Highlights
-
•
Examined how COVID-19 psychological stressors are linked with drinking behavior.
-
•
Also evaluated whether these links are different for men and women.
-
•
COVID-19 psychological distress was consistently related to alcohol use indices.
-
•
This pattern was significant only among women for quantity.
-
•
This pattern was not different for men and women for drinking frequency.
Keywords: Alcohol use, Heavy drinking episodes, Coronavirus, Stress
Abstract
The 2019 Coronavirus pandemic has brought about significant and unprecedented changes to the modern world, including stay-at-home orders, high rates of unemployment, and more than a hundred thousand deaths across the United States. Derived from the self-medication hypothesis, this research explored how perceived threat and psychological distress related to the COVID-19 pandemic are associated with drinking behavior among an American sample of adults. We also evaluated whether links between COVID-19-related perceived threat and psychological distress with drinking behavior are different for men and women. Participants (N = 754; 50% women) completed an online Qualtrics Panels study between April 17th and 23rd, 2020. Results suggested that psychological distress related to the COVID-19 pandemic was consistently related to alcohol use indices, and moderation results indicated this pattern was significant only among women for number of drinks consumed during the recent heaviest drinking occasion and number of drinks consumed on a typical evening. COVID-related distress’ link to frequency of drinking and heavy drinking episodes was not different for men and women. Our results suggest that continued monitoring, particularly among women, should be conducted as this pandemic continues to evolve to identify the long-term public health impacts of drinking to cope with COVID-19 distress.
1. Introduction
Towards the end of 2019, a previously unidentified coronavirus — severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) — was identified in Wuhan, Hubei Province, China (Sangeeta & Deepjyoti, 2020). The disease associated with this novel coronavirus strain eventually became ubiquitously known as the Coronavirus Disease 2019 (NIH, 2020). COVID-19 quickly spread globally, sparking widespread international public health concerns, and ultimately was deemed a pandemic (World Health Organization, 2020). In attempts to control the pandemic, governments across the world, including the United States (U.S.), implemented social distancing and stay-at-home measures which have resulted in millions of people being isolated at home. These ongoing disease containment strategies are unprecedented in the modern world, and very little is known of their effects on the health and well-being of adults in the U.S.
Over the past three decades, studies have shown that survivors of other types of community-wide disasters (including both natural disasters and acts of terrorism) suffer from both mental health problems and substance misuse. Specifically, research indicates that such community-wide disasters are prospectively linked to numerous behavioral health outcomes, including increased mental health concerns (Boscarino et al., 2011, Breslau et al., 2003, Nandi et al., 2005, Rohrbach et al., 2009, Vetter et al., 2008, Walsh et al., 2014) and escalations in use of alcohol (Flory et al., 2009, North et al., 2011).
Many scientists have predicted that the social distancing, stay-at-home orders, and quarantine measures society has undertaken as public health strategies for disease containment during this current pandemic will inadvertently lead to worsened mental health and increased substance misuse (Holmes et al., 2020) as we have seen with other disasters. A recent article in The Lancet similarly suggested that alcohol use during this pandemic may be a major public health concern (Clay & Parker, 2020). Indeed, data from prior pandemics as well as emerging data from the current COVID-19 crisis support these predictions. A recent rapid review (Brooks et al., 2020) identified 24 studies of the psychological impact of pandemic-related quarantine. High rates of psychological difficulties were observed including fear, nervousness, stress, depression, and irritability. They concluded that quarantine has negative psychological effects that can be severe and persistent for some (Brooks et al., 2020). Sprang and Silman (2013) studied psychological reactions to a pandemic disaster among those with exposure to varying disease containment strategies. Posttraumatic stress, a particularly severe form of psychological distress, was higher in those who had been quarantined with 25% meeting diagnostic criteria for posttraumatic stress disorder (Sprang & Silman, 2013). Studies emerging on psychological reactions to COVID-19 suggest that the pandemic is severely affecting mental health worldwide. For example, a general population study of psychological reactions to COVID-19 in Italy showed that ~20% experienced mild psychological distress with another ~20% showing moderate-to-severe distress from the pandemic (Moccia et al., in press). Zhu et al. (2020) found that COVID-19 quarantine in China was much more likely to lead to psychological distress among those for whom the quarantine had the greatest impact on daily life.
Research is also emerging that pandemics can have important impacts on drinking and substance use behavior. In March 2020, during the COVID-19 pandemic and while many Americans were under a stay-at-home order, market research by Nielsen showed that alcohol sales increased by 55% relative to the same time last year (Bremner, 2020). A recent Nanos poll similarly showed that Canadians are drinking more alcohol during the COVID-19 pandemic-related quarantine (Canadian Centre on Substance Use and Addiction, 2020). The largest increases were observed in 35–54-year-olds, where 25% acknowledged that they had increased their alcohol use during the pandemic, with 44% attributing this change to stress (Canadian Centre on Substance Use and Addiction, 2020). Longitudinal research in China during SARS concerningly indicated that some respondents who began abusing substances during the pandemic showed persistent substance abuse that lasted well beyond the pandemic (Wu et al., 2009).
There are several explanations for why alcohol use might increase during a pandemic and the associated restrictive disease-containment strategies (e.g., boredom, disruption to routines, distress). The Self-Medication Hypothesis posits that the use of certain substances, like alcohol, acutely relieves psychological suffering (Khantzian, 1997). Thus, many adults may use substances such as alcohol to cope with the perceived threat and/or psychological distress (Boschi et al., 2000, Stewart, 1996) associated with the COVID-19 pandemic. While potentially effective in the shorter-term, self-medication is typically seen as an avoidance coping strategy, which may paradoxically maintain or even increase distress in the longer term (see Stewart et al., 2016, for review). This type of coping-related drinking is also associated with risk for development of alcohol-related problems (Cooper et al., 2016). Given that during COVID-19-related social distancing, individuals may be faced with increased stress and uncertainty (Taylor, 2019) as well as anxiety and depressive symptoms (Brooks et al., 2020), those who experience more perceived threat and/or psychological distress may be those most likely to use alcohol to cope.
Outside of the context of a global pandemic, alcohol misuse is one of the leading causes of preventable death, contributing annually to ~three million deaths worldwide (NIAAA, 2020). In the U.S., nearly one in six adults engages in heavy episodic drinking (HED; i.e., consuming at least five drinks for men or four drinks for women in the span of two hours) (SAMHSA, 2018) four times per month, where they consume, on average, 7 drinks per episode (Kanny et al., 2018). While HED is most common in younger adults age 18–34, more than half of the total drinks consumed are by those age 35 and older (Kanny et al., 2018). Aside from acute consequences of heavy alcohol use such as alcohol poisoning and blackouts (White et al., 2018), there is the potential that for some, longer-term alcohol misuse might escalate into a full-blown alcohol use disorder.
1.1. Gender differences in self-medication
There are some important gender differences relevant to the self-medication hypothesis in the context of the COVID-19 pandemic. First, women are more likely than men to experience comorbid emotional (i.e., anxiety, depression, and PTSD) and alcohol use disorders (see Stewart et al., 2009, for a review). Second, some research suggests that women are more vulnerable to experiencing psychological distress from the pandemic (see reviews by Brooks et al., 2020, Taylor, 2019), suggesting women may be more motivated than men to drink to cope with pandemic-related distress. Indeed, the consensus from both human and animal studies is that women are more likely than men to drink in response to stress (e.g., Becker and Koob, 2016, Koob and White, 2017, Peltier et al., 2019). For example, the largest drinking motives study to date suggests that coping motives are more important for women’s than men’s drinking (Kuntsche et al., 2015).
The current study built upon emerging research demonstrating the COVID-19 pandemic is impacting both psychological distress and drinking behavior, by testing predictions derived from the self-medication hypothesis. A secondary goal was to determine whether such associations are stronger in women compared to men. Given that psychological distress and mental health concerns are prominent risk factors for the onset and maintenance of alcohol misuse and the fact that the potential public health effects of long-term social isolation on alcohol use and misuse are unknown, understanding the links of perceived threat/psychological distress with alcohol use patterns during COVID-19 is warranted.
The present study had the following primary hypotheses: (1) COVID-19-related perceived threat and psychological distress would be associated with alcohol consumption such that individuals who report more COVID-19-related perceived threat and psychological distress would also report higher levels of drinking behaviors during the past month; and (2) these associations would be moderated by gender such that the association between COVID-19-related perceived threat/psychological distress with alcohol consumption would be stronger among women compared to men.
2. Method
2.1. Participants and procedure
Participants included 754 individuals (50% [n = 377] women; 50% [n = 377 men1 ]) in the U.S. who were on average 41.7 years of age (SD = 10.39). Most (85.7%) were married, with another 10.0% in an exclusive relationship/with a life partner, and 4.3% engaged. On average, participants had been romantically involved with their partner for 10.0 (SD = 7.2) years. Most participants (84.2%) were White, with 6.1% Black, 4.2% Asian, 1.3% Native American/American Indian, 0.5% Native Hawaiian/Pacific Islander, 1.3% Multiracial, and 2.3% Other. Ten percent (10.2%) reported Hispanic ethnicity. Most participants (91.8%) identified as heterosexual, with another 5.0% bisexual, 2.4% homosexual, and 0.9% pansexual/other. Approximately two-thirds (67.8%) reported having children living at home with them at the time of the survey2 .
Qualtrics Panels is a survey management service wherein participants are recruited from a large pool of potential subjects based on criteria specified by the researcher. Qualtrics respondents completed the online survey through Qualtrics Panels between April 17 and April 23, 2020. Participants provided informed consent and were screened for eligibility. Eligible panel respondents met the following criteria: (a) at least 18 years of age; (b) consumed at least 12 alcoholic beverages in the last 12 months; (c) worked at least 20 h per week; (d) romantically involved with their current romantic partner for at least six months; and (e) cohabiting with that romantic partner. The panel was also split evenly by gender with 50% men and 50% women.
Participants who met eligibility criteria (N = 4,335) began the survey and were asked a series of questions about their demographics, alcohol use, and thoughts and feelings about the current COVID-19 pandemic. Two filter questions were included where participants were asked to select a specific answer (e.g., “Disagree a little”) to determine if they were paying attention and thus assess survey validity (Oppenheimer et al., 2009). There was also one speeder check performed by Qualtrics. Participants who failed the filter questions or speeder check (n = 3581) were immediately screened out and not included in analyses. Thus, results are presented only for the participants (N = 754) who passed the attention filters. Participants were compensated via Qualtrics according to their guidelines. Qualtrics was paid by the researchers at a rate of $6USD per subject, but the actual payment amount from Qualtrics to respondents was between $3 and $4. Study procedures were approved by the University IRB.
The timeframe for data collection (which asked about past month drinking, assessed between April 17–23, 2020) largely overlapped with COVID-19 closures of schools and implementation of “stay-at-home” orders issued by governors requiring individuals to stay home except for essential activities. For example, on March 15, 2020, school closures began in 29 states and the Centers for Disease Control and Prevention released guidelines recommending that for the next 8 weeks, “organizers (whether groups or individuals) cancel or postpone in-person events that consist of 50 people or more throughout the United States.” Beginning with California on March 19th and through April 7th with South Carolina, 42 states had issued stay-at-home orders (Kates et al., 2020).
3. Measures
3.1. COVID-19 stressors
Perceived threat related to COVID-19 was assessed with the Perceived Coronavirus Threat Questionnaire – Short version (Conway et al., 2020). This measure included three items: “Thinking about the coronavirus (COVID-19) makes me feel threatened,” “I am afraid of the coronavirus (COVID-19),” and “I am stressed around other people because I worry I’ll catch the coronavirus (COVID-19)” (α = 0.91). Psychological distress related to COVID-19 was assessed with the Psychological subscale of the Coronavirus Impacts Questionnaire – Short version (Conway et al., 2020). This included two items: “I have become depressed because of the coronavirus (COVID-19)” and “The coronavirus (COVID-19) outbreak has impacted my psychological health negatively” (α = 0.90).3
3.2. Alcohol use
To capture alcohol use during the pandemic, all alcohol questions asked about past month drinking. The Quantity/Frequency/Peak Alcohol Use Index (QF; Dimeff, 1999) was used to assess peak and typical drinks and drinking frequency. Number of drinks drinks on the heaviest occasion was measured by asking how many drinks individuals consumed on the occasion they drank the most in the past month. Responses ranged from 0 to 25+ (coded as 25). Number of drinks on a typical occasion was measured by asking how many drinks respondents drank on a typical evening in the past month. Responses ranged from 0 to 25+ (coded as 25). Drinking frequency was assessed by asking how many days of the week respondents drank in the past month (0 = I did not drink at all, 0.5=<once/month, 1 = once/month, 2 = two times/month, 3 = three times/month, 4 = once/week, 8 = twice/week, 12 = three times/week, 16 = four times/week, 20 = five times/week, 24 = six times/week, and 30 = every day). We also assessed the frequency of heavy drinking episodes by asking how many times in the past month participants had consumed more than 4 drinks (if a woman) or 5 drinks (if a man) within ~2 h. All questions referenced alcohol use during the past month, which would have overlapped completely with COVID-19.
3.3. Analytic plan
Given the non-normal (count) distribution of the drinking outcome variables, negative binomial regression models were used in all analyses (Hilbe, 2011). Covariates were selected based on their previously established associations with drinking behavior (i.e., age (Moore et al., 2005), gender (Erol & Karpyak, 2015; coded 0 = woman, 1 = man), and presence of children in the home (Bowden et al., 2019; coded 0 = no child at home, 1 = one or more children at home). as well as whether or not participants reported there was a ‘stay-at-home’ order in place in their location when the survey was taken (0 = no order in effect, 1 = order in effect).
Main effects were included in a first step and interactions were included in a second step. Moderation models evaluated whether the COVID-19-related predictors (perceived threat and psychological distress) were differentially related to drinking for men and women by examining the gender × COVID-19-related predictor interaction terms. Significant interactions were decomposed by examining simple slopes of the COVID-19 predictors for men and women separately. Simple slopes in negative binomial regression models are represented by rate ratios because log-linked coefficients are exponentiated for interpretation. Rate ratios represent the proportion of change in the dependent variable for each unit increase in the predictor. For example, a rate ratio of 1.15 represents a 15% increase in the alcohol-related outcome, whereas a rate ratio of 0.85 represents a 15% decrease in the alcohol-related outcome, for each one-unit increase in the predictor. While we report significance at traditional levels (i.e. p-value < 0.05), we also report whether effects are maintained after a Bonferroni correction (i.e., 4 tests: critical p-value = 0.0125) to enhance confidence in the findings.
4. Results
4.1. Descriptive statistics and preliminary associations
Descriptive statistics and bivariate correlations for all study variables are presented in Table 1 . Participants consumed, on average, almost six drinks on their heaviest drinking occasion in the past month (SD = 5.84). They reported drinking almost four drinks on a typical occasion (SD = 1.89), on average, and drinking on a mean of approximately 10 days in the last month (SD = 8.94). Participants reported approximately 1.4 heavy drinking episodes in the past month, on average (SD = 1.93). Both COVID-19-related perceived threat and psychological distress showed significant bivariate associations with all four drinking indices. Men and women did not differ in their COVID-19-related perceived threat or psychological distress (ps > 0.30); however, men reported greater drinking on all four indices (ps < 0.01).
Table 1.
Bivariate Correlations among All Study Variables.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Gender | |||||||
| 2. COVID-19-Related Threat | 0.00 | ||||||
| 3. COVID-19 Psychological Distress | 0.04 | 0.56*** | |||||
| 4. Drinks on Heaviest Occasion | 0.18*** | 0.11** | 0.16*** | ||||
| 5. Drinks on Typical Occasion | 0.17*** | 0.15*** | 0.20*** | 0.65*** | |||
| 6. Drinking Days (Past Month) | 0.12*** | 0.17*** | 0.22*** | 0.46*** | 0.47*** | ||
| 7. Number of Heavy Drinking Episodes | 0.20*** | 0.26*** | 0.26*** | 0.45*** | 0.54*** | 0.37*** | |
| Mean | 0.50 | 4.43 | 3.46 | 5.84 | 3.86 | 10.33 | 1.39 |
| SD | 0.50 | 1.89 | 2.01 | 5.70 | 4.09 | 8.94 | 1.93 |
| Range | 0–1 | 1–7 | 1–7 | 0–25 | 0–25 | 0–30 | 0–8 |
* Note. Gender was scored 0 = female, 1 = male.
4.2. Primary analyses
The psychological distress associated with COVID-19 – and not perceived threat of COVID-19 – was significantly related to a greater maximum number of drinks consumed, RR = 1.07, Z = 3.66, p < .001, drinks consumed on a typical occasion, RR = 1.08, Z = 4.06, p < .001, and number of drinking days in the past month, RR = 1.08, Z = 3.72, p < .001. Both psychological distress and perceived threat related to COVID-19 were associated with a greater number of heavy drinking episodes (distress RR = 1.08, Z = 2.57, p = .010, threat RR = 1.16, Z = 4.44, p < .001). The presence of children at home was also related to a higher number of drinks on a typical occasion, RR = 1.18, Z = 2.35, p = .019, as well as a greater number of heavy drinking episodes, RR = 1.67, Z = 4.37, p < .001. All main effects except for children on typical drinking quantity continued to be significant after the Bonferroni correction (Table 2 ).
Table 2.
Negative Binomial Regression Models Evaluating COVID-Related Threat and Psychological Impact on Alcohol Use.
| Step | Predictor | B | SE(b) | Z | p | RR | RR 95% CI |
|---|---|---|---|---|---|---|---|
| Outcome: Peak Number of Drinks on One Occasion | |||||||
| 1 | Stay-at-home order | 0.144 | 0.136 | 1.06 | 0.289 | 1.155 | 0.885, 1.507 |
| Gender | 0.361 | 0.062 | 5.87 | <0.001 | 1.435 | 1.272, 1.619 | |
| Age | −0.007 | 0.003 | −2.32 | 0.020 | 0.993 | 0.987, 0.999 | |
| Children in home | 0.073 | 0.067 | 1.09 | 0.275 | 1.076 | 0.943, 1.227 | |
| COVID-19 threat | 0.015 | 0.019 | 0.76 | 0.449 | 1.015 | 0.977, 1.054 | |
| COVID-19 distress | 0.066 | 0.018 | 3.66 | <0.001 | 1.068 | 1.031, 1.106 | |
| 2 | COVID-19 threat × Gender | −0.050 | 0.039 | −1.30 | 0.192 | 0.951 | 0.882, 1.026 |
| COVID-19 distress × Gender | −0.103 | 0.036 | −2.87 | 0.004 | 0.902 | 0.841, 0.968 | |
| Outcome: Number of Drinks on Typical Occasion | |||||||
| 1 | Stay-at-home order | 0.027 | 0.139 | 0.19 | 0.848 | 1.026 | 0.782, 1.348 |
| Gender | 0.357 | 0.063 | 5.63 | <0.001 | 1.429 | 1.262, 1.351 | |
| Age | −0.004 | 0.003 | −1.16 | 0.248 | 0.996 | 0.990, 1.003 | |
| Children in home | 0.164 | 0.070 | 2.35 | 0.019 | 1.179 | 1.028, 1.351 | |
| COVID-19 threat | 0.031 | 0.021 | 1.49 | 0.137 | 1.031 | 0.990, 1.074 | |
| COVID-19 distress | 0.076 | 0.019 | 4.06 | <0.001 | 1.079 | 1.040, 1.120 | |
| 2 | COVID threat × Gender | −0.014 | 0.041 | −0.35 | 0.729 | 0.986 | 0.910, 1.068 |
| COVID-19 distress × Gender | −0.136 | 0.037 | −3.66 | <0.001 | 0.873 | 0.811, 0.939 | |
| Outcome: Number of Days Consuming Alcohol | |||||||
| 1 | Stay-at-home order | −0.007 | 0.148 | −0.05 | 0.960 | 0.993 | 0.743, 1.326 |
| Gender | 0.200 | 0.068 | 2.94 | 0.003 | 1.221 | 1.069, 1.396 | |
| Age | 0.004 | 0.003 | 1.23 | 0.219 | 1.004 | 0.998, 1.011 | |
| Children in home | 0.021 | 0.075 | 0.28 | 0.781 | 1.021 | 0.881, 1.183 | |
| COVID-19 threat | 0.023 | 0.023 | 1.02 | 0.308 | 1.024 | 0.979, 1.070 | |
| COVID-19 distress | 0.077 | 0.023 | 3.72 | <0.001 | 1.081 | 1.037, 1.126 | |
| 2 | COVID threat × Gender | 0.016 | 0.046 | 0.35 | 0.725 | 1.016 | 0.928, 1.113 |
| COVID-19 distress × Gender | −0.037 | 0.042 | −0.88 | 0.381 | 0.964 | 0.887, 1.047 | |
| Outcome: Number of Heavy Drinking Episodes | |||||||
| 1 | Stay-at-home order | −0.095 | 0.220 | −0.43 | 0.665 | 0.909 | 0.591, 1.398 |
| Gender | 0.547 | 0.103 | 5.32 | <0.001 | 1.728 | 1.412, 2.114 | |
| Age | −0.035 | 0.005 | −6.38 | <0.001 | 0.966 | 0.955, 0.976 | |
| Children in home | 0.515 | 0.118 | 4.37 | <0.001 | 1.673 | 1.328, 2.108 | |
| COVID-19 threat | 0.149 | 0.034 | 4.44 | <0.001 | 1.161 | 1.087, 1.240 | |
| COVID-19 distress | 0.076 | 0.030 | 2.57 | 0.010 | 1.079 | 1.018, 1.144 | |
| 2 | COVID threat × Gender | −0.132 | 0.068 | −1.94 | 0.053 | 0.877 | 0.767, 1.002 |
| COVID-19 distress × Gender | −0.065 | 0.059 | −1.10 | 0.273 | 0.937 | 0.834, 1.052 | |
* Notes. RR = Rate Ratio. 95% CI = confidence interval of IRR. Gender was coded 0 = female, 1 = male. Statistically significant (p < .05) predictors are bolded.
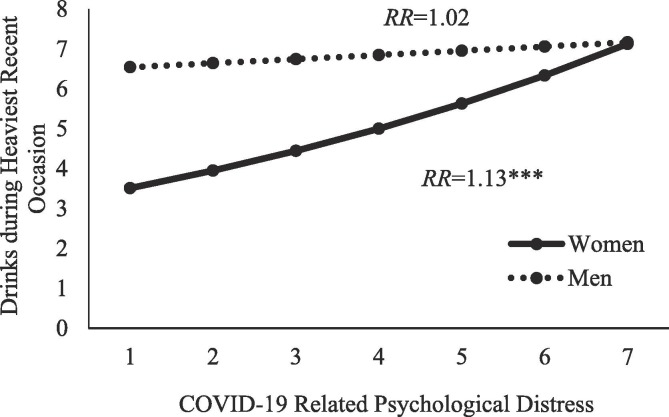
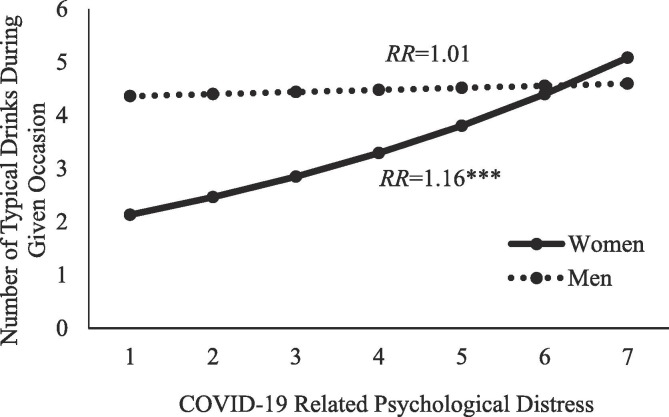
4.3. Moderation by gender
The association between COVID-19 psychological distress and both peak number of drinks and typical number of drinks per occasion were moderated by gender. These interactions were maintained after the Bonferroni correction. COVID-19 psychological distress was not differentially linked to drinking frequency and heavy drinking episodes among men and women. In the case of significant interactions, the same pattern emerged (see Fig. 1, Fig. 2 ). COVID-19 psychological distress was only associated with greater drinking for women (peak drinks RR = 1.13, Z = 4.82, p < .001; typical drinks RR = 1.16, Z = 5.59, p < .001), whereas COVID-19 psychological distress was unrelated to drinking for men (peak drinks RR = 1.02, Z = 0.58, p = .562; typical drinks RR = 1.01, Z = 0.32, p = .746). Thus, every one-unit increase in COVID-19-related psychological distress was associated with a 13% increase in women’s number of drinks consumed during their heaviest drinking occasion and a 16% increase in women’s number of drinks on a typical occasion in the past month.
Fig. 1.
COVID-19 psychological distress associated with peak number of drinks consumed on heaviest recent drinking occasion for women only. RR = Rate ratio. *** p < .001.
Fig. 2.
COVID-19 psychological distress associated with typical number of drinks consumed on a given occasion for women only. RR = Rate ratio. *** p < .001.
5. Discussion
Our results provide preliminary evidence that indices of COVID-19-related stress, particularly psychological distress, are associated with drinking behavior. Further, two of these associations -- the two related to quantity consumed -- are more pronounced for women than men, consistent with previous literature suggesting that the use of alcohol to cope with distress is more relevant to women’s than men’s drinking (Kuntsche et al., 2015). In both interactions, at low levels of COVID-related psychological distress, men display the usual pattern of drinking more than women (Stewart et al., 2009). However, as distress related to COVID-19 increases, women’s drinking “catches up” with or converges with that of the men (see Figures). Gender convergence refers to the observation that women’s drinking has been, over recent decades, catching up with men’s drinking as women face the stressors that were historically the domain of men (e.g., career stressors) (see Stewart et al., 2009). Our results suggest that exposure to a widespread situational stressor (i.e., COVID-19 psychological reactions) is having a similar effect of leading women to catch up to men in terms of their drinking behavior across several different indices. This gender convergence in heavy drinking at high levels of COVID-19-related distress is very concerning given that similar quantities of alcohol in women and men result in greater adverse effects for women (e.g., liver and heart disease) (Stewart et al., 2009). Interestingly, psychological distress related to COVID-19 was similarly related to increased drinking frequency and heavy drinking among men and women, suggesting that while women may drink more on a typical and heavy drinking occasion (peak and typical quantity), both men and women drink more often (in general and heavy drinking) in response to experiencing pandemic-related stress. We need to monitor the drinking quantity particularly in response to pandemic-related distress among women and the drinking frequency and heavy drinking frequency of those experiencing pandemic-related distress regardless of their gender.
While not a primary hypothesis, results also suggest that the presence of children in the home during the pandemic is related to increased drinking behavior among American adults. Although contrary to pre-pandemic research indicating that parents are less likely than non-parents to exceed guidelines for both lifetime and short-term alcohol risk (Bowden et al., 2019), our finding is particularly interesting given the increased burden that many parents are feeling as they navigate their own job as well as home-schooling their children. It is possible that having children in the home to care for and educate during the pandemic increases role overload, which has been linked previously with heavier alcohol use (Abbey et al., 1993). Indeed, prior research suggests that having children at home during the pandemic increases psychological distress (Kisely et al., 2020, Shevlin et al., 2020), which our results link to more frequent and heavier drinking.
5.1. Limitations and future directions
Despite making important contributions to the field, this study is not without limitations. First, our cross-sectional design precludes making assumptions about temporality or causality of the association between COVID-19-related stressors and drinking. Further, given this data was collected close to the start of social distancing measures in the U.S., we may not have captured routine behavior established once people have settled into the new reality of the pandemic and social distancing. Future research should continue to look at alcohol use trends across time as the pandemic continues to affect daily life. Further, a more comprehensive assessment of COVID-related threat and psychological distress would provide a more nuanced evaluation of what specific aspects of the pandemic experience are most strongly related to drinking behavior. Additionally, this sample comprised American adults cohabiting with a romantic partner, who were already regular drinkers, and who worked at least 20 h per week, which may limit generalizability of the results. Moreover, we cannot rule out that the greater reactivity of women’s drinking to the COVID-19 stressors was secondary to greater “room to move” in the women’s drinking data; however, this seems unlikely given that the men’s average values on the four drinking indices were nowhere close to ceiling (see Table 1 for means). Finally, while the pattern of findings is consistent with predictions emerging from the Self-Medication Hypothesis (Khantzian, 1997), we did not assess drinking motives during the pandemic period; future studies should directly assess the relations of COVID-19-related psychological distress with coping-motivated drinking (Cooper et al., 2016).
In support of previous literature, including a recent correspondence published in The Lancet suggesting that alcohol use during this pandemic may be a major public health concern (Clay & Parker, 2020), our results validate that mental health and associated alcohol use during the pandemic are of worthy of attention. As the pandemic continues to evolve, continued monitoring should be conducted, particularly among women. Ongoing monitoring will help determine the long-term mental health and alcohol-related public health impacts of the COVID-19 pandemic among adults, particularly in light of previous findings from SARS that increases in substance use to cope with the pandemic may persist beyond the pandemic (Wu et al., 2009).
6. Role of funding sources
This research was funded by the University of South Florida.
7. Author agreement
None of the original material contained in the manuscript has been published or submitted for publication elsewhere. All authors have approved the manuscript for submission, made substantial contributions to the conception, design, gathering, and/or interpretation of the data, and to the writing and intellectual content of the article.
CRediT authorship contribution statement
Lindsey M. Rodriguez: Conceptualization, Methodology, Software, Formal analysis, Writing - original draft, Project administration. Dana M. Litt: Conceptualization, Formal analysis, Writing - original draft. Sherry H. Stewart: Methodology, Writing - original draft, Project administration.
Footnotes
One person identified as transgender man and was coded as a man.
We tested for gender differences in demographics: Men and women were not different in age, relationship status, race, or ethnicity (all ps>0.05). Men and women did report differences in relationship length, sexual orientation, and presence of children in the household. Women reported being in relationships of longer length than men, t(7 5 2)=3.26, p=.001. Of those identifying as a sexual minority, a greater proportion were women (67%) compared to men (33%), χ2(1)=7.13, p=.008. Women and men also reported differences in the presence of children, χ2(1)=17.06, p<.001. Among those with children in the home, 55% were men and 45% were women.
We ran an exploratory principal components analysis on these five COVID-19 stress items in our total sample (N=754). A two-factor solution explained 87.7% of the variability in item scores. Examining the factor pattern matrix following oblique (oblimin) rotation indicated that the three COVID-19 perceived threat items showed strong salient loadings on the first factor (loadings ranging from 0.832 to 0.990) and negligible loadings on the second factor (loadings ranging from -0.100 to 0.137); the two COVID-19 psychological distress items showed strong salient loadings on the second factor (loadings ranging from 0.943 to 0.955) and negligible loadings on the first factor (loadings ranging from -0.002 to 0.018). The two factors were moderately intercorrelated (r = 0.552). These results show that perceived threat and psychological distress due to COVID-19 are indeed distinct constructs.
References
- Abbey A., Smith M.J., Scott R.O. The relationship between reasons for drinking alcohol and alcohol consumption: An interactional approach. Addictive Behaviors. 1993;18(6):659–670. doi: 10.1016/0306-4603(93)90019-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker J.B., Koob G.F. Sex differences in animal models: Focus on addiction. Pharmacological Reviews. 2016;68(2):242–263. doi: 10.1124/pr.115.011163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino J.A., Kirchner H.L., Hoffman S.N., Sartorius J., Adams R.E. PTSD and alcohol use after the World Trade Center attacks: A longitudinal study. Journal of Traumatic Stress. 2011;24(5):515–525. doi: 10.1002/jts.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschi S., Adams R.E., Bromet E.J., Lavelle J.E., Everett E., Galambos N. Coping with psychotic symptoms in the early phases of schizophrenia. American Journal of Orthopsychiatry. 2000;70(2):242–252. doi: 10.1037/h0087710. [DOI] [PubMed] [Google Scholar]
- Bowden J.A., Delfabbro P., Room R., Miller C., Wilson C. Parental drinking in Australia: Does the age of children in the home matter? Drug and Alcohol Review. 2019;38(3):306–315. doi: 10.1111/dar.12875. [DOI] [PubMed] [Google Scholar]
- Bremner J. Newsweek; 2020. U.S. alcohol sales increase 55 percent in one week amid coronavirus pandemic. [Google Scholar]
- Breslau N., Davis G.C., Schultz L.R. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60(3):289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Centre on Substance Use and Addiction. (2020). COVID-19 and Increased Alcohol Consumptions: NANOS Poll Summary Report. CCSA. Canadian Centre on Substance Use and Addiction.
- Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? The Lancet Public Health. 2020;5(5) doi: 10.1016/s2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway, L. G., III, Woodard, S. R., & Zubrod, A. (2020). Social psychological measurements of COVID-19: Coronavirus perceived threat, government response, impacts, and experiences questionnaires. https://doi.org/10.31234/osf.io/z2x9a.
- Cooper L.M., Kuntsche E., Levitt A., Barber L.L., Wolf S. Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In: Sher K.J., editor. Vol. 1. Oxford University Press; 2016. pp. 375–421. (The Oxford handbook of substance use and substance use disorders). [DOI] [Google Scholar]
- Dimeff L.A. Guilford Press; 1999. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. [Google Scholar]
- Erol A., Karpyak V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug and Alcohol Dependence. 2015;156:1–13. doi: 10.1016/j.drugalcdep.2015.08.023. [DOI] [PubMed] [Google Scholar]
- Flory K., Hankin B.L., Kloos B., Cheely C., Turecki G. Alcohol and cigarette use and misuse among Hurricane Katrina survivors: Psychosocial risk and protective factors. Substance Use and Misuse. 2009;44(12):1711–1724. doi: 10.3109/10826080902962128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbe J.M. 2nd ed. Cambridge University Press; 2011. Negative binomal regression. [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/s2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanny D., Naimi T.S., Liu Y., Lu H., Brewer R.D. Annual Total Binge Drinks Consumed by U.S. Adults, 2015. American Journal of Preventive Medicine. 2018;54(4):486–496. doi: 10.1016/j.amepre.2017.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kates, J., Michaud, J., & Tolbert, J. (2020, April 9). When state stay-at-home orders due to coronavirus went into effect. Kaiser Family Foundation. Retrieved June 16 from https://www.kff.org/other/slide/when-state-stay-at-home-orders-due-to-coronavirus-went-into-effect/.
- Khantzian E.J. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob, G. F., & White, A. (2017). Alcohol and the female brain National Conference on Alcohol and Opioid Use in Women & Girls: Advances in Prevention, Treatment, and Recovery Research, Washington D.C., MA. https://www.youtube.com/watch?v=uYVcQ3Ih-VY.
- Kuntsche E., Wicki M., Windlin B., Roberts C., Gabhainn S.N., van der Sluijs W.…Demetrovics Z. Drinking motives mediate cultural differences but not gender differences in adolescent alcohol use. Journal of Adolescent Health. 2015;56(3):323–329. doi: 10.1016/j.jadohealth.2014.10.267. [DOI] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V.…Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore A.A., Gould R., Reuben D.B., Greendale G.A., Carter M.K., Zhou K., Karlamangla A. Longitudinal patterns and predictors of alcohol consumption in the United States. American Journal of Public Health. 2005;95(3):458–465. doi: 10.2105/AJPH.2003.019471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandi A., Galea S., Ahern J., Vlahov D. Probable cigarette dependence, PTSD, and depression after an urban disaster: Results from a population survey of New York City Residents 4 Months after September 11, 2001. Psychiatry: Interpersonal & Biological Processes. 2005;68(4):299–310. doi: 10.1521/psyc.2005.68.4.299. [DOI] [PubMed] [Google Scholar]
- NIAAA. (2020). Alcohol Facts and Statistics. https://www.niaaa.nih.gov/sites/default/files/AlcoholFactsAndStats.pdf.
- NIH. (2020, April 6). COVID-19, MERS & SARS. National Institute of Allergy and Infectious Diseases. https://www.niaid.nih.gov/diseases-conditions/covid-19.
- North C.S., Ringwalt C.L., Downs D., Derzon J., Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Archives of General Psychiatry. 2011;68(2):173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- Oppenheimer D.M., Meyvis T., Davidenko N. Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology. 2009;45(4):867–872. doi: 10.1016/j.jesp.2009.03.009. [DOI] [Google Scholar]
- Peltier M.R., Verplaetse T.L., Mineur Y.S., Petrakis I.L., Cosgrove K.P., Picciotto M.R., McKee S.A. Sex differences in stress-related alcohol use. Neurobiology of Stress. 2019;10(100149) doi: 10.1016/j.ynstr.2019.100149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbach L.A., Grana R., Vernberg E., Sussman S., Sun P. Impact of Hurricane Rita on adolescent substance use. Psychiatry: Interpersonal and Biological Processes. 2009;72(3):222–237. doi: 10.1521/psyc.2009.72.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2018). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration.
- Sangeeta D., Deepjyoti K. Wuhan coronavirus: A fast-emerging global threat. International Journal of Health Research and Medico Legal Practice. 2020;6(1):79–82. doi: 10.31741/ijhrmlp.v6.i1.2020.17. [DOI] [Google Scholar]
- Mason, L., Martinez, A. P., McKay, R., Stocks, T. V., Bennett, P. H., Hyland, P., Karatzias, T., & Bentall, R. P. (2020). Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 Pandemic. https://psyarxiv.com/hb6nq/download/?format=pdf. [DOI] [PMC free article] [PubMed]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Stewart S.H. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120(1):83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart, S. H., Gavric, D., & Collins, P. (2009). Women, girls, and alcohol. In K. T. Brady, S. E. Back, & S. F. Greenfield (Eds.), Women and addiction: A comprehensive handbook (pp. 341-359). Guildford Press.
- Stewart S.H., Grant V.V., Mackie C.J., Conrod P.J. Comorbidity of anxiety and depression with substance use disorders. In: Sher K.J., editor. Vol. 2. Oxford University Press; 2016. pp. 149–186. (The Oxford handbook of substance use and substance use disorders). [DOI] [Google Scholar]
- Taylor S. Scholars Publishing; Cambridge: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Vetter S., Rossegger A., Rossler W., Bisson J.I., Endrass J. Exposure to the tsunami disaster, PTSD symptoms and increased substance use: An Internet based survey of male and female residents of Switzerland. BMC Public Health. 2008;8:92. doi: 10.1186/1471-2458-8-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K., Elliott J.C., Shmulewitz D., Aharonovich E., Strous R., Frisch A.…Hasin D. Trauma exposure, posttraumatic stress disorder and risk for alcohol, nicotine, and marijuana dependence in Israel. Comprehensive Psychiatry. 2014;55(3):621–630. doi: 10.1016/j.comppsych.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A.M., Tapert S., Shukla S.D. Binge drinking: Predictors, patterns, and consequences. Alcohol Research: Current Reviews. 2018;39(1):1–3. doi: 10.35946/arcr.v39.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Coronavirus disease 2019 (COVID-19): Situation report, 79. https://apps.who.int/iris/handle/10665/331720.
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z.…Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, S., Wu, Y., Zhu, C. Y., Hong, W. C., Yu, Z. X., Chen, Z. K., Chen, Z. L., Jiang, D. G., & Wang, Y. G. (2020, Apr 18). The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain, Behavior, and Immunity. https://doi.org/10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed]