Abstract
Introduction
Time is critical in the trauma setting. Emergency computed tomography (CT) scans are usually interpreted by the attending doctor and plans to manage the patient are implemented before the formal radiological report is available. This study aims to investigate the discrepancy in interpretation of emergency whole body CT scans in trauma patients by the trauma surgeon and radiologist and to determine if the difference in trauma surgeon and radiologist interpretation of emergency trauma CT scans has an impact on patient management.
Method
This prospective observational comparative study was conducted over a 6 month period (01 April–30 September 2016) at the Inkosi Albert Luthuli Central Hospital which has a level 1 trauma department. The study population comprised 62 polytrauma patients who underwent a multiphase whole body CT scans as per the trauma imaging protocol. The trauma surgeons' initial interpretation of the CT scan and radiological report were compared. All CT scans reported by the radiology registrar were reviewed by a consultant radiologist. The time from completion of the CT scan and completion of the radiological report was analysed.
Results
Since the trauma surgeon accompanied the patient to radiology and reviewed the images as soon as the scan was complete, the initial interpretation of the CT was performed within 15–30 min. The median time between the CT scan completion and reporting turnaround time was 75 (16–218) min. Critical findings were missed by the trauma surgeon in 4.8% of patients (bronchial transection, abdominal aortic intimal tear and cervical spine fracture) and non-critical/incidental findings in 41.94%. The trauma surgeon correctly detected and graded visceral injury in all cases.
Conclusion
There was no significant discrepancy in the critical findings on interpretation of whole body CT scans in polytrauma patients by the trauma surgeon and radiologist and therefore no negative impact on patient management from missed injury or misdiagnosis.
The turnaround time for the radiology report does not allow for timeous management of the trauma patient.
Keywords: CT scans, Polytrauma, Level 1 trauma centre
African relevance
-
•
Trauma remains a major disease burden in Africa and imaging modalities are becoming more available across the continent.
-
•
Resource restriction is a major concern for major trauma care in low- and middle-income countries and time is of the essence in managing the trauma patient.
-
•
There is a worldwide shortage of radiologists, particularly in Africa, thus the clinician must be proficient in assessing the available imaging for time-critical patients.
Introduction
Trauma is a leading cause of death worldwide, with a higher incidence in low- and middle-income countries than in high-income countries [1]. There are more deaths from trauma in sub-Saharan Africa than anywhere else in the world [2]. South Africa is regarded as one of the trauma capitals of the world. Almost three decades ago trauma in South Africa (SA) was likened to a malignant epidemic [3].
The overall trauma rate in the South African province of KwaZulu-Natal is 17 per 1000 population [4]. The high burden of trauma in public hospitals in KwaZulu-Natal has been analysed previously [[5], [6], [7]]. In KwaZulu-Natal pedestrian-motor vehicle collisions (PMVCs) are the commonest cause of trauma followed by interpersonal violence (IPV) namely stabs and gunshot wounds (GSW) [8].
Computed Tomography (CT) scanning is utilised as an important diagnostic tool in the assessment of trauma patients and CT scan of the head is one of the most commonly performed radiological investigations worldwide [9]. The urgent nature of trauma necessitates accuracy and speed in diagnosis and management.
Emergency CT scans are usually interpreted by the attending doctor and plans to manage the patient are implemented before the formal radiological report is available [9]. This is particularly true in the case of trauma patients where time is of the essence and the surgeon has to make a decision to operate. Furthermore, the workload of radiology departments has increased in recent years and the availability of radiologists is inadequate worldwide, particularly in developing countries [10., 11., 12.]. In 2016, there were just 913 radiologists registered with the Health Professions Council of South Africa [13]. Shortage of radiologists result in delays in imaging reporting and hence patient management [14]. This is the local scenario as several institutions with CT scanners in the province do not have radiologists or after hour radiological cover. Even when the radiologist is on site, the formal radiological report may be delayed. For example, the radiologist may be reporting other emergency CT scans or busy with an ultrasound in ICU. Hence, the emergency clinician is the primary interpreter of the emergency CT scan and makes management decisions based on his/her interpretation [15,16].
The aim of the study was to investigate the discrepancy in interpretation of emergency whole body CT scans in trauma patients by the trauma surgeon and radiologist and to determine if the difference in trauma surgeon and radiologist interpretation of emergency trauma CT scans has an impact on patient management. The degree and extent of inter-observer agreement between the radiology registrar and consultant radiologist was also investigated.
Methods
Ethics approval was obtained from the Biomedical Research Ethics Committee, College of Health Sciences, University of KwaZulu-Natal (BE488/15). This prospective cross-sectional comparative study was conducted over a 6-month period (01 April–30 September 2016) at the Inkosi Albert Luthuli Central Hospital (IALCH), an academic tertiary hospital in Durban, South Africa. IALCH has a level 1 trauma department which accepts patients directly from the scene and from any health facility throughout KwaZulu-Natal Province.
The study population comprised all acute polytrauma patients (adults and children) admitted to the trauma department who underwent multiphase whole body multidetector CT scans as per the polytrauma imaging protocol (Table 1). The CT scans were performed on the Siemens Somatom Definition AS 128 slice CT scanner or Siemens Somatom Definition Flash Dual Source CT Scanner (Siemens AG, Wittelsbacherplatz, Germany).
Table 1.
Polytrauma imaging protocol.
| Polytrauma imaging protocol |
|---|
| Unenhanced head and neck Arterial angiogram phase (utilising pre-monitoring) from base of neck to pubic symphysis - approximately 30 seconds post intravenous contrast injection Portal venous phase of the abdomen and pelvis (80 seconds post intravenous contrast injection) Additional phases tailored to case:
|
The trauma surgeons' initial interpretation of the CT scan and radiological report were compared. The trauma surgeons interpreting the scans in this study were consultant surgeons who were subspecialising or had already subspecialised in trauma. The trauma surgeons' interpretation of the CT scan abnormalities were made in clinical notes in the electronic patient record on the IALCH Hospital Information System. All CT scans were reported by the radiology registrar (minimum of 3 years of training), irrespective of the time of day, on the IALCH Radiology Information System.
The trauma surgeon telephonically requests the CT scan from the radiology registrar and thereafter liaises directly with the radiographers. There is no further communication with the radiology registrar until the formal report is issued. This has been the standard operating procedure at IALCH owing to a historic shortage of staff when radiology registrars were not on site and were on call at multiple hospitals simultaneously until the last few years. Furthermore, the radiology registrar is usually in the main radiology reporting suite at the opposite end of the department. He or she may also be busy with ultrasounds or fluoroscopy. The trauma surgeon accompanies the patient to the CT scanner and reviews the images as soon as the scan is complete, usually on the workstation in the CT scan department. An urgent clinical management decision is usually made, the trauma surgeon then returns to the trauma department with the patient. There is no communication with the radiologist until the radiology report is issued.
The scan was reviewed by a consultant radiologist (minimum of 5 years of experience) on the same day if performed during normal working hours or the next working day if performed after hours. The consultant radiologist report was the gold standard. If any errors were detected by the consultant radiologist in the report issued by the registrar, the clinician was informed and the report amended. The radiology registrars interpreting the CT scans were in the penultimate or final year of training and considered senior. Patient management and outcome was accessed from the clinical notes in the electronic patient record on the IALCH Hospital Information System. The time from completion of the CT scan and completion of the radiological report was also analysed.
After compiling the data, statistical analyses were performed using SPSS (SPSS version 21.0, IBM, Chicago, Illinois). By considering the trauma surgeon's report and consultant radiologist report as the gold standard, inter-rater reliability was assessed by calculating sensitivity, positive predictive value (PPV), concordance rate and accuracy. A p-value of <0.05 and 95% confidence intervals were used to indicate the statistical significance and prevision of the estimates.
Results
Multiphase whole body CT scans were performed on a total of 69 patients. Seven patients were excluded owing to missing/incomplete data and suboptimal CT scan images (motion artefact/incorrect contrast enhancement phase).
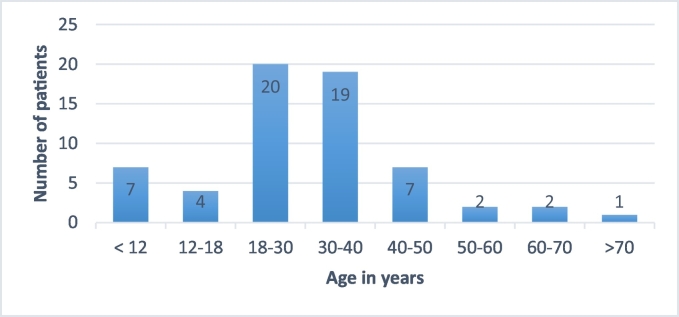
Of the 62 patients, 12 were female and 50 were males. The majority of patients were in the 18–30-year age group (Fig. 1).
Fig. 1.
Patient age and number.
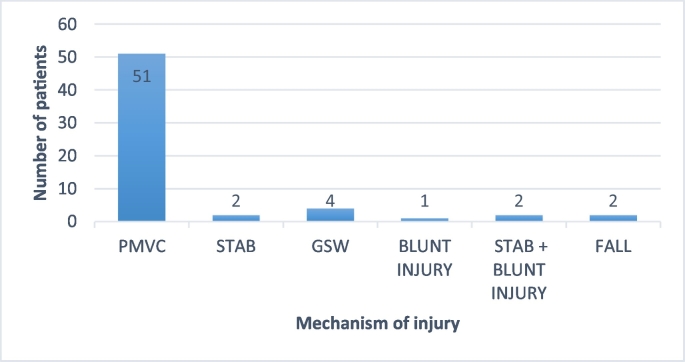
Considering the mechanisms of trauma, the majority were caused by PMVC. This comprised 20 (32.26%) patients involved in motor vehicle collisions (including 3 motorbike accidents) and 31 (50.00%) pedestrians struck by vehicles (Fig. 2). Other mechanisms of injury accounted for 17.74% of the total.
Fig. 2.
Mechanism of injury.
There were no normal CT scans. The trauma surgeon correctly identified all critical findings in 59 of 62 cases (95.16%) compared to the consultant radiologist as the gold standard. Visceral injury was correctly identified and graded in all cases as per American Association for the Surgery of Trauma (AAST) criteria. Sensitivity was 95.38% (95%CI 87.10–99.04) and PPV 100%. Concordance analysis revealed a concordance rate of 95.38% (95% CI 87.10–99.04%) between the trauma surgeon and radiologist. Percentage agreement was 95.16% (95% CI 89.82–100.50%).
Critical findings were missed by the trauma surgeon in 3 (4.84%) patients (left mainstem bronchial transection, abdominal aortic intimal tear and cervical spine fracture). This discrepancy was not statistically significant at p < 0.05 but are of clinical significance. Missed injuries, whether serious or minor, may not always contribute to the patient's clinical course and outcome, as with the patients in our study. However, missed critical findings are potentially clinically significant factors for patient morbidity and mortality, if not acted upon in survivors.
The patients with missed critical findings (bronchial transection and aortic intimal tear) demised a few hours after admission as they had multiple other severe injuries and were haemodynamically unstable. The patient with the aortic intimal tear was a 23 year old male motorbike crash victim. He sustained a profunda femoris artery injury, grade 5 splenic injury, grade 3 pancreatic injury, bilateral haemopneumothoraces, vertebral and rib fractures. The patient with the bronchial transection sustained multiple gunshot wounds and predominantly sustained chest trauma with bilateral haemopneumothoraces, pulmonary contusions, rib and thoracic spine fractures. The outcome or patient management would not have altered had the findings been picked up by the trauma surgeon, as the intimal tear would have had endovascular management only once the patient was stable. The patient with the bronchial transection had chest tubes in situ and died prior to any opportunity for thoracotomy. With regards to the missed cervical spine fracture by the trauma surgeon, no adverse outcome was noted as the patient was in a neck collar, the fracture was stable and the radiology report was issued within an hour. The patient was down-referred after 10 nights in hospital following surgery for long bone fractures.
Non-critical/incidental findings were missed or not mentioned by the trauma surgeon in 26 (41.94%) out of the 62 patients. These findings are described in Table 2. Percentage agreement in the interpretation of non-critical/incidental findings was 58.06% (95% CI 44.85–70.49%) between the trauma surgeon and radiologist. Although this discrepancy was significant at p < 0.05, there was no impact on the timeous management of the patient nor did this affect patient outcome.
Table 2.
Non critical or incidental findings missed or omitted by the trauma surgeon.
| Non critical/incidental findings |
|---|
| Surgical emphysema in 7 patients |
| Soft tissue haematomas in 4 patients |
| Full extent of facial bone fractures in 3 patients |
| Bifid cervical spinous process |
| Limbus vertebra of cervical spine |
| Aspiration in 5 patients |
| Fibrocavitatory changes in apex |
| Tuberculosis |
| Focal fatty infiltration of liver |
| Renal cyst |
| Adrenal incidentaloma |
Incidental findings reported by the trauma surgeon were blood within the stomach, bladder schistosomiasis and neurocysticercosis.
Two critical findings (3.23%) were missed by the radiology registrar. This discrepancy was not significant at p < 0.05. These were a subarachnoid haemorrhage and coeliac axis thrombus in another patient. The trauma surgeon had correctly identified these injuries and there was no negative impact on patient care.
Of the 62 polytrauma patients:
-
•
head injuries were identified in 29, which necessitated urgent neurosurgical referral
-
•
vascular injuries were noted in 7
-
•
vascular and neurosurgical injuries were identified in 3
-
•
14 demised
Since the trauma surgeon accompanied the patient to radiology and viewed the images as soon as the scan was complete, (often at the workstation in radiology) the initial interpretation of the CT was performed within 15–30 min. The median time between the CT scan completion and reporting turnaround time was 75 (16–218) min.
Discussion
The trauma surgeon's interpretation of a CT scan where time is of the essence is important; given the high trauma burden and scarcity of radiologists in Africa. To our knowledge, there has been no study comparing the evaluation of CT scans between radiologists and non-radiologists in South Africa. There have also been only a few studies internationally comparing the interpretation of body CT scans between surgeons and radiologists.
Studies have examined emergency physicians' skills in reading different radiologic studies. The majority of these studies have focused on plain X-rays and a few on CT brain scan interpretation by attending emergency physicians [17]. Discrepancy rates in radiograph interpretation of emergency physicians versus radiologists has been reported to be between 0.95% and 16.8% in different studies [18,19]. A significant discrepancy rate of 13.05% in the evaluation of trauma x rays (cervical spine, chest and pelvis) between on duty surgeons in the emergency room and radiologists was reported by Nasr et al. [20].
In 1995, Alfaro et al. reported a 38.7% non-concordance between EP and radiologists with potentially significant misinterpretations in 24.1% of cranial CT scans [15]. Since the advent of MDCT and availability of 3D multiplanar reformats, this has reduced. Studies have concluded that senior general surgical residents can accurately interpret trauma radiographs and CT brain [21]. There has been a study evaluating surgical resident interpretation of CT head, chest, abdomen and pelvis in acute injury. The surgical resident was accurate in 96% of CT head interpretation, 67% CT chest and 94% CT abdomen and pelvis [22].
This study demonstrates that the trauma surgeon can identify the majority of critical findings on an emergency polytrauma CT scan with a discrepancy rate of 4.84%. Although this discrepancy was clinically but not statistically significant, the outcome or patient management would not have altered had the findings been picked up by the trauma surgeon. Studies show that more injuries are clinically and radiologically missed in polytrauma patients. Patients with head injury, a Glasgow Coma Scale score of eight or lower and a high Injury Severity Score are more likely to have missed injuries or delayed diagnoses [23,24]. In a retrospective study of more than 2000 patients, Banaste et al. identified factors leading to missed injury in whole body CT in patients with multiple trauma [25]. More than two injured body parts, age older than 30 years, or an initial clinical severity class of 1 were associated with missed injury at whole body CT.
A study at a level two trauma centre revealed overall moderate agreement between radiologists and surgical residents' interpretation of CT scans of the head, facial bones, cervical spine, thoracic spine, lumbar spine, chest, abdomen and pelvis as well as chest and abdominal radiographs. Interestingly, maxillofacial CT scans had a 50% accuracy. No change in patient outcome or management was required [26].
The overall agreement between the trauma surgeon and consultant radiologist for the non-critical/incidental findings was 58.06% which is comparable to other studies. It is not known whether the trauma surgeon observed the surgical emphysema, aspiration and soft tissue haematomas but omitted documentation as this would not impact on immediate patient management. Furthermore, radiologists report all normal variants (bifid cervical spinous, process, limbus vertebra) and incidental findings (focal fatty infiltration of the liver, renal cyst, adrenal incidentaloma). The non-critical incidental findings had no impact on the emergency management of the trauma patient. The full description of facial bone fractures, tuberculosis and fibrocavitatory disease would have been available in the radiology report within a few hours and the patient managed accordingly, if required. Patient outcome was not adversely affected by the trauma surgeons' missing non-critical/incidental findings.
Wong et al. found a low error rate in surgical resident interpretation of after hour CT scans of the head and abdomen in trauma with no impact on patient management or outcome [9]. This was in line with our study. The trauma surgeons interpreting the scans in this study were consultant surgeons who were subspecialising or had already subspecialised in trauma hence the low discrepancy rate. Furthermore, they had the benefit of having evaluated the patient clinically prior to the CT scan.
This study revealed a 3.23% discrepancy between the radiology registrar and consultant radiologist for critical findings. Fortunately these (subarachnoid haemorrhage and coeliac axis thrombus) were identified by the trauma surgeon with no negative impact on patient management. Discrepancy rates in radiology resident interpretation of emergency CT scans (non-traumatic and traumatic) vary from 0.9 to 25.9% [[27], [28], [29], [30], [31]]. For body CT evaluation, there was a 5.4% rate of minor discrepancies and a 1.0% rate of major discrepancies between radiology registrar and consultant body imaging radiologist at a level 1 trauma centre [32]. Another study found a 2% discrepancy rate between radiology residents and radiologists in torso CT at a level 1 trauma centre [33]. A 2.0% overall rate of clinically significant discrepancies (those that would potentially alter the patient's clinical course prior to issue of the final report) was reported by Walls et al. [34]. The major discrepancy rates for abdominal/pelvic, chest, cervical spine and head CT were 4.1%, 2.5%, 1.0% and 0.7%, respectively. Polytrauma CT scan reporting after hours by radiology registrars is safe [27]. This consistent with the findings in our study.
The median time between the CT scan completion and reporting turnaround time at IALCH was 75 (16–218) min. In a level 1 trauma department at a South African hospital in another province, the median report turnaround time for trauma CT scans was 86 (53–146) min [35]. Our findings are fairly similar.
The sample size was a limitation to the study. The Hawthorne effect was a further limitation but was minimised as the majority of the trauma surgeons and radiologists were unaware of the methods of evaluation and details of the study. Another limitation was that the patient outcome was restricted to the inpatient at IALCH and further longitudinal follow-up was not possible. However, most patients had a 5–10 day stay and most occult injuries would have been revealed in this timeframe.
Conclusion
In the current study, there was no significant discrepancy in the critical findings on interpretation of whole body CT scans in polytrauma patients by the trauma surgeon and radiologist and therefore no negative impact on patient management from missed injury or misdiagnosis. Although a significant discrepancy exists in the interpretation of non-critical findings, this also did not impact patient outcome. The turnaround time for the formal radiology report does not allow for timeous management of the trauma patient.
Dissemination of results
The initial results were presented at the Cape Town Trauma Congress in November 2017.
Authors' contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: PP contributed 85% and TCH contributed 15%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
Prof Tim Hardcastle is an editor of the African Journal of Emergency Medicine. Prof Hardcastle was not involved in the editorial workflow for this manuscript. The African Journal of Emergency Medicine applies a double blinded process for all manuscript peer reviews. The authors declared no further conflict of interest.
References
- 1.Peden M., McGee K., Krug E. World Health Organization; Geneva: 2002. Injury – a leading cause of the global burden of disease 2000. [Google Scholar]
- 2.Bowley D.M., Khavandi A., Boffard K.D. The malignant epidemic-changing patterns of trauma. S Afr Med J. 2002;92:798–802. [PubMed] [Google Scholar]
- 3.Muckart D.J. Trauma – the malignant epidemic. S Afr Med J. 1991;79(2):93–95. [PubMed] [Google Scholar]
- 4.Lutge E., Moodley N., Tefara A., Sartorius B., Hardcastle T., Clark D. A hospital based surveillance system to access the burden of trauma in KwaZulu-Natal Province South Africa. Injury. 2015 Aug 21 doi: 10.1016/j.injury.2015.08.020. (pii: S0020-1383(15)00495-7) [DOI] [PubMed] [Google Scholar]
- 5.Hardcastle T., Samuels C., Muckart D. An assessment of the hospital disease burden and the facilities for the in-hospital care of trauma in KwaZulu-Natal, South Africa. World J Surg. 2013;37(7):1550–1561. doi: 10.1007/s00268-012-1889-1. [DOI] [PubMed] [Google Scholar]
- 6.Parkinson F., Kent S., Aldous C. Road traffic crashes in South Africa: the burden of injury to a regional trauma centre. S Afr Med J. 2013;103(11):850–852. doi: 10.7196/samj.6914. [DOI] [PubMed] [Google Scholar]
- 7.Laing G., Skinner D., Bruce J. Understanding the burden and outcome of trauma care drives a new trauma systems model. World J Surg. 2014;38(7):1699–1706. doi: 10.1007/s00268-014-2448-8. [DOI] [PubMed] [Google Scholar]
- 8.Lewis C., Wood D. Interpersonal violence as a major contributor towards the skewed burden of trauma in KwaZulu-Natal, South Africa. S Afr Med J. 2015;105(10):827–830. doi: 10.7196/SAMJnew.8380. [DOI] [PubMed] [Google Scholar]
- 9.Wong C., Taubman K., Hoehne F., Malholtra S., Naidu M., Parent D. The quality of surgical resident interpretation of after-hour CT scans of the head and abdomen in trauma. Am Surg. 2005;71(9):772–775. (PMID 16468516) [PubMed] [Google Scholar]
- 10.Diagnostic imaging. Radiologist sightings drop around the world. 14 July 2003. https://www.diagnosticimaging.com/article/radiologist-sightings-drop-around-world/ [Online]. Available from: [Accessed 8th July 2018]
- 11.Webber A. Shortage of radiologists could lead to service collapse. 23 Aug 2018. https://www.personneltoday.com/hr/radiologist-shortage-make-service-collapse/ [Online]. Available from:
- 12.Greene W. Philippine startup takes on global radiologist shortage. 8 Nov 2014. https://www.forbes.com/sites/techonomy/2014/11/08/philippine-startup-takes-on-global-radiologist-shortage/#174ea3e31235 [Online]. Available from.
- 13.Section 27. Radiologists ask panel for help on pricing. 5 May 2016. https://section27.org.za/2016/05/radiologists-ask-panel-for-help-on-pricing/ Available from: [Accessed 8th July 2018]
- 14.BBC.com Delays in radiology results affecting patient care. 19 July 2018. https://www.bbc.com/news/health-44871476?intlink_from_url=https://www.bbc.com/news/topics/cmw2w95pz95t/radiology&link_location=live-reporting-story/ [Online]. Available from: [Accessed 8th July 2018]
- 15.Alfaro D., Levitt M.A., English D.K., Williams V., Eisenberg R. Accuracy of interpretation of cranial computed tomography scans in an emergency medicine residency program. Ann Emerg Med. 1995;25(2):169–174. doi: 10.1016/S0196-0644(95)70319-5. [DOI] [PubMed] [Google Scholar]
- 16.Al-Reesi A., Stiell I.G., Al-Zadjali N., Cwinn A.A. Comparison of CT head interpretation between emergency physicians and neuroradiologists. Eur J Emerg Med. 2010;17(5):280–282. doi: 10.1097/MEJ.0b013e32833483ed. [DOI] [PubMed] [Google Scholar]
- 17.Dolatabadi A.A., Baratloo A., Rouhipour A., Abdalvand A., Hatamabadi H., Forouzanfar M. Interpretation of computed tomography of the head: emergency physicians versus radiologists. Trauma Monthly. 2013;18(2):86–89. doi: 10.5812/traumamon.12023. doi:10.5812%2Ftraumamon.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minnes B.G., Sutcliffe T., Klassen T.P. Agreement in the interpretation of extremity radiographs of injured children and adolescents. Acad Emerg Med. 1995;2(9):826–830. doi: 10.1111/j.1553-2712.1995.tb03279.x. [DOI] [PubMed] [Google Scholar]
- 19.Nolan T.M., Oberklaid F., Boldt D. Radiological services in a hospital emergency department--an evaluation of service delivery and radiograph interpretation. Aust Paediatr J. 1984;20(2):109–112. doi: 10.1111/j.1440-1754.1984.tb00055.x. 6466225. [DOI] [PubMed] [Google Scholar]
- 20.Nasr A., Nakano I.T., Rigolini A.V.B., Kato G.M.P., de Abreu Reis P.G.T. Radiologist vs surgeon: misdiagnoses in radiologic evaluation by on-duty surgeons in the emergency room. Panam J Trauma Critical Care Emerg Surg. 2012;1(1):38–43. doi: 10.5005/jp-journals-10030-1009. [DOI] [Google Scholar]
- 21.Vorhies R.W., Harrison P.B., Smith R.S., Helmer S.D. Senior surgical residents can accurately interpret trauma radiographs. Am Surg. 2002 Mar;68(3):221–225. 11893098 [PubMed] [Google Scholar]
- 22.Arentz C., Griswold J.A., Halldorsson A., Quattromani F., Dissanaike S. Best poster award: accuracy of surgery residents’ interpretation of computed tomography scans in trauma. Am J Surg. 2008;196:809–812. doi: 10.1016/j.amjsurg.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Pfeifer R., Pape H.C. Missed injuries in trauma patients: a literature review. Patient Safety in Surgery. 2008;2(20) doi: 10.1186/1754-9493-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hardcastle T.C. Missed injury: decreasing morbidity and mortality. A literature review. S Afr J Surg. 2011;49:199–201. [PubMed] [Google Scholar]
- 25.Banaste N., Caurier B., Bratan F., Bergerot J.F., Thomson V., Millet I. Whole-body CT in patients with multiple traumas: factors leading to missed injury. Radiology. 2018 Nov;289(2):374–383. doi: 10.1148/radiol.2018180492. [DOI] [PubMed] [Google Scholar]
- 26.Fakhoury E., Abolghasemi D., McKinney J., Naumova A., Wessner S. Surgical residents’ interpretation of diagnostic radiologic imaging in the traumatically injured patient. J trauma Acute Care Surg. 2018 Jan;84(1):146–149. doi: 10.1097/TA.0000000000001701. [DOI] [PubMed] [Google Scholar]
- 27.Briggs R.H., Rowbotham E., Johnstone A.L., Chalmers A.G. Provisional reporting of polytrauma CT by on-call radiology registrars. Is it Safe? Clinl Rad. 2010;65(8):616–622. doi: 10.1016/j.crad.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Miyakoshi A., Nguyen Q.T., Cohen W.A., Talner L.B., Anzai Y. Accuracy of preliminary interpretation of neurologic CT examinations by on-call radiology residents and assessment of patient outcomes at a level I trauma center. J Am Coll Radiol. 2009;6:864–870. doi: 10.1016/j.jacr.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 29.Lal N.R., Murray U.M., Eldevik O.P., Desmond J.S. Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. AJNR Am J Neuroradiol. 2000;21(1):124–129. doi: 10.1148/radiol.2493071543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Terreblanche O.D., Andronikou S., Hlabangana L.T. Should registrars be reporting after-hours CT scans? A calculation of error rate and the influencing factors in South Africa. Acta Radiol. 2012;53:61–68. doi: 10.1258/ar.2011.110103. [DOI] [PubMed] [Google Scholar]
- 31.De Witt J.F., Griffith-Richards S., Pitcher R.D. The accuracy of after-hour registrar computed tomography (CT) reporting in a South African tertiary teaching hospital. S Afr J Rad. 2014;18(1) doi: 10.4102/sajr.v18i1.591. Art. #591, 3 pages. [DOI] [Google Scholar]
- 32.Carney E., Kempf J., DeCarvalho V., Yudd A., Nosher J. Preliminary interpretations of after-hours CT and sonography by radiology residents versus final interpretations by body imaging radiologists at a level 1 trauma center. AJR. 2003;181:367–373. doi: 10.2214/ajr.181.2.1810367. [DOI] [PubMed] [Google Scholar]
- 33.Chung J.H., Strigel R.M., Chew A.R., Albrecht E., Gunn M.L. Overnight resident interpretation of torso CT at a level 1 trauma center an analysis and review of the literature. Acad Radiol. 2009 Sep;16(9):1155–1160. doi: 10.1016/j.acra.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 34.Walls J., Hunter N., Brasher P.M., Ho S.G. The DePICTORS Study: discrepancies in preliminary interpretation of CT scans between on-call residents and staff. Emerg Radiol. 2009 Jul;16(4):303–308. doi: 10.1007/s10140-009-0795-9. [DOI] [PubMed] [Google Scholar]
- 35.Tiemesmann T., Raubenheimer J., de Vries C. Temporal evaluation of computed tomographic scans at a Level 1 trauma department in a central South African hospital. S Afr J Rad. 2016;20(1) doi: 10.4102/sajr.v20i1.836. Art. #836, 5 pages. [DOI] [Google Scholar]