Abstract
Background:
End-of-life spending and health care utilization in older adults with COPD have not been previously described.
Methods:
We examined data from Medicare beneficiaries ≥65 years with COPD who died between 2013–2014. End-of-life measures were retrospectively reviewed for two years prior to death. Hospital referral regions (HRRs) were categorized into quintiles of age-sex-race-adjusted overall spending during the last two years of life. We examined geographic and spending quintile variation in spending and health care utilization across the continuum.
Results:
We investigated data from 146,240 decedents with COPD from 306 HRRs. Age-sex- race-adjusted overall spending per-decedent during the last two years of life varied significantly nationwide ($61,271±$11,639 per decedent; range: $48,288±$3,665 to $79,453±$9,242). Inpatient care accounted for 40.2% of spending ($24,626±$6,192 per decedent). Overall, 82%±4% of decedents were admitted to the hospital for 13.7±3.1 days and 55%±11% to an intensive care unit for 5.4±2.5 days. Compared to HRRs in the lowest spending quintile, HRRs in the highest spending quintile had 1.5-fold longer hospital length of stay. Skilled nursing facilities accounted for 11.6% of spending ($7101±$2403 per decedent) and were used by 38%±7% of decedents for 18.7±4.9 days. Hospice accounted for 10.3% of spending ($6,307±$2,201 per decedent) and was used by 47%±9% of decedents for 39.7±14.8 days. Significant geographic variation in hospice use existed nationwide.
Conclusions:
End-of-life spending and healthcare utilization in older adults with COPD varied substantially nationwide. Decedents with COPD frequently used acute and post-acute care near the end of life. Hospice use was higher than expected, with significant geographic disparities.
Keywords: COPD, hospice, palliative care, healthcare utilization, cost
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in the United States (US), and adults aged 75 years and older will account for half of the COPD population in the coming decade.1,2 Total direct costs attributable to COPD in the US will reach an estimated $50 billion dollars by 2020, half of which are paid for by Medicare.3 A significant portion of spending for the care of older adults is devoted to acute care at the end of life, and in cancer, this spending exhibits significant geographic variation.4,5 Compared to cancer, COPD patients often have greater symptom burden.6 Older COPD patients are at greater risk for hospitalizations due to severe exacerbations of COPD compared to their younger counterparts, and hospitalizations are associated with higher mortality and reduced quality of life in COPD.7 Access to hospice has demonstrated improvement in patient-centered outcomes in the terminal phase of illness in advanced cancer and heart failure.8–10 However, hospice and palliative care are rare in COPD.11,12 To guide policies that improve patient-centered care at the end of life for a rapidly growing population of older adults with COPD, studies examining end-of-life spending, health care utilization, and hospice use are needed.
We examined the spectrum of end-of-life spending and utilization in COPD by conducting a descriptive study of a nationwide decedent cohort of Medicare beneficiaries with COPD and exploring end-of-life measures going back to two years before death. We analyzed data from the Dartmouth Atlas Project, which includes regional and nationwide data from the Centers for Medicare and Medicaid Services (CMS).13,14 We examined the following in older decedents with COPD: 1) overall and category-specific end-of-life spending; 2) health care utilization across a continuum of services; and, 3) hospice use. We hypothesized that despite having high end-of-life spending and high health care utilization, hospice use in COPD would be proportionately low at the end of life and would vary nationwide.
METHODS
Study Population
The methods of the Dartmouth Atlas Project have been described in detail.13,15 The Dartmouth Atlas Project does not include data from beneficiaries who are members of Health Maintenance Organizations. The primary database was derived using 100% of the beneficiaries from CMS, including the following research files: 1) denominator; 2) MedPar; 3) inpatient; 4) physician/supplier Part-B; 5) outpatient; 6) home health agency (HHA); 7) hospice; and, 8) durable medical equipment (DME). We reviewed a cohort of patients who died between fiscal years 2013–2014 with primary and secondary discharge diagnoses for COPD by the following International Classification of Diseases, Ninth Revision (ICD-9) codes: 491xx, 492xx, 494xx, 496xx, 466.0x, and 466.0x only combined with secondary diagnoses 491xx, 492xx, 494xx, and 496xx. We reviewed end-of-life measures going back to two years prior to death. Decedents were restricted to those with full Part-A and Part-B entitlement whose age on the date of death was between 67–99 years. Data were assigned to the hospital referral region (HRR) most often used during the last two years of life. The databases used to generate performance measures included a complete sample of hospital admissions and hospice enrollments and 20% of claims from physicians and laboratories.
Outcomes
Spending
We used age-sex-race (ASR)-adjusted claims to estimate spending in the last two years of life, which is consistent with the Dartmouth Atlas Project. We reviewed overall spending per-decedent and categorical spending for inpatient, Part-B, outpatient facility, outpatient physician, medical equipment, home health, skilled nursing facility (SNF), long-term care, and hospice. We sub-classified Part-B spending into emergency room, imaging, procedures, tests, ambulance use, and other.
Healthcare Utilization
We categorized health care utilization into frequency of encounters, number of visits, and length of stay (LOS) per decedent. We measured encounter frequency as the percent of the cohort who experienced any of the following events in the last two years of life: hospital admission, ICU admission, SNF admission, receipt of medical equipment, home health aide, long-term care, hospice, and Part-B encounters. Visit data included the following: inpatient physician, emergency room, ambulatory physician (primary care and specialist), Rural and Federally Qualified Health Clinic, and home health. LOS was calculated as the number of days spent in the hospital, in the intensive care unit (ICU), in a SNF, or in hospice.
Statistical Analysis
We conducted the data analysis between January 1, 2018 to May 1, 2019. We reported overall and categorical expenditures as mean ± standard deviation (SD) dollars spent per decedent going back to the last two years of life. Encounters per decedent were reported as mean frequency (%) ± SD, and number of visits and LOS were reported as mean ± SD. For health care utilization, we used the full two years of observation before death as the denominator. We calculated crude hospital-specific rates by using the number of cohort members assigned to the hospital as the denominator. We categorized spending over the last two years of life into quintiles, with the first quintile representing the lowest mean ASR-adjusted spending per decedent. To reduce variability caused by low HRR volumes, we excluded HRRs with fewer than twenty COPD decedents. We investigated variation in spending, encounters, visits, and LOS across spending quintiles and generated turnip plots to examine dispersion within and across spending quintiles. We used Mapinfo (version 8.0) to generate nationwide maps of HRRs stratified by spending quintiles. We used SAS software (version 9.4) and Stata (version 15.1) to complete all statistical analyses. Data analysis and results were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement.16
SOURCES OF FUNDING
The data was created and obtained from The Dartmouth Atlas of Health Care, which is funded by the Robert Wood Johnson Foundation and The Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The sponsoring agencies were not involved in the study.
RESULTS
Cohort
Our cohort included 146,240 older decedents with COPD from 306 HRRs who died between 2013–2014. Two-year retrospective data covered a time period from 2011–2014. Table 1 includes data on the overall population. HRRs in higher spending quintiles were generally more populated and urban on average (Table 1).
Table 1.
Characteristics of the Overall* Population by End-of-Life Spending Quintiles
| Variables | Overall | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
|---|---|---|---|---|---|---|
| Number of HRRs | N=306 | n=62 | n=61 | n=61 | n=61 | n=61 |
| Mean (±SD) population in the HHR | 478 (416) | 278 (186) | 407 (311) | 535 (463) | 508 (395) | 665 (539) |
| Range, Beneficiary HRR Population | 61–2275 | 61–962 | 71–1514 | 88–2275 | 87–2123 | 167–2158 |
| Rural (%) | 32% (26%) | 51% (27%) | 46% (20%) | 32% (21%) | 23% (24%) | 6% (10%) |
| Age (years) | 75 (1) | 76 (1) | 75 (1) | 75 (1) | 75 (1) | 76 (1) |
| Gender | ||||||
| Female (%) | 56% (2%) | 55% (2%) | 55% (1%) | 56% (1%) | I 56% (1%) | 57% (2%) |
| Male (%) | 44% (2%) | 45% (2%) | 45% (1%) | 44% (1%) | ‘4% (1%) | 43% (2%) |
| Race | ||||||
| Non-Hispanic White (%) | 85% (13%) | 91% (10%) | 89% (9%) | 86% (9%) | 84% (12%) | 75% (15%) |
| African American (%) | 6% (8%) | 3% (6%) | 5% (7%) | 8% (8%) | 7% (7%) | 9% (8%) |
| Hispanic (%) | 5% (9%) | 1% (1%) | 3% (5%) | 3% (5%) | 7% (12%) | 10% (12%) |
| Other Unknown | 4% (5%) | 4% (8%) | 3% (3%) | 3% (2%) | 3% (2%) | 7% (6%) |
Notes: Data is presented as n (%) or mean (standard deviation).
This table presents data from the entire population.
Abbreviations: HRR = Hospital Referral Region
End-of-Life Spending in COPD
As shown in Figure 1a, significant geographic variation existed in overall end-of-life spending. High spending HRRs existed in highly-populated and major metropolitan areas. As shown in Table 2, the average ASR-adjusted overall spending per decedent with COPD during the last two years of life was $61,271±$11,639. Reimbursement for inpatient care accounted for 40.2% of overall spending ($24,626±$6,192 per decedent; Appendix Figure 1). Part-B accounted for 16.8% of overall spending ($10,309±$3,001 per decedent), with the greatest proportion allocated to emergency room reimbursement ($4,883±$1,720 per decedent). SNF spending accounted for 11.6% of overall spending ($7,101±$2,403 per decedent), and hospice spending accounted for 10.3% ($6,307±$2,201 per decedent). Outpatient spending accounted for less than 10% of overall spending (Table 2 and Appendix Figure 1).
Figure 1. Variation in Overall Medicare Spending Among Older Adults with COPD During the Last Two Years of Life.
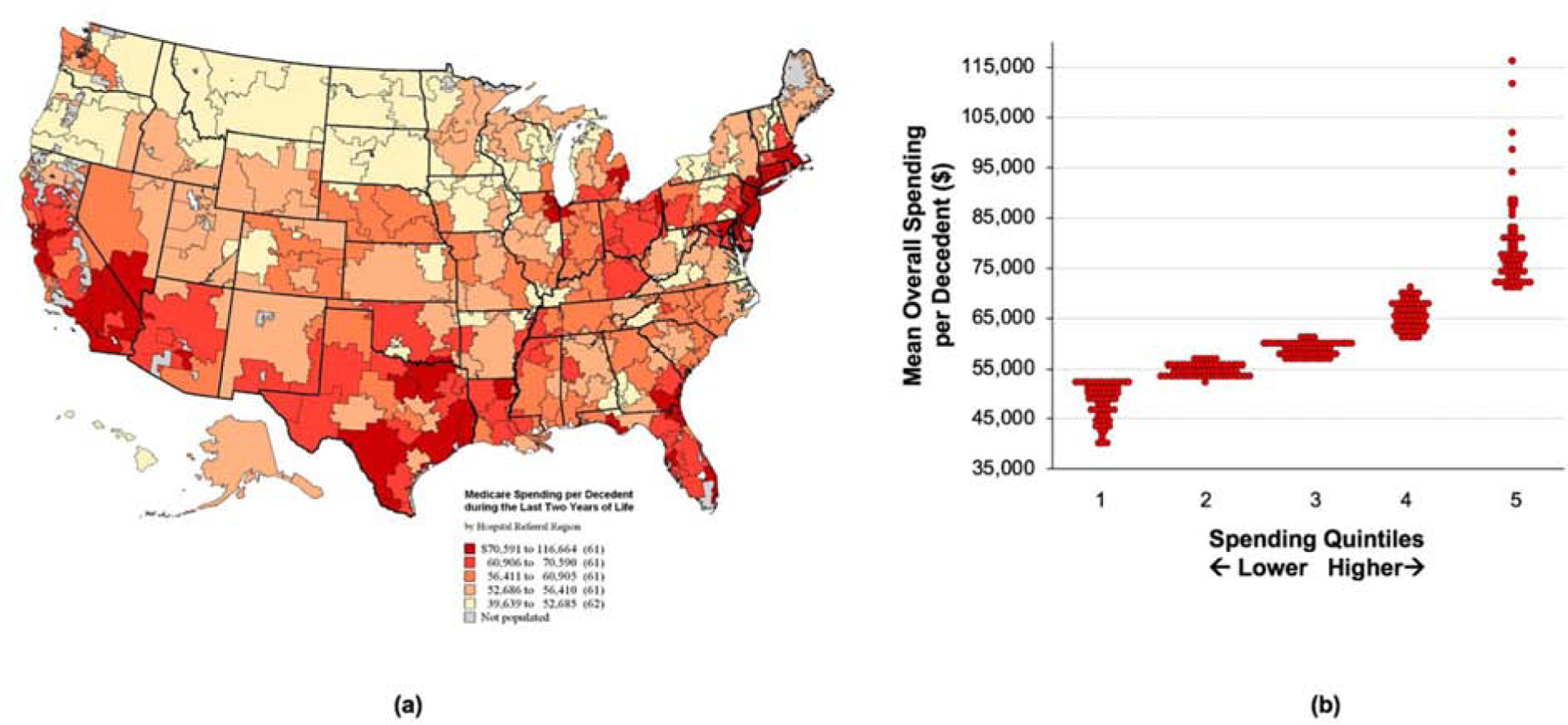
(a) This map illustrates geographic variation across the US in Medicare spending per decedent during the last two years of life. HRRs are color-coded across quintiles of increasing spending. (b) This turnip plot demonstrates the distribution in mean overall spending per decedent within and across spending quintiles.
Table 2.
COPD-Specific Spending per Decedent in the Last Two years of Life by Spending Quintiles, Adjusted for Age, Sex, and Race (n=146,240)
| Overall | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | |
|---|---|---|---|---|---|---|
| Spending Categories | ||||||
| Overall Spending ($) | 61271 (11639) |
48288 (3665) |
54582 (1157) |
58828 (1298) |
65418 (2689) |
79453 (9242) |
| Inpatient Reimbursement ($) |
24626 (6192) |
20137 (2469) |
22198 (2620) |
22782 (1781) |
25001 (3446) |
33084 (7980) |
| Skilled Nursing Facility ($) | 7101 (2403) |
5079 (1340) |
5794 (1150) |
6865 (1388) |
7611 (1722) |
10155 (2353) |
| Outpatient Facility ($) | 4740 (1231) |
5311 (1515) |
4970 (1276) |
4751 (1062) |
4433 (1043) |
4226 (873) |
| Outpatient Physician ($) | 150 (169) |
246 (197) |
195 (209) |
150 (129) |
104 (80) |
66 (166) |
| Medical Equipment ($) | 1816 (369) |
1781 (359) |
1864 (288) |
1886 (450) |
1779 (362) |
1770 (364) |
| Home Health Aide ($) | 3757 (1712) |
2244 (966) |
3400 (1331) |
3681 (1420) |
4577 (1673) |
4884 (1699) |
| Long T erm Care ($) | 3841 (2589) |
1729 (961) |
2475 (1188) |
3304 (1277) |
4602 (2567) |
5539 (3312) |
| Hospice ($) | 6307 (2201) |
5646 (2680) |
6296 (2182) |
6418 (1929) |
6877 (1899) |
6310 (2107) |
| Part-B Spending | ||||||
| Overall Part-B Spending ($) | 10309 (3001) |
7420 (1406) |
8517 (1309) |
9846 (1150) |
11450 (2421) |
14358 (2188) |
| Emergency Room ($) | 4883 (1720) |
3363 (665) |
3765 (578) |
4549 (632) |
5372 (1119) |
7388 (1487) |
| Imaging ($) | 777 (243) |
562 (129) |
655 (140) |
747 (125) |
891 (269) |
1033 (181) |
| Procedures ($) | 1747 (518) |
1326 (239) |
1503 (259) |
1656 (268) |
1962 (621) |
2294 (426) |
| Tests ($) | 635 (240) |
442 (139) |
537 (158) |
620 (147) |
703 (247) |
876 (230) |
| Ambulance ($) | 1185 (305) |
961 (250) |
1151 (338) |
1214 (267) |
1300 (296) |
1304 (234) |
| Other ($) | 2256 (714) |
1719 (558) |
2043 (652) |
2263 (600) |
2513 (673) |
2749 (616) |
Notes: Data is presented as mean (standard deviation).
As shown in Figure 1b, substantial variation in overall spending existed across spending quintiles, with some HRRs in the highest spending quintile exceeding $100,000 on average per decedent. We observed a nearly two-fold variation in overall spending across spending quintiles ($48,288±$3,665 to $79,453±$9,242; Table 2), with HRRs in higher spending quintiles spending more on average in all categories except for ambulatory care (Figure 2). Hospice spending varied within but not across spending quintiles.
Figure 2. Variation in Categorical Spending Across Spending Quintiles for Older Adults with COPD.
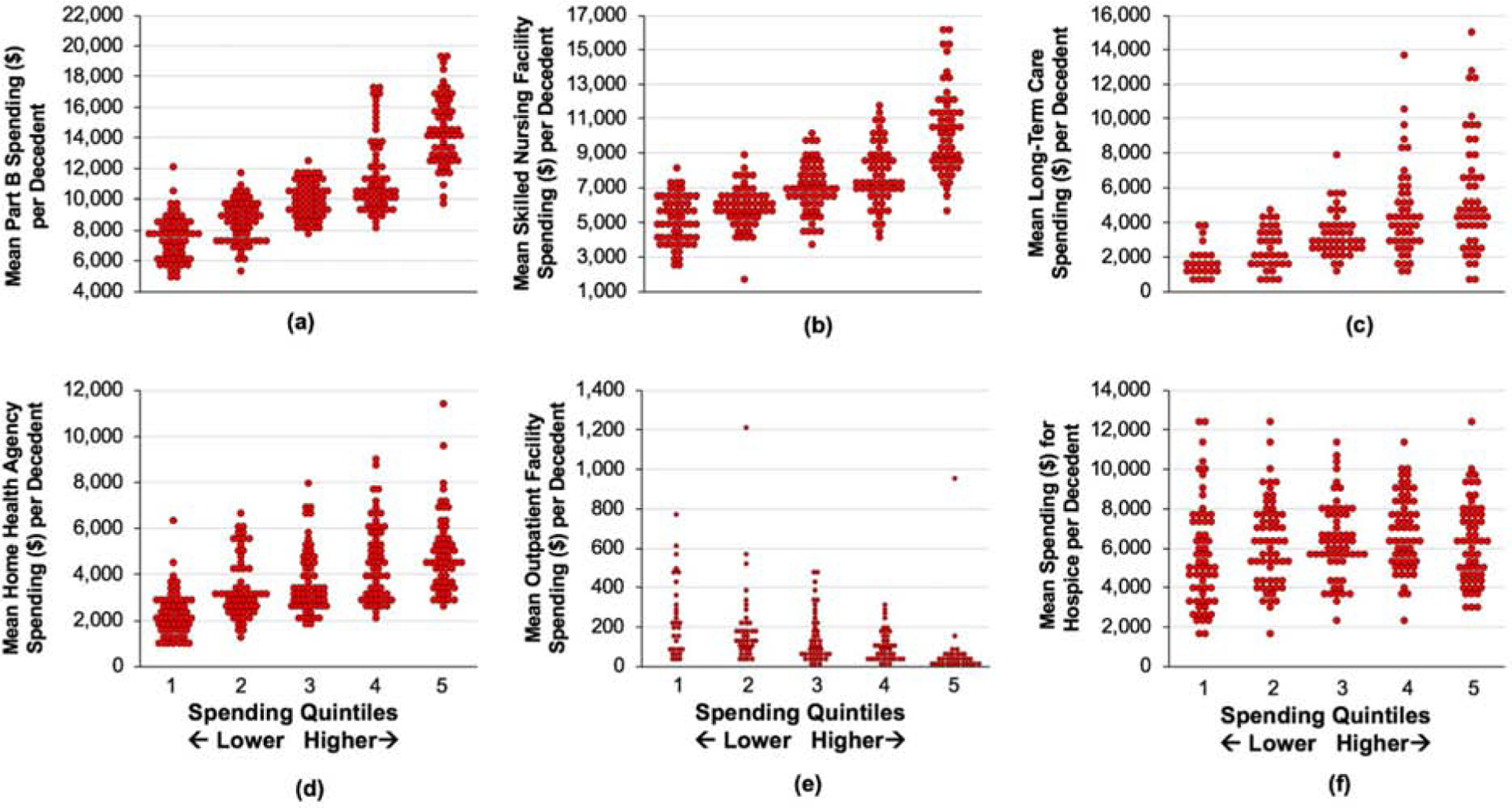
This graph demonstrates the variation in mean spending per decedent across spending quintiles during the last two years of life for the following categories: a) Part B; b) skilled nursing facility; c) long-term care; d) home health agency; e) outpatient facility; and f) hospice.
End-of-Life Healthcare Utilization in COPD
As shown in Table 3, 82%±4% of decedents with COPD were admitted to a hospital on average for 13.7±3.1 days, 55%±11% to an intensive care unit for 5.4±2.5 days, and 38%±7% to a SNF for 18.7±4.9 days on average in the last two years of life. Nearly all (99%) decedents had emergency care during that timeframe, 49%±9% used home health, and 12%±7% were admitted to a long-term care facility. HRRs in the highest spending quintiles compared to HRRs in the lowest quintiles exhibited a 1.5-fold longer LOS for the ICU (Table 3). Substantial geographic and spending quintile variation existed in hospital and ICU admissions, with some HRRs in the highest spending quintiles exceeding 20 inpatient days and 10 ICU days for COPD in the last two years of life (Appendix Figure 2).
Table 3.
COPD-Specific Healthcare Utilization per Decedent in the Last Two Years of Life, Adjusted for Age, Sex, and Race (n=146,240)
| Variables | Overall | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
|---|---|---|---|---|---|---|
| Frequency of Encounters Per-Decedent | ||||||
| Inpatient | 82% (4%) | 78% (5%) | 81% (4%) | 82% (4%) | 83% (3%) | 85% (3%) |
| ICU Admission | 55% (11%) | 44% (9%) | 50% (8%) | 56% (7%) | 58% (8%) | 64% (10%) |
| Skilled Nursing Facility | 38% (7%) | 34% (7%) | 35% (6%) | 39% (6%) | 39% (5%) | 43% (6%) |
| Medical Equipment | 73% (4%) | 72% (5%) | 74% (4%) | 74% (4%) | 74% (4%) | 72% (3%) |
| Home Health Aide | 49% (9%) | 40% (9%) | 47% (8%) | 49% (7%) | 54% (6%) | 54% (5%) |
| Long-Term Care | 12% (7%) | 7% (5%) | 9% (5%) | 11% (4%) | 15% (8%) | 15% (8%) |
| Hospice Enrollment | 47% (9%) | 44% (10%) | 46% (9%) | 48% (7%) | 50% (7%) | 45% (9%) |
| Part-B Durable Medical Equipment | 4% (2%) | 4% (1%) | 4% (2%) | 4% (2%) | 4% (2%) | 5% (2%) |
| Part-B Emergency | 99% (1%) | 99% (1%) | 99% (1%) | 100% (‘%) | 99% (1%) | 99% (1%) |
| Part-B Imaging | 97% (2%) | 96% (2%) | 97% (2%) | 98% (1%) | 98% (1%) | 98% (1%) |
| Part-B Procedures | 89% (5%) | 85% (5%) | 87% (4%) | 90° (3%) | 91% (3%) | 92% (3%) |
| Part-B Ambulance | 75% (10%) | 70% (10%) | 72% (12%) | 75% (10%) | 79% (8%) | 80% (5%) |
| Part-B Tests | 96% (3%) | 94% (3%) | 96% (2%) | 97% (2%) | 97% (2%) | 97% (1%) |
| Part-B Other | 93% (5%) | 89% (6%) | 92% (5 | 94% (2%) | 95% (3%) | 96% (2%) |
| Number of Visits Per-Decedent | ||||||
| Inpatient Physician | 30.7 (13.4) | 19.3 (5.4) | 22.9 (5.8) | 28.6 (6.5) | 35.0 (10.0) | 47.9 (13.7) |
| Emergency Room | 2.9 (0.5) | 2.5 (0.6) | 2.9 (0.5) | 3.1 (0.4) | 3.1 (0.4) | 3.0 (0.3) |
| Home Health | 24.4 (13.7) | 14.4 (7.3) | 23.7 (11.7) | 23.9 (11.9) | 30.1 (13.7) | 29.7 (16.3) |
| Primary Care Physician | 24.1 (4.9) | 20.0 (3.4) | 21.9 (3.1) | 23.4 (2.6) | 25.7 (3.6) | 29.2 (5.4) |
| Specialist Physician | 22.9 (10.6) | 13.9 (4.3) | 16.3 (4.5) | 21.2 (4.8) | 26.7 (8.6) | 36.5 (10.0) |
| Rural and Federally Qualified Health Clinics | 1.4 (1.4) | 2.0 (1.6) | 1.8 (1.7) | 1.5 (1.2) | 1.1 (1.0) | 0.6 (1.3) |
| Length of Stay Per-Decedent (Days) | ||||||
| Inpatient | 13.7 (3.6) | 11.2 (2.4) | 12.5 (2.0) | 13.4 (1.9) | 14.4 (1.9) | 17.1 (3.2) |
| ICU | 5.4 (2.5) | 3.3 (1.4) | 4.3 (1.5) | 5.3 (1.6) | 6.0 (1.8) | 8.1 (2.7) |
| Skilled Nursing Fa’ilit. | 18.7 (4.9) | 14.8 (3.8) | 16.9 (3.7) | 19.1 (4.2) | 20.0 (4.6) | 22.8 (4.3) |
| Hospice | 39.7 (14.8) | 37.1 (17.8) | 42.7 (15.6) | 41.0 (13.0) | 42.8 (12.4) | 35.1 (13.2) |
Notes: Data is presented as n (%) or mean (standard deviation).
Hospice Use in COPD
Overall, 47%±9% of decedents with COPD used hospice for 39.7±14.8 days during the last two years of life (Table 3). There was substantial geographic variation in hospice use, with no clear patterns emerging (Figure 3a). HRRs in Oregon, Nevada, Texas, Iowa, Georgia, and Florida frequently used hospice, while those in the central northwest had HRRs with rare hospice use. Similar to hospice spending, hospice use varied within but not across spending quintiles (Figure 3b).
Figure 3. Hospice Use During the Last Two Years of Life for Older Adults with COPD.
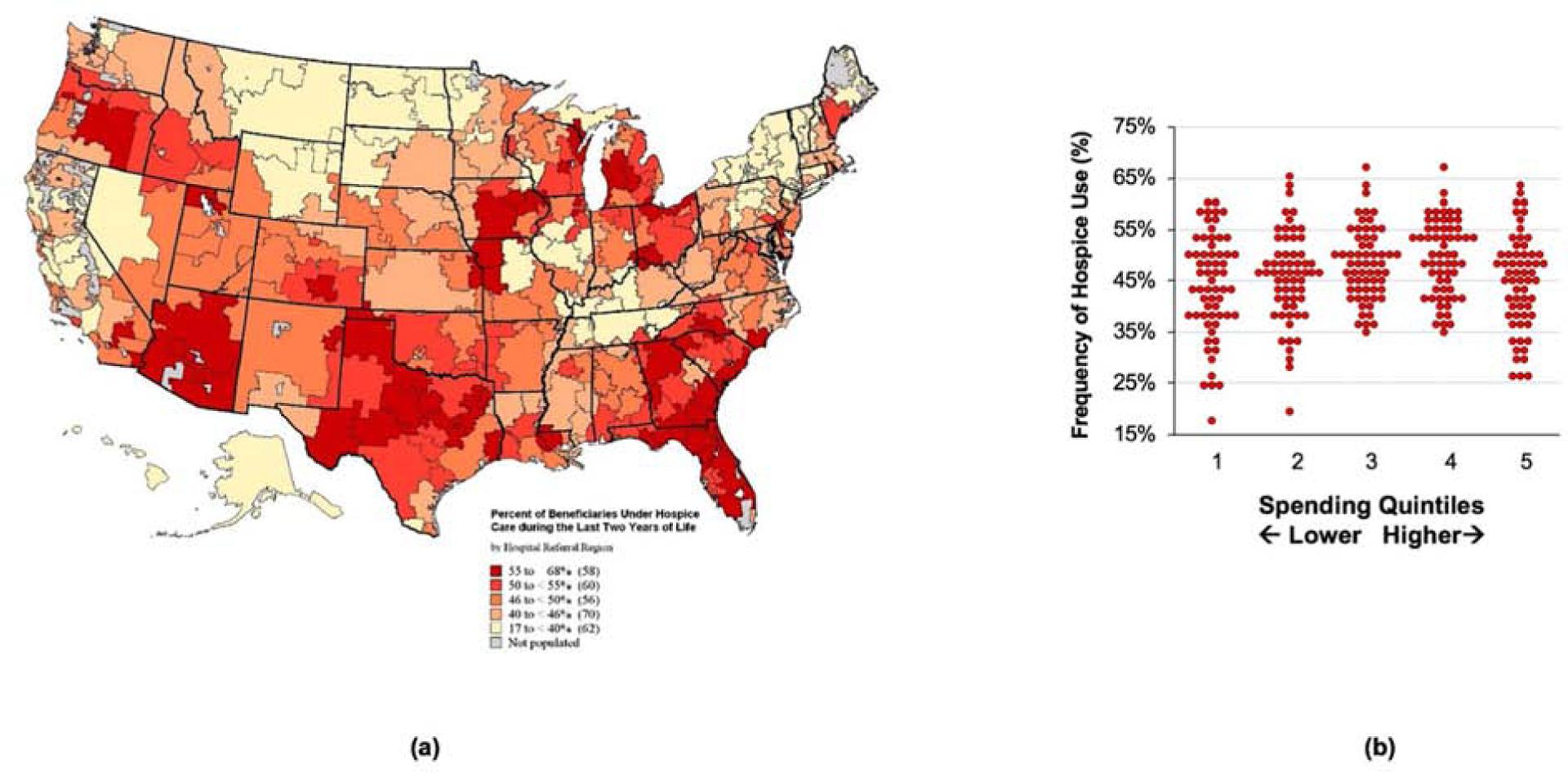
(a) This map illustrates the variation in hospice use in the last two years for older adults with COPD across the US. (b) This turnip plot demonstrates the variation in hospice use within and across spending quintiles.
DISCUSSION
In a decedent cohort of older Medicare beneficiaries with COPD who died between 2013–2014, end-of-life spending and health care utilization exhibited substantial variation nationwide. HRRs in higher spending quintiles compared to lowest spending quintiles spent nearly two-fold more on acute and post-acute care during the terminal phase of illness, which is consistent with data from the oncology literature.4,17 Though nearly half of the cohort used hospice, disparities in hospice use existed nationwide, and LOS in hospice was limited to one month on average. In some geographic areas, fewer than one in five decedents with COPD used hospice in the terminal phase of illness. Policy and clinical efforts addressing high end-of-life utilization of acute and post-acute care and nationwide disparities in hospice use in COPD are desperately needed.
Our data echo previous analyses of general populations of older adults with serious illness that also illustrated significant geographic and spending variability in end-of-life care.13,15 Older decedents with COPD in our cohort had high utilization of high-intensity acute care during the last two years of life, including hospitalizations (82%), ICU admissions (55%), emergency room visits (99%), imaging (97%), procedures (89%), and tests (96%). The acute care utilization in our cohort appears higher than a comparison population of older Medicare beneficiaries with dementia, only half of whom were hospitalized and visited the emergency room in the last year of life.18
Hospitalizations represent critical events in COPD that are associated with poor outcomes.7,19 With limited and variable access to pulmonologists in the US, primary care clinicians deliver the majority of care for COPD patients.20 In our cohort, HRRs in higher spending quintiles used more subspecialists overall yet also had more inpatient and ICU encounters per decedent and nearly two-fold longer LOS for acute care. The mean hospital LOS of 14 days in our study was longer than data from European populations of 8 days on average.21 Data demonstrate that older age, multimorbidity, mechanical ventilation, and COPD severity are associated with longer hospitalizations.22,23 However, many of these factors are non-modifiable, and few systems have yet to implement interventions that address the social determinants of health which also impact COPD hospitalizations.24 In the meantime, retrospective data indicate potential quality improvement initiatives which may be associated with reduced LOS and warrant further prospective research.25–27
Policies could also focus on standardizing COPD management in the post-acute care setting for older adults with COPD, which is often not guideline-directed28–30 and is challenging due to multiple transitions of care to home. In our cohort, 38% used SNF with the number of visits and LOS increasing across spending quintiles. Data have demonstrated that COPD patients discharged to SNF have increased risk for mortality and readmissions,31 and COPD-specific care delivered at SNFs is often not guideline-directed.32 In addition to improving the standardization of COPD care in acute and post-acute care facilities, policies focused on improving transitions of care from the hospital to the home and dissemination of COPD management guidelines to SNFs, long-term care facilities, and home health agencies may also be needed
Finally, we were surprised by the high frequency of hospice use (47%) in our cohort, especially with prior data demonstrating limited access in COPD and a low frequency (6%) of hospice deaths attributable to COPD in contrast to its nationwide rank.11 Despite the relatively high utilization of hospice in our cohort compared to prior studies, hospice was the only category that did not demonstrate an association with overall spending (Figure 2f). This could be due to multiple factors. First, significant geographic disparities in hospice use existed, with some HRRs exhibiting very low hospice use. This geographic variation has previously been demonstrated in the general population but not in a COPD cohort specifically.33 Second, significant variation in hospice spending and use existed within spending quintiles as demonstrated by the wide dispersions in Figure 2f and Figure 3b, respectively. Third, hospice spending did not show a proportionate increase across spending quintiles as would be expected with illness severity (Appendix Figure 1). Veterans with advanced cancer who received hospice had better quality of end-of-life care and less aggressive interventions at the end of life.8 However, length of time in hospice in our cohort was limited to roughly one month on average. To impact end-of-life care in COPD will require policies that enact palliative care proactively in the COPD trajectory before the terminal phase of illness to treat comprehensive symptoms, to engage in proactive outlook plan, and to transition to hospice earlier. Early specialist and nurse-led palliative care improved outcomes in cancer.34,35 However, several barriers exist to implementing early palliative care in COPD, including misconceptions among pulmonologists that palliative care is only end-of-life care and a lack of consensus specialist palliative care referral criteria in COPD.36 Efforts to address these barriers must be considered during policy implementation.
Several limitations exist in this study. We did not have access to data on spirometry to determine COPD severity, and inaccuracy of ICD coding can be a concern. However, this was a decedent cohort in the terminal phase of illness who were likely to have had more severe COPD, and claims-based diagnoses identify COPD with reasonable accuracy.37 Additionally, our analysis of Medicare beneficiaries limits generalizability across payer status and to those with Medicare Advantage or who may have paid out of pocket for services. However, Medicare spending accounts for the greatest proportion of COPD spending across payers in older adults.3 Furthermore, we were unable to differentiate the type of hospice care within our data set (e.g. home-based versus facility-based), which may limit analyses of spending gaps and hospice use. Finally, we recognize that the analysis included decedents from 2013–2014. Since this time, COPD was added as a diagnosis to the Hospital Readmission Reduction Program and palliative care has expanded overall, so further analyses will be needed in the context of these changes.38 Nonetheless, our results and conclusions are relevant now as there have been no major changes in the interim regarding COPD treatment near the end of life nor updates to guidelines specifically focused on end-of-life care in COPD that could substantially alter the results or conclusions.39,40 Despite these limitations, our analysis is the first to target the variation in COPD-specific spending, health care utilization, and hospice use during the last two years of life for a large cohort of decedents with COPD.
CONCLUSION
In a cohort of older Medicare beneficiaries who died with COPD between 2013–2014, end-of-life spending and health care utilization during the last two years of life varied substantially nationwide. HRRs in the highest spending quintiles spent nearly two-fold more on acute care and post-acute care. While hospice use was higher than expected, significant geographic disparities in use existed nationwide. These data can guide policies to improve the delivery of patient-centered end-of-life care for older adults with COPD. Future analyses should examine HRR- and patient-level characteristics associated with higher spending and utilization and examine rural-urban disparities in end-of-life care in COPD.
Supplementary Material
Highlights.
End-of-life spending in decedents with COPD varies nationwide.
Acute care drives the majority of end-of-life spending in COPD.
82% of decedents with COPD were hospitalized and half to an ICU at the end of life.
One-third of decedents with COPD used a skilled nursing facility at the end of life.
Half of COPD decedents used hospice, though geographic variation existed.
Abbreviations List:
- COPD
chronic obstructive pulmonary disease
- HRR
hospital referral region
- LOS
length of stay
- SNF
skilled nursing facility
- ASR
age-sex-race
- ICU
intensive care unit
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: ASI is supported by an AHRQ K12 (K12HS023009) awarded to the Center for Outcomes and Effectiveness Research and Education (COERE) at the University of Alabama at Birmingham, and by a Palliative Research Enhancement Project (PREP) pilot award from the UAB Center for Palliative and Supportive Care. CJB is supported by a VA Rehabilitation R&D Scientific Merit Award. MTD is supported by grants from NIH (1K24HL140108), Department of Defense, American Lung Association, contracted clinical trials from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, PneumRx/BTG, Pulmonx, and reports consulting from AstraZeneca, GlaxoSmithKline, Mereo, PneumRx/BTG, and Quark. MAB is supported by NR013665–01A1, NR011871–01, PCORI PLC-1609–36381, PLC-1609–36714. CAG, SSA, CSL, and JEB have no conflicts to report.
References
- 1.Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2016 NCHS Data Brief. Hyattsville, MD: National Center for Health Statistics;2017. [Google Scholar]
- 2.Khakban A, Sin DD, FitzGerald JM, et al. The Projected Epidemic of Chronic Obstructive Pulmonary Disease Hospitalizations over the Next 15 Years. A Population-based Perspective. Am J Respir Crit Care Med. 2017;195(3):287–291. [DOI] [PubMed] [Google Scholar]
- 3.Khakban A, Sin DD, FitzGerald JM, et al. Ten-Year Trends in Direct Costs of COPD: A Population-Based Study. Chest 2015;148(3):640–646. [DOI] [PubMed] [Google Scholar]
- 4.Morden NE, Chang CH, Jacobson JO, et al. End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health affairs. 2012;31(4):786–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teno JM, Gozalo P, Trivedi AN, et al. Site of Death, Place of Care, and Health Care Transitions Among US Medicare Beneficiaries, 2000–2015. JAMA. 2018;320(3):264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelley AS, Morrison RS. Palliative Care for the Seriously Ill. N Engl J Med. 2015;373(8):747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miravitlles M, Ferrer M, Pont A, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004;59(5):387–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mor V, Wagner TH, Levy C, et al. Association of Expanded VA Hospice Care With Aggressive Care and Cost for Veterans With Advanced Lung Cancer. JAMA Oncol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gozalo P, Plotzke M, Mor V, Miller SC, Teno JM. Changes in Medicare costs with the growth of hospice care in nursing homes. N Engl J Med. 2015;372(19):1823–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yim CK, Barron Y, Moore S, et al. Hospice Enrollment in Patients With Advanced Heart Failure Decreases Acute Medical Service Utilization. Circ Heart Fail. 2017;10(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yaqoob ZJ, Al-Kindi SG, Zein JG. Trends and Disparities in Hospice Use Among Patients Dying of COPD in the United States. Chest. 2017;151(5):1183–1184. [DOI] [PubMed] [Google Scholar]
- 12.Rush B, Hertz P, Bond A, McDermid RC, Celi LA. Use of Palliative Care in Patients With End-Stage COPD and Receiving Home Oxygen: National Trends and Barriers to Care in the United States. Chest. 2017;151(1):41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodman DC, Esty AR, Fisher ES, Chang C. Trends and Variation in End-of-Life Care for Medicare Beneficiaries with Severe Chronic Illness. A Report of the Dartmouth Atlas Project. 2011. www.dartmouthatlas.org/downloads/reports/EOL_Trend_Report_0411pdf. Accessed August 1, 2019. [PubMed] [Google Scholar]
- 14.Keating NL, Landrum MB, Huskamp HA, et al. Dartmouth Atlas Area-Level Estimates of End-of-Life Expenditures: How Well Do They Reflect Expenditures for Prospectively Identified Advanced Lung Cancer Patients? Health Serv Res. 2016;51(4):1584–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. Bmj. 2004;328(7440):607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 2014;12(12):1500–1524. [DOI] [PubMed] [Google Scholar]
- 17.Miesfeldt S, Murray K, Lucas L, Chang CH, Goodman D, Morden NE. Association of age, gender, and race with intensity of end-of-life care for Medicare beneficiaries with cancer. J Palliat Med. 2012;15(5):548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amjad H, Carmichael D, Austin AM, Chang CH, Bynum JP. Continuity of Care and Health Care Utilization in Older Adults With Dementia in Fee-for-Service Medicare. JAMA Intern Med. 2016;176(9):1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corlateanu A, Botnaru V, Covantev S, Dumitru S, Siafakas N. Predicting Health-Related Quality of Life in Patients with Chronic Obstructive Pulmonary Disease: The Impact of Age. Respiration. 2016;92(4):229–234. [DOI] [PubMed] [Google Scholar]
- 20.Croft JB, Lu H, Zhang X, Holt JB. Geographic Accessibility of Pulmonologists for Adults With COPD: United States, 2013. Chest. 2016;150(3):544–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruparel M, Lopez-Campos JL, Castro-Acosta A, Hartl S, Pozo-Rodriguez F, Roberts CM. Understanding variation in length of hospital stay for COPD exacerbation: European COPD audit. ERJ Open Res. 2016;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harries TH, Thornton HV, Crichton S, Schofield P, Gilkes A, White PT. Length of stay of COPD hospital admissions between 2006 and 2010: a retrospective longitudinal study. Int J Chron Obstruct Pulmon Dis. 2015;10:603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quintana JM, Unzurrunzaga A, Garcia-Gutierrez S, et al. Predictors of Hospital Length of Stay in Patients with Exacerbations of COPD: A Cohort Study. J Gen Intern Med. 2015;30(6):824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franssen FME, Smid DE, Deeg DJH, et al. The physical, mental, and social impact of COPD in a population-based sample: results from the Longitudinal Aging Study Amsterdam. NPJ primary care respiratory medicine. 2018;28(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alshabanat A, Otterstatter MC, Sin DD, et al. Impact of a COPD comprehensive case management program on hospital length of stay and readmission rates. Int J Chron Obstruct Pulmon Dis. 2017;12:961–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gulati S, Zouk AN, Kalehoff JP, et al. The use of a standardized order set reduces systemic corticosteroid dose and length of stay for individuals hospitalized with acute exacerbations of COPD: a cohort study. Int J Chron Obstruct Pulmon Dis. 2018;13:2271–2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parikh R, Shah TG, Tandon R. COPD exacerbation care bundle improves standard of care, length of stay, and readmission rates. Int J Chron Obstruct Pulmon Dis. 2016;11:577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Visentin E, Nieri D, Vagaggini B, Peruzzi E, Paggiaro P. An observation of prescription behaviors and adherence to guidelines in patients with COPD: real world data from October 2012 to September 2014. Current medical research and opinion. 2016;32(9):1493–1502. [DOI] [PubMed] [Google Scholar]
- 29.Foda HD, Brehm A, Goldsteen K, Edelman NH. Inverse relationship between nonadherence to original GOLD treatment guidelines and exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lipari M, Smith AL, Kale-Pradhan PB, Wilhelm SM. Adherence to GOLD Guidelines in the Inpatient COPD Population. J Pharm Pract 2018;31(1):29–33. [DOI] [PubMed] [Google Scholar]
- 31.Ganapathy V, Stensland MD. Health resource utilization for inpatients with COPD treated with nebulized arformoterol or nebulized formoterol. Int J Chron Obstruct Pulmon Dis. 2017;12:1793–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel M, Steinberg K, Suarez-Barcelo M, Saffel D, Foley R, Worz C. Chronic Obstructive Pulmonary Disease in Post-acute/Long-term Care Settings: Seizing Opportunities to Individualize Treatment and Device Selection. Journal of the American Medical Directors Association. 2017;18(6):553 e517–553 e522. [DOI] [PubMed] [Google Scholar]
- 33.Connor SR, Elwert F, Spence C, Christakis NA. Geographic variation in hospice use in the United States in 2002. J Pain Symptom Manage. 2007;34(3):277–285. [DOI] [PubMed] [Google Scholar]
- 34.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. [DOI] [PubMed] [Google Scholar]
- 35.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a Palliative Care Intervention on Clinical Outcomes in Patients with Advanced Cancer: The Project ENABLE II Randomized Controlled Trial. JAMA. 2009;302(7):741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iyer A, Dionne-Odom J, Khateeb D, et al. A Qualitative Study of Pulmonary and Palliative Care Clinician Perspectives on Early Palliative Care in Chronic Obstructive Pulmonary Disease. Journal of Palliative Medicine. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Macaulay D, Sun SX, Sorg RA, et al. Development and validation of a claims-based prediction model for COPD severity. Respiratory medicine. 2013;107(10):1568–1577. [DOI] [PubMed] [Google Scholar]
- 38.Krishnan JA, Gussin HA, Prieto-Centurion V, Sullivan JL, Zaidi F, Thomashow BM. Integrating COPD into Patient-Centered Hospital Readmissions Reduction Programs. Chronic obstructive pulmonary diseases. 2015;2(1):70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912–927. [DOI] [PubMed] [Google Scholar]
- 40.Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: A Review of the 2018 GOLD Report. Mayo Clinic proceedings. 2018;93(10):1488–1502. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


