Abstract
Introduction
Pneumatic weapons rarely cause severe trauma. However, pellet embolisation can cause severe and unexpected injuries.
Report
This is the case study of a 32 year old man, who was shot in the chest with a pneumatic rifle. Initially, urgent damage control surgery was performed to resolve pneumothorax and pericardial tamponade, but no projectile was found. Subsequent atypical symptomatology led to more extensive imaging that found a pellet embolised into the right carotid artery, thrombosis of the middle cerebral artery, and development of a large right hemispheric ischaemic area. After an unsuccessful endovascular intervention, the projectile was removed during an open surgical procedure. The right hemisphere oedema required decompressive hemicraniectomy, but long term intensive care and physiotherapy resulted in a satisfactory recovery with moderate neurological sequelae.
Conclusion
An unusual clinical presentation in combination with an absent exit wound might be symptomatic of projectile embolisation and should lead to a search for it. When the projectile position is convenient, surgical removal is the treatment of choice while an endovascular approach should be reserved for inaccessible locations or asymptomatic cases.
Keywords: Bullet embolisation, Decompressive craniectomy, Firearm injury, Stroke
Highlights
-
•
Projectile embolisation can lead to severe and unexpected pathologies.
-
•
Unusual clinical signs and an absent exit wound are suspicious of embolisation.
-
•
For symptomatic emboli, urgent projectile removal is necessary.
-
•
Surgical rather than endovascular removal is preferred for symptomatic emboli.
Introduction
Although pneumatic pistols and rifles may seem quite harmless, they are potentially lethal weapons. Compressed air (or another gas) propels 4.5 or 5.5 mm pellets. According to experimental studies, pellets must reach a speed of 38–70 m/sec to penetrate human skin. Nowadays, most pneumatic guns exceed this speed and some of them have a projectile speed comparable to conventional firearms. Children and young adults are injured most frequently, and the eye and the brain are among the most common serious impact locations.1
The exact incidence of projectile embolisation is not known. It has been estimated that 0.3% of penetrating gunshot injuries in the Vietnam War and 1.1% of those during the Afghanistan and Iraq conflicts led to embolisation. This proportion is probably higher in the civilian setting because of the lower projectile speed and energy.2 In 70% of cases, the bullet penetrates the arterial system through the thoracic or abdominal aorta or directly through the heart, even though embolisation from peripheral arteries has also been described.3
In this case, a pellet from a pneumatic rifle entered the left ventricle, travelled into the right internal carotid artery and caused an ischaemic stroke. The urgent development of the injury – cardiac tamponade and tension pneumothorax – caused diagnostic and therapeutic uncertainty, which will be further presented and discussed.
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
Case report
A 32 year old man shot himself in his own left hemithorax with a pneumatic rifle at 18:15 (T0). Pre-hospital, he was intubated and mechanically ventilated because of respiratory failure. After consultation with a high level emergency department, the patient was brought directly to the operating theatre at 19:30 (T0 + 75 min).
On admission, physical examination revealed reduced ventilation on the left side, SpO2 98%, heart rate of 115/min, and non-invasive blood pressure of 125/75 mmHg without vasopressor support. There was a small non-bleeding wound 5 cm below the centre of the left clavicle as the only indication of trauma. Neurological examination was limited by sedation. Under general anaesthesia with single lung ventilation, the entry point was examined via a left anterolateral thoracotomy. Besides the lung penetration, complicated by haemothorax (1000 mL), a pericardial wound with left ventricular penetration was revealed. However, no pellet was found.
At the end of the surgery (23:30; T0 + 5 hours 15 min), a chest Xray failed to localise the pellet. The patient did not regain consciousness and the pupils became slightly unequal. Computed tomography (CT) angiography of the head and neck showed the pellet in the lumen of the right internal carotid artery (ICA) 2 cm above the bifurcation (at the C2/3 level) with a distal filling defect and developing ischaemia in the middle cerebral artery territory (Fig. 1).
Figure 1.
Computed tomography angiogram of the head and neck obtained five hours after the injury. The image shows a pellet wedged in the lumen of the right internal carotid artery approximately 2 cm above the bifurcation (at the C2/C3 level), and a filling defect in the right middle cerebral and right internal carotid arteries distal to the pellet (right).
After consultation with a vascular surgeon, an interventional radiologist and a neurologist, endovascular pellet extraction and thrombo-aspiration was chosen. Despite repeated attempts, the procedure was unsuccessful, the pellet moved cranially and still obstructed the ICA (Fig. 2). Therefore, open surgery was performed at 02:30 (T0 + 8 hours 15 min), in which the right ICA was incised and the pellet and adjacent thrombus were extracted using a balloon (Fogarty) catheter.
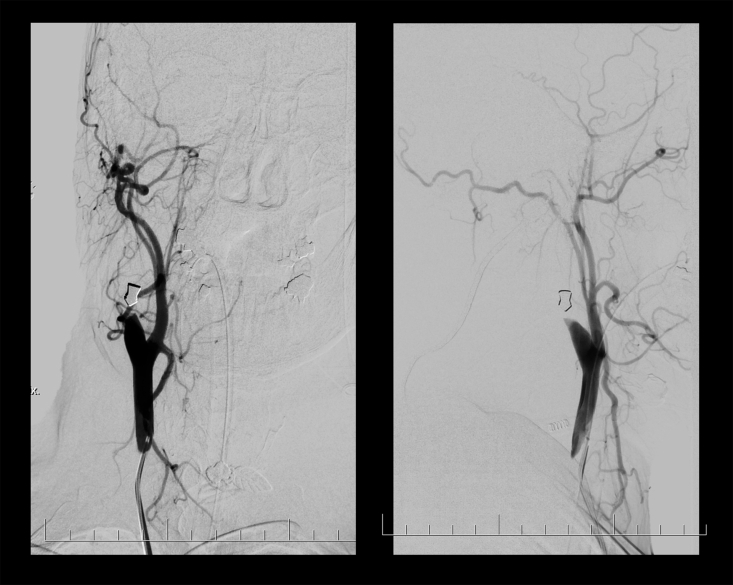
Figure 2.
Angiography of the neck and head. Anteroposterior (left) and lateral (right) views showing the pellet in the right internal carotid artery approximately 2 cm above the bifurcation. The internal carotid artery is completely occluded, only external carotid artery branches are displayed.
On the next day (Day 1; 9 hours after recanalisation), brain CT revealed ischaemia of most of the right hemisphere without bleeding or midline shift. Sedation was ceased and the patient regained consciousness with a left sided hemiplegia. However, an altered level of consciousness and unequal pupils were observed on Day 2. A repeat head CT showed a significant mass effect of the infarction with a midline shift of 11 mm, which was urgently treated by a right decompressive hemicraniectomy. Subsequent weaning was complicated by agitation, left sided hemiplegia and hemispatial neglect, but there was a gradual improvement of consciousness and left sided weakness.
On discharge from a rehabilitation facility, the patient had no alteration of consciousness and was able to lift the upper extremity with flexion and extension in the elbow, but distal mobility was absent. There was only mild paresis of the left lower limb and he was able to walk.
Discussion
This case report describes the management of a patient who suffered from pellet embolisation into the right internal carotid artery with serious consequences. Because only early carotid artery recanalisation could have reduced the neurological damage, there are two major issues: firstly, could the pellet embolisation have been diagnosed earlier, and secondly was the choice of treatment correct?
Regarding the timing of the pellet search, the initial neurological examination at the scene was limited by the necessity to manage cardiorespiratory instability. Later, in the operating theatre, the sedated and paralysed patient offered only minimal opportunities for performing a neurological assessment. Urgent damage control surgery had the highest priority and imaging (CT, Xray) would have caused a potentially hazardous delay. Suspicion of pellet embolisation emerged during surgery, but a chest Xray did not reveal the pellet's location. The cranial part of the operating table is radiopaque, which limited extending the imaging to the head and neck. The delayed return of consciousness with focal neurological signs led to the subsequent head CT, which located the pellet and detected the cerebral ischaemia.
The chosen therapeutic approach is more controversial. There is strong agreement that a symptomatic embolus must be removed. In this case, the choice of endovascular retrieval was probably a mistake. Although endovascular procedures have a moderate success rate of 63%,4 they are typically used for retrieval of asymptomatic projectiles, emboli from the pulmonary circulation or surgically inaccessible locations. Surgical extraction should have been chosen in this case because the pellet's position was convenient and could have led to faster recanalisation. Theoretically, a more extensive search for the pellet in the operating theatre using the Xray with urgent surgical removal (expected recanalisation at T0 + 6 hours) might have improved the neurological outcome compared with recanalisation at 8 hours 30 min as described in this case. A hybrid operating room would have been the ideal setting for managing this patient.
In a recent systematic review, emboli in the left sided circulation were often described as symptomatic and manifested by local tissue ischaemia.4 Hence, urgent embolus removal is necessary. Pellet migration during the retrieval attempt, which happened during endovascular extraction in this case, has been described in 9% of all cases. The entry point in this case was typical, the left heart, which together with the aorta followed by carotid arteries are the most common.3,4 The most frequent destinations are the pelvic and lower limb arteries followed by the middle cerebral and carotid artery. Cerebral embolisation also prevails on the right side (74% vs. 26%).4
On the other hand, venous and pulmonary circulation emboli are often asymptomatic, and a conservative approach is a reasonable alternative to endovascular or surgical removal. For a lead projectile, lead poisoning (plumbism) as a result of a retained projectile has been described in several cases, but the real risk of this phenomenon has not been determined clearly.5 When a projectile is located in the soft tissue, the risk of lead poisoning seems low and a conservative approach with follow up monitoring of lead toxicity is reasonable.6
Conclusion
Projectile embolisation is a rare but potentially serious complication of a gunshot injury. In a patient with a missing exit wound, it may manifest with unusual symptoms that do not correspond to the mechanism and localisation of the injury. All patients suspected of a symptomatic embolus must undergo a search for the projectile, and when positive it should be removed immediately to minimise ischaemic damage. Conversely, asymptomatic emboli do not always require aggressive management.
Conflicts of interest
None.
Funding
This work was supported by the Ministry of Education, Youth and Sports of the Czech Republic (LQ1605, NPU II).
Acknowledgements
The authors would like thank to Dr. M. Pavlík (intensivist), Dr. V. Weiss (neurologist), Dr. Z. Konečný (vascular surgeon), Dr. I. Suskevic (intervention radiologist), Dr. M. Reška (general surgeon), and Dr. R. Jančálek (neurosurgeon), who worked up the diagnostic and therapeutic plans in both the initial and later phases of the patient's treatment and provided valuable medical advice during the writing of this manuscript.
References
- 1.Ceylan H., McGowan A., Stringer M.D. Air weapon injuries: a serious and persistent problem. Arch Dis Child. 2002;86:234–235. doi: 10.1136/adc.86.4.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nolan T., Phan H., Hardy A.H., Khanna P., Dong P. Bullet embolization: multidisciplinary approach by interventional radiology and surgery. Semin Intervent Radiol. 2012;29:192–196. doi: 10.1055/s-0032-1326928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biswas S., Cadot H., Abrol S. Gunshot wound of the thoracic aorta with right popliteal artery embolization: a case report of bullet embolism with review of relevant literature. Case Rep Emerg Med. 2013;2013:198617. doi: 10.1155/2013/198617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuo A.H., Gregorat A.E., Restrepo C.S., Vinu-Nair S. Systematic review of civilian intravascular ballistic embolism reports during the last 30 years. J Vasc Surg. 2019;70:298–306. doi: 10.1016/j.jvs.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Rheinboldt M., Francis K. Systemic plumbism following remote ballistic injury. Emerg Radiol. 2014;21:423–426. doi: 10.1007/s10140-014-1207-3. [DOI] [PubMed] [Google Scholar]
- 6.Kollig E., Hentsch S., Willms A., Bieler D., Franke A. Gunshot wounds: should projectiles and fragments always be removed? Chirurg. 2014;85:607–615. doi: 10.1007/s00104-013-2643-4. [DOI] [PubMed] [Google Scholar]