Abstract
This retrospective study aimed to address whether or to what extent spatial and non-spatial factors with a focus on a healthcare delivery system would influence successful tuberculosis (TB) treatment outcomes in Urmia, Iran. In this cross-sectional study, data of 452 new TB cases were extracted from Urmia TB Management Center during a 5-year period. Using the Geographical Information System (GIS), health centers and study subjects’ locations were geocoded on digital maps. To identify the statistically significant geographical clusters, Average Nearest Neighbor (ANN) index was used. Logistic regression analysis was employed to determine the association of spatial and non-spatial variables on the occurrence of adverse treatment outcomes. The spatial clusters of TB cases were concentrated in older, impoverished and outskirts areas. Although there was a tendency toward higher odds of adverse treatment outcomes among urban TB cases, this finding after adjusting for distance from a given TB healthcare center did not reach statistically significant. This article highlights effects of spatial and non-spatial determinants on the TB adverse treatment outcomes, particularly in what way the policies of healthcare services are made. Accordingly, non-spatial determinants in terms of low socio-economic factors need more attention by public health policy makers, and then more focus should be placed on the health delivery system, in particular men’s health.
Keywords: Tuberculosis, Adverse treatment outcome, Health policy-making, Geographical Information System
1. Introduction
Globally, multidrug-resistant tuberculosis (MDR-TB), mainly because of prior failed or default treatment outcomes, is a serious problem in the fight against TB disease [1–4]. According to the World Health Organization (WHO) report in 2013, annually on average, 3.6% of new TB patients were diagnosed with MDR-TB and at least half a million people were diagnosed with MDR-TB worldwide, of whom the majority live in low- to middle-income countries (LMICs) [5]. As a major challenge to the control of MDR-TB, Directly Observed Treatment-Short Course (DOTS) was recommended by WHO to overcome failed and default treatment outcomes [6]. Nevertheless, in almost all LMICs that adopted the DOTS project, MDR-TB followed by high rates of adverse treatment outcomes is a common issue [7,8].
In spite of the evidence indicating the contribution of non-spatial characteristics, including age, gender, low education achievement, domicile and social class to determine the outcome of TB treatment [9,10], the spatial factor in terms of physical accessibility to a healthcare center during the drug treatment course has been less considered. Moreover, reasons for failed or default treatment outcome are multifaceted and involve a combination of spatial and non-spatial factors, along with how health policy was formulated to deliver healthcare services [11–14].
Iran as a middle-income country, located in the Eastern Mediterranean region with an average incidence rate of TB (all TB forms 0–24 per 100,000 population), has experienced increased incidence rates of TB drug resistance during recent years [15]. One step in order to determine the distribution of TB cases is visualizing the statistics by employing the application of the Geographical Information System (GIS) in the public health discipline; however, this was hardly considered an option in Iran, and its usage is limited [16]. Accordingly, there are a few studies on spatial patterns of TB and their related treatment outcomes that have focused on non-spatial factors. These studies have shown a link between ethnicity, previous unsuccessful treatment, age and sex with anti-TB drug resistance [15,17]; however, information on the effect of spatial and non-spatial determinants on TB treatment outcomes is scarce. Therefore, this retrospective study aimed to address whether or to what extent spatial and non-spatial factors with a focus on a healthcare delivery system would affect successful TB treatment outcomes in Urmia, Iran.
2. Methods
2.1. Study area and population
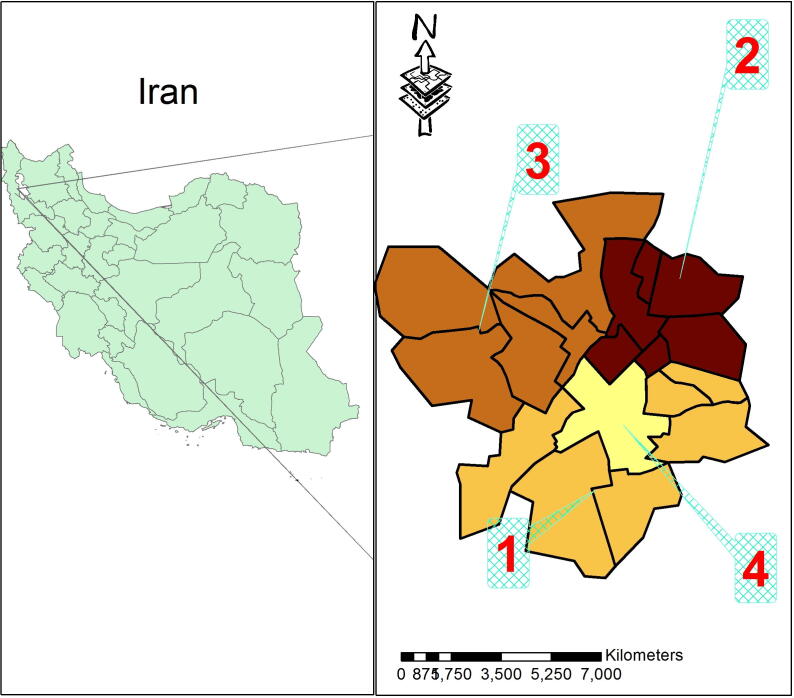
This cross-sectional study was conducted in Urmia, the capital of West Azerbaijan Province (WAP), which is located along the border of Turkey and the Lake of Urmia that extends to the East. The Urmia landmass is 5,125 square kilometers (km2), with a density of 85.2 inhabitants per km2. According to the 2006 census in Iran, the Urmia population was 875,000 (30% of total WAP population), with 69% urban residents and a male to female ratio of 51% [18]. According to the Human Development Index (HDI), the WAP is one of the most deprived regions in Iran [19]. The Urmia population is served by 18 urban and 33 rural health centers (on average, given that urban and rural health centers serve 48,000–60,000 and 6,000–8,000 inhabitants, respectively). The municipality includes four districts (Fig. 1), of which the district with the higher socioeconomic status is located in the central area (district number of 4), while others with lower socioeconomic status are concentrated in the northwest and northeast regions (district numbers 2 and 3). The population density per km2 for district numbers 1 and 4 and also 2 and 3 is homogenous across Urmia city, respectively [20].
Figure 1.
Socioeconomic status by districts according to Urban Sustainable Development Index (TOPSIS model), Urmia, Iran. Source: Mobaraki et al. [20].
2.2. Health care utilization among TB patients
According to the health service delivery system in Iran, the supervision and implementation of the DOTS project, as well as the follow-up of drug treatment adherence, is free of charge and health workers are referred to the closest healthcare center with respect to the TB patient‘s residence.
2.3. Data source and data collection procedure
Based on the integration of a TB program into the Primary Health Care (PHC) network in Iran (1990), all new cases of TB diagnosed by a qualified physician in clinics, hospitals or health centers should be reported to the Tuberculosis Management Center (TBMC). The TBMC database then has the most completed data source of TB at the national level and provides district health staff members with an opportunity to follow-up the treatment process with patients through home visiting in order to observe any suspected close contacts. The database provides information about socio-demographic characteristics, disease information such as smear positive/negative pulmonary and extra-pulmonary TB, family size and an accurate residential address. In the present study, all of the 454 new cases of TB during the period 20 March 2004–20 March 2009 were considered. In practice, because of no data regarding residential address for 2 patients, 452 cases were taken into account in this study.
2.4. GIS mapping
Digital maps of Urmia were provided by the GIS department of the WAP Governor’s Office. In the first step, the urban setting using ARC MAP 9.3 software, health centers, health posts and study subjects’ locations across catchment areas were geocoded. The process of geo-referencing was carried out for 401 of the TB cases (83%). From the 51 cases that were not geocoded, 35 of them were in prison and 16 patients had received TB drugs from TBMC directly. However, given that the TB diagnosis and treatment services are provided instantaneously in prisons in Iran, modeling of accessibility in terms of geographical distance from the health center was impossible.
In the second step, catchment areas for each health center which were derived from the TBMC were plotted on mapping files. For better visualization, the maps have been categorized by 1 km distances from health centers across the given catchment area. Each of the health catchment areas envelops the distribution of TB patients as satellites around healthcare centers where TB treatment is delivered as well. All of the health centers were under the direct supervision of the TBMC, and TB treatment services were provided by each one of them actively where patients lived across its related health center catchment area.
In the third step, in order to measure the distance from a patient’s home to the health center, “Minimum Euclidean distance,” which represented the straight line, was employed. Since primary healthcare services including the TB treatment program are delivered actively by community health workers (called Behvarz) in rural areas, on average, the patient’s distance from a given rural healthcare center was defined as 100 m.
In the fourth step, the number of adverse outcomes as defaulted or interrupted cases was demonstrated for each catchment area separately (Fig. 3).
Figure 3.
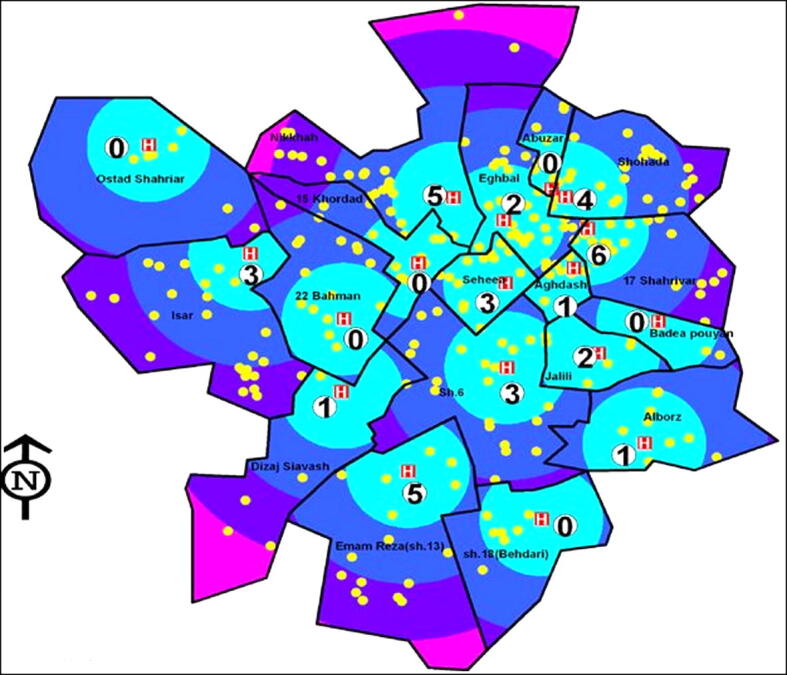
Spatial accessibility to TB health care center in Urmia, Iran.
2.5. Data analysis
The tool box of the Arc Map software version 9.3 was used for spatial analysis. The Average Nearest Neighbor (ANN) index was applied based on the minimum average Euclidean distances from each TB case to its nearest neighboring case to identify TB aggregations. The ANN index compares the average distance ratio of the nearest neighbor point (observed) with the average distance of expected points (as the distance between neighbors in a hypothetical random distribution). Values of the ANN index that are greater than the upper limit of the Z score indicate concentration, while values of the ANN index less than the lower limit of the Z score indicate dispersion. Distribution of TB case data was divided into two main categories based on treatment outcomes (failed or interruption versus recovery) and the association between two categories and socio-demographic determinants, including gender, age, type of TB, education attainment, job and domicile, which was tested by Odds Ratio. Finally, independent variables were entered stepwise into the logistic regression models in the order of eliminating confounding effects. The SPSS version 16.00 was used for data analysis.
2.6. Ethical permission
The ethical verification from the ethics committee of the Urmia University of Medical Sciences was obtained. Moreover, permission from the Deputy for Health Affairs managers was taken.
3. Results
3.1. Spatial clusters in urban and rural areas
Fig. 2 presents the spatial distribution of TB patients in urban area. Using the ANN index, it identified significant nonrandom dispersion of TB cases into context (ANN index: 0.79 Z score = −6.4766 and P value = 0.0001) with observed and expected mean distances of 230 and 292 m, respectively. Visually, three spatial clusters of TB cases were found during the study period of which most cases of TB were concentrated in impoverished and outskirts areas (district numbers 2 and 3).
Figure 2.

Spatial distribution of TB cases in Urmia, Iran.
3.2. Socio-demographic characteristics
Table 1 presents the distribution of socio-demographic features of TB patients and categories of treatment outcomes, divided into default or interruption and recovery outcomes. Moreover, univariate analysis of socio-demographic characteristics with respect to treatment outcome by means of crude Odds Ratio (OR) is presented in the last column of Table 1. The higher odds of TB adverse treatment outcome was found among men. Moreover, TB patients’ age between the two categories of treatment outcomes was similarly distributed. The proportion of default or interruption outcome was higher among patients with pulmonary TB disease, although this finding did not reach a statistically significant level. There was an association between the categories of education, occupation and treatment outcome, of which more vulnerable cases for default or interruption TB outcome belonged to the lower levels of education and self-employed occupation groups. In general, the urban residents consisted of a larger proportion of TB as well as a higher number of default and interrupted cases, but there was no significant association between domicile and outcome of TB treatment.
Table 1.
Classification of socio-demographic characteristics among TB patients with default/interruption and recovery outcomes. Urmia, Iran.
| Socio-demographic characteristics | Treatment outcome | Total No. | Crude odds ratio (95% CI) | |
|---|---|---|---|---|
| Default/interruption N = 50 (%) |
Recovery N = 402 (%) |
N = 452 (%) | ||
| Gender | ||||
| Female | 10 (5.5) | 172 (94.5) | 182 (40.3) | Reference |
| Male | 40 (14.8) | 230 (85.2) | 270 (59.7) | 2.99 (1.41–6.88) |
| Age | ||||
| <14 | 1 (12.5) | 7 (87.5) | 8 (1.8) | 1.28 (0.02–11.5) |
| 15–24 | 5 (10.6) | 42 (89.4) | 47 (10.5) | 1.07 (0.27–3.51) |
| 25–34 | 8 (9.5) | 76 (90.5) | 84 (18.7) | 0.94 (0.31–2.66) |
| 35–44 | 12 (15) | 68 (85) | 80 (17.8) | 1.58 (0.61–4.10) |
| 45–54 | 7 (12.1) | 51 (87.9) | 58 (12.9) | 1.23 (0.38–3.64) |
| 55–64 | 5 (9.6) | 47 (90.4) | 52 (11.6) | 0.95 (0.24–3.12) |
| >65 | 12 (10) | 108 (90) | 120 (26.7) | Reference |
| Type of TB | ||||
| Pulmonary (PTB) | 39 (13.2) | 257 (86.8) | 296 (65.5) | Reference |
| Extra-pulmonary (EPTB) | 11 (7.1) | 145 (92.9) | 156 (34.5) | 0.49 (0.22–1.03) |
| Education | ||||
| No schooling/illiterate | 14 (6.7) | 181 (93.3) | 195 (42.7) | 0.31 (0.14–0.68) |
| Primary school (Grade 1–5) | 22 (19.6) | 90 (80.4) | 112 (24.8) | Reference |
| Lower secondary school (Grade 6–8) | 6 (13.6) | 38 (86.4) | 44 (9.7) | 0.64 (0.19–1.82) |
| Upper secondary school (Grade 9–12) | 5 (9.4) | 48 (90.6) | 53 (11.7) | 0.42 (0.11–1.25) |
| University | 2 (10) | 18 (90) | 20 (4.6) | 0.45 (0.04–2.14) |
| Unspecified | 1 (3.8) | 24 (96.2) | 25 (5.8) | − |
| N/A (Children under 6 years) | 1 (33.3) | 2 (66.7) | 3 (0.7) | − |
| Occupation | ||||
| Self-employed | 20 (25) | 60 (75) | 80 (17.7) | Reference |
| Farmer | 5 (12.2) | 36 (87.8) | 41 (9.1) | 0.41 (0.11–1.28) |
| Labourer | 3 (10.7) | 25 (89.3) | 28 (6.2) | 0.36 (0.06–1.39) |
| Student | 3 (3.9) | 13 (96.1) | 16 (3.5) | 0.69 (0.11–2.90) |
| Housewife | 7 (4.7) | 141 (95.3) | 148 (32.7) | 0.14 (0.05–0.39) |
| Governmental employee | 3 (17.6) | 14 (82.4) | 17 (3.8) | 0.64 (0.10–2.66) |
| Unemployed | 5 (7.1) | 65 (92.9) | 70 (15.5) | 0.23 (0.06–0.69) |
| Retired | 1 (5) | 19 (95) | 20 (4.4) | 0.15 (0.003–1.14) |
| N/A(Children under 6 years) | 1 (33.3) | 2 (66.7) | 3 (0.7) | − |
| Unspecified | 2 (6.9) | 27 (93.1) | 29 (6.4) | − |
| Domicile | ||||
| Urban | 12.7 | 87.3 | 68 | Reference |
| Rural | 7.6 | 92.4 | 32 | 0.56 (0.25–1.17) |
3.3. Physical accessibility to health centers
Fig. 3 shows the distribution of TB patients, health centers and health post with catchment area. In comparison with average-weighted case distance from health center, mean distance of patients with default/interrupted outcome was higher than others, but its difference was not statistically significant (1286 ± 708 and 1079 ± 715 m, P value = 0.09).
Table 2 presents the results of logistic regression analysis based on some important variables that were selected for the model after controlling the confounding effects. Accordingly, no significant differences regarding failure or interrupted outcome were observed through age groups and education strata. Compared with PTB, EPTB was associated with higher odds of adverse treatment outcome. In addition, men were more than twice significantly as odds to be among TB cases with default or interruption outcomes as women. Despite a tendency toward higher odds of adverse treatment outcomes for urban dwellers after adjusting for distance from any TB health care center, this finding did not reach a statistically significant level.
Table 2.
Multivariate analysis of the parameters associated with default/interruption outcome of treatment. Urmia, Iran.
| Explanatory variables | Adjusted odds ratio(CI) | P value |
|---|---|---|
| Age | 0.99 (0.97–1.01) | 0.381 |
| Gender (male vs. female) | 2.50 (1.17–5.34) | 0.017 |
| Education | 0.92 (0.75–1.13) | 0.452 |
| Type of disease (PTB vs. EPTB) | 2.20 (0.97–5.01) | 0.058 |
| District (rural vs. urban) | 0.69 (0.26–1.86) | 0.476 |
| Distance from health center (meter) | 1 (1.00–1.001) | 0.159 |
4. Discussion
4.1. Main findings
This is the first study with an integrated approach to highlight the effect of spatial and non-spatial determinants on TB incidence and disease control. The univariate analysis in this study showed that the non-spatial factors, including insecure jobs, low education level and sex were associated with adverse TB treatment outcome. In addition, the TB cases with failure or interruption treatment outcome did not reside further away from related health centers in the urban areas. The multivariate analysis highlighted female sex as a significant protected variable against adverse treatment outcome. Moreover, TB cases are not distributed at random, and there is a strong heterogeneity across the geographic areas of Urmia, of which the most likely clusters were detected in old, poor and on the outskirts of urban areas, namely district numbers 2 and 3.
Based on the national figures of TB in Iran, women are over-represented among all age groups [21]. In contrast, findings in a previous study in WAP indicated the lower notification rates of TB among women [22]. The better treatment outcomes in women could be partially explained by: they seek timely TB diagnosis and they are more likely to continue therapy; consequently, they have a better treatment outcome. However, there are reasons to believe that the adverse treatment outcomes are more likely to occur in men in Iran [23–25]. This might be explained by socio-economic issues via poor access to health centers, of which men are more likely to fear losing insecure jobs and, consequently, tend to delay TB care-seeking [9]. Probably as a result, the higher prevalence of MDR-TB among Iranian men [15] would be explained by the above reasons. In contrast, findings from a study in Egypt showed no significant gender differences toward TB treatment outcome [26]. The reason for that might be a result of extreme job importance and its security for Iranian men.
The other important finding of this study was related to the role of poverty with respect to old, poor and the outskirts of urban areas. This is in line with most studies in which traditionally TB was recognized as a disease of the poor. The result of other studies also represented TB clusters in more deprived areas in urban settings, where living conditions are at the minimum level [27–30]. It is questionable whether the socioeconomic status of TB cases at the individual level could be playing a determinant factor in the adverse treatment outcome prevalent in the urban outskirts, too [31,32]. The lack of access due to geographical distance to a healthcare center was found to be one of the main determinants related to default or failure treatment outcome and poor health of populations as a whole in developing countries [10,33,34]. Nevertheless, living in poor and remote urban areas seems to have more effect on increasing the number of TB cases, as well as those with adverse treatment outcomes [34,35]. As a result, the most likely barriers to accessing a healthcare center might be explained by poverty in terms of treatment costs and a low level of knowledge regarding free-of-charge diagnostic and therapeutic TB services in Iran. According to the Ministry of Health and Medical Education (MOHME) reports in Iran, at least 40% of people who need various types of outpatient services have delayed seeking treatment, mostly due to increased costs of medical services over the last two decades [36]. This implies that the free-of-charge diagnosis and treatment of TB should be announced, particularly in both health centers and hospital services.
However, though physical accessibility to health services influences the health outcome, the probable reasons to prove that TB patients in urban outskirts are more vulnerable to adverse treatment outcomes can be described in the way the Primary Health Care (PHC) policies are made [14]. Accordingly, some studies in LMICs like Nepal, Thailand, Uzbekistan and Senegal established a relationship between active case findings of TB and cases undergoing supervised health treatments in a facility-based institution with a lower incidence rate of failure or interruption outcomes of treatment [37–40]. Hence, it is not surprising to find higher rates of failure and interruption outcomes of treatment mainly owing to passive TB case findings and following-up of treatment adherence in urban districts of Iran, while TB-related services are actively delivered by community health workers (called Behvarz) in rural areas, and its PHC network in terms of accessibility is demonstrated as one of the best in the Middle-East region [41,42].
4.2. Strengths and limitations
This is the first study in Iran to use a holistic approach toward spatial and non-spatial determinants of TB incidence and disease control. Nevertheless, some limitations should be considered. First, spurious addresses of some patients (4 cases) were obtained based on the general family address due to implications related to the administration or utilization of DOTS; if the number is too low, it cannot affect the result of the study. The other limitation is the heterogeneity of the population density across given health center catchments. In order to overcome this problem, the administrative data that were provided by the Development Department of Urmia Deputy for health affairs were used where health catchment borders are determined based on equal population size. Even though, some health centers may be cases for population heterogeneity because of urbanization promotion and development measures. Although using the Minimum Euclidean distance might not be appropriate to calculate the distances from the patients’ homes to the nearest health center, as many other studies worldwide the straight-line distance from the facility was used in this study because the calculation of the actual distance from the patients’ homes to the nearest health center for a given catchment area was impossible in an urban setting. Finally, indicators related to health services utility, as well as healthcare-seeking behavior, might have been a subject for adverse outcome. However, it was not included within the scope of this study. This subject not only makes for an interesting topic for future investigations, but it is currently under way.
5. Conclusion
This study highlights the effect of spatial and non-spatial determinants of TB incidence and disease control, particularly with regard to the way the policies of health-care services are made. Accordingly, non-spatial factors in terms of low socio-economic status need for more attention by public health policy makers, and then more focus should be placed on the health delivery system, particularly in men. In addition, using the GIS/GPS application with a view to TB distribution and physical accessibility to healthcare centers is a novel method in Iran and it can be developed to reach other related public health disciplines.
Acknowledgements
This study has been funded by grants from the Deputy for Research Affairs of Urmia University of Medical Sciences. We are grateful to all TB local focal points that assisted with this study through the data collection process. Moreover, we would like to thank Ardashir Yousefzadeh, from the GIS department of WAP Governor regarding his critical comments with regard to providing digital maps.
Contributor Information
Goodarz Kolifarhood, Email: Gfarhood@gmail.com.
Davoud Khorasani-Zavareh, Email: Davoud.khorasani@gmail.com.
Shaker Salarilak, Email: Salarilak@yahoo.com.
Alireza Shoghli, Email: Shoghli@zums.ac.ir.
Nasim Khosravi, Email: Nasimkhosravi.khosravi3@gmail.com.
Competing interests
No competing interests were declared by the authors.
Author contribution
Mr. Kolifarhood had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Shaker Salarilak and Dr. Khorasani-Zavareh contributed equally to the paper.
Study concept and design: Dr. Shaker Salarilak, Mr. Kolifarhood, Dr. Khorasani-Zavareh.
Acquisition of data: Dr. Shaker Salarilak, Mr. Kolifarhood, Dr. Khorasani-Zavareh, Dr. Shoghli, Ms. Khosravi.
Analysis and interpretation of data: Mr. Kolifarhood, Ms. Khosravi.
Drafting of the manuscript: Mr. Kolifarhood, Dr. Khorasani-Zavareh, Dr. Shoghli, and Ms. Khosravi.
Critical revision of the manuscript for important intellectual content: Dr. Khorasani-Zavareh, Dr. Shoghli, Dr. Shaker Salarilak
Obtained funding: Dr. Shaker Salarilak, Mr. Kolifarhood.
Administrative, technical, or material support: Dr. Shaker Salarilak, Mr. Kolifarhood,
Study supervision: Dr. Shaker Salarilak, Dr. Khorasani-Zavareh
References
- [1].World Health Organization Tuberculosis MDR-TB and XDR-TB 2008 Report. Available from: URL: < www.who.int/tb> (Cited 6.11.2010).
- [2].Uplekar M, Pathania V, Raviglione M. Private practitioners and public health: weak links in tuberculosis control. Lancet. 2001;358:912–6. doi: 10.1016/s0140-6736(01)06076-7. [DOI] [PubMed] [Google Scholar]
- [3].World Health Organization Tuberculosis control in the Eastern Mediterranean Region. Available from: URL: < www.who.EM/TUB/256/E>.
- [4].Lawson L, Yassin MA, Abdurrahman ST, Parry CM, Dacombe R, Sogaolu OM, et al. Resistance to first-line tuberculosis drugs in three cities of Nigeria. Trop Med Int Health. 2011;8:974–80. doi: 10.1111/j.1365-3156.2011.02792.x. [DOI] [PubMed] [Google Scholar]
- [5].World Health Organization . World Health Organization; 2013. Multidrug-resistant tuberculosis (MDR-TB) 2013. Available from: URL: < www.who.int/tb> (Cited: GTB number C7). [Google Scholar]
- [6].Frieden TR, Sbarbaro JA. Promoting adherence to treatment for tuberculosis: the importance of direct observation. Bull World Health Organiz. 2007;85:407–9. doi: 10.2471/blt.06.038927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Volmink J, Garner P. [Directly observed therapy for treating tuberculosis] Cochrane Database Syst Rev. 2006;2:CD003343. doi: 10.1002/14651858.cd003343.pub2. [DOI] [PubMed] [Google Scholar]
- [8].Kranzer K, Lawn SD, Meyer-Rath G, Vassall A, Raditlhalo E, Govindasamy D, et al. Feasibility, yield, and cost of active tuberculosis Case finding linked to a mobile HIV service in cape town, South Africa: a cross-sectional study. PLoS Med. 2012;9:e1001281. doi: 10.1371/journal.pmed.1001281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].World Health Organization . World Health Organization; 2005. Addressing poverty in TB control-Options for national TB control programmes. WHO/HTM/TB/2005.352. [Google Scholar]
- [10].Shargie EB, Lindtjørn B. Determinants of treatment adherence among smear-positive pulmonary tuberculosis patients in southern Ethiopia. PLoS Med. 2007;4:e37. doi: 10.1371/journal.pmed.0040037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Comolet TM, Rakotomalala R, Rajaonarioa H. Factors determining compliance with tuberculosis treatment in an urban environment, Tamatave, Madagascar. Int J Tuberc Lung Dis. 1998;11:891–7. [PubMed] [Google Scholar]
- [12].Randremanana RV, Richard V, Rakotomanana F, Sabatier P, Bicout DJ. [Bayesian mapping of pulmonary tuberculosis in Antananarivo, Madagascar] BMC Infect Dis. 2010;10:21. doi: 10.1186/1471-2334-10-21. Available from: URL: < http://www.biomedcentral.com/1471-2334/10/21>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Boateng SA, Kodama T, Sata F, Bonsu G, Osawa E. Community-involved strategy to improve tuberculosis (TB) treatment outcomes in Eastern Region of Ghana. J Nat Inst Public Health. 2012;61:357–65. [Google Scholar]
- [14].Mahendradhata Y, Lambert M, Van Deun A, Matthys F, Boelaert M, Van der Stuyft P. Strong general health care systems: a prerequisite to reach global tuberculosis control targets. Int J Health Plann Manag. 2003;18:S53–65. doi: 10.1002/hpm.724. [DOI] [PubMed] [Google Scholar]
- [15].Merza MA, Farnia P, Tabarsi P, Khazampour M, Masjedi MR, Velayati AA. Anti-tuberculosis drug resistance and associated risk factors in a tertiary level TB centre in Iran: a retrospective analysis. J Infect Dev Countries. 2011;5:511–9. doi: 10.3855/jidc.1259. [DOI] [PubMed] [Google Scholar]
- [16].Mesgari MS, Masoomi Z. GIS applications in public health as a decision making support system and its limitation in Iran. World Appl Sci J. 2008;3:73–7. [Google Scholar]
- [17].Shamaei M, Marjani M, Chitsaz E, Kazempour M, Esmaeili M, Farnia P, et al. First-line anti-tuberculosis drug resistance patterns and trends at the national TB referral center in Iran-eight years of surveillance. Int J Infect Dis. 2009;13:e236–40. doi: 10.1016/j.ijid.2008.11.027. [DOI] [PubMed] [Google Scholar]
- [18].Statistical Center of Iran National portal of statistics. 2010 Mar 1; Available from: URL: < http://www.amar.org.ir/Default.aspx?tabid=552>.
- [19].Zeynalzadeh R, Borzouian S, Ghajari AR. Determine of the Status of Provinces in case of Human Development Indicators in Education, 1997–2009 in period. Q J Hum Geogr. 2012;4:63–81. [Google Scholar]
- [20].Mobaraki O, Abdoli A. The hierarchy analysis of Urmia city zones based on urban sustainable development indexes. J Appl Res Geogr Sci. 2013;13:49–65. [Google Scholar]
- [21].World Health Organization . Geneva, Switzerland: World Health Organization; 2010. Global Tuberculosis Control: Global, Regional and country specific data for key indicators. WHO/HTM/TB/2010.7. [Google Scholar]
- [22].Kolifarhood G, Salarilak S, Dastgiri S, Mikaili P, Khorasani-Zavareh D, Khosravi N, et al. Trends and socio-demographic determinants of pulmonary and extra pulmonary tuberculosis disease in West Azerbaijan Province and Iran. J Appl Environ Biol Sci. 2012;2:560–6. [Google Scholar]
- [23].Comolet TM, Rakotomalala R, Rajaonarioa H. Factors determining compliance with tuberculosis treatment in an urban environment, Tamatave, Madagascar. Int J Tuberc Lung Dis. 1998;2:891–7. [PubMed] [Google Scholar]
- [24].Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Victor O, Ombeka VO, et al. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: A case control study. BMC Public Health. 2011;11:696. doi: 10.1186/1471-2458-11-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Dooley KE, Lahlou O, Ghali I, Knudsen J, Elmessaoudi MD, Cherkaoui I, et al. Risk factors for tuberculosis treatment failure, default, or relapse and outcomes of retreatment in morocco. BMC Public Health. 2011;11:140. doi: 10.1186/1471-2458-11-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kamel MI, Rashed S, Foda N, Mohie A, Loutfy M. Gender differences in health care utilization and outcome of respiratory tuberculosis in Alexandria. Eastern Mediterr Health J. 2003;9:741–56. [PubMed] [Google Scholar]
- [27].Munch Z, Van Lill WP, Booysen CN, Zietsman HL, Enarson DA, Beyers N. Tuberculosis transmission patterns in a high-incidence area: a spatial analysis. Int J Tuberc Lung Dis. 2003;7:271–7. [PubMed] [Google Scholar]
- [28].Vendramini SH, Santos ML, Gazetta CE, Chiaravalloti-Neto F, Ruffino-Netto A, Villa TC. Tuberculosis risks and socio-economic level: a case study of a city in the Brazilian south-east, 1998–2004. Int J Tuberc Lung Dis. 2006;10:1231–5. [PubMed] [Google Scholar]
- [29].Ximenes RA, Albuquerque M, Souza WA, Montarroyos UR, Diniz GT, Luna CF, et al. Is it better to be rich in a poor area or poor in a rich area? A multilevel analysis of a case-control study of social determinants of tuberculosis. Int J Epidemiol. 2009:1–10. doi: 10.1093/ije/dyp224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Murray EJ, Marais BJ, Mans G, Beyers N, Ayles H, Godfrey-Faussett P, et al. Multidisciplinary method to map potential tuberculosis transmission ‘hot spots’ in high-burden communities. Int J Tuberc Lung Dis. 2009;13:767–74. [PubMed] [Google Scholar]
- [31].Randremanana RV, Sabatier P, Rakotomanana F, Arthur Randriamanantena A, Richard V. Spatial clustering of pulmonary tuberculosis and impact of the care factors in Antananarivo City. Trop Med Int Health. 2009;14:429–37. doi: 10.1111/j.1365-3156.2009.02239.x. [DOI] [PubMed] [Google Scholar]
- [32].Yeh YP, Chang HJ, Yang J, Chang SH, Suo J, Chen TH. Incidence of tuberculosis in mountain areas and surrounding townships: dose-response relationship by geographic analysis. AEP. 2005;15:526–32. doi: 10.1016/j.annepidem.2004.08.005. [DOI] [PubMed] [Google Scholar]
- [33].Tanser FC. The application of GIS technology to equitably distribute fieldworker workload in a large, rural South African health survey. Trop Med Int Health. 2002;7:80–90. doi: 10.1046/j.1365-3156.2002.00825.x. [DOI] [PubMed] [Google Scholar]
- [34].Jacobson LM, Garcia-Garcia MD, Hernandez-Avila JE, Cano-Arellano B, Small PM, Sifuentes-Osornio J, et al. Changes in the geographical distribution of tuberculosis patients in Veracruz, Mexico, after reinforcement of a tuberculosis control programme. Trop Med Int Health. 2005;10:305–11. doi: 10.1111/j.1365-3156.2005.01392.x. [DOI] [PubMed] [Google Scholar]
- [35].Randremanana RV, Sabatier P, Rakotomanana F, Randriamanantena A, Richard V. Spatial clustering of pulmonary tuberculosis and impact of the care factors in Antananarivo City. Tropical Med Int Health. 2009;14:429–37. doi: 10.1111/j.1365-3156.2009.02239.x. [DOI] [PubMed] [Google Scholar]
- [36].MOHME . Achievements, challenges and landscape towards health system of Islamic Republic of Iran. Tehran, Iran: Iran Ministry of Health and Medical Education; 2010. [Google Scholar]
- [37].Mathema B, Pande SB, Jochem K, Houston RA, Smith I, Bam DS, et al. Tuberculosis treatment in Nepal: a rapid assessment of government centers using different types of patient supervision. Int J Tuberc Lung Dis. 2001;5:912–9. [PubMed] [Google Scholar]
- [38].Okanurak K, Kitayaporn D, Wanarangsikul W, Koompong C. Effectiveness of DOT for tuberculosis treatment outcomes: a prospective cohort study in Bangkok Thailand. Int J Tuberc Lung Dis. 2007;11:762–8. [PubMed] [Google Scholar]
- [39].Hasker E, Khodjikhanov M, Usarova S, Asamidinov U, Yuldashova U, Werf MJ, et al. Default from tuberculosis treatment in Tashkent, Uzbekistan; Who are these defaulters and why do they default? BMC Infect Dis. 2008;8:97. doi: 10.1186/1471-2334-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Thiam S, LeFevre AM, Hane F, Ndiaye A, Ba F, Fielding KL, et al. Effectiveness of a strategy to improve adherence to tuberculosis treatment in a resource-poor setting: a cluster randomized controlled trial. JAMA. 2007;297:380–6. doi: 10.1001/jama.297.4.380. [DOI] [PubMed] [Google Scholar]
- [41].Shadpour K. Primary health care networks in the Islamic Republic of Iran. Eastern Mediterr Health J. 2000;6:822–5. [PubMed] [Google Scholar]
- [42].Tavassoli M. Iranian health houses open the door to primary care. Bull World Health Organ. 2008;86:585–6. doi: 10.2471/blt.08.030808. [DOI] [PMC free article] [PubMed] [Google Scholar]