Abstract
Objective:
To measure caregiver and clinician perception of false memories in the lives of patients with memory loss due to Alzheimer’s disease (AD) and Mild Cognitive Impairment (MCI) using a novel false memories questionnaire. Our hypotheses were that false memories are occurring as often as forgetting according to clinicians and family members.
Method:
This prospective, questionnaire-based study consisting of 20 false memory questions paired with 20 forgetting questions, had two forms: one for clinicians and the other for family members of older subjects. 226 Clinicians and 150 family members of 49 patients with AD, 44 patients with mild cognitive impairment (MCI), and 57 healthy older controls (OCs) completed the questionnaire.
Results:
False memories occurred nearly as often as forgetting according to clinicians and family members of patients with MCI and AD. Family members of OCs and patients with MCI had fewer false memories compared to those of the AD group. As MMSE scores decreased, the mean score increased for both forgetting and false memories. Among clinicians, correlations were observed between the dementia severity of patients seen with both forgetting and false memories questionnaire scores as well as with the impact of forgetting and false memories on daily life.
Conclusion:
Patients with AD experience false memories almost as frequently as they do forgetting. Given how common false memories are in AD patients, additional work is needed to understand the clinical implications of these false memories on patients’ daily lives. The novel false memories questionnaire developed may be a valuable tool.
Keywords: alzheimer’s disease, dementia, mild cognitive impairment, everyday function, memory and surveys
Introduction
Non-pharmacological techniques such as pill boxes and reminder notes can enable individuals with moderate or even severe amnesia due to stroke or encephalitis to live independently (Acevedo & Loewenstein, 2007). These memorial aids typically fail in patients with Alzheimer’s disease (AD) due, in part, to an increased tendency to form false memories (Malone et al., 2018). False memories may occur in several forms. For example false memories may be related to events that never occurred or to events that are distorted or mis-remembered (Malone et al., 2018). It is possible that false memories have an equal or greater impact on function in the lives of patients with mild cognitive impairment (MCI) and AD dementia compared to forgetting itself. For example, elevated rates of false memories in AD patients increase the likelihood that patients will mis-remember having taken their medications or turned off the stove when they have not performed these activities.
Using experimental methods developed to examine false memory in healthy individuals (Cotel, Gallo, & Seamon, 2008; Devitt & Schacter, 2016; Norman & Schacter, 1997; Daniel L. Schacter, Israel, & Racine, 1999), we and others have examined false memories in patients with AD in laboratory settings. This work established that many AD patients’ false memories were related to the fact that they could remember the general idea, meaning, or gist of an event, but not the specific details (Budson, Daffner, Desikan, & Schacter, 2000). Part of their difficulty with false memories was related to the fact that patients have an abnormal sense of familiarity for things that were actually new (Deason et al., 2017).
In the laboratory, patients with AD show higher rates of false memories than do healthy older adults and those with amnesia due to other causes, possibly related to an abnormal liberal response bias (Budson, Wolk, Chong, & Waring, 2006; Koutstaal, Verfaellie, & Schacter, 2001; D. L. Schacter, Verfaellie, Anes, & Racine, 1998; Snodgrass & Corwin, 1988). Furthermore, false memories among possible AD patients may be a more specific indicator of AD pathology than memory performance alone (Hildebrandt, Haldenwanger, & Eling, 2009a, 2009b). One longitudinal investigation of preclinical AD has shown that distorted and false memories may be useful clinically for identifying preclinical AD (Schmid, Taylor, Foldi, Berres, & Monsch, 2013).
Thus, false memories may have diagnostic and prognostic value for patients with memory disorders that can be used by their clinicians. In addition, it is generally accepted by the clinical and scientific community that disruption of memory impacts function in AD patients, and thus we believe that false memories are likely to have significant functional impact as well.
It is important to better understand the cognitive and physiologic basis of false memories in MCI and AD so that interventions can be developed to reduce false and distorted memories, and thus help patients maintain function in daily life. Given the lack of a gold standard tool for assessing false memories in daily life, it was necessary to develop a questionnaire designed to measure the occurrence of false memories in the lives of patients with MCI and AD. Use of a false memories questionnaire may also improve our understanding of the basis of false memories that, in turn, may enable us to find ways to reduce false memories.
The present study set out to answer several main questions. First, how common are false memories in patients with AD, MCI, and older adults, when compared to forgetting? Second, what were clinicians’ impressions of how common false memories are in patients with AD compared to forgetting? These questions motivated our two hypotheses.
First, we hypothesized that false memories are occurring as often as forgetting in AD patients, which led us to measure the occurrence of false memories and forgetting in the daily lives of older controls (OC), MCI and AD patients according to the views of family members and clinicians. Second, since awareness of false memories may be related to clinicians’ experience level, we hypothesized that clinicians who have more contact with patients with MCI and AD would likely report that false memories are occurring as often as forgetting.
Methods
Family members.
150 family members of individuals with MCI (44 participants), AD dementia (49 participants), and healthy OCs (57 participants) were recruited from the Boston University Alzheimer’s Disease Center and the Veterans Affairs Boston Healthcare System, both in Boston, MA. Patients met criteria for MCI or probable AD dementia as described by the National Institutes of Aging–Alzheimer’s Association (Albert et al., 2011; McKhann et al., 2011). See Table 1 for Mini Mental State Examination (MMSE; (Folstein, Folstein, & McHugh, 1975) scores and demographics. Patients were assessed and diagnosed by a neurologist and/or neuropsychologist and were excluded for clinically significant depression, alcohol and drug use, prior stroke, traumatic brain injury, unstable medical condition, or other neurological disorder.
Table 1.
Family member data: Demographic and prevalence information from associated patients
| N | Age | Education | MMSE | forgetting prevalence** |
false memory prevalence** |
Average forgetting score |
Average false memories score |
|
|---|---|---|---|---|---|---|---|---|
| OC | 57 | 76.04d* | 16.79 | 29.37 | 10.53%(c) d†- | 7.02% (c)d†- | .66 | .48 |
| (SD) | (7.16) | d†b* | d†b† | - | 33.33%(l)b*d* | (.62) | (.48) | |
| (2.44) | (1.10) | 45.61%(l)d†b† | ||||||
| MCI | 44 | 79.88 | 15.11a* | 25.73 | 25.00%(c) d†- | 6.80%(c)d†- | .95 | .74 |
| (SD) | (7.98) | (2.85) | a†d† | 79.55%(l)a† | 63.64%(l)a*d* | (.59) | (.49) | |
| (5.56) | ||||||||
| AD | 49 | 81.65a* | 14.41a† | 19.44 | 69.39%(c) | 53.06%(c)a†b†- | 1.90 | 1.65 |
| (SD) | (7.79) | (2.79) | a†b† | a†b†- | 89.80%(l)a† b* | (.79) | (.84) | |
| (6.05) | 95.92%(l)a† |
Abbreviations: OC, Older Controls; MCI, patients with mild cognitive impairment; AD, patients with Alzheimer’s disease dementia. Standard deviations are in parentheses. One AD and one MCI subject were missing age and education.
different from OC
different from MCI
different from AD
p < .01
p < .001
conservative and
liberal estimates of forgetting prevalence, see methods for more details.
Clinicians.
226 clinicians who self-reported seeing patients with AD dementia as part of their practice were recruited for this study using flyers and direct recruitment following conference sessions by study staff members from four sources: 1) Harvard Dementia Update Course 2015 in Boston, MA; 2) Alzheimer’s Association International Conference 2015 in Washington, DC; 3) Gerontological Society of America Annual Scientific Meeting 2015 in Orlando, FL; and 4) online through Survey Monkey. Demographic information for clinicians can be found in Table 2. This study was approved by the Institutional Review Board at Boston University School of Medicine and the Veterans Affairs Boston Healthcare System.
Table 2.
Demographic information for clinicians
| Profession | Years in Practice (SD) |
Number of Clinicians that see >50% AD, MCI and other dementias |
Number of Clinicians that see 25-50% AD, MCI and other dementias |
Number of Clinicians that see 10-25% AD, MCI and other dementias |
Number of Clinicians that see 0- 10% AD, MCI and other dementias |
Mean Number of AD Patients Currently Followed (SD) |
Mean % of patients followed with very mild to mild AD |
Mean % of patients followed with moderate AD |
Mean % of patients followed with severe AD |
|---|---|---|---|---|---|---|---|---|---|
| Neurologist(N=43) | 17.81 (11.26) | 22 | 10 | 7 | 4 | 216.62 (265.86) | 39.53% | 40.35% | 18.81% |
| Geriatrician(N=41) | 20.85 (10.73) | 24 | 10 | 6 | 1 | 94.14 (103.73) | 33.23% | 42.33% | 24.76% |
| Nurse(N= 34) | 20.92 (11.01) | 23 | 6 | 3 | 2 | 242.29 (625.47) | 29.76% | 40.88% | 27.37% |
| Psychiatrist(N= 25) | 21.52 (12.17) | 7 | 8 | 3 | 7 | 68.77 (115.24) | 32.95% | 42.50% | 21.31% |
| Neuropsychologist(N=23) | 13.59 (10.88) | 17 | 4 | 2 | 0 | 87.27 (101.76) | 50.70% | 38.75% | 11.44% |
| Social Worker(N=21) | 16.60 (12.29) | 17 | 2 | 2 | 0 | 61.45 (95.12) | 35.27% | 40.83% | 21.76% |
| Psychologist(N=17) | 16.33 (11.63) | 9 | 5 | 2 | 1 | 52.33 (53.13) | 48.81% | 31.25% | 21.00% |
| *Other(N=12) | 15.08 (13.80) | 9 | 1 | 1 | 1 | 35.60 (45.90) | 33.41% | 39.66% | 27.72% |
| Internal Medicine(N=10) | 22.88 (12.27) | 1 | 3 | 5 | 1 | 46.88 (36.14) | 36.66% | 43.88% | 19.44% |
| Total / Mean(N= 226) | 18.70 (11.62) | 129 | 49 | 31 | 17 | 124.78 (275.89) | 21.15% | 16.19% | 15.35% |
Questionnaire Development and Validity Analysis
The false memories questionnaire is a novel, 40-item questionnaire with two versions: a family member version and a clinician version (see Appendices A and B for the complete questionnaire). Items on the questionnaire were largely designed to investigate forgetting and false memory in daily life, such as those concepts explored in the activities of daily living questionnaire (Lawton & Brody, 1969). In addition, two questions regarding function were added for clinicians. Each forgetting question was paired with a false memory question. For example, “How often do your patients/does your loved one forget to pay a bill?” was paired with “How often do your patients/does your loved one think they’ve paid a bill when they haven’t?” These pairs were placed adjacent to each other on the questionnaire. For each question, family members and clinicians were provided with the following response options (assigned to numeric values): Often = 3, Sometimes = 2, Rarely = 1, Never = 0, and Don’t Know (not scored).
The Clinician version started with questions regarding demographics, including medical specialty, years practicing, percentage of patients seen with MCI or AD dementia (item 3 of clinician questionnaire), how many patients with AD followed (item 4 of clinician questionnaire), and the average severity of the patients with AD. The questionnaires themselves were identical between the clinician and family member versions with the exception of the word “patient” in the clinician version replaced by the word “loved one” in the family member version and the addition of two questions in the clinician version regarding the impact of forgetting and false memories on patient function.
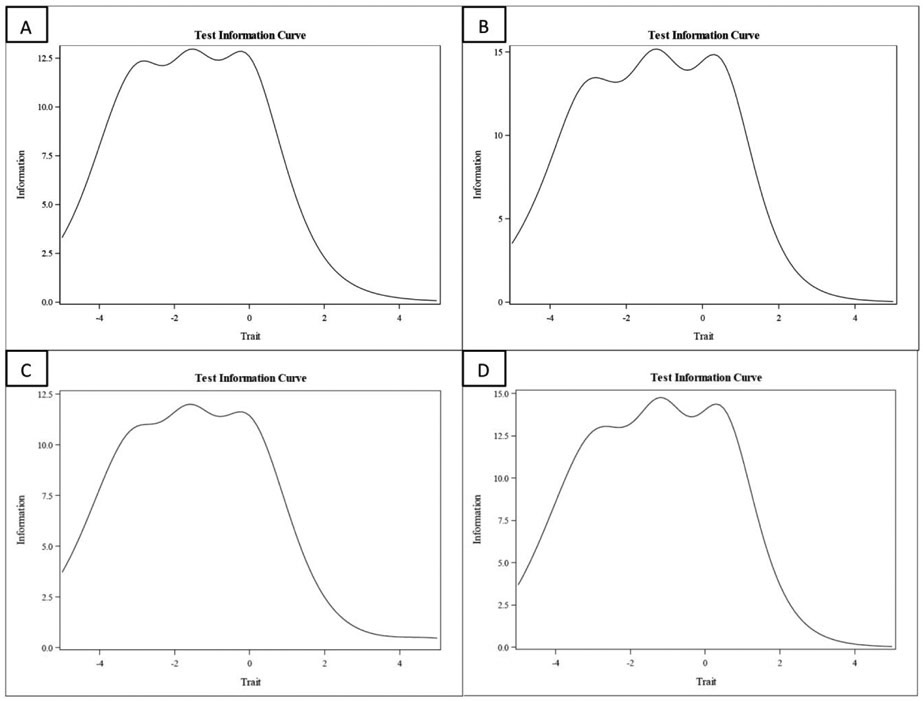
Confirmatory factor analyses (CFAs) were used to evaluate the dimensionality of each survey questionnaire. Item response theory (IRT) models were applied to each item question for purposes of item parameter estimation and evaluating test information functions for the false memory and forgetfulness questionnaires separately. One-dimensional IRT structures were parameterized with the two-parameter logistic model, which was applied to all 20-item questions with ordinal scores. A byproduct of IRT estimation is the ability to plot test information curves (TICs), which graphically represent the quality of measurement provided by an item question across the range of latent ability that underlies test takers’ performance. The higher the TIC is at a given level of the construct, the smaller the standard error of measurement. Hence, TICs are directly related to the reliability of each of the two tasks, completion of the forgetting questions and false memory questions as shown in Figure 1.
Figure 1.
A. Test information curve for clinician forgetting questions B. Test information curve for clinician false memory questions. C. Test information curve for family member forgetting questions. D. Test information curve for family member false memory questions.
Forgetting:
All question items were at least moderately related to the latent construct of forgetting and they varied from 0.61 to 0.87. Item slopes varied widely (2.0 to 6.5) as shown in Figure 1A & C. Cronbach’s alpha for forgetting questions for both clinicians and family members was very high (0.97).
False memory:
All question items were at least moderately related to the latent construct of false memory and they varied from 0.63 to 0.87. Item slopes varied widely (1.9 to 5.8) as shown in Figure 1B & D. As with the Forgetting questionnaire, Cronbach’s alpha for false memory questions for both clinicians and family members was very high (0.97) with similar but lower information coverage. The TIC shows that high information is especially concentrated in the middle of the latent construct with good coverage across different levels.
Overview of Data Analytic Strategy
Clinician Data Analysis:
Clinician data was analyzed by first examining group differences for question type using ANOVA. Then we performed correlation and linear regression analyses between co-variates related to clinician expertise and experience. These co-variates had the potential to modify clinician’s perceptions of false memories and forgetting and their respective functional impact. Average forgetting and false memory scores were then analyzed using an ANCOVA including both co-variates, “% of patients seen ” and “patient severity” as expertise and experience variables that correlated with outcomes of interest.
Rationale for inclusion of clinician expertise and experience variables as co-variates in clinician analysis:
Clinician expertise and experience may play a large role on a clinician’s reporting of both forgetting and false memories. Thus, we performed initial correlations between clinicians’ responses to questions regarding percent of patients seen with Alzheimer’s disease, mild cognitive impairment, and other dementias and memory disorders (question 3, clinician questionnaire), as well as the severity of AD patients seen (question 4, clinician questionnaire) with average forgetting and false memories scores, as well as with their perception of the impact of false memories and forgetting. These initial correlations, which showed a relationship between expertise and experience variables (“patients seen” and “patient severity”) and outcomes of interest (see results section), led us to perform an ANCOVA to evaluate the effects of expertise and experience on the perception of false memories and forgetting. The question posed to clinicians that allowed calculation of the patient experience variable was, “What percentage of your patients with Alzheimer’s disease show the following severity for each group: Very Mild-Mild, Moderate, and Severe.” Given our hypothesis that false memories and forgetting would both vary with patient severity, it is important to factor in each clinician’s experience with patients of various severities into our analyses.
Family Member Data Analysis:
Average forgetting and false memory scores for each clinical group were analyzed using an ANCOVA controlling for age and education. Correlations were performed between MMSE scores and both average forgetting and average false memory scores. Finally, prevalence of both false memories and forgetting was calculated using two methods of converting false memory and forgetting scores for individuals to dichotomous results indicating either the presence or absence of forgetting and false memories in an individual. Two methods were used because one was overly conservative and one overly liberal in estimations of forgetting and false memories. Prevalence was then compared between groups using a Chi-squared test.
Don’t Know Data Analysis:
A repeated-measures ANOVA was performed between the percentage of “Don’t Know” responses for clinicians for each question type (forgetting and false memories), and an analogous group by question type ANOVA was used to analyze the percentage of “Don’t Know” responses for family members.
Results
Clinician Data
Analysis of clinicians’ answers to the two functional questions, “How often do your patients forget information that is important to their function?” and “How often do your patients have distorted, confused, or false memories of information that is important to their function?” showed a significant effect of question type (forgetting vs. false memory) (F(1,220)=31.627; p<.001; η2 = .126), suggesting that forgetting (M=2.71, SE=.033) was perceived as more frequently impacting patients’ function compared to false memories (M=2.49, SE=.043).
The first measure, “patients seen,” was obtained from the question, “What percentage of patients with Alzheimer’s disease, mild cognitive impairment, and other dementias do you see?” A four-point scale (1=0%-10%, 2=10%-25%, 3=25%-50%, 4=>50%) was used. The second measure, “patient severity,” was obtained by computing a severity score from the answer to the question, “What percentage of your patients with Alzheimer’s disease show the following severity”. Clinicians were asked to report percentages for “Very mild – mild”, “Moderate”, and “Severe” severities. Severity score was computed as [(%Very mild – mild*1) + (%Moderate*2) + (%Severe*3)/300(Maximum score)].
Pearson bivariate correlation analyses were conducted between mean forgetting and false memories questions scores and expertise and experience variables computed above. “Patients seen” and “Patient severity” showed positive correlations with forgetting (r = .253, p = < .001; r = .224, p = < .001; respectively) and false memories average scores (r = .155, p = < .05; r = .183, p = < .01; respectively).
“Patients seen” and “Patients severity” also explained a significant proportion of variance of forgetting R2 = .096, F(2, 223) = 11.866, p < .001 and false memories R2 = .048, F(2, 222) = 5.621, p < .005, predicting clinicians’ perception of forgetting and false memories (β = .218, t(223) = 3.37, p < .001; β = .182, t(223) = 2.81, p < .005; respectively). “Patient severity” predicted false memories (β = .159, t(218) = 2.38, p < .05) and “Patients seen” was nearly significant (β = .123, t(222) = 1.85, p =.06). This analysis suggests that, similar to the analysis of the two functional questions, when taking expertise and experience into account, clinicians’ perceptions of the frequency of forgetting and false memories did not differ and that expertise and experience influences clinicians’ rating of the frequency of both false memories and forgetting.
When we included the expertise and experience variables (“patients seen” and “patient severity”) as covariates in the global questions analysis, the main effect of question Type (forgetting vs. false memory) was not significant, F(1, 218) = 7.87, p = .319, η2 = .005. Both “Patients seen” and “patient severity” showed a positive correlation with clinician’s perception of the impact of forgetting on function (r = .277, p < .001; r = .298, p < .001; respectively) and the impact of false memories on function (r = .210, p < .005; r = .189, p < .005; respectively). This result suggests that clinician expertise and experience modifies clinicians’ perceptions of the functional impact of forgetting and false memories and that when accounting for expertise and experience, clinicians rate forgetting and false memories as impacting function at the same frequency.
The mean scores for the 20 forgetting and 20 false memory questions were then analyzed including “Patients seen” and “Patient severity” as covariates. When performing an ANCOVA including “Patients seen” alone as a co-variate, the main effect of question type forgetting (M = 2.35; SE = .026) vs. false memory (M = 2.19; SE = .031) was not significant F(1, 222) =.723, p = .40, η2 = .003. When performing an ANCOVA including “Patient severity” alone as a covariate, there was a main effect of question type, forgetting vs. false memory, F(1, 222) =6.805, p = 0.01, η2 = .03. Finally, while performing an ANCOVA using both co-variates, the main effect of question type forgetting vs. false memory was not significant F(1, 222) =.662, p = .417, η2 = .003, although it was significant using an ANOVA not controlling for “Patients seen” and “Patient severity,” F(1, 224) = 53.964, p <.001, η2 = .194.
Family Member Data
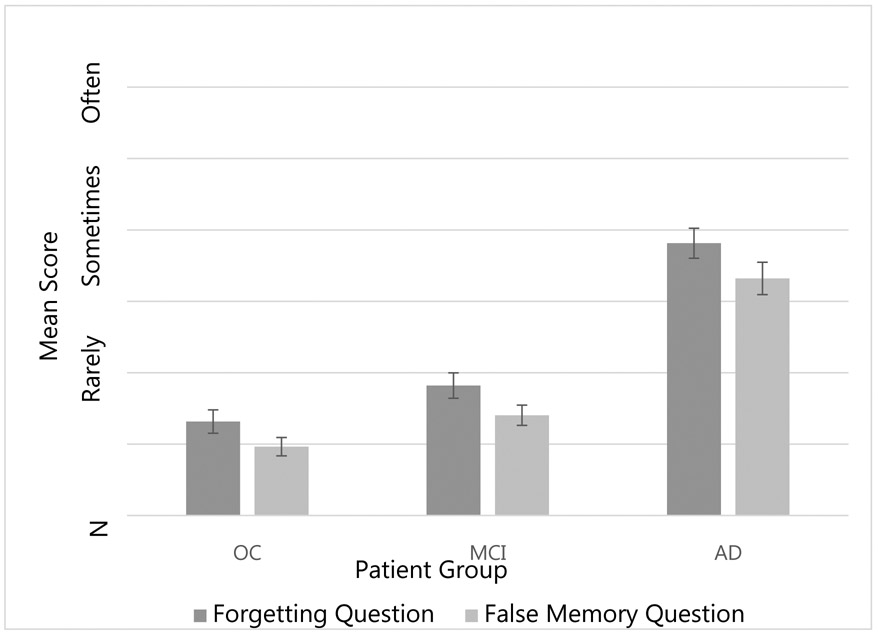
Mean scores for the forgetting and false memory questions for each of the family member groups can be seen in Figure 2. Mean scores were analyzed using a 3 (group: OC, MCI, AD) X 2 (question type: forgetting, false memory) ANCOVA including age and education as covariates. One AD subject and one MCI subject did not have age and education recorded and were excluded from these analyses. A main effect of group was observed (F(2, 143) = 34.67, p < .001, η2 = .326). When comparing the estimated marginal means, family members of OCs reported less forgetting and fewer false memories combined (M = .66; SE = .087) compared to patients with AD (M = 1.69; SE = .093; p < 0.001). Patients with AD (M = 1.69; SE = .093; p < 0.001) also had more false memories and forgetting compared to patients with MCI (M = .82; SE = .095; p < 0.001). Neither a main effect of question type or group X question type interaction were observed (F < 1, p > .1).
Figure 2.
Mean Memory Question scores by patient group for family member data
We also analyzed Mean scores using a 3 (group: OC, MCI, AD) X 2 (question type: forgetting, false memory) ANOVA without including age and education as covariates. A main effect of group was observed (F(2, 147) = 52.04, p < .001, η2 = .415). When comparing the estimated marginal means, AD patients had greater forgetting and false memory scores (M =1.8, SE = .091) compared to the MCI group (M=0.87; SE=.096 p <.0001) and compared to OCs (M= 0.57, SE = 0.08 ; p<.0001). A main effect of question type was also observed, (F(2, 147) = 68.832, p < .001, η2 = .319), (Mean forgetting=1.19, SE=.056; Mean false memories =0.97, SE= .05). A group X question type interaction was not observed (F < 1, p > .1).
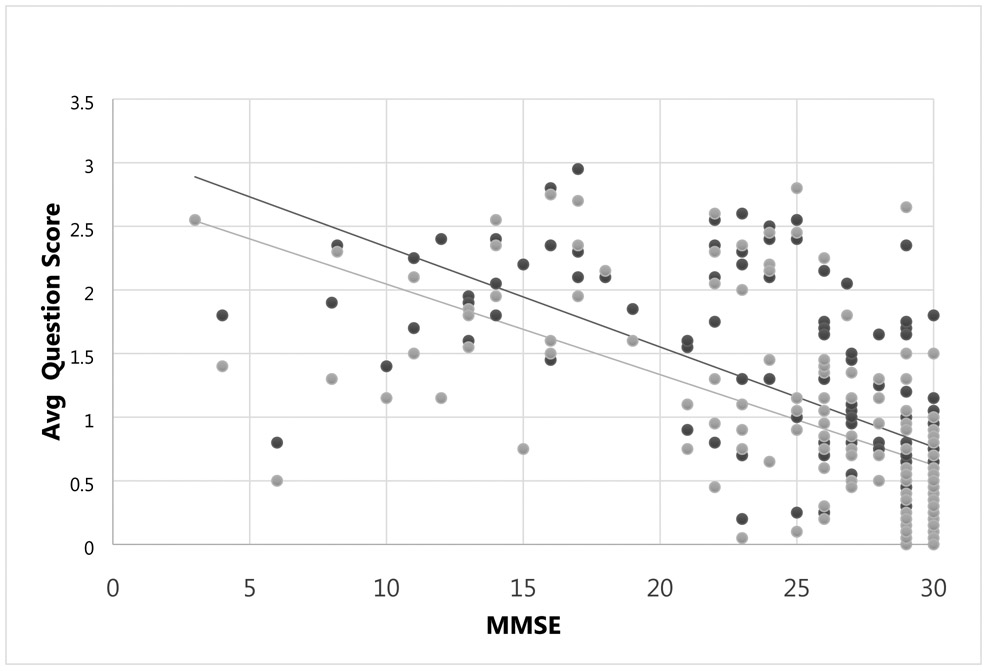
Finally, Pearson bivariate partial correlations between MMSE scores and each average question type score, correcting for age and education yielded correlations between MMSE score and both average forgetting (r = −.456, p < .001) and false memory (r = −.441, p < .001), see Figure 3. These results indicated that as MMSE scores decreased, both forgetting and false memories increased.
Figure 3.
Scatterplot of correlation between MMSE and average forgetting score (dark grey) and average false memory score (light grey) for family member data. 0=Never, 1=Rarely, 2=Sometimes, 3=Often
Prevalence
Prevalence of false memories and forgetting were calculated for OC, MCI, and AD subjects using two methods as described below. The first, more conservative method, used average questionnaire responses 3 (Often) and 2 (Sometimes) translated into the binary value 1, and responses 1 (Rarely) and 0 (Never) were translated into the binary value 0. Having assigned every subject to either a 1 (presence of false memories/forgetting) or 0 (absence of false memories/forgetting), the prevalence was calculated by dividing the number of subjects that experienced false memories/forgetting (binary score of 1) by the total number of subjects.
Using this initial method, there was a higher prevalence of forgetting for the AD group compared to MCI (χ2 = 18.095; p < .001) and OC (χ2 = 38.484; p < .001), and a marginally significant trend for MCI compared to OC (χ2 = 3.653; p = .056). A higher prevalence of false memories was found for AD compared to MCI (χ2 = 22.874; p < .001) and OC (χ2 = 27.264; p < .001); no difference was found between MCI and OC (χ2 = .002; p = .966). No differences were found between forgetting and false memories prevalence within groups for AD (χ2 = 2.724; p = .101) or OC (χ2 = .435; p = .510), but the MCI group showed more forgetting than false memories (χ2 = 5.388; p < .020) (Table 1).
Given that the rate of forgetting in the AD group was 69% and thus lower than would be expected clinically, it is likely that this conservative method may underestimate the true rates of false memory and forgetting as rare answers were counted as representing the absence of false memories and forgetting.
Thus, we performed a secondary analysis of prevalence using more liberal criteria for the presence of forgetting and false memories where we calculated the binary value of presence versus absence of false memories and forgetting using the answers 3 (often), 2 (sometimes), and 1 (rarely) as criteria for presence of false memories and forgetting, and only the answer choice 0 (never) as consistent with absence of false memories or forgetting. Using these methods, we re-calculated the prevalence of forgetting and false memories between the three groups (see Table 1).
Using the second, more liberal method, there was a higher prevalence of forgetting for the AD group compared to MCI (χ2 = 5.74; p < .05) and OC (χ2 = 30.57; p < .001), and MCI compared to OC (χ2 = 11.93; p < .001). A higher prevalence of false memories was found for AD compared to MCI (χ2 = 8.98; p <.005) and OC (χ2 = 34.52; p < .001); MCI and OC (χ2 = 9.08; p < .005). No differences were found between forgetting and false memories prevalence within groups using this method AD (χ2 = 1.37; p = .24), MCI (χ2 = 2.71; p = 0.10), and OC (χ2 = 1.78; p = 0.18) (Table 1). See Table 1 for prevalence using both methods for each group.
Don’t Know Response Analysis
Finally, in order to investigate whether false memories may be under-recognized by family members and clinicians, we analyzed the mean percentage of “Don’t Know” responses for each group (all family member groups and clinicians) by question type. “Don’t Know” is different from missed items because it is a specific choice that participants could choose (see Appendix B, family member questionnaire). This “Don’t Know” response analysis did not include any questions left unanswered so as not to confound these responses with inadvertently skipped answers.
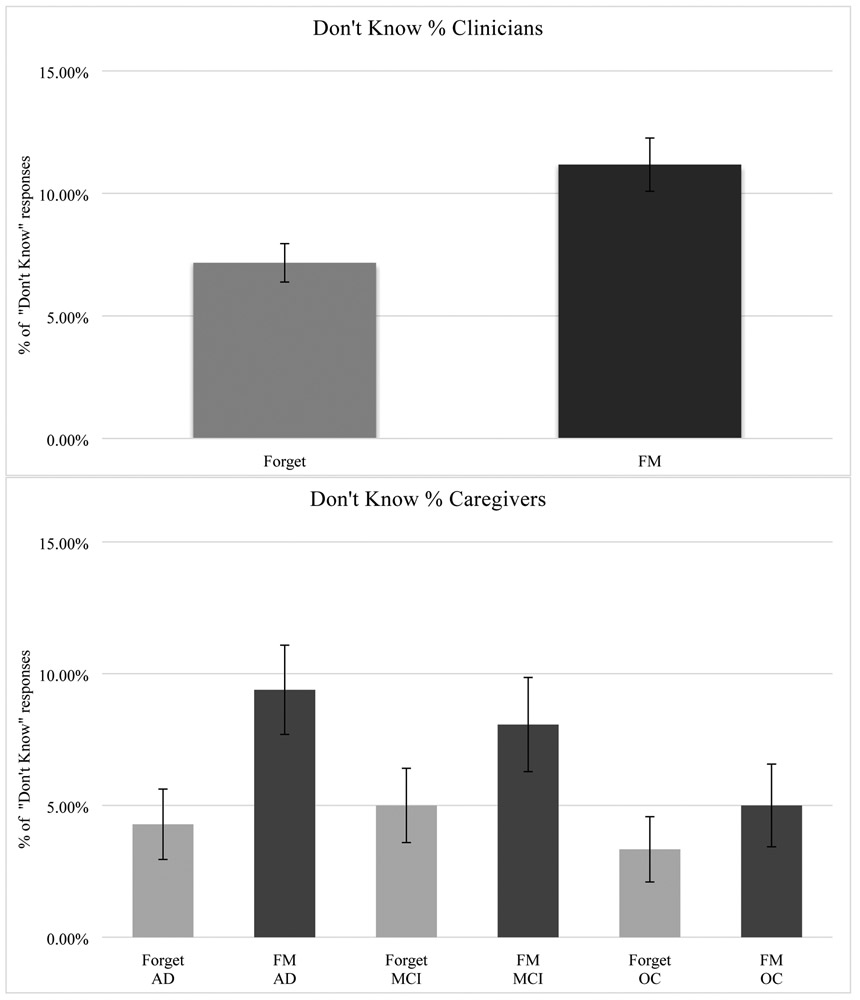
Clinicians
A repeated-measures ANOVA was performed between the percentage of Don’t Know responses for forgetting and false memory questions, which revealed a main effect of question type (F(1, 225)=37.402, p<.001, η2 = .142), such that the mean percentage of Don’t Know responses for false memories questions ( M=11.2%, SE= 0.011) was significantly higher than the mean percentage of Don’t Know responses for forgetting questions (M=7.2%, SE=0.008). (See Figure 4A).
Figure 4.
Mean difference between don’t know responses for forgetting and false memories questions (A) given by clinicians and (B) in the AD, OC and MCI caregiver groups.
Family members
A 3 (group: OC, MCI, AD) X 2 (question type: forgetting, false memories) repeated-measures ANOVA was used to analyze the mean percentage of Don’t Know responses for family members. A main effect of question type was observed (F(1, 147)=42.606, p<.001, η2 = .225), such that the mean percentage of Don’t Know responses for false memory questions (M=7.5%, SE= 0.011) was significantly higher than the mean percentage of Don’t Know responses for forgetting questions (M=4.2%, SE=0.008).
A group X question type interaction was observed (F(2, 147)=4.169, p<.05, η2 = .054). The mean percentage of Don’t Know responses for family members of AD patients for the false memories questions (M=9.4%, SE=0.017) was significantly higher than the mean percentage of Don’t Know responses for the forgetting questions (M=4.3%, SE=0.013; p<0.001), as they were for the MCI patients: false memory questions (M=8.1%, SE=0.018), forgetting questions (M=5.0%, SE=0.014; p< 0.05). No significant difference was observed for the Don’t Know responses in the OC group between false memories (M=5.0%, SE=0.016) and forgetting responses (M=3.3%, SE=0.012; p=0.310). No main effect of group type was observed for the Don’t Know responses (F(2, 147)=1.088, p=.339, η2 = .015). (See Figure 4B).
Discussion
This is the first study to our knowledge that measured clinician and family member perceptions of false memories and their frequency in the daily life of memory patients. To test our hypotheses that false memories were occurring as often as forgetting, we developed a questionnaire given the lack of gold standard or other validated instrument for the measurement of false memories in daily life. Contrary to our hypothesis, we found that patients with AD, MCI, and OCs all experience false memories less frequently than they do forgetting, as reported by both family members and clinicians. However, when correcting for the number of dementia patients seen and their severity, there was no difference in the average forgetting and average false memory score reported by the clinicians. Furthermore, our analysis of “Don’t Know” responses suggests that false memories may be under-reported by both clinicians and family members. Lastly, even taking our primary results at face value, prevalence calculations using family member data found that false memories in the AD and MCI groups were quite high—almost as high as forgetting. False memories were also present to some degree in OCs, consistent with prior findings (Daniel L. Schacter et al., 1999). To our knowledge, this is the first report of the estimated prevalence of false memories in the daily life of older adults as well as in patients with MCI and AD.
Using both the clinician and family member data, we found that the degree of false memories among MCI and AD patients correlated strongly with the severity of their cognitive impairments. Specifically, MMSE scores correlated with family member average forgetting and false memory scores and, among clinicians, measures of clinical severity correlated with average forgetting and false memory scores. Given that MMSE scores have been shown to correlate with function in daily life (Tekin, Fairbanks, O'Connor, Rosenberg, & Cummings, 2001), our finding that false memories correlate with MMSE has potential bearing on the impact of false memories in daily life. Our results also indicated that clinicians who see more AD patients and/or a higher percentage of more impaired patients report a greater impact of forgetting and false memories on the daily lives of their patients. In fact, when accounting for clinicians’ expertise and experience with AD patients, clinicians tend to think forgetting and false memories impact patients’ lives at equivalent rates. Taken together, the clinician results also showed that clinicians’ expertise and experience plays a crucial role in their perception of false memories. Future studies could directly compare false memories questionnaire results to detailed measures of activities of daily living, in order to further investigate the impact of false memories in the daily lives of patients with AD and MCI.
Correcting for age and education between OC and AD groups can lead to inherent bias in some circumstances (Miller & Chapman, 2001) therefore we performed an ANOVA comparing average forgetting and false memory scores between patient groups not controlling for age and education. ANOVA results of average forgetting and false memories scores between patient groups and question type, not controlling for age and education, there is a main effect of question type and forgetting scores are greater than false memory scores. Of note, both forgetting and false memories have been reported to be highly associated with healthy aging as well as Alzheimer’s disease (Balota, Watson, Duchek, & Ferraro, 1999; Norman & Schacter, 1997; Tun, Wingfield, Rosen, & Blanchard, 1998). Demographics for the three cohorts (Table 1) show that the AD group was older and less educated than the OC group and furthermore, that the MCI group was also less educated than the OC group, but more educated than the AD group. These findings are in keeping with previous literature that older and less educated individuals are at greater risk of AD (Alzheimer's Association Facts and Figures, 2019). Furthermore, age is independently associated with increases in false memories (Norman & Schacter, 1997). Using an analysis which does not account for age and its potential impact on forgetting and false memories introduces potential confounding as it is difficult to determine if our dependent variable of interest, incidences of forgetting and false memories, are in fact elevated in older cohorts due to normal aging or due to the increased incidence of MCI and AD that also occurs with aging and may independently affect rates of both forgetting and false memories. Since our cohorts differed in age and education, we felt it most appropriate to use an ANCOVA accounting for age and educational differences between cohorts when analyzing group differences in forgetting and false memory scores.
Therefore, although we report an additional analysis using ANOVA without the effect of age and education included, we believe that it is most appropriate to interpret and discuss data related to our initial ANCOVA analysis using age and education and co-variates. Therefore, the average forgetting and false memory scores may be interpreted as follows: forgetting and false memory scores are either equal (ANCOVA) or forgetting scores are somewhat larger than false memory scores (ANOVA) (1.19 vs. 0.97). In either case, although the difference in the ANOVA is significant, the numerical values are similar, suggesting that false memories are being perceived as occurring nearly as frequently as forgetting. Thus, researchers, pharmaceutical companies designing clinical trials, and clinicians should consider the existence of false memories as an additional clinical symptom that occurs frequently in patients with Alzheimer’s disease.
There are no currently used guidelines, gold standards, or generally accepted questionnaires to help clinicians detect false memories. This lack of tools to measure false memories in current clinical practice may lead less experienced clinicians to underestimate or ignore false memories during assessment. We hope the questionnaire developed here provides a starting point to measure false memories in AD and MCI. Our validity analyses indicate that both the false memory and forgetting parts of our questionnaire were related to the latent construct of each question type, given that the information response curve for each question type was high, with good coverage across the range of abilities within the patient population, as shown in Figure 1.
It should be noted that this is a questionnaire-based study and thus subject to reporting limitations of a second-party observer. It is therefore possible that the true frequency and prevalence of false memories among patients with MCI and AD is being under recognized as there is currently no gold standard method of assessing the true frequency of false memories in daily life. Future ecological studies aimed at investigating the true incidence of false memories in daily life will be useful in conjunction with our newly developed questionnaire.
We used two methods to calculate the prevalence of false memories and forgetting in our population. Using the more liberal calculation method for prevalence, as expected, we found high rates of both forgetting and false memories, with the AD group approaching 96% forgetting and almost as much (90%) false memory. The OC group, showed forgetting at nearly 46%, and false memories occurring in approximately one-third. These high rates are likely attributable to the fact that even healthy older adults experience many instances of forgetting and false memories. Using the conservative calculation method resulted in comparatively lower prevalence of both forgetting and false memories across groups compared to the liberal method. While conservative method for the OC group showed lower baseline rates of forgetting (10.53%) and false memories (7.02%), the AD group approached only 69.39% forgetting, which is below the rate of forgetting one would expect based on clinical observation of AD patients. Thus, each method for calculating prevalence may be over- or under-estimating the true prevalence, and the conservative method is potentially advantageous in that likely reflects more of the pathologic instances of forgetting and false memories and less of the baseline rate of each behavior that can occur with normal aging and the liberal method is potentially useful as well as it tends to reflect the clinically seen rates of forgetting in the AD group, and thus may be a more accurate representation of false memory prevalence in the AD group.
The Don’t Know analysis revealed that both clinicians and family members of AD and MCI patients made more Don’t Know responses for false memory questions compared to forgetting questions. Clinicians and family members are thus less certain about how often their patients and loved ones are having false memories compared to how certain they are about how often they are forgetting, given that Don’t Know responses were higher for false memory questions than for forgetting questions for both groups. This result suggests that false memories are likely under-recognized and under-reported.
In regards to the relative impact of forgetting versus false memories on function when accounting for our expertise and experience measures (‘patients seen’ and ‘patient severity’ in clinician data, respectively), perceived functional impact of false memories and forgetting was indistinguishable. False memories may have an equal or greater functional impact compared to forgetting in AD and MCI, but as shown in the “Don’t Know” analysis, due to under-reporting our results could be underestimating the impact of false memories on daily life. Even if false memories have less impact on function than forgetting, we would argue strongly that does not mean they should be ignored. With 5.8 million Americans with Alzheimer’s disease being attended to by more than 16 million caregivers over 18.5 billion hours (association, 2019) even a small increase in our understanding of these patients’ impairments could make a large impact on people’s lives. Thus, the development of questionnaires to measure False memories in daily life is important.
The false memories questionnaire developed, similar to other instruments commonly used in the AD population, is a caregiver-reported instrument. Although caregiver-reported instruments may have drawbacks, such as variability related to how well the caregiver knows the patients, we believe that it is better than a self-reported questionnaire for the following reasons. Previous studies have shown an absence of relationship between subjective memory complaints and objective impairment in patients with AD, likely due to poor insight (Jungwirth et al., 2004). These findings are also supported by the results of other studies of patients with dementia that show a higher correlation between clinical outcomes and caregiver-reported quality of life (QOL) compared to self-reported QOL (Jungwirth et al., 2004; Lenehan, Klekociuk, & Summers, 2012). It is likely that self-report measures of false memories would suffer from the same biases due to lack of insight when used for self-report. However, it is possible that those with MCI, given their earlier stage of disease, may have retained awareness and may be able to self-report about episodes of false memories. This is an area of possible exploration for future studies.
This study measured clinicians’ impression of patient function but not family members’ impressions of function. We plan to examine family members’ impression of patient function in future studies.
This study did not explicitly address different types of false memories: events that occurred in altered form versus events that never occurred. However, the questionnaire covers topics related to misremembering and memory distortions in questions 8, 12, and 14 (see Appendix for complete questionnaire) while other questions are related to memory for events that did not happen.
Furthermore, as this study was questionnaire-based, it did not address whether patients truly had false memories; future studies could perhaps use continuously recording cameras to track an individual’s actual actions and measure their reported true memories, false memories, and forgetting against this objective standard. In addition, we did not measure family member exposure to or time with patients—a relevant variable we plan to collect in future work as it could influence family members’ perceptions of false memories.
In summary, knowledge of false memories in AD and MCI groups may be clinically important. Others have previously noted that memory distortions among AD patients result in behavioral disturbances that may impair ability to live independently (Borson & Raskind, 1997). It has also been suggested that the degree of measured false memories is a more specific indicator of AD pathology than memory performance alone (Hildebrandt et al., 2009a). We have shown that although false memories are less prevalent than forgetting in AD and MCI patients, they are nearly as common as forgetting. The false memories questionnaire created as part of this study may be helpful as a clinical and research tool to measure false memories in daily life.
Acknowledgements:
This work was supported by the National Institutes of Health (grant number P30-AG013846, A.B.) and also from the United States Department of Veterans Affairs, Merit Review Award (grant number, CX000736, A.B.)
Appendix A. False Memories Questionnaire for Clinicians
Understanding Clinician Impressions of Memory Impairments: A Survey Study
Thank you in advance for your interest in filling out this survey. The purpose of this survey is to obtain your impression of different types of memory deficits that patients with Alzheimer’s disease and other dementias experience in day-to-day life. Questions in this survey will ask you about different memory problems your patients or their caregivers may report having and frequency of their occurrence. You will be asked to answer each question as best as possible. This survey is voluntary and should only take about 10 minutes of your time. All responses will be anonymous. Thank you for your participation in this survey. If you have any questions, you may contact our laboratory at 857-364-4554 or e-mail us at ctcnbrainlab@gmail.com.
- What best describes your medical specialty or profession? (check the box that is the most appropriate, or fill in the blank below)
- Geriatrician
- Internal Medicine / Primary Care Neurologist
- Neuropsychologist
- Nurse
- Nurse Practitioner
- Physician Assistant
- Psychiatrist
- Psychologist
- Social Worker
- Other (please list): _______________
How many years have you been in practice? _____years
- What percentage of patients with Alzheimer’s disease, mild cognitive impairment, and other dementias and memory disorders do you see?
- >50%
- 25-50%
- 10-25%
- 0-10%
How many patients with Alzheimer’s disease do you currently follow?
- What percentage of your patients with Alzheimer’s disease show the following severity (please fill in the blanks with the appropriate percentage)?
- Very Mild - Mild ______
- Moderate ______
- Severe ______
Instructions for attached questionnaire
For the following questionnaire, you will be asked to provide an impression of memory problems your patients may experience for everyday activities. You are asked to provide your impressions for all the patients you have seen, not one specific patient. For each question, please check off the appropriate box if you have observed that specific memory problem with a patient yourself, if your patients have reported any of the following memory problems, or their families or caregivers have reported any of these memory problems. Please try to answer every question. If you do not know the answer to the question, please check of the box “Do not know.”
- How often do your patients forget information that is important for their function?
- Often
- Sometimes
- Rarely
- Never
- Do not know
- How often do your patients have distorted, confused, or false memories for information that is important for their function?
- Often
- Sometimes
- Rarely
- Never
- Do not know
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Appendix B. False Memories Questionnaire for Family Members
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Footnotes
Potential Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Acevedo A, & Loewenstein DA (2007). Nonpharmacological cognitive interventions in aging and dementia. J Geriatr Psychiatry Neurol, 20(4), 239–249. doi: 10.1177/0891988707308808 [DOI] [PubMed] [Google Scholar]
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, … Phelps CH (2011). The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement, 7(3), 270–279. doi: 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- association, A. s. (2019). Alzheimer’s Disease Facts and Figures. Retrieved from Alzheimer’s Dementia:
- Balota DA, Watson JM, Duchek JM, & Ferraro FR (1999). Cross-modal semantic and homograph priming in healthy young, healthy old, and in Alzheimer's disease individuals. J Int Neuropsychol Soc, 5(7), 626–640. [DOI] [PubMed] [Google Scholar]
- Borson S, & Raskind MA (1997). Clinical features and pharmacologic treatment of behavioral symptoms of Alzheimer's disease. Neurology, 48(5 Suppl 6), S17–24. [DOI] [PubMed] [Google Scholar]
- Budson AE, Daffner KR, Desikan R, & Schacter DL (2000). When false recognition is unopposed by true recognition: gist-based memory distortion in Alzheimer's disease. Neuropsychology, 14(2), 277–287. [DOI] [PubMed] [Google Scholar]
- Budson AE, Wolk DA, Chong H, & Waring JD (2006). Episodic memory in Alzheimer's disease: separating response bias from discrimination. Neuropsychologia, 44(12), 2222–2232. doi: 10.1016/j.neuropsychologia.2006.05.024 [DOI] [PubMed] [Google Scholar]
- Cotel SC, Gallo DA, & Seamon JG (2008). Evidence that nonconscious processes are sufficient to produce false memories. Conscious Cogn, 17(1), 210–218. doi: 10.1016/j.concog.2007.01.009 [DOI] [PubMed] [Google Scholar]
- Deason RG, Nadkarni NA, Tat MJ, Flannery S, Frustace B, Ally BA, & Budson AE (2017). The use of metacognitive strategies to decrease false memories in source monitoring in patients with mild cognitive impairment. Cortex, 91, 287–296. doi: 10.1016/j.cortex.2017.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devitt AL, & Schacter DL (2016). False memories with age: Neural and cognitive underpinnings. Neuropsychologia, 91, 346–359. doi: 10.1016/j.neuropsychologia.2016.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 12(3), 189–198. [DOI] [PubMed] [Google Scholar]
- Hildebrandt H, Haldenwanger A, & Eling P (2009a). False recognition correlates with amyloid-beta (1–42) but not with total tau in cerebrospinal fluid of patients with dementia and mild cognitive impairment. J Alzheimers Dis, 16(1), 157–165. doi: 10.3233/JAD-2009-0931 [DOI] [PubMed] [Google Scholar]
- Hildebrandt H, Haldenwanger A, & Eling P (2009b). False recognition helps to distinguish patients with Alzheimer's disease and amnestic MCI from patients with other kinds of dementia. Dement Geriatr Cogn Disord, 28(2), 159–167. doi: 10.1159/000235643 [DOI] [PubMed] [Google Scholar]
- Jungwirth S, Fischer P, Weissgram S, Kirchmeyr W, Bauer P, & Tragl KH (2004). Subjective memory complaints and objective memory impairment in the Vienna-Transdanube aging community. J Am Geriatr Soc, 52(2), 263–268. [DOI] [PubMed] [Google Scholar]
- Koutstaal W, Verfaellie M, & Schacter DL (2001). Recognizing identical versus similar categorically related common objects: further evidence for degraded gist representations in amnesia. Neuropsychology, 15(2), 268–289. [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Lenehan ME, Klekociuk SZ, & Summers MJ (2012). Absence of a relationship between subjective memory complaint and objective memory impairment in mild cognitive impairment (MCI): is it time to abandon subjective memory complaint as an MCI diagnostic criterion? Int Psychogeriatr, 24(9), 1505–1514. doi: 10.1017/S1041610212000695 [DOI] [PubMed] [Google Scholar]
- Malone C, Deason RG, Palumbo R, Heyworth N, Tat M, & Budson AE (2018). False memories in patients with mild cognitive impairment and mild Alzheimer's disease dementia: Can cognitive strategies help? J Clin Exp Neuropsychol, 1–15. doi: 10.1080/13803395.2018.1513453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr., Kawas CH, … Phelps CH (2011). The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement, 7(3), 263–269. doi: 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GA, & Chapman JP (2001). Misunderstanding analysis of covariance. J Abnorm Psychol, 110(1), 40–48. doi: 10.1037//0021-843x.110.1.40 [DOI] [PubMed] [Google Scholar]
- Norman KA, & Schacter DL (1997). False recognition in younger and older adults: exploring the characteristics of illusory memories. Mem Cognit, 25(6), 838–848. [DOI] [PubMed] [Google Scholar]
- Schacter DL, Israel L, & Racine C (1999). Suppressing false recognition in younger and older adults: The distinctiveness heuristic. Journal of Memory and Language, 40(1), 1–24. doi: 10.1006/jmla.1998.2611 [DOI] [Google Scholar]
- Schacter DL, Verfaellie M, Anes MD, & Racine C (1998). When true recognition suppresses false recognition: evidence from amnesic patients. Journal Of Cognitive Neuroscience, 10(6), 668–679. [DOI] [PubMed] [Google Scholar]
- Schmid NS, Taylor KI, Foldi NS, Berres M, & Monsch AU (2013). Neuropsychological signs of Alzheimer's disease 8 years prior to diagnosis. J Alzheimers Dis, 34(2), 537–546. doi: 10.3233/JAD-121234 [DOI] [PubMed] [Google Scholar]
- Snodgrass JG, & Corwin J (1988). Pragmatics of measuring recognition memory: applications to dementia and amnesia. J Exp Psychol Gen, 117(1), 34–50. [DOI] [PubMed] [Google Scholar]
- Tekin S, Fairbanks LA, O'Connor S, Rosenberg S, & Cummings JL (2001). Activities of daily living in Alzheimer's disease: neuropsychiatric, cognitive, and medical illness influences. Am J Geriatr Psychiatry, 9(1), 81–86. [PubMed] [Google Scholar]
- Tun PA, Wingfield A, Rosen MJ, & Blanchard L (1998). Response latencies for false memories: gist-based processes in normal aging. Psychol Aging, 13(2), 230–241. [DOI] [PubMed] [Google Scholar]