Abstract
Background: In June–July 2008 a non-governmental organization (NGO) in Jalalpur Jattan (JPJ), Gujrat, Pakistan arranged two voluntary HIV screening camps after numerous HIV-infected persons reported to their treatment center in Lahore; 88 (35.8%) of 246 persons screened in those camps were positive by rapid test. Intense media coverage made the residents of JPJ hostile to further inquiries. The Pakistan Field Epidemiology Training and Laboratory Training Program (FELTP) was requested by the Provincial AIDS Control Program to carry out an epidemiological investigation.
Methods: HIV-positive persons or family members of patients who died of AIDS and consented to be interviewed during the period 15 December 2008 to 2 January 2009 were investigated. Enhanced contact tracing was done to identify additional cases. A structured questionnaire was used to collect data regarding clinical history, risk factors, and HIV knowledge and practices. The national HIV/STI Referral Laboratory collected blood samples for HIV serology and molecular studies independently following pre- and post-counseling.
Results: A total of 53 HIV-infected persons were investigated. Out of these, 47 (88.7%) were alive at the time of investigation and 27 (50.9%) of the cases were female with 6 children aged 10 years or less. Median age was 35 years (mean 34.7, range 3–70). Most frequent symptoms were unexplained fever 42 (79.2%), diarrhea 34 (64.15%) and skin infections 27 (50.9%); 13 (24.5%) had co-infection with tuberculosis (TB) and 10 (18.9%) with hepatitis (B or C). Use of injections 51 (96.2%), dental procedures 21 (40%) and barber shop visits among males 18 (72%) were common risk factors. Extramarital sex was reported by 4 (9.4%). Only 19 (35.8%) were aware that HIV can be sexually transmitted and 18 (34%) were aware of HIV transmission by blood transfusion. Phylogenetic analysis revealed HIV infection in this group was HIV-1 Subtype A, transmitted over a decade, and the situation is endemic rather than an outbreak.
Conclusion: The investigation indicates high rates of HIV infection in JPJ. Unlike other studies from Pakistan, a high proportion of cases in females and children less than 10 years of age were observed. Socio-cultural norms and stigmatization limited in-depth investigation of sexual and behavioral practices and history of drug abuse. A shift of HIV infection from high-risk groups to the general population was seen and requires vigilant surveillance besides targeted health education, clinical management, lab facilities for diagnosis and monitoring, and voluntary counseling and testing services to limit disease spread.
Keywords: Outbreak, Investigation, HIV/AIDS, Gujrat, Pakistan
1. Background
The global HIV/AIDS pandemic has become one of the most important health problems of the past two decades. HIV incidence and associated mortality have continued to increase, especially in resource-poor countries. In 2004, about five million new infections and three millions deaths worldwide were estimated [1]. According to UNAIDS estimates from 147 United Nations Member States, more than 33 million people are living with HIV as of 2007, with an adult (15–49 years) prevalence of around 0.9% [2]. The HIV/AIDS pandemic has destabilized the health infrastructures, social systems, and economic growth especially in many resource-poor countries.
In Pakistan, HIV was introduced in the late 1980s, especially among injection drug users (IDUs), commercial sex workers (CSWs) and repatriated migrant laborers. According to UNAIDS estimate, the number of people living with HIV in Pakistan increased from less than a few hundred in 1990 to around 97,400 in 2009. The estimated number of deaths owing to AIDS increased from 1900 in 2001 to around 6000 in 2009 [3].
The burden of HIV in the general population in Pakistan is very low, with an estimated prevalence of less than 0.1%. The number of registered HIV cases in Pakistan is 4374 as of February 2011. By the end of 2010, around 1320 HIV cases were given Anti-Retroviral (ARV) drug therapy, which included 908 males, 355 females and 57 children less than 15 years [4]. Among the pockets of high-risk groups (IDUs, CSWs, and migrant workers), HIV prevalence is >5% and is believed to be rising. Recent national surveys indicate that the spread of the disease from high-risk groups to the general population may be owing to “bridge groups,” i.e., clients of sex workers and truckers which are presumed to overlap with the high-risk groups and general population [5].
Punjab is the most populous province of Pakistan with a total of 1387 registered HIV cases as of February 2011. The urban areas of Punjab have reported the existence of high-risk groups, including CSWs, truck drivers and IDUs. Not only do the large cities have an increasing number of cases, but the smaller cities/towns are also reporting HIV/AIDS cases.
According to the District Health authorities in Gujrat, JPJ has an area of 3192 square kilometers and a population of 2.53 million, of which about 100,000 are currently working in the Middle East, Europe and the United States of America. Gujrat District has three Tehsils–Gujrat, Kharian and Sarai Alamgir and 119 union councils. Jalalpur Jattan (JPJ) is a small town in Tehsil Gujrat and is divided into four administrative units as union councils. According to the 1998 population census, the total population of JPJ is around 120,000, with a population density of 642 persons/sq km and a rural:urban ratio of 2.3:1. The union council 61/2 has a population of 29,476 and is the second most populous union council in JPJ [6].
Two HIV screening camps were organized by a non-governmental organization (NGO), New Light AIDS Control Society (NLACS) in JPJ on 27 June and 1 July 2008. According to NLACS, the increased number of HIV-infected persons coming from the area prompted them to set up these camps. NLACS reported that 246 people underwent HIV testing, of which 88 (35.8%) were tested HIV-positive on three successive HIV rapid tests. Out of these, 74 were found positive by the ELISA method [7]. The extensive media coverage of high HIV infection in this town made the local community hostile to any further investigation. In this situation the Punjab AIDS Control Program (PACP) requested FELTP Pakistan to investigate the outbreak.
2. Aims and objectives
The objectives of the investigation were to determine the extent and chain of transmission of HIV infection within JPJ; to assess the adequacy of case and contact investigations; to identify additional contacts and sites of potential transmission of HIV infection: and to devise appropriate strategies and formulate recommendations to interrupt and prevent further transmission of HIV infection in JPJ.
3. Methodology
3.1. Study duration and setting
A field investigation was carried out from 15 December 2008 to 2 January 2009 in JPJ town in collaboration with the Civil Hospital-JPJ, support staff from the Health Department, and Executive District Office (EDO) Health Gujrat.
3.2. Case selection and inclusion criteria
All HIV-positive persons from JPJ town who consented to be interviewed from 15 December 2008 to 2 January 2009 were eligible for inclusion in this study. Eligible participants were either HIV-reactive by NACP or possessed documentary evidence of being HIV-positive from a recognized health facility. Persons from JPJ who had died of HIV/AIDS were also included provided that family members were available and willing to be interviewed.
3.3. Definitions
The following operational definitions were developed and used for the outbreak investigation:
-
•
A family was defined as parents, their children and grandchildren;
-
•
Two or more families having maternal or paternal relationship were considered relatives of each other;
-
•
Two or more HIV-infected persons from two or more different households of the same street of JPJ were identified as geographical clusters.
3.4. Enhanced contact tracing
The team started the investigation with the available list of 20 HIV-reactive persons at the Civil Hospital JPJ because the list of 88 people detected by the NGO was not available to NLACS or to the local health authorities. Enhanced contact tracing [8] and interviews were undertaken with the support of local health staff, and the persons involved in high-risk behaviors were encouraged to visit the VCT center arranged by the NACP.
3.5. Visit to the sites of transmission
Residences, along with private hospitals, nursing homes, clinics and labs run by qualified and unqualified healthcare providers, in JPJ were visited. Team members also visited areas known to be frequented by commercial sex workers, IDUs and transgender sex workers.
3.6. Data collection
The data were collected using a structured questionnaire. Demographic, clinical and exposure/contact information was collected to determine the risk factors and to monitor the behavioral patterns of the population. Even though a comprehensive questionnaire was used for the investigation, interviews were not limited to the questionnaire, and interviewees were given opportunities to go beyond the structured questionnaire. All subjects were verbally informed about the objectives of the investigation, the confidential nature of the interview, and the rights of the participants to refuse to answer questions, as well as the right of participants to end the interview at any time. For minors and children, informed consent was obtained only from their parents/guardians.
3.7. Sample collection, handling and transportation
Sample collection, handling, testing and transportation were done independently by the National HIV/STI Referral Lab of the NACP, Islamabad, according to CDC guidelines. Prior to sample collection, pretest counseling was done by a trained counselor from the NACP. The samples were collected for a rapid screening test by a latex aggregation test device (CAPILLUS HIV1/HIV2, Trinity, Biotec, USA) and post-test counseling was provided. After obtaining consent, blood samples were taken for confirmatory tests by ELISA using the Micro ELISA System (Vironostika, HIV Uni-Form II Ag/Ab, Biomerieux, Netherlands) and Western Blot Test with NEW LAV BLOT 1 (Biorad, France) at the National HIV/STI Referral Lab at NIH, Islamabad. Rapid Screening tests for diagnosis of Hepatitis B and C and Mycobacterium tuberculosis (MTB) were also offered. Nineteen unlinked anonymous reactive samples from JPJ were shipped in dry ice to the CDC, Atlanta, for advanced phylogenetic molecular studies.
3.8. Line listing and GPS mapping
A line listing, which included information about demographics, clinical and risk factor details was prepared and reviewed by the investigation team on a daily basis. Any missing information was investigated and updated on a regular basis. Data were entered into a specially designed database in Microsoft Access. The statistical analysis was done using Epi Info (version 3.5.1) and presented as proportions and percentages. A Global Positioning System (GPS) device (GPS 60, Gramin, USA) was used for mapping of sites, including small streets, hospitals, private clinics and labs, drug shooting spots and other places of interest to identify the geographical clustering.
4. Results
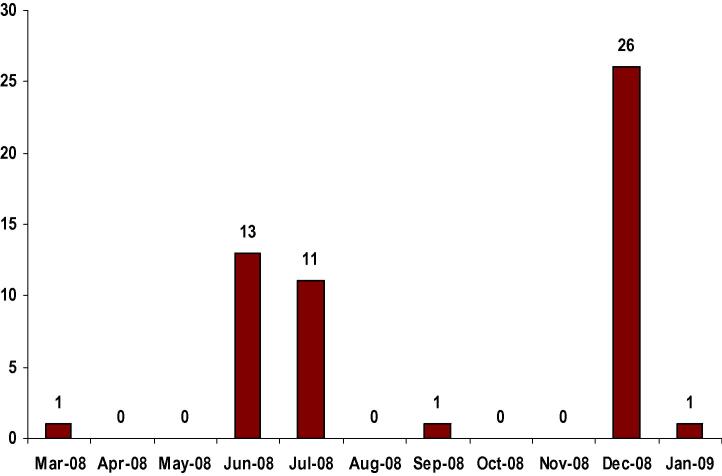
A total of 53 HIV-infected persons were investigated during the outbreak investigation. The distribution of these HIV-infected persons by the month in which they were tested reactive and their status reported to the local health authority is shown in Fig. 1. Out of the 53 HIV-infected persons investigated, 47 (88.7%) were alive and available for an in-person interview, while interviews with family members were conducted for the 6 deceased individuals.
Figure 1.
Distribution of these HIV-infected persons by the month.
The mean age of the subjects was 34.7 years (range: 3–70 years), with a median age of 35 years. The highest number of HIV infections was found in persons between the ages of 31 and 40 years (n = 16; 30.20%) followed by those aged 21–30 years (n = 13; 24.5%), aged 41–50 (n = 12, 22.64%) and aged 1–10 years (n = 06, 11.32%). The details are given in Table 1. Twenty eight (52.8%) females and 25 (47.2%) males were investigated. Among those investigated, 27 (51%) were diagnosed by NACP, while the remaining 26 (49%) were already confirmed by other sources. Twelve (22.6%) were undergoing or had a history of treatment. As regards marital status, 40 (75.5%) were married, 12 (22.64%) were unmarried and 1 (1.88%) was widowed.
Table 1.
Age wise distribution of HIV-reactive cases.
| S. No | Age group in years | HIV-infected persons | Percentage (%) |
|---|---|---|---|
| 1 | 1–10 | 06 | 11.32 |
| 2 | 11–20 | 01 | 1.88 |
| 3 | 21–30 | 13 | 24.53 |
| 4 | 31–40 | 16 | 30.20 |
| 5 | 41–50 | 12 | 22.64 |
| 6 | >50 | 5 | 9.43 |
The GPS mapping of the cases revealed that the maximum number of HIV-infected persons investigated during the outbreak was clustered around the Islampura (n = 17) area, New Noshehra (n = 11) area and Muwal (n = 6) area.
Among the signs/symptoms studied, most of the reactive cases had unexplained fever (n = 42, 79.2%), diarrhea (n = 34, 64.15%), recurrent skin infections (n = 27, 50.9%) and chest infections/RTI (n = 13, 24.5%). History of co-infection with Hepatitis B and C viruses was reported by 10 HIV-infected persons (5 each for hepatitis B and C), while tuberculosis was present in 13 (24.5%) of the HIV-positive cases. The details are presented in Table 2.
Table 2.
Frequency of signs and symptoms of investigated cases.
| S. No | Signs/symptoms/co-infections | Number (%) |
|---|---|---|
| 1 | Unexplained fever | 42 (79.2) |
| 2 | Diarrhea | 34 (64.15) |
| 3 | Skin infections | 27 (50.9) |
| 4 | Chest infection/RTIs | 13 (24.5) |
| 5 | Tuberculosis | 13 (24.5) |
| 6 | Hepatitis B | 5 (9.4) |
| 7 | Hepatitis C | 5 (9.4) |
| 8 | Cancer | 0 (0) |
The most common risk factor for HIV infection was the history of injections (n = 51, 96.2%). Forty-one cases (77.4%) frequently received injections during medical visits while only 12 (22.6%) received injections rarely. Twenty seven (96.4%) female patients had a history of ear and nose piercing, out of which 17 (63%) had a history of ear/nose piercings carried out at home.
Twenty-one (40%) of the cases interviewed had a history of dental procedures. Out of these, 12 (57%) gave a history of visiting quacks (any medical practitioner with questionable ability and reputation). Eighteen (72%) of the men had a history of barber shop visits on a monthly or even more frequent basis. Sixteen out of those (90%) reported that their barber used removable blades. Fourteen (26.5%) gave a history of undergoing a surgical procedure from which 10 (71.4%) underwent a surgical procedure from a medical doctor; while one had the history of a surgical procedure from a barber (information about the remaining two was not available). Eight (15%) had a history of receiving a blood transfusion; out of which 6 (75%) received a transfusion from a local public or private hospital. Only 1 out of the 53 admitted intravenous drug abuse in the past. However, during the outbreak investigation, the team noticed that there were at least two spots where discarded injection vials of narcotic analgesics were found along with the used syringes. The team also observed that a small group of people were injecting drugs during their visits. Five (9.4%) respondents reported a history of extramarital sex. All were heterosexual men. Only 2 HIV-reactive cases admitted to having paid for sex and only two cases gave a history of using condoms every time; 46 (87%) of the participants declined to give information about condom use. Five knew about the presence of a brothel house in the area in the recent past; while only one had the knowledge of an active brothel house still operational in the area. The details are presented in Table 3.
Table 3.
Frequency of risk factors and practices among investigated cases.
| Risk factors/practices | Frequency number (%) |
|---|---|
| General | |
| Injection in illness | 51 (96.2) |
| Dentists/dental procedures | 21 (39.6) |
| Surgery/surgical procedures | 14 (26.4) |
| Blood transfusion | 8 (15.1) |
| Travel abroad | 5 (9.5) |
| Tattoo marking | 4 (7.5) |
| Extramarital sex | 4 (7.5) |
| Sharing of shaving razor | 1 (1.9) |
| Used IV drugs | 1 (1.9) |
| Sharing of tooth brush/miswak | Nil |
| Gender specific | |
| Ear/nose piercing (only females, n = 28) | 27 (96.4) |
| Barber shop (only males, n = 25) | 18 (72) |
The travel history of HIV-infected persons investigated reveals that 5 (9.5%) had a history of travel abroad. Four had traveled to different Middle Eastern and Far Eastern countries. Two had been deported from the Middle East after confirmation of their positive HIV antibody result. Among those investigated, an unqualified healthcare worker was HIV-positive and had a history of multiple needle pricks.
Twenty-nine (55.8%) investigated cases claimed that they were aware of routes of HIV transmission. However, only 19 (35.8%) were aware that HIV can be sexually transmitted. Only eighteen (34%) were aware of HIV transmission through blood and blood products. Similarly, 19 (35.8%) respondents knew that sharing of sharps and syringes may result in the transmission of HIV. Five (9.4%) knew about mother-to-child transmission of HIV. Twenty-two (41.5%) were not aware of specific treatments for HIV. Thirty-three (63.5%) stated that they had the knowledge about the prevention of HIV. Seventeen (33.3%) of the respondents considered that HIV is prevented by avoiding contaminated blood transfusion, while only 12 (24%) responded that HIV can be prevented by protected sex.
Epidemiological investigation indicated that all patients could be distributed into 9 geographical clusters involving 13 families and 8 individuals.
A total of 19 unlinked anonymous reactive samples from JPJ were shipped in dry ice to the CDC, Atlanta, for advanced molecular studies, including HIV/AIDS phylogenetic testing. The phylogenetic analysis was done by amplifying envelope (env) and protease genes using universal primers because of the lack of clinical and demographical information. Phylogenetic analysis of 10 of the 19 samples was done using the envelope gene sequences by pairwise distance calculation method using the Kimura 2-parameter Nucleotide Model for genetic distance evaluation. The results of the molecular studies confirmed the presence of HIV 1 subtype A in the current endemic in JPJ. The pairwise analysis also reveals that the average distance of the tested viruses is 9% with a range of 6–13% with an annual variation of 1%.
5. Discussion
The report presented here describes the epidemiological characteristics of 53 HIV-infected persons identified in the outbreak investigation in JPJ, Gujrat district, Pakistan. The investigation indicates the rise in HIV infections in the JPJ area and the probable shift of infection from core (high-risk) groups to the general population, which may require further epidemiological studies. This may also indicate that there has been a transition in transmission patterns as of the major urban cities to the small rural towns of Pakistan which is alarming since approximately 66% of the Pakistani population live in rural areas [9]. The virus also seems to have now established a foothold, as evidenced by the sporadic HIV outbreaks among the injecting drug user community.
Pakistan remained relatively safe from indigenous HIV infections for around two decades, and most HIV infections were attributed to imported cases among HIV-positive Pakistani workers deported from Middle Eastern countries in the early 1990s with little indication of indigenous transmission limited to high-risk groups. Previous research suggests that between 70,000 and 120,000 IDUs and about 200,000 sex workers reside in Pakistan. Out of these, about 30–50% live in Pakistan’s largest cities [9]. The other factors contributing to the spread of HIV in Pakistan include the widespread presence and interlinking of IDUs and high-risk sexual networks, mobility of high-risk populations, high volumes of migrant laborers within and outside of Pakistan, increasing poverty and high illiteracy rates. This is the same pattern that has been observed in several other Asian countries [10–13].
During the field investigation, intensive efforts were undertaken to collect as much clinical, social, behavioral and epidemiological information as possible; however, interviewed people were reluctant to provide detailed sexual and drug abuse history because of socio-cultural norms and fears of stigmatization. Another limitation was difficulty in recalling events that happened far in the past.
In 2004, 23% of injecting drug users and 4% of male sex workers have been found to be positive for HIV from Karachi. An outbreak of HIV/AIDS was also reported from Larkana, Sindh, among injection drug users in July 2003, which may have provided a home-base for the virus in Pakistan. A study done by Bokhari et al. predicted that the presence of high sero-prevalence of HIV among high-risk groups together with unsafe medical injections could be a source of HIV transmission into the general population [14].
Even though HIV-infected persons described in this outbreak investigation are not representative of the JPJ population, nearly equal male to female ratio is different from earlier data reported from Pakistan which showed male predominance [15]. Another important finding of this investigation was the high HIV positivity among children. Six (11.32%) of the HIV-infected persons in this group were children under 10 years of age.
The use of injections for illness by more than 95% of the investigated cases was also a major finding while a significant proportion of investigated persons provided the history of invasive surgical and dental procedures in the past. These observations in the presence of poor sterilization practices could have promoted the spread of HIV and other blood-borne viruses. Use of unsafe injection practices both in formal and non-formal health care settings has been documented in Pakistan. Both patient’s and provider’s preference for injections in place of oral drugs has become a major public health concern in Pakistan [16].
There is also substantial evidence that a community of intravenous drug users exists not only in the affected areas of JPJ, but other areas of town as well. The HIV prevalence remained very low in drug-using populations (0% to 2%) till 2003; however, among commercial sex workers and prisoners, the seroprevalence rates have ranged from 0% to 1.8%. In 2003, however, an outbreak of HIV infection among injection drug users (IDUs) in a prison located outside of Karachi was reported, in which among 175 prisoners tested, 17 (9.7%) were HIV-positive. In 2004, another outbreak of HIV among injection drug users was detected in Karachi, where 23% of IDUs tested were HIV-positive [17]. The HIV prevalence rates among drug users in other regions of Pakistan have not been studied; however, findings of this study further emphasize the need for a more focused approach toward harm reduction in the IDUs.
In the past, contact investigations have been used as a tool for prevention of HIV and sexually transmitted infections (STIs) [18,19]. The investigation team found this method also applicable to this outbreak investigation as it can also be used to explore the epidemiology of HIV in high-risk populations and areas, to provide personalized education, and to identify individuals who engage in high-risk behaviors [20].
In Pakistan, very limited information is available on the prevalence of specific HIV genotypes. According to the study by Khan et al. HIV 1 subtype A was present in a community of intravenous drug users in Karachi [21]. The presence of cluster sequences indicates that the HIV in this area may have a common ancestor when compared with other sequences in this analysis. The presence of a 1% variability rate per year in the env gene region is very significant, and preliminary results indicate that the samples tested were not directly linked. This suggests that the introduction of HIV to this area was not recent and provides evidence of continuing transmission over the years. The same has been seen in the famous Libyan HIV outbreak involving foreign medical staff [22]. Although the analysis does not support the transmission of HIV among the individuals whose samples were tested for phylogenetic testing, only 10 samples from JPJ were successfully tested for phylogenetic characteristics.
This outbreak demonstrates that there is a significant cause for concern regarding the spread of HIV in the JPJ region. The information was collected in 21 days through enhanced contact tracing. The spatial clustering of HIV-infected persons is suggestive of HIV transmission primarily within two geographically small areas of JPJ. A conclusive source of the outbreak was difficult to be traced as the transmission spread was over a decade. However, there are a number of risk factors which may have contributed to the alarming rise in the number of HIV-infected persons. These include: expatriates HIV-positive persons deported from different countries and not well educated concerning preventive measures, unsafe injection practices, presence of injecting drug users in the community, invasive surgical/dental procedures, unsafe ear/nose piercing practices and unsafe sexual practices.
There was a brothel in the close vicinity of the affected area where female commercial sex workers came from different areas. With reports of AIDS cases and deaths in JPJ through electronic and print media, local law enforcement authorities sealed the brothel and arrested the owner. However, the commercial sex workers were able to escape and were not traceable; their HIV status is therefore not known. There were reports of another brothel in the vicinity of the affected area, whose CSWs came from JPJ and other parts of Punjab, and there are at least two known pick-up points (commonly known as “lover points”) which have been identified as hot spots for promoting pre- and extra-marital sexual practices, especially among young people.
Based on the study findings, it was recommended that a surveillance center needs to be established in the Gujrat district on a priority basis with the facilities to screen and offer VCT to screen pregnant women, TB-positive patients, STD patients and to carry-out the surveillance for perinatal HIV exposure. This area should be included in the upcoming round of second generation surveillance [23]. The HIV screening of blood before transfusion should be made mandatory. The need was also felt to raise the awareness among the residents of JPJ; therefore it was recommended that an intensive awareness campaign regarding health education and safe injection practices should be launched and strengthened and focused on HIV/AIDS. Condom promotion, diagnosis and treatment of STIs and safer sex activity counseling should be given to HIV/AIDS patients, as well as IDUs should also be taken into consideration to limit the sexual transmission of HIV in JPJ [24]. To understand HIV transmission in the local context, it is recommended that a good cross-sectional study with an analytical component to look for risk factors should be conducted.
6. Conflict of interest
None declared.
References
- [1].Hogan DR, Baltussen R, Hayashi C, Lauer JA, Salomon JA. Cost effectiveness analysis of strategies to combat HIV/AIDS in developing countries. BMJ. 2005 Dec 17;331(7530):1431–7. doi: 10.1136/bmj.38643.368692.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].UNAIDS . Executive Summary. Report of global AIDS epidemic. UNAIDS; 2008. Jul, [Google Scholar]
- [3].UNAIDS AIDS info country fact sheets. 2011 Available from: URL: http://www.unaids.org/en/dataanalysis/tools/aidsinfo/countryfactsheets/http://www.unicef.org/infobycountry/pakistan_pakistan_statistics.html; [accessed April 2011].
- [4].UNGASS PAKISTAN REPORT . Progress report on the Declaration of Commitment on HIV/AIDS for the United Nations General Assembly Special Session on HIV/AIDS. Islamabad: National AIDS Control Program, Ministry of Health, Government of Pakistan; 2010. [Google Scholar]
- [5].HIV second generation surveillance in Pakistan . Round III. Islamabad, Pakistan: National AIDS Control Programme, Ministry of Health; 2008. [Google Scholar]
- [6].District census report of Gujrat. Islamabad: Population Census Organization, Statistics Division; 1998. [Google Scholar]
- [7].Outbreak Investigation report, Mohallah Joggi Pura. Gujrat: New Light AIDS Control Society and Provincial AIDS Control Programme; 2008. [Google Scholar]
- [8].Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR. Recommendations and reports. 2005 Dec 16;54(RR-15) [PubMed] [Google Scholar]
- [9].HIV second generation surveillance in Pakistan, National Report Round III. Pakistan: NACP, MOH; [Google Scholar]
- [10].Saleem NH, Adrien A, Razaque A. Risky sexual behaviour, knowledge of sexually transmitted infections and treatment utilization among a vulnerable population in Rawalpindi, Pakistan. South East Asian J Trop Med Public Health. 2008;39(4):642–8. [PubMed] [Google Scholar]
- [11].Emmanuel F, Fatima M. Coverage to curb the merging HIV epidemic among injecting drug users in Pakistan: delivering prevention services where most needed. Int J Drug Policy. 2008;19(Suppl. 1):S59–64. doi: 10.1016/j.drugpo.2007.12.012. [DOI] [PubMed] [Google Scholar]
- [12].Zahid AK, Gibeny L, Ahmed JA, Vermund SH. HIV/AIDS and its risks factors in Pakistan. AIDS. 1997;11:843–8. doi: 10.1097/00002030-199707000-00002. [DOI] [PubMed] [Google Scholar]
- [13].Rai MA, Warraich HJ, Ali SH, Nerurkar VR. HIV/AIDS in Pakistan: the battle begins. Retrovirology. 2007;4:22. doi: 10.1186/1742-4690-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bokhari A, Nizamani NM, Jackson DJD, Rehan NE, Reahman M, Muzaffar R, et al. HIV risk in Karachi and Lahore, Pakistan: an emerging epidemic in injecting and commercial sex networks. Int J STD AIDS. 2007;18:486–92. doi: 10.1258/095646207781147201. [DOI] [PubMed] [Google Scholar]
- [15].Rajabali A, Khan S, Warraich HJ, Khanani MR, Ali SH. HIV and homosexuality in Pakistan. Lancet Infect Dis. 2008;8(8):511–5. doi: 10.1016/S1473-3099(08)70183-X. [DOI] [PubMed] [Google Scholar]
- [16].Khawaja ZA, Gibney L, Ahmed AJ, Vermund SH. HIV/AIDS and its risk factors in Pakistan. AIDS. 1997;11(7):843–8. doi: 10.1097/00002030-199707000-00002. [DOI] [PubMed] [Google Scholar]
- [17].Kuo I, Ul-Hasan S, Galai N, Thomas DLD, Zafar T, Ahmed MA, et al. High HCV seroprevalence and HIV drug use risk behaviors among injection drug users in Pakistan. Harm Reduct J. 2006;3:26. doi: 10.1186/1477-7517-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Australasian contact tracing manual, A practical handbook for health care providers managing people with HIV, viral hepatitis, other sexually transmissible infections (STIs) and HIV-related tuberculosis. 3rd ed 2006. [Google Scholar]
- [19].Frerichs RR. HIV contact tracing. SEA-AIDS network; June 10, 1998. < http://www.ph.ucla.edu/epi/seaids/seasids_52.html> [accessed 01.04.09].
- [20].Legal aspects of HIV/AIDS, a guide for policy and law reform. The World Bank; 2007. [Google Scholar]
- [21].Khan S, Rai MA, Khanani MR, Khan NM, Ali SH. HIV-1 subtype A infection in a community of intravenous drug users in Pakistan. BMC Infect Dis. 2006;6:164. doi: 10.1186/1471-2334-6-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].de Oliveira T, Pybus OG, Rambaut A, Salemi M, Cassol S, Ciccozzi M, et al. Molecular epidemiology: HIV-1 and HCV sequences from Libyan outbreak. Nature. 2006;444:836–7. doi: 10.1038/444836a. [DOI] [PubMed] [Google Scholar]
- [23].Abu-Raddad L, Akala FA, Semini I, Riedner G, Wilson D, Tawil O. Middle East and North Africa HIV/AIDS epidemiology synthesis project. World Bank/UNAIDS/WHO publication. Washington DC: The World Bank Press; 2010. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa: time for strategic action. [DOI] [Google Scholar]
- [24].World Health Organization HIV/AIDS Department; 2009. Apr, PRIORITY INTERVENTIONS HIV/AIDS prevention, treatment and care in the health sector. (version 1.2). [Google Scholar]