Since first cases of pneumonia of unknown etiology were reported on December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a global health issue and its related disease (COVID-19) was finally declared a pandemic by World Health Organization on March 2020 [1]. To date, there is no evidence that consistently supports any treatment for COVID-19 patients, so identifying new therapeutic options seems crucial in the management of this disease. Imatinib is a tyrosine kinase inhibitor with a well-known anti-tumor activity against several cancers including chronic myeloid leukemia and gastrointestinal stromal tumors. According to previously published data, this drug has also shown antiviral, immunomodulatory and endothelium-protective properties which may be potentially helpful in COVID-19. In fact, imatinib has been pointed out as an unexplored treatment for SARS-CoV-2 infection [2]. We report the case of a patient with COVID-19 pneumonia who received imatinib due to clinical deterioration despite dual therapy with hydroxychloroquine (HCQ) and lopinavir/ritonavir (LPV/r).
On March 12, a 38-year-old woman was admitted to our department with a 6-day history of fever up to 39 °C, arthralgia, malaise and cough. Her blood pressure, heart rate and respiratory rate were all normal. Her temperature was 37.1 °C and oxygen saturation was 96% while she was breathing ambient air. Physical examination only revealed minimal wheezing on chest auscultation. Laboratory results showed a mild elevation of C-reactive protein (CRP) and lactate dehydrogenase (LDH) levels, and a normal lymphocyte count (Table 1 ). Chest X-ray confirmed bilateral pneumonia. Polymerase chain reaction test for SARS-CoV-2 in nasopharyngeal swab was positive, so treatment with HCQ and LPV/r, as well as empiric therapy with ceftriaxone, was initiated in accordance with hospital protocol.
Table 1.
- Laboratory results.
| Variable | Day 6 of symptoms | Day 10 of symptoms | Day 13 of symptoms (day 2 of imatinib) |
Day 14 of symptoms (day 3 of imatinib) |
Day 16 of symptoms (day 5 of imatinib and discharge) |
20 days after discharge |
|---|---|---|---|---|---|---|
| CRP, mg/dL | 4.79⁎ | 21.00⁎ | – | 25.04⁎ | 7.52⁎ | 0.57⁎ |
| Procalcitonin, ng/mL | – | 0.1 | 0.09 | 0.06 | 0.05 | 0.01 |
| LDH, IU/L | 338⁎ | 532⁎ | 318⁎ | 306⁎ | 326⁎ | 222 |
| Venous lactate, mmol/L | 1.0 | 3.2⁎ | 2.7⁎ | 2.5⁎ | 1.6⁎ | 1.1 |
| White-cell count, × 109/L | 7.09 | 8.48 | 10.19 | 9.67 | 7.61 | 10.25 |
| Neutrophil count, × 109/L | 5.44 | 6.76 | 8.29⁎ | 7.92⁎ | 5.56 | 6.07 |
| Lymphocyte count, × 109/L | 1.17 | 1.31 | 1.09 | 0.84† | 1.35 | 3.14 |
| D-dimer, ng/mL | – | 580⁎ | 760⁎ | 1129⁎ | – | 449 |
CRP = C-reactive protein; LDH = Lactate dehydrogenase.
The value was above the reference range.
The value was below the reference range.
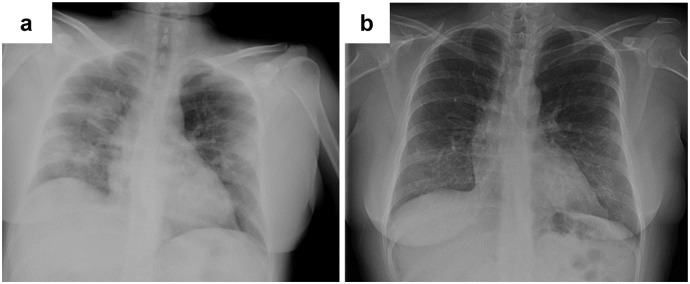
The patient reported initial improvement; however, on March 15 (day 9 of symptoms) fever recurred and supplemental oxygen by nasal cannula at a rate of 3 l per minute was required. Furthermore, both an increase in CRP levels (Table 1) and radiological deterioration were observed (Fig. 1 , a). These clinical changes suggested that the disease was progressing to an early phase of a hyperinflammatory state despite treatment with HCQ and LPV/r; thus, after assessing the safety profile of imatinib [3] and reviewing previous publications about its antiviral and immunomodulatory properties, we considered that this drug may have potentially beneficial effects in such clinical scenario. Hence, informed consent was obtained and imatinib (400 mg once daily) was added on day 12 of symptoms, while ceftriaxone was interrupted since there was no evidence of concurrent bacterial infection. Three days later the fever disappeared, supplemental oxygen was discontinued and radiological stability of pulmonary opacities was confirmed. Moreover, improvement in laboratory parameters was observed on day 5 of imatinib so it was stopped and the patient was subsequently discharged on day 16 of symptoms after also completing 9 days of HCQ and LPV/r. She remained asymptomatic on April 11 (20 days after discharge), her blood tests were then normal (Table 1) and pulmonary opacities had almost disappeared (Fig. 1, b).
Fig. 1.
a Portable chest X-ray showing radiological deterioration with bilateral patchy opacities (March 17, day 11 of symptoms). b Marked improvement of opacities in posteroanterior chest radiograph (April 11, day 20 after discharge and day 36 after the onset of symptoms).
Although developed targeting the oncogenic fusion protein BCR-ABL, imatinib is able to inhibit other tyrosine kinases such as c-KIT, platelet-derived growth factor receptor and Abelson kinases (ABL) type 1 and 2 [4]; therefore, it has been postulated that the biological activity of this drug is not restricted to anticancer effects. In this regard, immunomodulatory properties of imatinib have been reported. Murine models of sepsis and acute lung injury have suggested a protective role of this drug by reducing pulmonary edema, preventing histological damage and improving endothelial barrier dysfunction, probably through attenuation of proinflammatory cytokine release including interleukin-6 and tumor necrosis factor-alpha [4,5]. These effects over inflammatory activation might be mediated by the inhibition of transcription factor NF-κB according to previous evidence from both animal models and studies with human cells [[4], [5], [6]]. Since NF-κB represents a key element in several inflammatory pathways [7], imatinib could be helpful to modulate host immune response against SARS-CoV-2. This is particularly noteworthy given that hyperinflammation plays a central role in severe COVID-19 [3,8].
In addition, imatinib has shown in vitro antiviral activity against severe acute respiratory syndrome and Middle East respiratory syndrome coronaviruses [9], which are phylogenetically related to SARS-CoV-2 [10]. In this sense, ABL2 appears to be involved in the virus-cell fusion process, so its blockage could modulate the entry of coronaviruses into host cells [9]. These data also suggest that imatinib might be useful in early stages of SARS-CoV-2 infection, although further research is needed to ascertain the antiviral properties of this drug in COVID-19.
To our knowledge, this is the first reported case of SARS-CoV-2 infection successfully treated with imatinib. However, elucidating the relevance of any therapeutic intervention from a single case report is always controversial since clinical outcomes may be influenced by some confounding factors such as the concomitant use of other therapies. Nevertheless, taking into account all the above mentioned data, we believe that imatinib should be considered a potential treatment for COVID-19.
Funding
No external funding was received.
Declaration of Competing Interest
David Bernal-Bello is the principal investigator of a non-sponsored randomized trial assessing the therapeutic role of lopinavir/ritonavir, imatinib, and baricitinib in COVID-19 patients. The rest of the authors are sub-investigators in this project. All authors declare no other competing interests.
References
- 1.World Health Organization (WHO) Novel Coronavirus (2019-nCoV) Situation Report - 51 11 March 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- 2.Gasmi A., Noor S., Tippairote T., Dadar M., Menzel A., Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernal-Bello D., Jaenes-Barrios B., Morales-Ortega A., Ruiz-Giardin J.M., García-Bermúdez V., Frutos-Pérez B., Farfán-Sedano A.I., de Ancos-Aracil C., Bermejo F., García-Gil M., Zapatero-Gaviria A., San Martín-López J.V. Imatinib might constitute a treatment option for lung involvement in COVID-19. Autoimmun. Rev. 2020;19 doi: 10.1016/j.autrev.2020.102565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rizzo A.N., Sammani S., Esquinca A.E., Jacobson J.R., Garcia J.G., Letsiou E., Dudek S.M. Imatinib attenuates inflammation and vascular leak in a clinically relevant two-hit model of acute lung injury. Am. J. Physiol. Cell. Mol. Physiol. 2015;309:1294–1304. doi: 10.1152/ajplung.00031.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stephens R.S., Johnston L., Servinsky L., Kim B.S., Damarla M. The tyrosine kinase inhibitor imatinib prevents lung injury and death after intravenous LPS in mice. Physiol. Rep. 2015;3 doi: 10.14814/phy2.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciarcia R., Vitiello M.T., Galdiero M., Pacilio C.P., Iovane V., d’Angelo D., Pagnini D., Caparrotti G., Conti D., Tomei V., Florio S., Giordano A. Imatinib treatment inhibit IL-6, IL-8, NFKB and AP-1 production and modulate intracellular calcium in CML patients. J. Cell. Physiol. 2012;227:2798–2803. doi: 10.1002/jcp.23029. [DOI] [PubMed] [Google Scholar]
- 7.Ingraham N.E., Lotfi-Emran S., Thielen B.K., Techar K., Morris R.S., Holtan S.G., Dudley R.A., Tignanelli C.J. Immunomodulation in COVID-19. Lancet Respir. Med. 2020;8:544–546. doi: 10.1016/S2213-2600(20)30226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Felsenstein S., Herbert J.A., McNamara P.S., Hedrich C.M. COVID-19: immunology and treatment options. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman C.M., Sisk J.M., Mingo R.M., Nelson E.A., White J.M., Frieman M.B. Abelson kinase inhibitors are potent inhibitors of severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus fusion. J. Virol. 2016;90:8924–8933. doi: 10.1128/JVI.01429-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., Bi Y., Ma X., Zhan F., Wang L., Hu T., Zhou H., Hu Z., Zhou W., Zhao L., Chen J., Meng Y., Wang J., Lin Y., Yuan J., Xie Z., Ma J., Liu W.J., Wang D., Xu W., Holmes E.C., Cao G.F., Wu G., Chen W., Shi W., Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]