Abstract
Objective
In the present study, we quantified the effect of the coronavirus disease 2019 (COVID-19) on the volume of adult and pediatric neurosurgical procedures, inpatient consultations, and clinic visits at an academic medical center.
Methods
Neurosurgical procedures, inpatient consultations, and outpatient appointments at Vanderbilt University Medical Center were identified from March 23, 2020 through May 8, 2020 (during COVID-19) and March 25, 2019 through May 10, 2019 (before COVID-19). The neurosurgical volume was compared between the 2 periods.
Results
A 40% reduction in weekly procedural volume was demonstrated during COVID-19 (median before, 75; interquartile range [IQR], 72–80; median during, 45; IQR, 43–47; P < 0.001). A 42% reduction occurred in weekly adult procedures (median before, 62; IQR, 54–70; median during, 36; IQR, 34–39; P < 0.001), and a 31% reduction occurred in weekly pediatric procedures (median before, 13; IQR, 12–14; median during, 9; IQR, 8–10; P = 0.004). Among adult procedures, the most significant decreases were seen for spine (P < 0.001) and endovascular (P < 0.001) procedures and cranioplasty (P < 0.001). A significant change was not found in the adult open vascular (P = 0.291), functional (P = 0.263), cranial tumor (P = 0.143), or hydrocephalus (P = 0.173) procedural volume. Weekly inpatient consultations to neurosurgery decreased by 24% (median before, 99; IQR, 94–114; median during, 75; IQR, 68–84; P = 0.008) for adults. Weekly in-person adult and pediatric outpatient clinic visits witnessed a 91% decrease (median before, 329; IQR, 326–374; median during, 29; IQR, 26–39; P < 0.001). In contrast, weekly telehealth encounters increased from a median of 0 (IQR, 0–0) before to a median of 151 (IQR, 126–156) during COVID-19 (P < 0.001).
Conclusions
Significant reductions occurred in neurosurgical operations, clinic visits, and inpatient consultations during COVID-19. Telehealth was increasingly used for assessments. The long-term effects of the reduced neurosurgical volume and increased telehealth usage on patient outcomes should be explored.
Key words: COVID-19, Elective surgery, Neurological surgery, SARS-CoV-2, Telehealth, Trauma
Abbreviations and Acronyms: ACS, American College of Surgeons; COVID-19, Coronavirus disease 2019; CPT, Current Procedural Terminology; ED, Emergency department; IQR, Interquartile range; VUMC, Vanderbilt University Medical Center
Introduction
Coronavirus disease 2019 (COVID-19) resulting from infection with novel severe acute respiratory syndrome coronavirus 2 was initially identified in December 2019.1, 2, 3 By March 2020, COVID-19 had been declared a global pandemic, and the executive branch of the U.S. government announced a national emergency.4 , 5 Rapidly evolving guidelines emphasized social distancing as a necessary strategy to reduce viral spread.6 , 7 Subsequently, a series of federal recommendations and executive orders from 31 states recommended the cancellation of elective scheduled medical procedures.8, 9, 10, 11 However, the dichotomization of elective versus nonelective procedures has been criticized for inadequately risk-stratifying patients.12 Within neurological surgery, concerns exist about the potential harms created by delays in care.13 The potential adverse effects resulting from a delay in an elective procedure vary by neurosurgical subspecialty, whether vascular, oncology, functional, spine, or pediatrics. Patients with tumors amenable to endoscopic endonasal resection could be especially at risk, because many institutions have followed guidelines recommending the indefinite cancellation of these cases owing to the aerosolizing nature of the approach.14, 15, 16 The effect of COVID-19 on neurosurgical case volume has been anecdotally reported through social networks, news media, and editorial pieces.13 , 17 , 18 A survey study assessing global neurosurgical volume changes during COVID-19 found that roughly one half of the respondents had reported a >50% decrease in total operative volume.19 However, these estimates and reports have not yet been quantified in the scientific literature.
In addition to procedures, inpatient consultations and outpatient encounters have been affected by COVID-19. To limit viral exposure, hospital administrators have adopted new protocols for in-hospital telehealth consultations to the emergency department (ED), in addition to telehealth consultations for outpatient clinics.20 , 21 Patient volume has also decreased as adult and pediatric EDs have experienced declines in non–COVID-related patients.22 The federal government has incentivized telehealth services by expanding safety net insurance policies and temporarily waiving certain requirements of the Health Insurance Portability and Accountability Act’s privacy rule.23 Before COVID-19, telehealth was rarely used in standard neurosurgical practice in the United States. However, in the setting of social distancing measures and concerns for the spread of infection, healthcare systems have escalated telehealth infrastructure to prevent lapses in care while protecting patients and faculty from exposure.24 , 25
With these rapid changes in U.S. healthcare infrastructure, institutions have described the profound effects of COVID-19 on neurosurgical practice through surveys and anecdotal reports. However, to the best of our knowledge, we are unaware of scientific data quantifying the effect of COVID-19 on the volume of neurosurgical care. In the present study, we aimed to quantify the effects of the COVID-19 pandemic on neurosurgical procedures, outpatient clinics, and inpatient consultation volume, stratified by age and subspecialty, at a large, academic, level 1 trauma center in the southeastern United States.
Methods
Study Population
We identified patients who had undergone a neurosurgical procedure, inpatient consultation, or outpatient clinic visit at Vanderbilt University Medical Center (VUMC), including Monroe Carell Jr. Children’s Hospital at Vanderbilt. VUMC is an academic, level 1 trauma center with 1019 beds operating in the southeast U.S. region. Patient records from March 23, 2020 through May 8, 2020 were collected and categorized as “during COVID-19.” This was the 7-week period immediately after the signing of a Tennessee gubernatorial executive order preventing “nonessential procedures.”9 Patient records from an analogous 7-week period from March 25, 2019 through May 10, 2019 were collected and categorized as “before COVID-19.” In addition to these periods, data were collected from the 59-week period spanning March 23, 2019 through May 8, 2020 to allow us to descriptively visualize neurosurgical volume trends over time.
Data Collection
Data were extracted from the institution’s electronic medical records using the Clarity reporting database (Epic Systems Corp., Verona, Wisconsin, USA). Neurosurgical operations were identified by the designation of ≥1 neurosurgery faculty as the primary or secondary surgeon for the case. Inpatient adult and pediatric neurosurgery consultations were extracted for the same period. Completed clinic visits with neurosurgery faculty, including telehealth visits, were also collected. Cases, inpatient consultations, and clinic visits were then classified into the primary indicator variable of before COVID-19 or during COVID-19. Sociodemographic data were collected, including patient age, race, primary insurance type, and home address postal code (Table 1 ). Adult procedures were defined as those performed on patients aged ≥18 years at the operation. Pediatric procedures were defined as those performed on patients aged <18 years. Procedures were defined using Current Procedural Terminology (CPT) codes. Inpatient consultations were grouped according to the team ordering the consultation and whether the patient had had a concurrent trauma surgery consultation during the same encounter. Clinic visits were divided by telehealth status. To determine the distance from the patient’s home to the hospital, the geometric centroid of the patient’s home postal code was mapped in relation to the GPS (global positioning system) coordinates of VUMC. Driving distances were calculated using R statistical software (R Foundation for Statistical Computing, Vienna, Austria) with Google Maps JavaScript API. Insurance type was categorized as Medicare, Medicaid, private, or uninsured (self-pay).
Table 1.
Cohort Demographics
| Variable | Total | Before COVID-19 | During COVID-19 | Univariable |
Multivariable |
|||
|---|---|---|---|---|---|---|---|---|
| Test Statistic | P Value | OR | 95% CI | P Value | ||||
| Study period (weeks) | 14 | 7 | 7 | NA | NA | NA | NA | NA |
| Adults | ||||||||
| Neurosurgical procedures | 696 | 439 | 257 | |||||
| Patient age (years) | H = 0.88 | 0.348 | 0.99 | 0.98–1.00 | 0.112 | |||
| Median | 60 | 60 | 59 | |||||
| IQR | 47–69 | 47–70 | 46–69 | |||||
| Race | χ2 = 0.07 | 0.963 | ||||||
| White | 607 (87) | 382 (87) | 225 (88) | Ref | Ref | Ref | ||
| Black | 65 (9) | 42 (10) | 23 (9) | 0.86 | 0.47–1.53 | 0.613 | ||
| Other | 24 (3) | 15 (3) | 9 (4) | 1.31 | 0.53–3.12 | 0.550 | ||
| Insurance type | χ2 = 1.93 | 0.588 | ||||||
| Private | 329 (49) | 210 (49) | 119 (49) | Ref | Ref | Ref | ||
| Medicare | 276 (41) | 176 (41) | 100 (41) | 1.13 | 0.77–1.68 | 0.532 | ||
| Medicaid | 25 (4) | 14 (3) | 11 (5) | 1.26 | 0.54–2.89 | 0.588 | ||
| Uninsured | 43 (6) | 31 (7) | 12 (5) | 0.50 | 0.21–1.07 | 0.088 | ||
| Distance from hospital (miles) | H = 1.57 | 0.210 | 1.00 | 1.00–1.00 | 0.061 | |||
| Median | 150 | 152 | 142 | |||||
| IQR | 110–233 | 113–234 | 110–223 | |||||
| Children | ||||||||
| Neurosurgical procedures | 162 | 96 | 66 | |||||
| Patient age (years) | H = 0.52 | 0.471 | 0.99 | 0.93–1.04 | 0.600 | |||
| Median | 4 | 5 | 2 | |||||
| IQR | 1–13 | 1–14 | 0–13 | |||||
| Race | χ2 = 1.88 | 0.390 | ||||||
| White | 126 (78) | 73 (76) | 53 (80) | Ref | Ref | Ref | ||
| Black | 20 (12) | 11 (11) | 9 (14) | 0.97 | 0.32–2.85 | 0.950 | ||
| Other | 16 (10) | 12 (12) | 4 (6) | 0.44 | 0.11–1.45 | 0.201 | ||
| Insurance type | χ2 = 1.47 | 0.479 | ||||||
| Private | 125 (77) | 71 (74) | 11 (17) | Ref | Ref | Ref | ||
| Medicaid | 33 (20) | 22 (23) | 54 (82) | 0.71 | 0.29–1.66 | 0.437 | ||
| Uninsured | 4 (2) | 3 (3) | 1 (2) | 0.61 | 0.03–5.65 | 0.684 | ||
| Distance from hospital (miles) | H = 5.41 | 0.021 | 1.00 | 1.00–1.00 | 0.035 | |||
| Median | 163 | 140 | 198 | |||||
| IQR | 106–266 | 99–207 | 113–371 | |||||
Data presented as n (%), unless noted otherwise.
COVID-19, coronavirus disease 2019; OR, odds ratio; CI, confidence interval; NA, not applicable; IQR, interquartile range; Ref, reference.
Clinical Management During COVID-19
The Tennessee executive order provided general guidance to delay “any medical procedure that is not necessary to address a medical emergency or to preserve the health and safety of a patient, as determined by a licensed medical provider.”9 Similar to executive orders from other states, no official documentation was provided to guide Tennessee’s triage strategies.8 In anticipation of this order and the potential surge in patients, VUMC implemented recommendations on March 20, 2020 to cancel elective procedures for all specialties.26 An elective procedure was defined by VUMC as surgery that could safely wait 8 weeks. This timeline correlated with the 6–8-week delay estimated by the American College of Surgeons (ACS) for triage of nonemergent surgical procedures.27 Although the ACS guidelines might have influenced decisions, they were not formally adopted by VUMC. Thus, the decision to delay a procedure was left to the discretion of the attending neurosurgeon of record. Examples of procedures that were generally considered to be nonelective included malignant brain and spine tumors, severe myelopathy, new-onset hydrocephalus or shunt malfunction, a ruptured aneurysm or other vascular malformation, intracranial hemorrhage evacuation, and unstable spinal fractures.
Primary Outcome
The primary outcome was the weekly volume of neurosurgical procedures categorized by type. Neurosurgical procedure categories were decoded from CPT codes and grouped into the following categories: spine, endovascular, open vascular, functional, cranial tumor, hydrocephalus, cranioplasty, and other. These categories were then divided into adult and pediatric. The CPT codes associated with each category of procedure in the study population are provided in Supplementary Table 1. Each category was defined by and further divided into subcategories according to clinical similarities, urgency, and approach (Table 2 ). Spine was subdivided into traumatic spinal fusion, nontraumatic spinal fusion, and nontraumatic laminectomy, discectomy, foraminotomy, or spinal mass resection without fusion. Endovascular was subdivided into diagnostic cerebral angiography, mechanical thrombectomy for acute ischemic stroke, endovascular treatment of a ruptured intracranial aneurysm or vascular malformation, and endovascular treatment of an unruptured intracranial aneurysm or vascular malformation. Open vascular was subdivided into craniotomy for acute vascular condition (e.g., spontaneous intracranial hemorrhage evacuation, decompressive craniectomy for stroke, clipping of a ruptured aneurysm) and craniotomy for a nonacute condition (e.g., treatment of an unruptured aneurysm or vascular malformation). Functional was subdivided into craniotomy for deep brain stimulation, implantable pulse generator revision or replacement, and other functional procedures (e.g., craniotomy for epilepsy, spinal stimulator insertion, intrathecal baclofen pump insertion or revision, selective dorsal rhizotomy). Cranial tumor was subdivided into craniotomy for mass resection or brain biopsy and an endoscopic endonasal approach for mass resection. Hydrocephalus was defined as ventriculoperitoneal shunt insertion or revision or endoscopic third ventriculostomy. Other procedure was defined as any procedure that did not fit into the previous categories. Procedure subcategories with a lower clinical likelihood of categorization into “high acuity” tier 3a or 3b, as defined by the ACS guidelines, are indicated in Table 2.27
Table 2.
Weekly Adult and Pediatric Neurosurgical Procedures Stratified by Tennessee Gubernatorial Executive Order
| Variable | Before COVID-19 | During COVID-19 | Test Statistic (H) | P Value |
|---|---|---|---|---|
| Study period (weeks) | 7 | 7 | NA | NA |
| Total weekly cases | 75 (72–80) | 45 (43–47) | 38.47 | <0.001∗ |
| Weekly adult cases | 62 (54–70) | 36 (34–39) | 37.08 | <0.001∗ |
| Weekly pediatric cases | 13 (12–14) | 9 (8–10) | 12.33 | 0.004∗ |
| Adult weekly procedures | ||||
| Spine | 20 (18–23) | 8 (6–10) | 37.76 | <0.001∗ |
| Trauma-related spinal procedures | 1 (1–4) | 2 (2–2) | 0.33 | 0.575 |
| Non–trauma-related spinal fusion† | 16 (14–16) | 4 (3–7) | 39.20 | <0.001∗ |
| Non–trauma-related laminectomy, discectomy, foraminotomy, mass resection without fusion† | 3 (3–6) | 1 (0–2) | 11.11 | 0.006∗ |
| Endovascular | 13 (12–18) | 7 (6–10) | 19.03 | <0.001∗ |
| Mechanical thrombectomy for acute ischemic stroke | 3 (1–4) | 3 (2–3) | 0.02 | 0.901 |
| Endovascular treatment of ruptured intracranial aneurysm or vascular malformation | 2 (1–2) | 2 (2–2) | 0.11 | 0.746 |
| Diagnostic angiogram† | 8 (8–10) | 4 (3–5) | 9.37 | 0.010∗ |
| Endovascular treatment of unruptured intracranial aneurysm or vascular malformation† | 3 (2–5) | 1 (1–1) | 19.11 | <0.001∗ |
| Open vascular | 2 (1–4) | 1 (1–2) | 1.22 | 0.291 |
| Craniotomy for spontaneous intracranial hemorrhage evacuation, decompressive craniectomy for stroke, or clipping of ruptured aneurysm | 1 (1–2) | 0 (0–0) | NA | NA |
| Craniotomy for treatment of unruptured aneurysm or vascular malformation† | 1 (0–2) | 1 (1–1) | NA | NA |
| Functional | 9 (8–10) | 6 (6–8) | 1.38 | 0.263 |
| Implantable pulse generator revision or replacement | 3 (3–4) | 5 (4–6) | NA | NA |
| Craniotomy for deep brain stimulation† | 3 (2–3) | 0 (0–0) | NA | NA |
| Other: craniotomy for epilepsy, spinal stimulator insertion, intrathecal baclofen pump insertion or revision, selective dorsal rhizotomy† | 5 (3–6) | 2 (1–2) | NA | NA |
| Cranial tumor | 7 (6–8) | 5 (5–6) | 2.45 | 0.143 |
| Craniotomy for mass resection or brain biopsy | 5 (2–6) | 5 (4–6) | NA | NA |
| Endoscopic endonasal approach surgery for mass resection† | 2 (1–4) | 0 (0–0) | NA | NA |
| Hydrocephalus | 3 (2–4) | 2 (2–2) | 2.10 | 0.173 |
| Cranioplasty† | 2 (2–3) | 0 (0–0) | 35.25 | <0.001∗ |
| Other procedure† | 3 (2–6) | 4 (4–5) | 0.49 | 0.498 |
Data presented as median (interquartile range).
COVID-19, coronavirus disease 2019; NA, not applicable.
Statistically significant.
Procedure types with a low clinical likelihood of categorization as high acuity tier 3a or 3b according to American College of Surgeons guide for triage of nonemergent surgical procedures.
Secondary Outcomes
Secondary outcomes included the volume of inpatient consultations, trauma-related cranial neurosurgical procedures, and outpatient clinic encounters. Inpatient consultations were subcategorized according to whether the patient had also received a trauma consultation during the encounter. Trauma-related cranial procedures were defined as craniotomy for traumatic intracranial hemorrhage evacuation or decompressive craniectomy. Outpatient clinic encounters were categorized according to subspecialty and whether they had been performed via telehealth or in-person.
Statistical Analysis
All statistical analyses were generated using R, version 3.6 (R Foundation for Statistical Computing). Aggregations for data display were performed using Tableau, version 2019.3 (Tableau Software, Mountain View, California, USA). Graphs were created to visualize the volume of neurosurgical procedures, inpatient consultations to neurosurgery, and outpatient clinic encounters from March 23, 2019 through May 8, 2020. For data that did not follow a normal distribution, the median and interquartile range (IQR) are reported, instead of the mean ± standard deviation. The Kruskal-Wallis rank sum test was used for univariable analyses involving 1 categorical and 1 continuous variable (e.g., comparisons between during COVID-19 and before COVID-19) for the weekly volume of neurosurgical procedures, inpatient consultations, and outpatient clinic visits, as well as for patient age and distance traveled for the neurosurgical procedure. If the analysis of a parent procedural category showed a significant change during COVID-19, a statistical analysis of the procedural subcategories was performed. The Pearson χ2 test was used to analyze 2 categorical variables (e.g., comparisons between during COVID-19 and before COVID-19 for race and insurance type for patients undergoing a neurosurgical procedure). The H statistic of the Kruskal-Wallis test is an approximation of a distributed χ2, which represents the variance of ranks between groups. Multivariable analysis of the demographic features of the patients undergoing a neurosurgical procedure was also performed comparing the data during COVID-19 and before COVID-19. After dividing the adult and pediatric populations, 2 multiple logistic regression analyses were performed to model the occurrence of a procedure during COVID-19 as a function of the demographic variables of age, race, insurance type, and distance traveled. White race and private insurance were the reference categories for race and insurance type, respectively. Statistical significance was set a priori at P < 0.05.
Results
Sociodemographic Data
A total of 858 neurosurgical procedures (696 adult and 162 pediatric), 1485 inpatient consultations (1253 adult and 232 pediatric), and 3736 outpatient clinic encounters (3158 adult and 578 pediatric) had met the inclusion criteria for the before COVID-19 and during COVID-19 periods. The median age of our cohort for the adult and pediatric groups was 60 years (IQR, 47–69) and 4 years (IQR, 1–13 years), respectively. Most patients were White, comprising 87% of adult patients (n = 607) and 78% of pediatric patients (n = 126). Most adult patients (49%; n = 329) were privately insured, and 41% (n = 276) had Medicare insurance. Of the pediatric patients, 125 (77%) were privately insured. The median distance that patients had traveled from their home to receive operative care at our institution was 150 miles (IQR, 110–233 miles) for the adult group and 163 miles (IQR, 106–266 miles) for the pediatric group (Table 1). Of the inpatient consultations, 362 were trauma-related (24%). For adults and children, the rate of telehealth encounters of the total outpatient encounters during COVID-19 was 88% (n = 924) and 47% (n = 85), respectively.
Neurosurgical Procedures
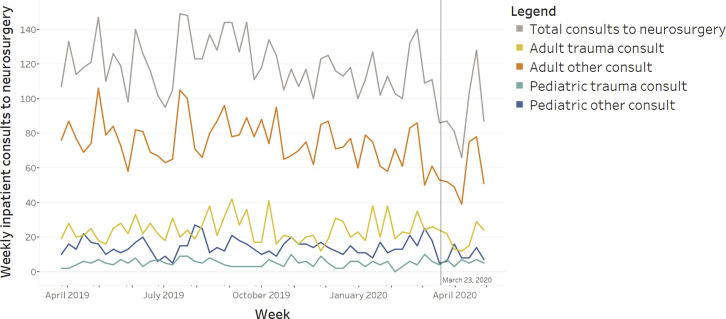
Overall, we found a 40% reduction in weekly procedural volume (median before, 75 per week; IQR, 72–80 per week; median during, 45 per week; IQR, 43–47 per week) during COVID-19 (H = 38.47; P < 0.001). This downtrend had begun ~2 weeks before the March 23 Tennessee executive order (Figure 1 ). A significant increase had occurred in the distance (median before, 140 miles; IQR, 99–207 miles; median during, 198 miles; IQR, 113–371 miles) traveled to the hospital for a neurosurgical procedure for the pediatric patients during COVID-19 (H = 5.41; P = 0.021). Multivariable analysis revealed that the distance traveled to the hospital remained significantly associated with the COVID-19 period for pediatric patients (odds ratio, 1.001/1 mile; 95% confidence interval, 1.000–1.001; P = 0.035). Differences in the distance traveled by adult patients for surgery (median before, 152 miles; IQR, 113–234 miles; median during, 142; IQR, 110–223 miles) was not significantly associated with the COVID-19 period on univariable (H = 1.57; P = 0.210) or multivariable (odds ratio, 1.000/1 mile; 95% confidence interval, 0.999–1.000; P = 0.061) analysis. No other demographic variables in the adult or pediatric populations were significantly associated with the during COVID-19 period (Table 1).
Figure 1.
Number of weekly neurosurgical procedures over time, stratified by patient age group.
Adult procedures had decreased by 42% (median before, 62 per week; IQR, 54–70 per week; median during, 36 per week; IQR, 34–39 per week; H = 37.08; P < 0.001), and pediatric procedures had decreased by 31% (median before, 13 per week; IQR, 12–14 per week; median during, 9 per week; IQR, 8–10 per week; H = 12.33; P = 0.004; Table 2). Among the categories of adult procedures, significant reductions had occurred in spine (median before, 20 per week; IQR, 18–23 per week; median during, 8 per week; IQR, 6–10 per week; H = 37.76; P < 0.001), endovascular (median before, 13 per week; IQR, 12–18 per week; median during, 7 per week; IQR, 6–10 per week; H = 19.03; P < 0.001), and cranioplasty (median before, 2 per week; IQR, 2–3 per week; to median during, 0 per week; IQR, 0–0 per week; H = 35.25; P < 0.001) cases. No significant changes were found in procedural volume for open vascular (median before, 2 per week; IQR, 1–4 per week; median during, 1; IQR, 1–2 per week; H = 1.22; P = 0.291), functional (median 9 per week; IQR, 8–10 per week; median during, 6; IQR, 6–8 per week; H = 1.38; P = 0.263), cranial tumor (median before, 7 per week; IQR, 6–8 per week; median during, 5 per week; IQR, 5–6 per week; H = 2.45; P = 0.143), hydrocephalus (median before, 3 per week; IQR, 2–4 per week; median during, 2 per week; IQR, 2–2 per week; H = 2.10; P = 0.173), or other procedure (median before 3 per week; IQR, 2–6 per week; median during, 4 per week; IQR, 4–5 per week; H = 0.49; P = 0.498) categories within the adult population (Table 2). The specific subcategories of adult procedures with significant reductions are listed in Table 2. Craniotomy for deep brain stimulation decreased from a median of 3 per week (IQR, 2–3 per week) to 0 (IQR, 0–0), although statistical testing was not performed because of the nonsignificance of the parent functional category. An analysis of the specific categories for pediatric procedures was not performed owing to insufficient volume to power the analysis.
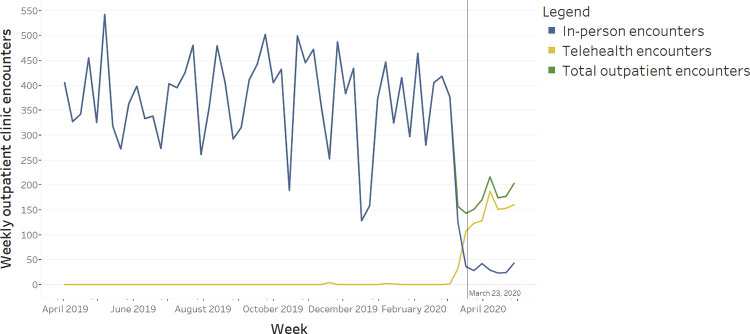
Inpatient Consultations to Neurosurgery and Trauma-Related Cranial Procedures
Weekly neurosurgical consultations during COVID-19 had decreased by 28% (median before, 121 per week; IQR, 116–128 per week; median during, 87 per week; IQR, 84–95 per week; H = 9.08; P = 0.011). Adult consultations had decreased by 24% (median before, 99 per week; IQR, 94–114 per week; median during, 75 per week; IQR, 68–84 per week; H = 9.99; P = 0.008). No significant reductions were found in pediatric consultations (median before, 18 per week; IQR, 14–22 per week; median during, 13 per week; IQR, 12–17 per week; H = 1.37; P = 0.265). The number of weekly trauma-related consultations did not significantly change for adults (median before, 21 per week; IQR, 20–24 per week; median during, 22; IQR, 14–24 per week; H = 0.19; P = 0.672) or children (median before, 4 per week; IQR, 3–6 per week; median during, 5; IQR, 4–7 per week; H = 1.43; P = 0.256). The weekly volume of trauma-related cranial procedures had not significantly decreased for adults (median before 3 per week; IQR, 2–4 per week; median during, 2 per week; IQR, 2–4 per week; H = 0.20; P = 0.663) or children, although it had approached significance for children (median before, 1 per week; IQR, 0–1 per week; median during, 0 per week; IQR, 0–0 per week; H = 3.24; P = 0.097; Table 3 ).
Table 3.
Weekly Inpatient Consultations to Neurosurgery and Trauma-Related Neurosurgical Procedures Stratified by Gubernatorial Executive Order and Mechanisms of Injury∗
| Variable | Before COVID-10 | During COVID-19 | Test Statistic (H) | P Value |
|---|---|---|---|---|
| Study period (weeks) | 7 | 7 | NA | NA |
| Total weekly consultations | 121 (116–128) | 87 (84–95) | 9.08 | 0.011† |
| Adult | ||||
| Weekly total consultations | 99 (94–114) | 75 (68–84) | 9.99 | 0.008† |
| Weekly trauma consultations | 21 (20–24) | 22 (14–24) | 0.19 | 0.672 |
| Weekly other consultations | 77 (72–88) | 52 (50–64) | 7.50 | 0.018† |
| Pediatric | ||||
| Weekly total consultations | 18 (14–22) | 13 (12–17) | 1.37 | 0.265 |
| Weekly trauma consultations | 4 (3–6) | 5 (4–7) | 1.43 | 0.256 |
| Weekly other consultations | 16 (12–16) | 8 (6–11) | 3.99 | 0.069 |
| Weekly trauma-related cranial procedures | ||||
| Adult | 3 (2–4) | 2 (2–4) | 0.20 | 0.663 |
| Pediatric | 1 (0–1) | 0 (0–0) | 3.24 | 0.097 |
Data presented as median (interquartile range).
COVID-19, coronavirus disease 2019; NA, not applicable.
Procedures directly affiliated with trauma-related consultations were also included as a measure of injury severity before and after the executive order; the weekly trauma-related cranial procedures included craniotomy for intracranial hemorrhage evacuation and decompressive craniectomy.
Statistically significant.
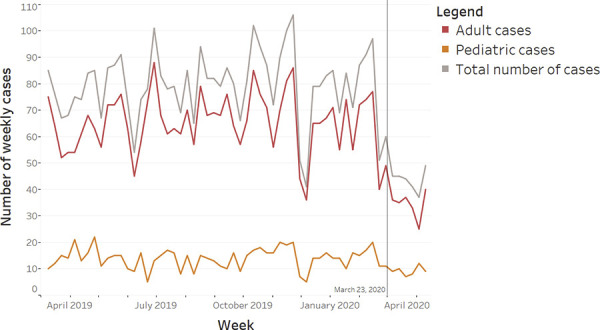
Outpatient Neurosurgery Clinic Encounters
A total decrease of 47% had occurred in completed outpatient clinic encounters (median before, 329 per week; IQR, 326–374 per week; median during, 174; IQR, 160–190 per week; H = 36.75; P < 0.001). Of the specific clinics, significant reductions had occurred in encounters for spine clinic (median before, 191 per week; IQR, 182–207 per week; median during, 87 per week; IQR, 78–100 per week; H = 36.75; P < 0.001), vascular clinic (median before, 26 per week; IQR, 22–28 per week; median during, 11 per week; IQR, 8–16 per week; H = 21.20; P < 0.001), functional clinic (median before, 30 per week; IQR, 26–30 per week; median during, 13 per week; IQR, 9–19 per week; H = 15.12; P = 0.002), and pediatrics clinic (median before, 57 per week; IQR, 44–66 per week; median during, 27 per week; IQR, 21–32 per week; H = 37.65; P < 0.001). No significant reductions were found in encounters for the tumor clinic (median before 32 per week; IQR, 20–34 per week; median during, 18; IQR, 16–24 per week; H = 1.37; P = 0.265) or pituitary clinic (median before, 1 per week; IQR, 0–4 per week; median during, 3 per week; IQR, 1–3 per week; H = 0.00; P = 0.950). In-person clinic encounters had decreased by 91% during COVID-19 (median before, 329 per week; IQR, 326–374 per week; median during, 29 per week; IQR, 26–39 per week; H = 36.75; P < 0.001). In contrast, telehealth visits had concurrently increased from a median of 0 per week before COVID-19 (IQR, 0–0 per week) to a median of 151 per week during COVID-19 (IQR, 126–156 per week; H = 73.50; P < 0.001; Table 4 ).
Table 4.
Weekly Neurosurgical Outpatient Clinic Visits Stratified by Gubernatorial Executive Order, Neurosurgical Subspecialty, and Encounter Type
| Variable | Before COVID-19 | During COVID-19 | Test Statistic (H) | P Value |
|---|---|---|---|---|
| Study period (weeks) | 7 | 7 | NA | NA |
| Weekly clinic visits | 329 (326–374) | 174 (160–190) | 36.75 | <0.001∗ |
| Weekly telehealth encounters | 0 (0–0) | 151 (126–156) | 73.50 | <0.001∗ |
| Weekly in-person encounters | 329 (326–374) | 29 (26–39) | 36.75 | <0.001∗ |
| Weekly spine encounters | 191 (182–207) | 87 (78–100) | 36.75 | <0.001∗ |
| Weekly vascular encounters | 26 (22–28) | 11 (8–16) | 21.20 | <0.001∗ |
| Weekly functional encounters | 30 (26–30) | 13 (9–19) | 15.12 | 0.002∗ |
| Weekly tumor encounters | 32 (20–34) | 18 (16–24) | 1.37 | 0.265 |
| Weekly pituitary encounters | 1 (0–4) | 3 (1–3) | 0.00 | 0.950 |
| Weekly pediatric encounters | 57 (44–66) | 27 (21–32) | 36.75 | <0.001∗ |
Data presented as median (interquartile range).
COVID-19, coronavirus disease 2019; NA, not applicable.
Statistically significant.
Discussion
The COVID-19 pandemic has created unprecedented barriers to the delivery of neurosurgical care in the United States. In the present study, we have described the experience of a single academic institution in the southeastern United States after a nonspecific governmental mandate to cancel elective procedures, similar to those enacted in 30 other states.8 The resultant guidelines applied by our institution mirrored those from nationwide academic and private hospitals with similar mandates.28 At our institution, the clinical volumes had subsequently decreased across all neurosurgical procedures, inpatient consultations, and clinic visits by 40%, 28%, and 47%, respectively (Figure 1, Figure 2, Figure 3 ). The effect on procedures and clinic visits was noted across both pediatric and adult practices, although it was less marked for children. For adults, the most affected subspecialty services were elective spine and endovascular cases; however, a significant reduction was also seen for cranioplasty cases. When sociodemographic variables were assessed across all ages, the only notable change was an increase in the median distance traveled for pediatric patients requiring neurosurgical procedures. In addition to inpatient encounters, the ramifications of the pandemic were sustained on an outpatient level. In-person outpatient visits experienced a marked 91% reduction, with an extraordinarily rapid escalation in telehealth visits. As neurosurgical departments adapt to the COVID-19 pandemic, an understanding of the disproportionate effects of the pandemic on specific subspecialties at our institution could inform targeted care reescalation in other programs and future research assessing the effects of the pandemic on neurosurgical outcomes and long-term telehealth usage.
Figure 2.
Number of weekly inpatient consultations to neurosurgery over time, stratified by patient age group and trauma-related versus non–trauma-related consultation.
Figure 3.
Number of weekly clinic visits over time, stratified by telehealth and in-person visits.
The lack of a centralized framework for care allocation during the COVID-19 pandemic has led to individual hospital systems, professional medical organizations, and surgeons independently navigating important clinical and public health decisions. A joint letter to Surgeon General Adams on behalf of U.S. hospitals outlined the concerns that COVID-19 recommendations are “without clear agreement on how we classify various levels of necessary care.”29 Although the ACS released guidelines for triage of nonemergent surgical procedures,27 the guidelines contained no frameworks specific to neurosurgical procedures. Similar to language used in other states, Tennessee’s executive order mandated the cancellation of all “nonessential” procedures, except those for which “postponement would significantly impact the health, safety, or welfare of the patient.”8 , 9 A federal guide published by the Centers for Medicare and Medicaid Services noted that decisions “remain the responsibility of local healthcare delivery systems… and those surgeons who have direct responsibility for their patients.”30 Because of the paucity of detailed triage frameworks for neurosurgery, our institution deferred the final decision of procedure cancellation to the attending surgeon. The reduction in procedural volume and outpatient encounters began in the 2 weeks before the Tennessee executive order (Figures 1 and 3). We suspect this represented anticipation of the looming events by surgeons and potential concerns among patients regarding in-hospital viral exposure. The changes in procedural volume during COVID-19 were not substantially affected by sociodemographic variables, with the exception of an increase in the median distance traveled for pediatric cases. This finding might be related to referrals from regional centers offering limited services because of the pandemic and could be further explored in a study incorporating multiple pediatric neurosurgery centers.
As expected, the largest procedural reductions in our analysis were found in the subspecialties with robust elective practices, such as spine and endovascular neurosurgery. However, the number of time-sensitive procedures within each of these practices remained unchanged, such as trauma-related spinal procedures, endovascular treatment of stroke, and endovascular treatment of ruptured vascular pathology. In the period before COVID-19, the generally nonemergent procedure subcategories (Table 2) comprised ~74% of the adult neurosurgical procedural volume. The decrease of 42% in the adult procedural volume in our analysis indicates the persistence of some nonemergent procedures at the attending surgeon’s discretion. A review of the medical records of nontraumatic spine procedures performed during COVID-19 revealed trends of worsening neurologic examination findings, the development of structural instability, malignant spread, and abscesses informing the decision to operate. For diagnostic angiograms and endovascular treatment of unruptured vascular pathologies, a review of medical records during the COVID-19 period showed that these procedures were generally characterized by lesions with a high risk of ischemia or rupture and those causing neurological symptoms. These trends might be generalizable to other large tertiary care centers with comparable caseloads. A review of VUMC’s elective satellite spine practices showed a largely unchanged rate of 1–2 procedures per month. However, the procedures performed in these centers during COVID-19 had been similarly marked by patients with acute worsening of neurological symptoms. The consequences of delayed management for nonacute conditions have yet to be determined. However, the initial effects measured in the present study have set the foundation for future research. For example, unsecured cerebral aneurysms are known to have a risk of rupture of ~1% annually, and delayed deep brain stimulation is known to prolong debilitating extrapyramidal symptoms.31, 32, 33 Both of these types of procedures showed a volume reduction during COVID-19 in our study. Furthermore, spine and endovascular procedures are critical drivers of revenue for many hospitals, and the possible financial difficulties from a prolonged reduction in these procedures should be considered.34 As elective procedures resume, hospitals could experience an imbalance between surgical demand and available operating room space. One predictive modeling study estimated a median timeline of 45 weeks required for institutions to clear the estimated backlog of operations incurred during COVID-19.35 Importantly, this projection assumed a cancellation rate of 72%, markedly greater than the 40% procedural volume decrease noted in the present study. Within neurosurgical practice, these projections could be refined using data from the pandemic and postpandemic period. For future pandemics or similar medical disasters, validated predictive models could inform an outcomes-based framework to better define elective surgery, direct surgical patient care, and allocate surgical resources.
In addition to surgical procedures, inpatient consultations witnessed marked reductions for both children and adults. This effect was likely widespread throughout the United States and not confined to neurosurgery, given the 43% reduction in ED volume reported by the Centers for Disease Control and Prevention from mid-March through April 2020.22 Anecdotal evidence has pointed to patient concerns about exposure to COVID-19 as a principal driving factor for the reduction in ED visits,36 which could explain the significant reduction in non–trauma-related consultations (Figure 2). Consultations for trauma-related injuries were similar before and after the gubernatorial order, indicating that the frequency of traumatic injuries remained stable despite the stay at home orders issued within Tennessee and 45 other states.37 In addition, although a 25% reduction in motor vehicle accidents was reported in Tennessee (mirroring similar reductions nationwide),38, 39, 40, 41 no significant changes were found in the incidence of traumatic cranial procedures for adults or children. This trend might have resulted from the many “essential workers” who had continued to commute to work as well as the unchanged rate of firearm-related crimes in the Nashville area, trends also witnessed in other major cities such as Chicago and Philadelphia.42, 43, 44 The reinstatement of normal societal operations in the postpandemic period might increase inpatient consultations once more; however, the extent remains to be seen.
In the outpatient setting, the unprecedented increase in telehealth clinic visits from 0 151 per week was an important counterbalancing measure against the sudden decrease of in-person clinic visits (Figure 3). Telehealth’s introduction to the mainstream will require careful evaluation regarding the safety, satisfaction, and efficiency outcomes as neurosurgery clinics adapt to virtual environments during the pandemic and beyond. Even before the pandemic, telehealth had a promising record of improving patient satisfaction, increasing access to care, and reducing costs.45 , 46 The traditional barriers to telehealth, such as reimbursement policies, digital learning curves, integration into clinical workflows, and dedicated staffing,47 have been overcome during the pandemic at many institutions allowing for a quick expansion of telehealth usage.24 , 25 Given the reported positive effects on clinic workflow and patient satisfaction, it will be important for the neurosurgical community to assess how telehealth and its associated benefits can continue to be incorporated into daily practice.
Although the present study examined many important neurosurgical practice changes in response to the COVID-19 pandemic, the study did have limitations. As a single-center study, the statistical power was insufficient to analyze results for many individual surgical procedures; therefore, most procedures were grouped within their parent neurosurgical subspecialty. A more in-depth analysis could be completed using data from multiple institutions. A multi-institutional study would also help to assess regional variability in the United States resulting from local COVID-19 disease burden, state and local ordinances, and unique hospital-driven regulations in response to the pandemic. The focus of the present study on a large, tertiary, level 1 trauma center limited its generalizability to smaller hospitals that treat fewer trauma or transfer patients. Although we attempted to analyze the pandemic’s effects on satellite, largely elective, neurosurgical practices in the VUMC system, our investigation was limited by the low sample size. Second, the present report only included data through the first 7 weeks after the gubernatorial order to cease elective surgery, a short period. Because an aim of our study was to help institutions understand the disease’s immediate effect on their neurosurgical volume, expediency was deemed key. As additional data from the pandemic and postpandemic period become available, a more robust analysis of procedural changes could be performed. Similarly, the before COVID-19 period was defined using a period of 7 weeks from 2019 analogous to the during COVID-19 period. Although this reduced the effects of seasonal variation, the resultant decrease in sample size increased the likelihood of a type II error. Third, our analysis was unable to differentiate returning or follow-up outpatient visits from new patient visits owing to a limitation in the electronic medical records’ categorization of encounter type after implementing telehealth visits. A future study could aim to compare the data between returning and new patients. Fourth, the neurosurgical cases were identified according to the faculty listed as the principal or secondary surgeon. We attempted to be as thorough as possible by identifying co-surgeons in common collaborative cases. However, some cases could have been missed if a neurosurgeon had not been listed as a surgeon, which would have led to an underestimation of the true neurosurgical case volume. Finally, bedside and outpatient procedures, such as radiosurgery, pain procedures, deep brain stimulation bone markers, external ventricular drain placement, and intracranial pressure monitor placement were not included; thus, this further underestimates the true effect of the COVID-19 pandemic on neurosurgical practice.
Conclusions
The COVID-19 pandemic has led to significant and measurable decreases in neurosurgical caseload, inpatient consultations, and outpatient clinic visits. All subspecialties were affected. However, spine incurred the largest effects in both inpatient and outpatient settings. These results might be generalizable to similarly large, level 1 trauma centers and could also inform the design of multi-institutional analyses measuring the nationwide effects of the pandemic. As elective procedures and in-person clinical encounters resume, the effects of the reduced volume during COVID-19 on long-term patient outcomes warrants further investigation. Despite the decline of in-person neurosurgical clinic visits, telehealth visits witnessed a marked increase during the study period, indicative of quick practice adaptability to a rapidly changing situation. The possibility of sustainable telehealth integration into neurosurgical workflows and the resultant effects on access to care should be monitored and evaluated. These findings could guide the reescalation of neurosurgical care, better inform a united approach to neurosurgical care during the next pandemic or medical disaster, and provide the foundation for future neurosurgical outcomes research.
CRediT authorship contribution statement
Pious D. Patel: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Visualization, Writing - original draft, Writing - review & editing. Katherine A. Kelly: Writing - original draft, Writing - review & editing. Rebecca A. Reynolds: Conceptualization, Data curation, Methodology, Writing - original draft, Writing - review & editing. Robert W. Turer: Conceptualization, Data curation, Methodology, Writing - original draft, Writing - review & editing. Sanjana Salwi: Formal analysis, Methodology, Writing - original draft. S. Trent Rosenbloom: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Christopher M. Bonfield: Writing - original draft, Writing - review & editing. Robert P. Naftel: Writing - original draft, Writing - review & editing.
Footnotes
Conflict of interest statement: Dr. Reynolds serves as a Fogarty Global Health Trainee affiliated with the Vanderbilt-Emory-Cornell-Duke consortium and is supported by the Fogarty International Center at the National Institutes of Health (grant R25TW009337). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix
Supplementary Table 1.
Common Procedural Terminology Codes Associated with Each Category of Neurosurgical Procedures Defined∗
| Category | CPT Codes |
|---|---|
| Spine | 20250, 20930, 20931, 20936, 20937, 22015, 22100, 22101, 22102, 22110, 22116, 22206, 22207, 22210, 22212, 22214, 22216, 22224, 22325, 22326, 22533, 22551, 22552, 22554, 22556, 22558, 22585, 22586, 22590, 22595, 22600, 22610, 22612, 22614, 22630, 22632, 22633, 22634, 22800, 22802, 22804, 22840, 22842, 22843, 22844, 22845, 22846, 22849, 22850, 22852, 22853, 22854, 22855, 22856, 38724, 62287, 62350, 62351, 63001, 63003, 63005, 63011, 63012, 63015, 63016, 63017, 63020, 63030, 63035, 63042, 63045, 63046, 63047, 63048, 63055, 63056, 63081, 63082, 63085, 63266, 63271, 63275, 63276, 63277, 63280, 63281, 63282, 63283, 63286, 63287, 63303, 63662, 63688, 63709, 63740, 75705, 20692AO, 22558T, 22842TL, 22843GR, 22845C, 22845T, 22846C, 63047M, 63048M, C9757, PBONSPINE |
| Endovascular | 36013, 36215, 36216, 36218, 36221, 36223, 36224, 36226, 36227, 36245, 36470, 36620, 37215, 37216, 37217, 37218, 37236, 61624, 61626, 61630, 61635, 75650, 75671, 0075T, 36215P, 36216P, 36217P, 36218P, 75650T, STROKE |
| Open vascular | 61154, 61156, 61312, 61313, 61314, 61680, 61682, 61686, 61692, 61697, 61700, 61702, 61711, 70552 |
| Functional | 20670, 20680, 61533, 61534, 61536, 61537, 61538, 61540, 61541, 61566, 61760, 61860, 61863, 61864, 61867, 61880, 61885, 61886, 61888, 62355, 63650, 63655, 63661, 63664, 63685, 64555, 64568, 64570, 64575, 64585, 95970, 95971, 95972, 61781A, 61867–50, 61868–50, 61215, 62365, 62369, 63170, 63190, 63195, J0475, J0476 |
| Craniotomy for deep brain stimulation | 61860, 61863, 61864, 61867, 61867–50, 61868–50 |
| Cranial tumor | 31257, 31259, 61140, 61510, 61512, 61514, 61516, 61518, 61519, 61520, 61521, 61524, 61526, 61546, 61548, 61570, 61601, 61605, 61608, 61750, 61751, 62164, 62165, 61520A, 61526A |
| Hydrocephalus | 49324, 49325, 49418, 62161, 62220, 62230, 62256, 62258, 62223AX, 62230E, 62230V |
| Cranioplasty | 21180, 61316, 62120, 62121, 62142, 62143, 62145, 62147, 62148, 62121A |
| Trauma-related | 61343, 61345, 61450, 61154T |
CPT, Common Procedural Terminology.
The list is not comprehensive and is specific to the patient population included in the present study.
Supplementary Data
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. https://doi.org/10.1001/jama.2020.2648 [e-pub ahead of print]. JAMA. accessed April 22, 2020. [DOI] [PubMed]
- 3.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. Responding to Community Spread of COVID-19: Interim Guidance, 7 March 2020.https://extranet.who.int/iris/restricted/handle/10665/331421 Available at: [Google Scholar]
- 5.Trump D.J. 2020. Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak.https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/ Available at: [Google Scholar]
- 6.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas R.F., Christopher T.L. Identifying and interrupting superspreading events—implications for control of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26:1059–1066. doi: 10.3201/eid2606.200495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Surgeons . 2020. COVID-19: Executive Orders by State on Dental, Medical, and Surgical Procedures.https://www.facs.org/covid-19/legislative-regulatory/executive-orders Available at: [Google Scholar]
- 9.Lee B. 2020. Executive Order 18: An Order to Reduce the Spread of COVID-19 by Limiting Nonemergency Health Care Procedures.https://publications.tnsosfiles.com/pub/execorders/exec-orders-lee18.pdf Available at: [Google Scholar]
- 10.Lee B. 2020. Executive Order 25: An Order to Reduce the Spread of COVID-19 by Limiting Nonemergency Healthcare Procedures.https://publications.tnsosfiles.com/pub/execorders/exec-orders-lee25.pdf Available at: [Google Scholar]
- 11.Centers for Disease Control and Prevention . 2020. Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States.https://asprtracie.hhs.gov/technical-resources/resource/8232/interim-guidance-for-healthcare-facilities-preparing-for-community-transmission-of-covid-19-in-the-united-states Available at: [Google Scholar]
- 12.Stahel P.F. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wellons J.C., Grant G., Krieger M.D. Editorial: early lessons in the management of COVID-19 for the pediatric neurosurgical community from the leadership of the American Society of Pediatric Neurosurgeons. https://doi.org/10.3171/2020.3.Peds20215 [e-pub ahead of print]. J Neurosurg. accessed April 22, 2020. [DOI] [PMC free article] [PubMed]
- 14.Patel Z.M., Fernandez-Miranda J., Hwang P.H. Letter: precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020;87:E66–E67. doi: 10.1093/neuros/nyaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu W., Huang X., Zhao H., Jiang X. A COVID-19 patient who underwent endonasal endoscopic pituitary adenoma resection: a case report. https://doi.org/10.1093/neuros/nyaa147 [e-pub ahead of print]. Neurosurgery. accessed April 22, 2020. [DOI] [PMC free article] [PubMed]
- 16.North American Skull Base Society . 2020. NASBS Statement on COVID-19 Transmission During Endonasal Surgery.https://www.nasbs.org/wp-content/uploads/2020/04/nasbs-statement-on-covid-19-transmission-during-endonasal-surgery-3.20.20.pdf Available at: [Google Scholar]
- 17.Prall J.A., Davis J.D., Jenkins N.R. Editorial: community practice in the time of COVID-19. https://doi.org/10.3171/2020.4.Jns201033 [e-pub ahead of print]. J Neurosurg. accessed April 25, 2020. [DOI] [PMC free article] [PubMed]
- 18.Amin-Hanjani S., Bambakidis N.C., Barker F.G. Editorial: COVID-19 and neurosurgical practice: an interim report. https://doi.org/10.3171/2020.4.Jns201099 [e-pub ahead of print]. J Neurosurg. accessed April 25, 2020. [DOI] [PMC free article] [PubMed]
- 19.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention . 2020. Healthcare Facilities: Preparing for Community Transmission.https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html Available at: [Google Scholar]
- 21.American Medical Association . 2020. Telehealth Implementation Playbook.https://www.ama-assn.org/system/files/2020-04/ama-telehealth-playbook.pdf Available at: [Google Scholar]
- 22.Centers for Disease Control and Prevention COVIDView: Emergency Department Visits: Percentage of Visits for COVID-19-Like Illness (CLI) or Influenza-like Illness (ILI) https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/04242020/covid-like-illness.html Available at:
- 23.Centers for Medicare and Medicaid Services . 2020. Medicare Telemedicine Health Care Provider Fact Sheet.https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available at: [Google Scholar]
- 24.Patel P.D., Cobb J., Wright D. Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: barriers, solutions, results. https://doi.org/10.1093/jamia/ocaa065 [e-pub ahead of print]. J Am Med Inform Assoc. accessed April 25, 2020. [DOI] [PMC free article] [PubMed]
- 25.Wosik J., Fudim M., Cameron B. Telehealth transformation: COVID-19 and the rise of virtual care. https://doi.org/10.1093/jamia/ocaa067 [e-pub ahead of print]. J Am Med Inform Assoc. accessed May 17, 2020. [DOI] [PMC free article] [PubMed]
- 26.Balser J.R. 2020. Transcript: Dr. Jeff Balser on Altering Approach to Elective Care.https://www.vumc.org/coronavirus/transcript-dr-jeff-balser-altering-approach-elective-care Available at: [Google Scholar]
- 27.American College of Surgeons . 2020. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures.https://www.facs.org/covid-19/clinical-guidance/triage Available at: [Google Scholar]
- 28.Dyrda L. 2020. 12+ Health Systems Canceling, Postponing Surgeries Due to the Coronavirus Outbreak.https://www.beckershospitalreview.com/patient-flow/12-health-systems-canceling-postponing-surgeries-due-to-the-coronavirus-outbreak.html Available at: [Google Scholar]
- 29.American Hospital Association (AHA), the Association of American Medical Colleges (AAMC), the Children’s Hospital Association (CHA), and the Federation of American Hospitals (FAH) Open letter to Vice Admiral Jerome M. Adams, MD, United States Surgeon General; March 15, 2020. https://www.aamc.org/system/files/2020-03/HALOLettertoSG-031520.pdf Available at:
- 30.Centers for Medicare and Medicaid Services . 2020. Non-Emergent, Elective Medical Services, and Treatment Recommendations.https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf Available at: [Google Scholar]
- 31.Almeida L., Deeb W., Spears C. Current practice and the future of deep brain stimulation therapy in Parkinson’s disease. Semin Neurol. 2017;37:205–214. doi: 10.1055/s-0037-1601893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiebers D.O. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–110. doi: 10.1016/s0140-6736(03)13860-3. [DOI] [PubMed] [Google Scholar]
- 33.Williams L.N., Brown R.D., Jr. Management of unruptured intracranial aneurysms. Neurol Clin Pract. 2013;3:99–108. doi: 10.1212/CPJ.0b013e31828d9f6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benzil D.L., Zusman E.E. Defining the value of neurosurgery in the new healthcare era. Neurosurgery. 2017;80(suppl):S23–S27. doi: 10.1093/neuros/nyx002. [DOI] [PubMed] [Google Scholar]
- 35.Nepogodiev D., Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. https://doi.org/10.1002/bjs.11746 [e-pub ahead of print]. Br J Surg. accessed May 17, 2020. [DOI] [PMC free article] [PubMed]
- 36.Bruggeman L., Bhatt J. 2020. “They are terrified”: Fearing coronavirus, people with potentially fatal conditions avoid emergency care.https://abcnews.go.com/Health/terrified-fearing-coronavirus-people-potentially-fatal-conditions-avoid/story?id=70306931 Available at: [Google Scholar]
- 37.Mervosh S., Lu D., Swales V. 2020. See Which States and Cities Have Told Residents to Stay at Home.https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html Available at: [Google Scholar]
- 38.Tennessee Department of Safety and Homeland Security . 2020. Fatal & Serious Injury Crashes.https://www.tn.gov/safety/stats/dashboards/fatalseriousinjurycrashes.html Available at: [Google Scholar]
- 39.Rice B. 2020. Report: Ohio has seen a decrease in traffic accidents due to the new coronavirus pandemic.https://www.cincinnati.com/story/news/2020/04/16/report-ohio-has-seen-decrease-traffic-accidents-due-new-coronavirus-pandemic/5146034002/ Available at: [Google Scholar]
- 40.Shilling F., Waetjen D. Road Ecology Center at UC Davis; 2020. Special Report (Update): Impact of COVID19 Mitigation on Numbers and Costs of California Traffic Crashes.https://roadecology.ucdavis.edu/files/content/projects/COVID_CHIPs_Impacts_updated_415.pdf Available at: [Google Scholar]
- 41.Washington State Patrol . 2020. Collision Analysis Tool.https://fortress.wa.gov/wsp/collisionanalysistool/ Available at: [Google Scholar]
- 42.Tennessee Bureau of Investigation . 2020. TBI Releases January-March 2020 Statewide Crime Trends.https://tbinewsroom.com/2020/04/15/tbi-releases-january-march-2020-statewide-crime-trends/ Available at: [Google Scholar]
- 43.Dazio S., Briceno F., Tarm M. 2020. Crime drops around the world as COVID-19 keeps people inside.https://apnews.com/bbb7adc88d3fa067c5c1b5c72a1a8aa6 Available at: [Google Scholar]
- 44.Kaufman E. 2020. Please, Stop Shooting. We Need the Beds.https://www.nytimes.com/2020/04/01/opinion/covid-gun-violence-hospitals.html Available at: [Google Scholar]
- 45.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7:e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maryam A. Telemedicine and its role in revolutionizing healthcare delivery. Am J Account Care. 2017;5:e1–e5. [Google Scholar]
- 47.Lin C.-C.C., Dievler A., Robbins C., Sripipatana A., Quinn M., Nair S. Telehealth in health centers: key adoption factors, barriers, and opportunities. Health Affairs. 2018;37:1967–1974. doi: 10.1377/hlthaff.2018.05125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.