Abstract
Cardiovascular disease (CVD) persists as the leading cause of death and disability in many Americans including Hispanics. Primary prevention for CVD may be achieved through regular aspirin use in high risk individuals. This study examined regular aspirin use and specific attitudes and social norms toward CVD and aspirin use within an urban Hispanic population in Minnesota. A sample of primary prevention Hispanics aged 45–79 years were surveyed about CVD history and risk factors, aspirin use, demographic characteristics, and health beliefs and social norms in relation to CVD and aspirin. Relative risk estimation using Poisson regression with robust error variance was used to examine associations with aspirin use. In this sample of 152 Hispanics (55% women), the mean age was 53 years, 70% had a regular healthcare provider, and 22% used aspirin. Aspirin discussions with a regular healthcare provider were strongly associated with aspirin use (adjusted risk ratio 3.02, 95% CI 1.20–7.60). There was a positive association between health beliefs and social norms that affirm preventive behaviors and aspirin use (adjusted linear risk ratio 1.23, 95% CI 1.04–1.45) while uncertainty about the role of aspirin for individual use and in the community was negatively associated with aspirin use (adjusted linear risk ratio 0.85, 95% CI 0.70–1.03). This growing population may benefit from health education about CVD risk and the role of aspirin in prevention.
Keywords: aspirin, prevention, cardiovascular disease, Hispanics, health behavior
Introduction
Cardiovascular disease (CVD) persists as a major public health issue within the United States and continues to be the leading cause of death and disability.1 In the Hispanic population, CVD is the most common cause of death, but mortality rates are lower compared to non-Hispanic Whites.1 In health literature, this has been described as the Hispanic paradox since Hispanics are more likely to experience traditional CVD risk factors such as diabetes, hypercholesteremia, physical inactivity and lower socioeconomic status,2–4 which makes the reasons for the lower mortality rates unclear.
One recommended strategy to prevent CVD is the use of low dose aspirin. Aspirin works to prevent heart attacks and strokes through inhibiting platelet aggregation and preventing thrombotic cardiovascular events. It is a low cost, easily accessible option for CVD prevention. The United States Preventive Services Task Force (USPSTF) 2016 recommendations state that adults between the ages of 50–69 who have not suffered a CVD event (primary prevention) should consider regular aspirin use in the setting of elevated risk for a CVD event (≥10% 10-year CVD risk) and low bleeding risk;5 however, recent studies have questioned aspirin use being appropriate for primary prevention due to concerns of overuse, bleeding risks, and the harms potentially outweighing the possible benefits.6–9 Secondary prevention aspirin use in those who have experienced a prior CVD event is a well-established therapy. Although aspirin recommendations have been in place for many years, regular primary prevention aspirin use in those with moderate to high risk is suboptimal, with little impact from guideline publications.10 In addition, the use of aspirin as a cardiovascular preventive medication differs greatly among different racial and ethnic populations, 11–18 yet little is known about why this variation exists.
Previous studies looking at preventive aspirin use in Hispanic populations are limited and vary in their scientific approaches.11–19 Overall, Hispanics have lower rates of aspirin use when compared to non-Hispanic Whites,11–18 which may illustrate a population in need of increased education about appropriate aspirin use. Potential barriers to dissemination of public health information include limited materials in the appropriate primary language, lower health literacy and a deficiency in cultural competency on the part of the educators.
This study examined CVD risk and aspirin use patterns among an urban Hispanic population and investigated associations between demographic characteristics, physician-related aspirin discussions, and health behavior beliefs and social norms with regular aspirin use for primary prevention.
Methods
Study Population
A survey was administered from April to July 2017 in the Minneapolis- Saint Paul metropolitan areas. Men and women ages 45–79 years who identified as a race other than White were recruited with the help of community health workers with prior experience working in communities of color. Recruitment sites included churches, gyms, public events (community and health fairs), senior housing and community centers. All eligible individuals gave verbal informed consent, and were offered a $10 gift card to participate.
Survey data were collected from a total of 797 individuals. For this analysis, only participants who identified themselves as Hispanic were included (n=198). Participants residing outside of Minnesota (n=6), missing aspirin use information (n=5), or having a previous CVD history (n=35) were excluded. This resulted in a final sample of 152 Hispanic primary prevention participants. The University of Minnesota Institutional Review Board (IRB) evaluated and approved this study.
Data Collection/Definitions
Qualified community health workers administered a 10-minute, in-person survey to individuals meeting the study criteria. The survey was conducted in English or Spanish depending on participant preference. Overall, 114 out of 797 surveys (14.3%) were administered in Spanish, of which 77 out of 152 (50.7%) are included in this analysis. The survey queried information on demographics, CVD history, CVD risk factors—diabetes mellitus, hyperlipidemia, hypertension, and smoking status (current, former, never)—aspirin use, health care provider information, and health behavior beliefs and social norms. A history of CVD was defined as the self-reported history of a heart attack, stroke, or peripheral artery disease, or an endovascular or surgical procedure to revascularize coronary, carotid, or limb arteries. All referrals to aspirin use in this manuscript assumes self-reported regular aspirin use, defined as daily or every other day use in order to prevent a heart attack or stroke. Aspirin contraindications included a self-reported history of a gastrointestinal bleed/peptic ulcer, an aspirin allergy, or other antithrombotic use such as warfarin or clopidogrel.
Health behavior beliefs and social norms were examined through nine questions formulated on the theory of planned behavior.20 Questions based on this theory have been used to evaluate health behaviors related to CVD and aspirin use in prior studies.21–24 The nine health behavior belief questions examined CVD risk perceptions and aspirin beliefs/perceptions using a 4-point Likert scale: “Strongly Agree”, “Agree”, “Disagree”, and “Strongly Disagree”. Participants could respond with “Don’t Know” as well. For this analysis, “Strongly Agree” and “Agree” were grouped together as one category (“Agree”), and “Strongly Disagree” and “Disagree” were combined to form another category (“Disagree”).
Statistical Analysis
Categorical variables are presented as frequency (percent); age is presented as mean ± standard deviation (SD).
Since aspirin use was a common outcome in this sample (>10%), relative risk estimation using Poisson regression with robust error variance estimation25 was used to examine age-adjusted, univariate associations between demographic characteristics and cardiovascular risk factors and aspirin use. Those variables associated with aspirin use were then included in a multivariable model.
For the health behavior belief questions, the proportion of “Agree”, “Disagree” and “Don’t Know” responses to each of the nine questions are presented; aspirin use was recorded for each category. Poisson regression was used to examine the age-adjusted and multivariable associations of total number of “Agree” and “Don’t Know” responses with aspirin use. The total number of “Agree” and “Don’t Know” responses were modeled as tertiles and as a linear variable. A sensitivity analysis was performed that excluded those who had any aspirin contraindications. All analyses were performed using Stata version 15 (Stata Corp, College Station, Texas, USA).
Results
The characteristics of the Hispanic participants are shown in Table 1. Mean age was 53 years; over half were 45–49 years old. The sample consisted of 55% women. Almost half of the Hispanic participants were married and did not graduate from high school. Many of the individuals (40%) had no self-reported CVD risk factors, and 70% reported having a regular healthcare provider.
Table 1:
Characteristics of primary prevention Hispanic participants (n=152)
| Demographics | |
| Age, years | 53.0 ± 8.6 |
| 45–49 | 84 (55.3) |
| 50–59 | 34 (22.4) |
| 60–69 | 24 (15.8) |
| 70–79 | 10 (6.6) |
| Sex | |
| Women | 83 (54.6) |
| Men | 42 (27.6) |
| Unknown | 27 (17.8) |
| Education | |
| <High school graduate | 73 (48.0) |
| High school graduate | 25 (16.5) |
| Some college | 32 (21.1) |
| College graduate/graduate school | 18 (11.8) |
| Other | 4 (2.6) |
| Marital status | |
| Married | 72 (47.4) |
| Single | 26 (17.1) |
| Divorced | 22 (14.5) |
| Separated | 15 (9.9) |
| Widowed | 9 (5.9) |
| Other | 8 (5.3) |
| Risk factors | |
| Diabetes | 57 (37.5) |
| Hyperlipidemia | 43 (28.3) |
| Hypertension | 56 (36.8) |
| Smoking status | |
| Never | 110 (72.4) |
| Former | 21 (13.8) |
| Current | 21 (13.8) |
| Number of risk factors | |
| None | 60 (39.5) |
| 1 | 37 (24.3) |
| 2 | 29 (19.1) |
| 3–4 | 26 (17.1) |
| Aspirin contraindications | |
| Gastrointestinal bleed/peptic ulcer | 11 (7.2) |
| Aspirin allergy | 4 (2.6) |
| Anticoagulant use | 14 (9.2) |
| Any contraindications | 25 (16.5) |
| Health provider inquiries | |
| Regular health care provider | 106 (69.7) |
| Any aspirin discussion with provider | 64 (42.1) |
| Survey administered in Spanish | 77 (57.7) |
Data are presented as n (%) for categorical variables and as mean ± standard deviation for age as a continuous variable.
Aspirin Use Prevalence and Associations
In this sample, 33 out of 152 participants (22%) were regular aspirin users. There were several factors associated with aspirin use in the age-adjusted models (Table 2). Increasing age and more cardiovascular risk factors (diabetes, hyperlipidemia, and hypertension) were positively associated with aspirin use. The strongest associations with aspirin were seen in participants with ≥3 CVD risk factors compared to no risk factors (risk ratio - RR 5.23, 95% CI 2.07–13.22) and those who had an aspirin discussion with a health care provider (RR 4.19, 95% CI 1.83–9.56). The final multivariable model included age, diabetes, hyperlipidemia, hypertension, smoking status, and any aspirin discussion with a health care provider (Table 2). After adjustment, all of the positive associations of each variable in the model were attenuated, although any aspirin discussion with a health care provider still had a strong association (adjusted RR 3.02, 95% CI 1.20–7.60).
Table 2:
Age-adjusted and multivariable-adjusted associations of regular aspirin use with demographics and cardiovascular risk factors in Hispanic primary prevention participants
| N | Regular aspirin use n (%) | Age-adjusted RR (95% CI) | Multivariable RR (95% CI) | |
|---|---|---|---|---|
| Overall | 152 | 33 (22%) | ||
| Age, years | 1.06 (1.03–1.08) | 1.02 (0.99–1.05) | ||
| 45–49 | 84 | 10 (12%) | 1 (Reference) | |
| 50–59 | 34 | 10 (29%) | 2.47 (1.13–5.41) | |
| 60–69 | 24 | 8 (33%) | 2.80 (1.24–6.32) | |
| 70–79 | 10 | 5 (50%) | 4.20 (1.79–9.85) | |
| Sex | ||||
| Women | 83 | 12 (14%) | 1 (Reference) | |
| Men | 42 | 14 (33%) | 1.82 (0.92–3.59) | |
| Unknown | 27 | 7 (26%) | 1.67 (0.75–3.70) | |
| Education | ||||
| <High school graduate | 73 | 14 (19%) | 0.91 (0.36–2.34) | |
| High school graduate | 25 | 4 (16%) | 0.94 (0.28–3.18) | |
| Some college | 32 | 11 (34%) | 1.60 (0.61–4.19) | |
| College degree/graduate school | 18 | 4 (22%) | 1 (Reference) | |
| Other | 4 | 0 (0%) | - | |
| Marital status | ||||
| Married | 72 | 17 (24%) | 1 (Reference) | |
| Single | 26 | 5 (19%) | 0.75 (0.33–1.71) | |
| Divorced | 22 | 4 (18%) | 0.71 (0.27–1.84) | |
| Separated | 15 | 1 (7%) | 0.20 (0.03–1.42) | |
| Widowed | 9 | 6 (67%) | 1.80 (1.01–3.21) | |
| Other | 8 | 0 (0%) | - | |
| Diabetes | ||||
| Yes | 57 | 22 (39%) | 2.71 (1.43–5.13) | 1.43 (0.72–2.85) |
| No | 95 | 11 (12%) | 1 (Reference) | 1 (Reference) |
| Hyperlipidemia | ||||
| Yes | 43 | 18 (42%) | 2.32 (1.23–4.36) | 1.66 (0.93–2.96) |
| No | 109 | 15 (14%) | 1 (Reference) | 1 (Reference) |
| Hypertension | ||||
| Yes | 56 | 22 (39%) | 2.62 (1.33–5.18) | 1.27 (0.63–2.57) |
| No | 96 | 11 (11%) | 1 (Reference) | 1 (Reference) |
| Smoking status | ||||
| Never | 110 | 19 (17%) | 1 (Reference) | 1 (Reference) |
| Former | 21 | 9 (43%) | 1.91 (1.05–3.49) | 1.44 (0.90–2.32) |
| Current | 21 | 5 (24%) | 1.11 (0.46–2.66) | 1.13 (0.49–2.62) |
| Number of risk factors | ||||
| None | 60 | 5 (8%) | 1 (Reference) | |
| 1 | 37 | 6 (16%) | 1.85 (0.60–5.64) | |
| 2 | 29 | 7 (24%) | 2.34 (0.83–6.60) | |
| 3–4 | 26 | 15 (58%) | 5.23 (2.07–13.22) | |
| Regular health care provider | ||||
| Yes | 106 | 28 (26%) | 1.94 (0.79–4.81) | |
| No | 46 | 5 (11%) | 1 (Reference) | |
| Any aspirin discussion with provider | ||||
| Yes | 64 | 26 (41%) | 4.19 (1.83–9.56) | 3.02 (1.20–7.60) |
| No | 88 | 7 (8%) | 1 (Reference) | 1 (Reference) |
RR: risk ratio; CI: confidence interval
Two sensitivity analyses were performed. The first analysis excluded those who had any aspirin contraindications (n=25) and the second adjusted for the number of CVD risk factors instead of each CVD risk factor separately. The results in both analyses were similar to the primary analysis (data not shown).
Attitudes and Social Norms toward CVD and Aspirin
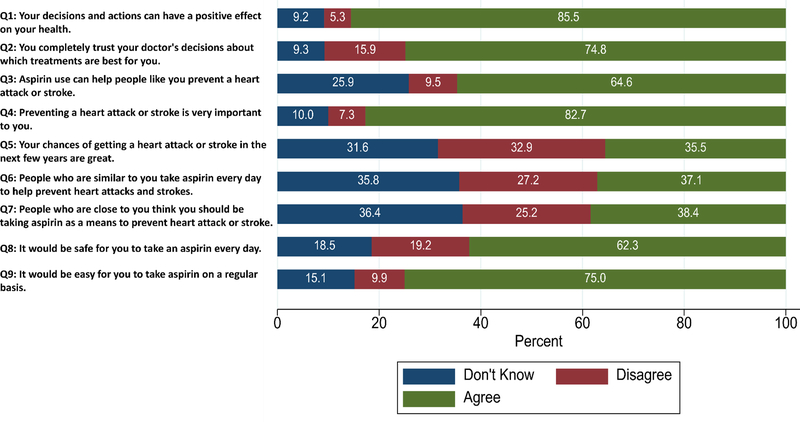
The responses to the attitudes and social norms toward CVD and aspirin questions are shown in Figure 1. An “Agree” response was the most common, but many participants chose “Don’t Know”, especially for the questions pertaining to aspirin use (Q3, Q6-Q9). Over one quarter of participants answered “Don’t Know” in response to questions about aspirin effectiveness (Q3) and social norms around aspirin use (Q6–7). Aspirin use was highest in the participants who answered “Agree” compared to other responses (Table S1).
Figure 1:
Health behavior question responses in Hispanic primary prevention participants
In Table 3, the number of “Agree” responses (possible range 0–9) was positively associated with aspirin use in the multivariable model (linear RR 1.23, 95% CI 1.04–1.45). The number of “Don’t Know” responses was negatively associated with aspirin use after age adjustment (linear RR 0.77, 95% CI 0.63–0.93). This association was attenuated in the multivariable model (linear RR 0.85, 95% CI 0.70–1.03). Similar results were found in sensitivity analyses excluding those who had any aspirin contraindications and adjusting for the number of CVD risk factors instead of each CVD risk factor separately (data not shown).
Table 3:
Age and multivariable-adjusted associations of regular aspirin use with number of “Agree” and “Don’t Know” responses to health behavior questions in Hispanic primary prevention participants
| Number of “Agree” Responses |
Number of “Don’t Know” Responses |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Regular aspirin use | Age-adjusted | Multivariable | N | Regular aspirin use | Age-adjusted | Multivariable | ||
| n (%) | RR (95% CI) | RR (95% CI) | n (%) | RR (95% CI) | RR (95% CI) | ||||
| Tertile 1 (<5) | 51 | 4 (8%) | 1 (reference) | 1 (reference) | Tertile 1 (0) | 66 | 21 (32%) | 1 (reference) | 1 (reference) |
| Tertile 2 (5–6) | 48 | 6 (13%) | 1.43 (0.42–4.83) | 1.00 (0.32–3.13) | Tertile 2 (1–3) | 52 | 9 (17%) | 0.56 (0.29–1.08) | 0.83 (0.41–1.67) |
| Tertile 3 (7–9) | 53 | 23 (43%) | 4.46 (1.65–12.10) | 2.91 (1.05–8.10) | Tertile 3 (4–9) | 34 | 3 (9%) | 0.30 (0.09–0.97) | 0.51 (0.15–1.67) |
| Linear | 152 | 33 (22%) | 1.36 (1.18–1.57) | 1.23 (1.04–1.45) | Linear | 152 | 33 (22%) | 0.77 (0.63–0.93) | 0.85 (0.70–1.03) |
Multivariable regression adjusted for age (as a continuous variable), diabetes, hyperlipidemia, hypertension, smoking status, and any aspirin discussion with a health care provider.
RR: risk ratio; CI: confidence interval
Discussion
In this survey of urban Hispanics from Minnesota, regular aspirin use and attitudes and social norms towards CVD prevention and aspirin were examined within primary prevention participants. Overall, preventative aspirin use was low in this relatively young sample with few CVD risk factors. An aspirin discussion with a health provider was associated with aspirin use after adjustment for age and other CVD risk factors. In addition, those who answered “Agree” to personal and social perspectives on prevention and aspirin use were associated with aspirin use. Many participants were uncertain about the role of aspirin for themselves and their community, and this uncertainty was negatively associated with aspirin use.
Hispanic Aspirin Use
The results seen in this study are similar to previous studies in the literature and illustrate suboptimal use of aspirin in Hispanic populations.11–19 Any minor differences in aspirin use between these studies may be due to different survey methodologies, different study objectives, different CVD definition criteria to determine a primary prevention sample, and different age ranges of participants, with some having younger individuals before the age of 45 included in their study sample.11,12,15–19 Younger individuals (less than 50 years) are currently not recommended for aspirin use by the USPSTF due to their low risk, although the recent AHA/ACC 2019 guideline recommendations include individuals as young as 40 years.26 In this study, close to half of the analytic sample were below 50 years old, and almost 40% of individuals did not have any CVD risk factors. While there are concerns of aspirin overuse in low risk individuals and suboptimal aspirin use in high risk individuals, this study suggests that overuse is uncommon in young people and those with few CVD risk factors.
Health Provider Discussion about Aspirin
In this study, we found that a discussion about aspirin with a healthcare provider was associated with aspirin use in multivariable modeling. Two other studies also identified the importance of a healthcare provider discussion in recommending aspirin use.15,16 A healthcare provider has the potential to be a strong influence for recommending appropriate preventive aspirin use. In one study, physician recommended aspirin use was much higher than self-initiated aspirin use (20% and 3%, respectively).16 In this sample, 70% of participants had a regular healthcare provider, which is lower than what was seen in African Americans (>90%) from a similar geographic area.24 Enabling and improving access to a regular healthcare provider for Hispanics may allow the possibility of more aspirin discussions to take place within healthcare settings.
Attitudes and Social Norms toward CVD and Aspirin
Attitudes and social norms toward CVD and aspirin use have not been studied extensively, especially in Hispanics. The results of this study illustrate the need for education to increase CVD awareness and aspirin’s role in CVD prevention. Previous studies have shown that racial disparities exist for CVD awareness, with Hispanics more likely to have lower awareness about CVD (heart disease and/or stroke)27,28,37–40,29–36 compared to non-Hispanic Whites. A number of issues may affect attitudes and social norms toward aspirin use. Language barriers may exist such as limited English fluency and proficiency or a low health literacy may contribute to ethnic disparities for aspirin and CVD awareness.31,33,34,38,41–43 The use of bilingual services and translation of education materials may help in limiting such a barrier. In addition, Hispanic culture needs to be considered and incorporated into any process as traditional outreach methods and programs may not be as effective if they are not tailored specifically to the population to be studied.36 Finally, a key barrier to both aspirin and CVD awareness is related to confusion in the media,37 where the media spin of treatment studies may affect an individual’s interpretation of the study results.44
Strengths/Limitations
This study has several strengths and limitations. The inclusion of health behavior beliefs and social norm questions provided a greater insight into a participant’s health education and awareness. This small Hispanic sample from Minnesota may not be widely generalizable to other Hispanic populations throughout the rest of the United States. However, the aspirin use results seen in this study appear to be consistent with previous studies. A bias may exist by surveying participants at community-based sites, as those who are less engaged in the community would not be represented in this sample. Since many of the screening locations were health-based, there is a likelihood that those who were surveyed may be healthier or more interested in their health than those who did not attend these events. Self-reported information about medical history and medication use could not be adjudicated, but there is plausible evidence that supports the accuracy of self-reported aspirin use.45 We were unable to calculate a CVD risk score in order to determine if an individual was at a high, moderate or low risk for a CVD event. Treating Hispanics as one homogenous group may underestimate any disparities in aspirin use within specific Hispanic/Latino subgroups, but a previous study found aspirin use to be similar across subgroups in individuals at high risk for a CVD event.19
Conclusion
This study investigated aspirin use and the health beliefs and perceptions of CVD risk and aspirin in an urban Hispanic population. Overall, an aspirin discussion with a health provider was associated with increased aspirin use, and health behavior responses to CVD and aspirin-related questions also played a role in aspirin use. This growing population may benefit from health education about CVD risk and the role of aspirin in prevention.
Supplementary Material
Acknowledgments
Funding: This study was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, Grant No. R01HL126041.
Footnotes
Compliance with Ethical Standards
Conflict of interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10). doi: 10.1161/cir.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez CJ, Allison M, Daviglus ML, et al. Status of cardiovascular disease and stroke in hispanics/latinos in the united states: A science advisory from the american heart association. Circulation. 2014;130(7):593–625. doi: 10.1161/CIR.0000000000000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balfour PC, Ruiz JM, Talavera GA, Allison MA, Rodriguez CJ. Cardiovascular disease in Hispanics/Latinos in the United States. J Lat Psychol. 2016;4(2):98–113. doi: 10.1037/lat0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw PM, Chandra V, Escobar GA, Robbins N, Rowe V, Macsata R. Controversies and evidence for cardiovascular disease in the diverse Hispanic population. J Vasc Surg. 2018;67(3):960–969. doi: 10.1016/j.jvs.2017.06.111 [DOI] [PubMed] [Google Scholar]
- 5.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 2016;164(12):836–845. doi: 10.7326/M16-0577 [DOI] [PubMed] [Google Scholar]
- 6.Gaziano JM, Brotons C, Coppolecchia R, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392(10152):1036–1046. doi: 10.1016/S0140-6736(18)31924-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowman L, Mafham M, Wallendszus K, et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–1539. doi: 10.1056/NEJMoa1804988 [DOI] [PubMed] [Google Scholar]
- 8.McNeil JJ, Nelson MR, Woods RL, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519–1528. doi: 10.1056/NEJMoa1803955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNeil JJ, Wolfe R, Woods RL, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509–1518. doi: 10.1056/NEJMoa1805819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van’t Hof JR, Duval S, Walts A, Kopecky SL, Luepker RV., Hirsch AT. Contemporary primary prevention aspirin use by cardiovascular disease risk: Impact of US preventive services task force recommendations, 2007–2015: A serial, cross-sectional study. J Am Heart Assoc. 2017;6(10). doi: 10.1161/JAHA.117.006328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown DW, Shepard D, Giles WH, Greenlund KJ, Croft JB. Racial differences in the use of aspirin: An important tool for preventing heart disease and stroke. Ethn Dis. 2005;15(4):620–626. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L41645129. [PubMed] [Google Scholar]
- 12.Ajani UA, Ford ES, Greenland KJ, Giles WH, Mokdad AH. Aspirin use among U.S. adults: Behavioral risk factor surveillance system. Am J Prev Med. 2006;30(1):74–77. doi: 10.1016/j.amepre.2005.08.042 [DOI] [PubMed] [Google Scholar]
- 13.Qato DM, Lindau ST, Conti RM, Schumm LP, Alexander GC. Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiol Drug Saf. 2010;19(8):834–842. doi: 10.1002/pds.1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanchez DR, Diez Roux AV, Michos ED, et al. Comparison of the racial/ethnic prevalence of regular aspirin use for the primary prevention of coronary heart disease from the multi-ethnic study of atherosclerosis. Am J Cardiol. 2011;107(1):41–46. doi: 10.1016/j.amjcard.2010.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mainous AG, Tanner RJ, Shorr RI, Limacher MC. Use of aspirin for primary and secondary cardiovascular disease prevention in the United States, 2011–2012. J Am Heart Assoc. 2014;3(4). doi: 10.1161/JAHA.114.000989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gu Q, Dillon CF, Eberhardt MS, Wright JD, Burt VL. Preventive aspirin and other antiplatelet medication use among U.S. adults aged≥ 40 years: Data from the national health and nutrition examination survey, 2011–2012. Public Health Rep. 2015;130(6):643–654. doi: 10.1177/003335491513000614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis JS, Lee HY, Kim J, et al. Use of non-steroidal anti-inflammatory drugs in US adults: Changes over time and by demographic. Open Hear. 2017;4(1):e000550. doi: 10.1136/openhrt-2016-000550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Brien CW, Juraschek SP, Wee CC. Prevalence of Aspirin Use for Primary Prevention of Cardiovascular Disease in the United States: Results From the 2017 National Health Interview Survey. Ann Intern Med. July 2019. doi: 10.7326/M19-0953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qato DM, Lee TA, Durazo-Arvizu R, et al. Statin and aspirin use among hispanic and latino adults at high cardiovascular risk: Findings from the hispanic community health study/study of latinos. J Am Heart Assoc. 2016;5(4):1–11. doi: 10.1161/JAHA.115.002905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ajzen I The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 21.Norman P, Conner M, Bell R. The theory of planned behavior and smoking cessation. Heal Psychol. 1999;18(1):89–94. doi: 10.1037/0278-6133.18.1.89 [DOI] [PubMed] [Google Scholar]
- 22.Plotnikoff RC, Lubans DR, Costigan SA, McCargar L. A Test of the Theory of Planned Behavior to Predict Physical Activity in an Overweight/Obese Population Sample of Adolescents From Alberta, Canada. Heal Educ Behav. 2013;40(4):415–425. doi: 10.1177/1090198112455642 [DOI] [PubMed] [Google Scholar]
- 23.Oldenburg NC, Duval S, Luepker RV., et al. A 16-Month Community-Based Intervention to Increase Aspirin Use for Primary Prevention of Cardiovascular Disease. Prev Chronic Dis. 2014;11:130378. doi: 10.5888/pcd11.130378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van’t Hof JR, Duval S, Misialek JR, et al. Aspirin Use for Cardiovascular Disease Prevention in an African American Population: Prevalence and Associations with Health Behavior Beliefs. J Community Health. 2019;44(3):561–568. doi: 10.1007/s10900-019-00646-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 26.Arnett DK, Blumenthal RS, Albert MA, et al. 2019. ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Circulation. March 2019:CIR0000000000000678. doi: 10.1161/CIR.0000000000000678 [DOI] [Google Scholar]
- 27.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women’s Heart Disease and Stroke Campaign Task Force. Arch Fam Med. 2000;9(6):506–515. http://www.ncbi.nlm.nih.gov/pubmed/10862212 Accessed July 25, 2019. [DOI] [PubMed] [Google Scholar]
- 28.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking Women’s Awareness of Heart Disease: An American Heart Association National Study. Circulation. 2004;109(5):573–579. doi: 10.1161/01.CIR.0000115222.69428.C9 [DOI] [PubMed] [Google Scholar]
- 29.Mochari-Greenberger H, Miller KL, Mosca L. Racial/Ethnic and Age Differences in Women’s Awareness of Heart Disease. J Women’s Heal. 2012;21(5):476–480. doi: 10.1089/jwh.2011.3428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lutfiyya MN, Bardales R, Bales R, et al. Awareness of heart attack and stroke symptoms among Hispanic male adults living in the United States. J Immigr Minor Heal. 2010;12(5):761–768. doi: 10.1007/s10903-009-9250-y [DOI] [PubMed] [Google Scholar]
- 31.Giardina EGV, Mull L, Sciacca RR, et al. Relationship between cardiovascular disease knowledge and race/ethnicity, education, and weight status. Clin Cardiol. 2012;35(1):43–48. doi: 10.1002/clc.20992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferris A, Robertson RM, Fabunmi R, Mosca L. American Heart Association and American Stroke Association national survey of stroke risk awareness among women In: Circulation. Vol 111 Lippincott Williams & Wilkins; 2005:1321–1326. doi: 10.1161/01.CIR.0000157745.46344.A1 [DOI] [PubMed] [Google Scholar]
- 33.Ojike N, Azizi S. Racial Disparity in Stroke Awareness in the US: An Analysis of the 2014 National Health Interview Survey. J Neurol Neurophysiol. 2016;07(02). doi: 10.4172/2155-9562.1000365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giardina E-GV, Sciacca RR, Flink LE, Bier ML, Paul TK, Moise N. Cardiovascular Disease Knowledge and Weight Perception Among Hispanic and Non-Hispanic White Women. J Women’s Heal. 2013;22(12):1009–1015. doi: 10.1089/jwh.2013.4440 [DOI] [PubMed] [Google Scholar]
- 35.Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3(2):120–127. doi: 10.1161/CIRCOUTCOMES.109.915538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mosca L, Hammond G, Mochari-Greenberger H, et al. Fifteen-year trends in awareness of heart disease in women: Results of a 2012 American Heart Association national survey. Circulation. 2013;127(11):1254–1263. doi: 10.1161/CIR.0b013e318287cf2f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mosca L, Mochari H, Christian A, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113(4):525–534. doi: 10.1161/CIRCULATIONAHA.105.588103 [DOI] [PubMed] [Google Scholar]
- 38.Christian AH, Rosamond W, White AR, Mosca L. Nine-Year Trends And Racial And Ethnic Disparities in Women’s Awareness of Heart Disease And Stroke: An American Heart Association National Study. J Women’s Heal. 2007;16(1):68–81. doi: 10.1089/jwh.2006.m072 [DOI] [PubMed] [Google Scholar]
- 39.Villablanca AC, Slee C, Lianov L, Tancredi D. Outcomes of a Clinic-Based Educational Intervention for Cardiovascular Disease Prevention by Race, Ethnicity, and Urban/Rural Status. J Women’s Heal. 2016;25(11):1174–1186. doi: 10.1089/jwh.2015.5387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martinez M, Prabhakar N, Drake K, et al. Identification of barriers to stroke awareness and risk factor management unique to hispanics. Int J Environ Res Public Health. 2015;13(1):23. doi: 10.3390/ijerph13010023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40(1):52–59. http://www.ncbi.nlm.nih.gov/pubmed/11748426 Accessed June 25, 2019. [DOI] [PubMed] [Google Scholar]
- 42.Sentell T, Braun KL. Low Health Literacy, Limited English Proficiency, and Health Status in Asians, Latinos, and Other Racial/Ethnic Groups in California. J Health Commun. 2012;17(sup3):82–99. doi: 10.1080/10810730.2012.712621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. hispanics. Am J Prev Med. 2006;30(3):189–196. doi: 10.1016/j.amepre.2005.10.024 [DOI] [PubMed] [Google Scholar]
- 44.Boutron I, Haneef R, Yavchitz A, et al. Three randomized controlled trials evaluating the impact of “spin” in health news stories reporting studies of pharmacologic treatments on patients’/caregivers’ interpretation of treatment benefit. BMC Med. 2019;17(1). doi: 10.1186/s12916-019-1330-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zantek ND, Luepker RV, Duval S, Miller K, Oldenburg N, Hirsch AT. Confirmation of reported aspirin use in community studies: Utility of serum thromboxane B2 measurement. Clin Appl Thromb. 2014;20(4):385–392. doi: 10.1177/1076029613486537 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.