Abstract
Introduction
The height of the opioid epidemic in the USA has led to an increasing call for access to medication assisted treatment for opioid use disorder, including buprenorphine initiation from the emergency department (ED). However, only a small percentage of emergency physicians feel prepared or have the necessary training to prescribe buprenorphine. Twitter has increasingly been used as a tool for medical education, and there is growing interest in using this forum to actively engage medical providers and the public. This study examined the views regarding ED initiation of buprenorphine treatment among contributors to the quarterly American College of Medical Toxicology (ACMT) tweetchat, #firesidetox, and the demographics of the participants.
Methods
A mixed methods descriptive study was conducted to analyze individual responses and self-identified demographics among Twitter users participating in the #firesidetox tweetchat regarding the ACMT position statement about ED initiation of buprenorphine treatment.
Results
This tweetchat included 86 participants, the majority of whom were clinicians in the USA. Physicians accounted for 46% of participants primarily emergency medicine physician toxicologists and authored 75% of the tweets. It consisted of 317 tweets which most frequently described clinical vignettes or experience (46%) or medical education (25%) related to buprenorphine and had themes related to treatment initiation location (ED vs outpatient vs home) (8.6%) and challenges and solutions to buprenorphine administration (8.6%).
Conclusions
A tweetchat can be used to disseminate and discuss the adoption of buprenorphine in the ED. Importantly, the tweetchat provides a forum for experts to share narratives and expertise on implementation and barriers and successes in operationalizing buprenorphine administration in emergency departments.
Keywords: Twitter, Buprenorphine, Social media, Medication assisted treatment, Opioid use disorder
Introduction
In the last 13 years, Twitter has become a popular social media platform for accessing news, engaging in discussion, and expanding social networks. Twitter has 326 million monthly active users, 100 million daily active users, and 500 million tweets per day [1]. It provides a real-time internet forum in which individual users can compose publicly available messages, reply to messages, and reference other web sources. Additionally, the use of a hashtag helps aggregate tweets of similar topics that can then be queried, discussed, and searched retrospectively for reference and referral. These features of Twitter make it an attractive option for medical professionals to discuss, disseminate, and reflect on pertinent medical topics.
One unique feature of Twitter is the tweetchat. Tweetchats are real-time discussions among users where participants respond to tweets of a selected topic identified by a unique hashtag [2]. These tweetchats have served as an extension of the traditional in-person journal club and allowed increasingly diverse and wide reach among medical specialties [3]. Within medical toxicology, the American College of Medical Toxicology (ACMT) has used a quarterly tweetchat, #firesidetox, to facilitate discussions surrounding important journal articles for US and international toxicologists [4]. The #firesidetox tweetchat attracts a mean of 23 participants and 329,200 impressions (unique views from Twitter users) [4]. The procedures for selecting manuscripts and topics for #firesidetox have been previously described and demonstrated to be feasible in promoting discussion and collaboration among medical toxicologists and medical toxicology professional organizations [4].
On May 28, 2019, a #firesidetox tweetchat featured the ACMT position statement on access to medication assisted treatment (MAT) from the emergency department (ED) for individuals with opioid use disorder [5]. While many advocates have called for increasing access to MAT to combat the opioid epidemic, there remain operational and ideological barriers to initiating buprenorphine as MAT from the ED. Accordingly, the #firesidetox tweetchat was designed to be a forum to promote the ACMT position statement advocating for access to buprenorphine in the ED and to describe members’ experience initiating MAT from the ED. Given the ability of a tweetchat to form a permanent, searchable record, we sought to describe important topics, themes, and discussions that emerged from this #firesidetox.
Methods
We conducted a mixed-methods descriptive study in collaboration with a moderator of the #firesidetox tweetchat. An established, structured, quarterly tweetchat created by the ACMT and tagged #firesidetox was used as the discussion forum for this study. The #firesidetox tweetchat typically features a manuscript published in JMT selected by members of the #firesidetox steering committee. Three pre-determined topics selected from the manuscript are tweeted over an hour to foster discussion. Twitter conversation is moderated by a member of the #firesidetox steering committee to facilitate and provide questions for discussion. The tweetchat was structured according to existing protocols [4].
Prior to the tweetchat date, the ACMT position statement on ED-based buprenorphine administration was selected for discussion and made open access [5]. Expert participants were selected from the position statement’s authors. The position statement authors, the ACMT Twitter account, and regular participants of #firesidetox tweetchats sent #firesidetox tweetchat reminders via Twitter to help advertise #firesidetox to colleagues, medical professionals, other medical societies, and the general public. Email reminders were also sent to ACMT members. This study was reviewed and approved by the Institutional Review Board of the University of Pennsylvania.
Data Analysis
We downloaded the full tweetchat transcript (tweets with the #firesidetox hashtag and the replies to these tweets) at the start of the tweetchat and up to 48 hours after the conclusion of the tweetchat. We chose this parameter to remain consistent with previous #firesidetox metrics reporting and to capture asynchronous conversation from participants who were not able to engage in the tweetchat in real time. We obtained Twitter metrics using publicly available data from Symplur Healthcare Hashtags searching for #firesidetox. These metrics included number of participants, total number of tweets, impressions (the number of times a tweet is viewed by a unique user), tweets per hour, and tweets per participant.
Advertising tweets and tweets unrelated to the tweetchat discussion were eliminated from the transcript. We then utilized an adapted applied thematic analysis to qualitatively examine emerging topics, themes, and tweet content during the tweetchat [6]. We first identified key topics a priori using the structured questions of the tweetchat, which included the definition of MAT, initiation of buprenorphine in the ED, and specific protocols and expert advice related to implementation of buprenorphine in the ED. Next, we reviewed the transcript, generating additional topics, specific themes, and analysis of tweet content that were described during the discussion. The transcript was independently reviewed by three team members and tweets were assigned specific thematic codes. After coding, the coded tweets were read in aggregate and discussed by the research group. The list of final categorizations was reviewed by the study group, and tweet categorizations were quantified to glean information about what types of topics, themes, and content were discussed most, and how this discussion differed from previous ACMT tweetchats. We determined participant demographics based on publicly available information found in their Twitter profiles and tweets from the tweetchat to determine gender, occupation, and location.
Results
Overall, 86 Twitter users participated in this tweetchat (Table 1). Participants represented 27 different states in the USA and 5 additional countries (Canada, Poland, Qatar, Belgium, and Great Britain). Thirty-seven participants identified as physicians; 23% were toxicologists. Participants also included 5 pharmacists, 6 residents, 1 medical student, and 15 members of the public. Of the physician participants, 76% were emergency medicine physicians. Internal Medicine, Pathology, and Psychiatry were also represented (Table 1). Toxicologists authored 58% of all tweets while physicians authored 75% of tweets. Characterization was based on personal information shared in the tweetchat or in a user’s tweets or Twitter bio; therefore, if users did not specify their gender or occupation, they were counted in the “unknown” categories, which represented 24% of gender categorizations and 16% of occupation categorizations (Table 1).
Table 1.
Twitter demographics.
| N of participants (%) | N of tweets (%) | |
|---|---|---|
| Individuals | 80 | 246 |
| Gender | ||
| Male | 32 (40.0) | 151 (61.4) |
| Female | 29 (36.3) | 65 (26.4) |
| Unknown | 19 (23.8) | 30 (12.2) |
| Occupation | ||
| Toxicologist | 18 (22.5) | 140 (57.6) |
| Pharmacist | 5 (6.3) | 7 (2.9) |
| Physiciana | 37 (46.3) | 181 (74.5) |
| Emergency medicine | 28 (32.5) | 98 (36.2) |
| Internal medicine | 2 (2.3) | 12 (4.4) |
| Pathology | 1 (1.2) | 2 (0.7) |
| Psychiatry | 2 (2.3) | 3 (1.1 s) |
| Unknown | 8 (9.3) | 14 (5.2) |
| Resident | 6 (7.5) | 2 (0.8) |
| Medical student | 1 (1.3) | 0 (0) |
| Nurse | 6 (7.5) | 14 (5.8) |
| Physician’s assistant | 1 (1.3) | 1 (0.4) |
| Nurse practitioner | 1 (1.3) | 1 (0.4) |
| Paramedic | 3 (3.8) | 13 (5.3) |
| Person in recovery | 3 (3.8) | 10 (4.1) |
| Member of the public | 15 (18.8) | 19 (7.8) |
| Unknown | 13 (16.3) | 19 (7.8) |
| Organizations | 6 | 25 |
| Total | 86 | 271 |
aAll but one toxicologist were physicians and thus counted in both the “toxicologist” and “physician” categories
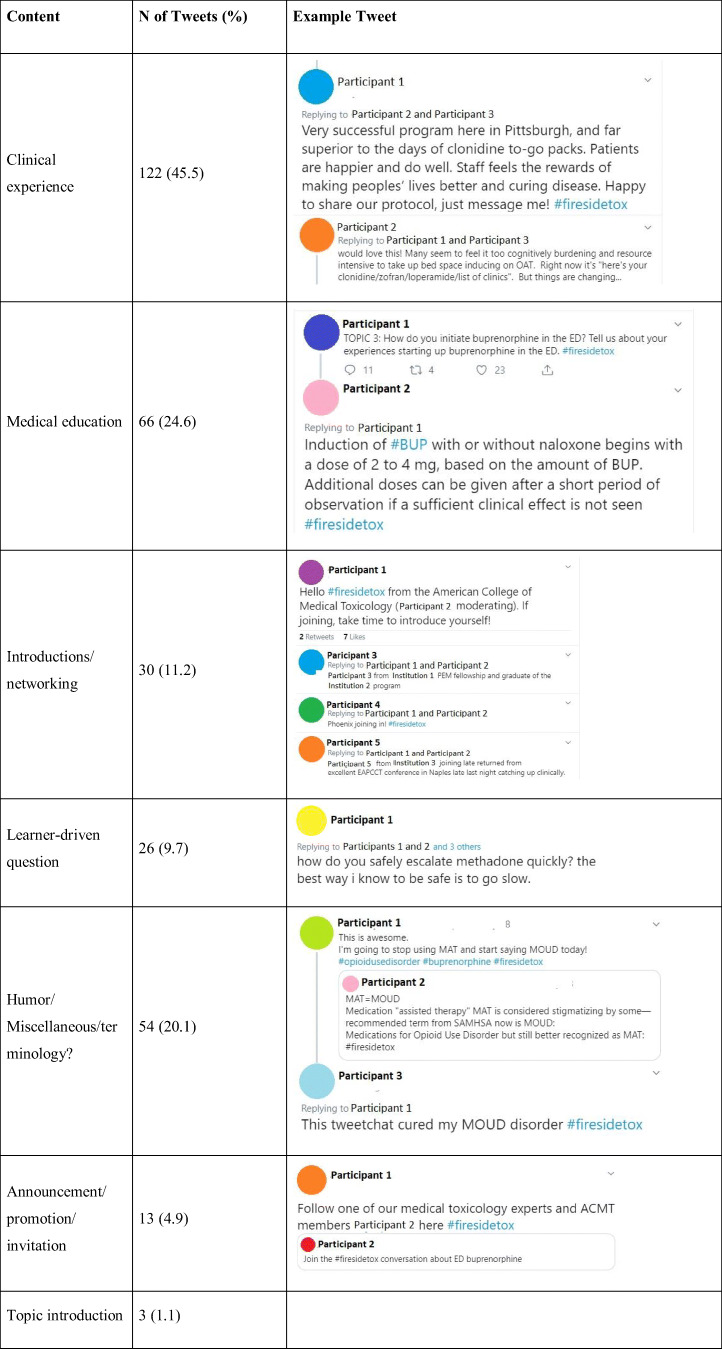
The tweetchat included 317 total tweets and generated 961,092 impressions, nearly three times the average number of impressions for the previous 6 #firesidetox tweetchats and 18% more than the largest of the six (Table 2) [4]. After excluding advertising or unrelated tweets, 268 unique tweets were included in the discussion. The majority of tweets touched on clinical experience (46%) or medical education (25%) related to buprenorphine (Table 3). This tweetchat included a higher percentage of tweets categorized as clinical experience and a smaller percentage categorized as medical education compared with previous #firesidetox tweetchats (4 and 54% respectively for all previous tweetchats). Topics formally addressed by the tweetchat were the definition of MAT, how buprenorphine fits into this definition (Topic 1, 32%), and why the ED is an important place to initiate buprenorphine (Topic 2, 14%). Additionally, the tweetchat directed discussion about implementation of ED buprenorphine, focusing on protocols and success stories (Topic 3, 13%). Other common topics discussed in the tweetchat included buprenorphine induction, the x-waiver, and buprenorphine follow-up after induction (Fig. 1).
Table 2.
Mean number of participants, tweets, and impressions for an ACMT #firesidetox tweetchat.
| Date | Topic | Number of participants | Tweets | Impressions |
|---|---|---|---|---|
| 1/12/17 | Kratom | 24 | 156 | 212,701 |
| 4/20/17 | Cannabinoid hyperemesis | 16 | 160 | 159,042 |
| 7/20/17 | Synthetic cannabinoids | 18 | 133 | 143,869 |
| 11/8/17 | Fentanyl | 27 | 166 | 315,893 |
| 1/30/18 | Role of clinical pharmacologists | 32 | 137 | 814,493 |
| Previous mean | 23.4 | 150.4 | 329,200 | |
| 5/28/19 | ED buprenorphine | 90 | 317 | 961,092 |
| Percent change from mean | 385% | 211% | 292% | |
| Mean | 34.5 | 178.2 | 434,515 |
Table 3.
Tweets by content.
Fig. 1.
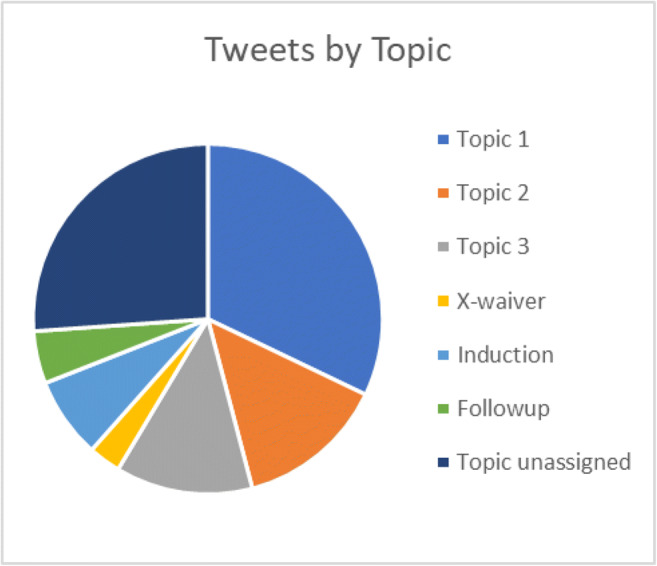
Chart demonstrating breakdown of tweets by topic. aTopic 1 pertains to the definition of medication assisted therapy (MAT) and how buprenorphine fits into this definition. bTopic 2 pertains to why the ED is an important place to initiate buprenorphine. cTopic 3 pertains to implementation of ED buprenorphine, focusing on protocols and success stories.
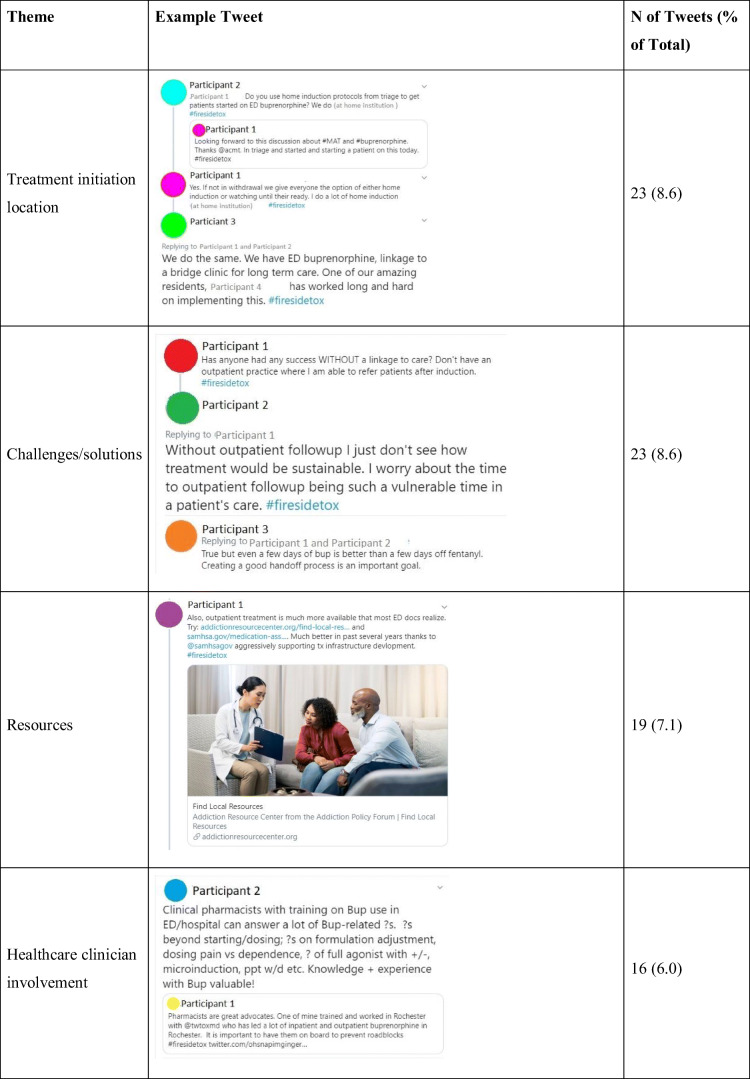
The most important two themes identified were: (1) treatment initiation location (ED vs outpatient vs home) (8.6%) and (2) challenges to buprenorphine administration and potential solutions (8.6%). Other themes included medical education resources for buprenorphine administration and clinician involvement in buprenorphine programs (Table 4). Themes often overlapped with specific tweet topics, and some tweets touched on more than one theme.
Table 4.
Themes of tweets.
Tweets pertaining to treatment location often mentioned administration of buprenorphine in the ED as compared with other locations, such as home induction or outpatient clinics. These tweets often overlapped with the “challenges” theme, as multiple participants questioned the utility of ED buprenorphine if sufficient follow-up could not be established prior to ED discharge or the concern that patients would divert or misuse the buprenorphine prescribed to them through the ED. Other participants referenced the x-waiver program as another hurdle in prescribing buprenorphine from the ED. Experts in the field offered advice and their clinical vignettes of success in ED or home induction of buprenorphine. The “resources” theme often involved participants providing links to established algorithms, literature, or apps that they use when considering ED buprenorphine induction. These resources were often shared in reply to tweets referencing challenges with ED buprenorphine induction or in response to direct questions. The final theme pertained to discussions about how other healthcare professionals could be involved in the care of OUD patients, along with toxicologists and other physicians. These discussions highlighted how pharmacists were invaluable to established ED buprenorphine programs; nurses and social workers were also mentioned.
Discussion
This investigation demonstrates that tweetchats can be used to provide a collaborative real-time forum for experts to share their knowledge of a novel treatment approach and bolster support for dissemination and implementation. We found that Twitter can be a platform to share experiences surrounding buprenorphine initiation and administrative and institutional barriers associated with buprenorphine. These shared experiences through Twitter among experienced buprenorphine providers and those who are seeking to initiate an ED buprenorphine program represent an alternative method of providing a network of informal support to ED buprenorphine access and can be used to support providers to seek to deliver MAT in the emergency department setting.
Compared with previous #firesidetox tweetchats, this tweetchat drew more participants, created more impressions, and garnered more tweets than all previous #firesidetox discussions [4]. Our tweetchat tripled the number of participants and doubled the number of tweets compared with previous #firesidetox tweetchats. We suspect that increased attention in this tweetchat may be due to partnership with other professional organizations who also endorsed the discussed position statement (i.e., the American College of Emergency Physicians) [5]. Additionally, we think the recent attention focused on ED buprenorphine in both lay and peer-reviewed literature generated interest and potential participation in the tweetchat outside of targeted recruitment. Tweetchat participation growth is likely multifactorial and may be attributed to the timeliness of the discussion topic, interest from both the healthcare and non-healthcare communities, and increased email and Twitter marketing efforts prior to this tweetchat compared with previous ACMT tweetchats.
Another distinguishing feature of this tweetchat was tweet content. Tweets included more personalized stories compared with previous ACMT tweetchats. Clinical vignettes included individual accounts of successful MAT initiatives, including “my first induction” accounts. These narratives also included specific guidance on navigating challenges to buprenorphine prescribing from the ED. Concepts of these narratives included the challenge of obtaining an x-waiver, helping patients establish follow up care for MAT, and stigma surrounding MAT. Several tweets cited specific references to published guidelines outside the ACMT position statement [7].
Overall, this study suggests that tweetchats are a novel tool to provide participants with a unique platform for discussion on timely and challenging healthcare topics. While the study did not have a defined endpoint or measurement of effectiveness, the tweetchat was effective in disseminating information on ED buprenorphine as reflected in the increased number of impressions for this tweetchat compared with prior similar chats. Similar to other social media programs, Twitter has the advantage of being open to the public due to its design as a microblogging social network. Currently, Twitter is the 7th most popular social media platform in the USA, but has distinct advantages over its competitors like Facebook, Instagram, and Snapchat in providing a platform for discussion [8]. First, Twitter allows for free-flowing discussions without requiring subscriptions to specific channels, pages, or accounts, and specific hashtags allow communities interested in specific topics to quickly find the “chatter” and contribute. The organized, real-time nature of a tweetchat allowed toxicologists, pharmacists, and physicians across the USA and the world to engage in a moderated discussion about buprenorphine programs in the ED. The real-time feature of this forum also permitted the moderator to steer discussion towards participants’ specific concerns. Importantly, the tweetchat connected leaders of nascent programs with leaders of established programs, offering resources for developing programs going forward. Finally, it created a written record of these ideas, resources, and champions which may be accessed by interested Twitter members at any future time.
This study has several limitations. First, this study was limited to participants who use Twitter, and therefore, is missing a large group of clinicians, learners, and the public in its reach. However, any forum, whether virtually-based or in-person, will exclude some relevant participants, and thus is not unique to the tweetchat. In the future, other forms of social media may be used to expand participation. Similarly, tweets were only included for analysis if they had the #firesidetox hashtag or were replies to tweets with the hashtag, which allows the possibility that some tweets and discussion threads were missed if they did not include the hashtag. Second, this discussion was intended for medical education and the medical community. There was limited participation by non-medical members, and we could not gain insight into the public’s perception and knowledge of ED buprenorphine. To better characterize the general public’s perceptions of buprenorphine, we may host a future tweetchat designed specifically to engage with the public. Additionally, characterization of participant demographics was limited to information shared in the tweetchat or on a user’s Twitter bio and was not verified, which may have led to the analysis missing important subsets of the participant population. Finally, the tweetchat analysis was related entirely to tweet content, themes, and topics. The study did not assess whether this tweetchat changed perceptions or practices among its participants. Future directions should focus primarily on post-tweetchat follow up with participants. We can consider measuring participant satisfaction with tweetchats, assessing facts retained from tweetchat data and learning if tweetchats changed participants’ medical practice.
Conclusion
In conclusion, the study results support tweetchats as a discussion forum for healthcare professionals to share their experiences and expertise on a specific topic of interest, such as buprenorphine induction in the ED, and disseminate this expertise to other healthcare professionals across the globe. By sharing successful narratives and clinical vignettes and answering questions about challenges, the tweetchat provided specific and enhanced education to participants who are interested in ED buprenorphine. The study also suggests that social media platforms contribute valuable qualitative data for better understanding perceptions about specialized topics and for rapidly disseminating relevant medical information.
Sources of Funding
PRC is funded by NIH K23DA044874, R01DA047236, Gilead Sciences, and the Hans and Mavis Lopater Psychosocial Fund. AS is funded by NIH R01DA046619.
Compliance with Ethical Standards
Conflict of Interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aslam S. Twitter by the Numbers (2019): Stats, demographics & fun facts. https://www.omnicoreagency.com/twitter-statistics/.
- 2.Topf JM, Sparks MA, Phelan PJ, Shah N, Lerma EV, Graham-Brown MPM, et al. The evolution of the journal club: from Osler to Twitter. Am J Kidney Dis. 2017;69:827–836. doi: 10.1053/j.ajkd.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 3.Roberts MJ, Perera M, Lawrentschuk N, Romanic D, Papa N, Bolton D. Globalization of continuing professional development by journal clubs via microblogging: a systematic review. J Med Internet Res. 2015;17:e103. doi: 10.2196/jmir.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chai PR, Ruha A-M, Wong KE, Monette DL, Spyres MB, Lapoint J, Greller H, Mycyk MB. The virtual toxicology journal club: the dissemination and discussion of noteworthy manuscripts using twitter. J Med Toxicol. 2018;14:212–217. doi: 10.1007/s13181-018-0670-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wax PM, Stolbach AI, Schwarz ES, Warrick BJ, Wiegand TJ, Nelson LS. ACMT position statement: buprenorphine administration in the emergency department. J Med Toxicol. 2019;15:215–216. doi: 10.1007/s13181-019-00712-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chai PR, Ranney ML, Rosen RK, Lewis DM, Boyer EW. Crowd-sourced focus groups on twitter: 140 characters of research insight. Proceedings of the 50th Hawaii International Conference on System Sciences; 2017. http://hdl.handle.net/10125/41611.
- 7.Herring AA, Perrone J, Nelson LS. Managing opioid withdrawal in the emergency department with buprenorphine. Ann Emerg Med. 2019;73:481–487. doi: 10.1016/j.annemergmed.2018.11.032. [DOI] [PubMed] [Google Scholar]
- 8.Perrin A, Anderson M. Social media usage in the U.S. in 2019. Pew Research Center 2019. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/.