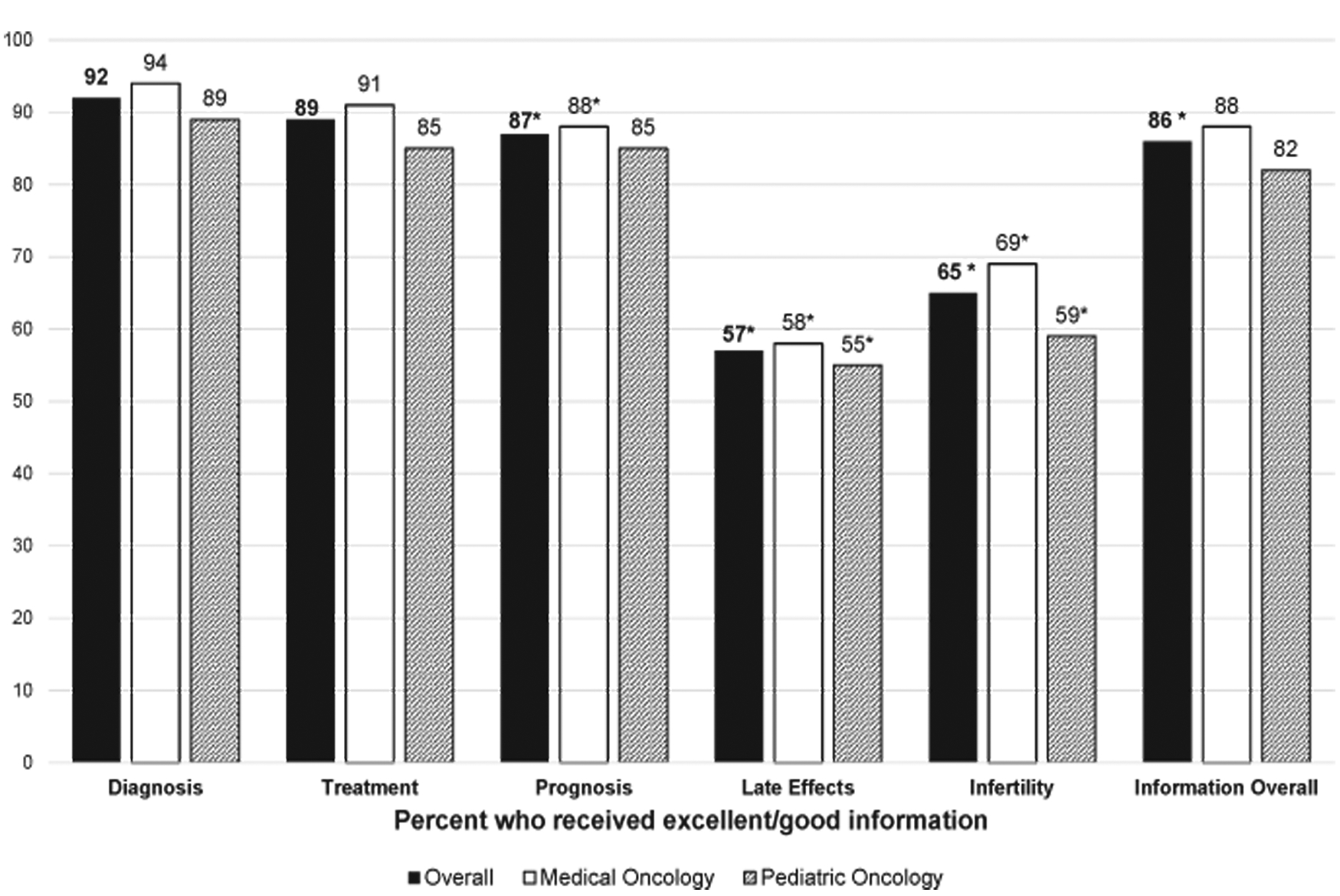
Percentage of respondents who felt they received excellent or good information. *P<0.05 using McNemar’s test of symmetry comparing quality of information in each area with quality of information about diagnosis. N=200.
Discussion:
AYAs with cancer face high risks of late effects and infertility; these late effects can be detrimental to quality of life and may delay AYAs from embarking on their independent lives.15 In this study, we evaluated the importance of late effects information to AYAs in the early treatment period, and the value of this information to treatment decision-making. We found that most AYAs consider information about risks of late effects and infertility to be very important and salient to treatment decision-making. However, many felt they received suboptimal information about these issues as compared with the generally high-quality information they received about their diagnoses.
Prior studies have shown that AYAs with cancer want to be actively involved in treatment decision-making.9,17 In this study, we found that early information about the risks of late effects and infertility plays an important role in treatment decision-making for many AYAs. However, only 57% of AYAs in our study felt they received high quality information about their risks of late effects, suggesting that some patients may have insufficient information for optimal treatment decision-making. High-quality communication and information to support treatment decision-making contributes to overall care satisfaction, whereas unmet information needs are associated with lower health-related quality of life.11,27,28 Providing up-front information about risks of late effects can empower patients to make informed decisions about their care, and may set the stage for future engagement in survivorship care and risk-based screening for late effects. Future research is needed to develop and evaluate optimal ways of providing this information at the beginning of treatment in an age appropriate manner that takes into account AYA cognitive and emotional development. However, we expect that doing so can allow patients to engage in informed, shared treatment decision-making, prepare them for survivorship, and promote better adjustment to life after cancer.
We evaluated information preferences about risk of infertility separately from general late effects as we hypothesized that AYAs may have distinct perspectives about this topic. Consultation for fertility preservation options were available to all patients throughout the study period; however, there was not a standardized approach to providing information about risk of infertility at our institution. The American Society of Clinical Oncology (ASCO) recommends that fertility preservation options be discussed as early as possible with all patients of reproductive age whose treatment carries a risk of infertility, particularly as interventions to preserve fertility are considered standard practice and are widely available.21 We found that young adult patients age 22–29, those treated by medical oncologists, those who were financially independent or living independently, and those who felt they had more favorable prognoses were more likely to value early information about risk of infertility. This is a group for whom fertility issues are likely more salient as they may feel closer to this life stage. Yet only two-thirds of patients felt they received high-quality information about their risk of infertility, and 6% reported that they received no information about fertility.
We should note that we did not evaluate individual patient risk of infertility in our study. Given the spectrum of diagnoses, participants likely had variable risks of infertility, with some patients receiving treatments with little or no risk. It is possible that providers tailored information about infertility based on risk, such that those at greatest risk for infertility received more information, and those whose treatment carried no risk of infertility received limited information. Alternatively, conversations may have been held but not recalled by patients who may have been understandably stressed at diagnosis. Nonetheless, many patients felt they received suboptimal information despite their strong preference for this information. Other work has found similar rates of satisfaction with fertility counseling and suggests that inadequate information about this topic may preclude uptake of fertility preservation interventions,29 underscoring the importance of this information.
Over half of the respondents in our study were distressed by information about risks of late effects, and nearly half were distressed by information about potential infertility. This is in stark contrast to AYA feelings about prognostic information; only 10% of AYAs considered it extremely or very upsetting to know their chance of cure.8 Those who were distressed by information about risks of late effects or infertility were more likely to value information about these topics. This parallels prior findings of parental perspectives on late effects information, as parents of children with cancer similarly find late effects information distressing but extremely valuable.16 While providers may hesitate to offer information about late effects to those who are visibly distressed by this subject, AYAs seem to value information about potential late effects even if they find this information upsetting.
Our study took place at a single, large, academic cancer center with limited racial and ethnic diversity, potentially limiting the generalizability of our findings. Though many AYA patients are treated at similar centers, future research should explore the communication preferences of more vulnerable populations. We evaluated the perspectives of AYAs with a variety of malignancies who were treated by pediatric and medical oncologists. Late effect risks and communication practices may differ by treatment center, disease group, and medical and pediatric oncologists may have different approaches to providing information about fertility and late effects. Furthermore, we do not know the actual risks of infertility or late effects faced by our participants. A larger multi-center study is required to confirm these findings and explore the impact of different information provision practices across centers and disease groups. Our study was limited by its observational design, which was reliant on participant recall of topics discussed and quality of information provided; we do not know the actual content discussed with participants of our study. However, participant recall of information is an important measure of information comprehension and retention. While many patients reported that consideration of late effects risks greatly influenced their treatment decision-making, we do not know how these considerations affected their choices, or whether those who worried about late effects made different treatment decisions.
The transition from focusing on the present to a future orientation is an important component of AYA psychosocial development that may have substantial implications for health and wellbeing.30 Our finding that AYAs with cancer value information about late effects and infertility and consider these risks when making treatment decisions suggests that many AYAs are able to imagine and plan for a future after cancer treatment. Yet, many find this information distressing, and many feel they receive inadequate information about these topics. Given the high levels of distress associated with information about risks of late effects and infertility, which may inhibit AYA’s abilities to fully process and engage with provided information, thoughtful approaches to communication are needed. We must develop and test optimal ways of providing this information in a timely and sensitive manner to meet AYA information preferences, to facilitate treatment decision-making, and to support their vision of life post-cancer treatment.
Funding:
NIH Agency for Healthcare Research and Quality K12 HS022986 (KAG); Young Adult Program at the Dana-Farber Cancer Institute (KMF and JWM); Korostoff-Murray family (JWM)
Footnotes
Conflicts of Interest: None
References:
- 1.Keegan TH, Ries LA, Barr RD, et al. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer. 2016;122(7):1009–1016. [DOI] [PubMed] [Google Scholar]
- 2.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. The New England journal of medicine. 2006;355(15):1572–1582. [DOI] [PubMed] [Google Scholar]
- 3.Woodward E, Jessop M, Glaser A, Stark D. Late effects in survivors of teenage and young adult cancer: does age matter? Ann Oncol. 2011;22(12):2561–2568. [DOI] [PubMed] [Google Scholar]
- 4.Ramirez LY, Huestis SE, Yap TY, Zyzanski S, Drotar D, Kodish E. Potential chemotherapy side effects: what do oncologists tell parents? Pediatr Blood Cancer. 2009;52(4):497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hewitt MGS, Stoval E, editors. From Cancer Patient to Cancer Survivor: lost in transition. Washington, D.C.: National Academies Press; 2005. [Google Scholar]
- 6.In: Bonnie RJ, Stroud C, Breiner H, eds. Investing in the Health and Well-Being of Young Adults. Washington (DC)2015. [PubMed] [Google Scholar]
- 7.Brand SR, Fasciano K, Mack JW. Communication preferences of pediatric cancer patients: talking about prognosis and their future life. Supportive care in cancer. 2017;25(3):769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mack JW, Fasciano KM, Block SD. Communication About Prognosis With Adolescent and Young Adult Patients With Cancer: Information Needs, Prognostic Awareness, and Outcomes of Disclosure. J Clin Oncol. 2018:Jco2018782128. [DOI] [PubMed] [Google Scholar]
- 9.Weaver MS, Baker JN, Gattuso JS, Gibson DV, Sykes AD, Hinds PS. Adolescents’ preferences for treatment decisional involvement during their cancer. Cancer. 2015;121(24):4416–4424. [DOI] [PubMed] [Google Scholar]
- 10.Kelly KP, Mowbray C, Pyke-Grimm K, Hinds PS. Identifying a conceptual shift in child and adolescent-reported treatment decision making: “Having a say, as I need at this time”. Pediatr Blood Cancer. 2017;64(4). [DOI] [PubMed] [Google Scholar]
- 11.Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6(3):239–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Syed IA, Klassen AF, Barr R, et al. Factors associated with childhood cancer survivors’ knowledge about their diagnosis, treatment, and risk for late effects. J Cancer Surviv. 2016;10(2):363–374. [DOI] [PubMed] [Google Scholar]
- 13.DeRouen MC, Smith AW, Tao L, et al. Cancer-related information needs and cancer’s impact on control over life influence health-related quality of life among adolescents and young adults with cancer. Psychooncology. 2015;24(9):1104–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zebrack BJ, Eshelman DA, Hudson MM, et al. Health care for childhood cancer survivors: insights and perspectives from a Delphi panel of young adult survivors of childhood cancer. Cancer. 2004;100(4):843–850. [DOI] [PubMed] [Google Scholar]
- 15.Barnett M, McDonnell G, DeRosa A, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. 2016;10(5):814–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenzang KA, Cronin AM, Kang TI, Mack JW. Parental distress and desire for information regarding long-term implications of pediatric cancer treatment. Cancer. 2018;124(23):4529–4537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mack JW, Fasciano KM, Block SD. Adolescent and Young Adult Cancer Patients’ Experiences With Treatment Decision-making. Pediatrics. 2019;143(5). [DOI] [PubMed] [Google Scholar]
- 18.Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: parental optimism and the parent-physician interaction. J Clin Oncol. 2007;25(11):1357–1362. [DOI] [PubMed] [Google Scholar]
- 19.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol. 2006;24(33):5265–5270. [DOI] [PubMed] [Google Scholar]
- 20.Irene Su H, Lee YT, Barr R. Oncofertility: Meeting the Fertility Goals of Adolescents and Young Adults With Cancer. Cancer J. 2018;24(6):328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oktay K, Harvey BE, Partridge AH, et al. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018;36(19):1994–2001. [DOI] [PubMed] [Google Scholar]
- 22.Greenzang KA, Cronin AM, Mack JW. Parental preparedness for late effects and long-term quality of life in survivors of childhood cancer. Cancer. 2016;122(16):2587–2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mack J, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Peace of mind and sense of purpose as core existential issues among parents of children with cancer. Archives Ped Adol Med. 2009. June;163(6):519–524. [DOI] [PubMed] [Google Scholar]
- 24.Lee SJ, Fairclough D, Antin JH, Weeks JC. Discrepancies between patient and physician estimates for the success of stem cell transplantation. JAMA. 2001;285(8):1034–1038. [DOI] [PubMed] [Google Scholar]
- 25.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. [DOI] [PubMed] [Google Scholar]
- 26.Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. [DOI] [PubMed] [Google Scholar]
- 27.Smith AW, Keegan T, Hamilton A, et al. Understanding care and outcomes in adolescents and young adult with Cancer: A review of the AYA HOPE study. Pediatric blood & cancer. 2019;66(1):e27486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zebrack B, Kent EE, Keegan TH, Kato I, Smith AW. “Cancer sucks,” and other ponderings by adolescent and young adult cancer survivors. Journal of psychosocial oncology. 2014;32(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel V, Jones P, Judd A, Senko V, Altieri G, Pettee D. Recollection of Fertility Discussion in Adolescent and Young Adult Oncology Patients: A Single-Institution Study. J Adolesc Young Adult Oncol. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Johnson SR, Blum RW, Cheng TL. Future orientation: a construct with implications for adolescent health and wellbeing. Int J Adolesc Med Health. 2014;26(4):459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]


