Abstract
The COVID-19 pandemic has necessitated increased use of telemedicine for diagnosis and management of musculoskeletal disorders. We describe the virtual/telemedicine encounter and management of a patient with knee pain initially diagnosed as gonarthrosis but that actually resulted from an impending pathologic fracture of the femur. Definitive diagnosis and treatment occurred only after completion of the impending fracture. The multiple factors making telemedicine encounters challenging which contributed to this outcome are highlighted. Orthopedists need awareness of these challenges and must take steps to mitigate the risk of complications possible with continued increased utilization of telemedicine during this pandemic and beyond.
Keywords: Coronavirus, Telemedicine, Orthopedic surgery, Delayed diagnosis, Impending fracture
Intro
Telemedicine or virtual visits (VVs) refers to the treatment of various medical conditions without seeing the patient in person. Encounters conducted over the phone without video imaging to conduct evaluation and management visits are termed telephonic E&M visits. eVisits, like EMR messaging or e-mail, utilize internet-based forms of communication [1], however eVisits must include history taking, diagnosis and intervention [2]. eVisits commonly incorporate both audio and video transmission.
The COVID-19 pandemic has transformed VVs from a technically demanding and rarely-used option into a necessity used by a large proportion of physicians around the world. Our health care system averaged 17 VVs/day prior to the WHO declaration of the pandemic. Since that time, we completed on average 1440 VVs/day (>65,000 cumulative VVs). During this same period our department averaged over 100 VVs/day.
Telemedicine visits have enabled us to continue to evaluate patients while maintaining social distancing and minimizing patient visits to the hospital. However, these technologies are not without risk, as this case illustrates.
Case report
A 65-year-old Spanish-speaking-only female presented to the orthopedic surgery clinic on 01 Apr 2020 for increasing right knee pain. She had been seen by her PCP who obtained radiographs and referred her to the clinic for evaluation of presumed gonarthrosis.
An eVisit (with audio and video interaction) to the orthopedic clinic was planned. However, the patient was not able to engage the video component and it was converted to a telephonic-only visit. No Spanish-interpreter was available, so the patient's children, who were fluent in both English and Spanish, were enlisted to provide translation. The patient reported a history of difficulty with ambulation and pain in her right lower extremity necessitating use of a cane. She couldn't describe the exact nature of the pain, but localized it to the knee and thigh for three months prior to presentation. Her past medical history was significant for morbid obesity (BMI = 45) and a remote history of thyroid cancer treated with complete thyroid resection.
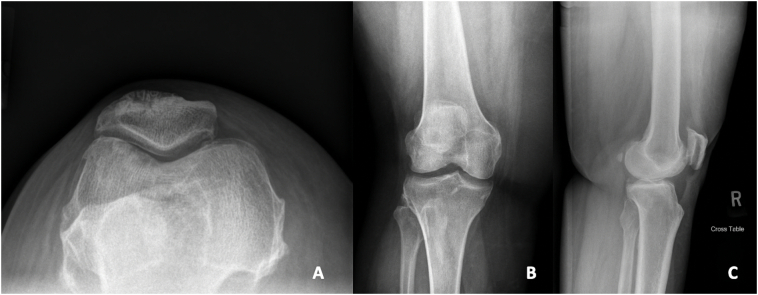
No physical examination was possible because of the virtual nature of the encounter. Three non-weight bearing radiographs of her right knee were evaluated as part of the encounter (Fig. 1). These demonstrated mild arthritic changes of the patellofemoral joint. No appreciable deformity was noted. A diagnosis of mild right knee arthritis was made. Non-operative management including weight loss, NSAIDs and physical therapy to include a home exercise program was decided upon.
Fig. 1.
Knee radiographs. Sunrise (A), anteroposterior (B) and lateral (C) view of the patient's right knee.
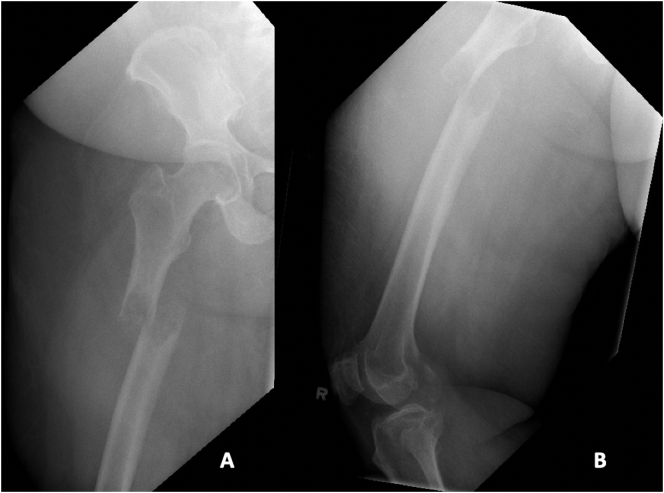
On 13 Apr 2020, while at home the patient twisted her body with a resultant fall, pain in her right thigh, and inability to stand. She was transported to our hospital by emergency services. In the emergency department, her right lower extremity was shortened and her thigh was tender to palpation but her integument and neurovascular exam were intact. Radiographs of her right femur revealed a displaced, oblique subtrochanteric fracture through a lytic lesion (Fig. 2). Further history revealed that her prior thyroid cancer had metastasized to a rib that required resection. Standard lab testing for patients with known skeletal metastases was initiated. She was admitted and a bone scan and skeletal survey was performed to ensure there were no other sites of impending fracture and to identify possible targets for radiation therapy.
Fig. 2.
Anteroposterior (A) and lateral (B) radiographs of the right femur at site of pathologic fracture.
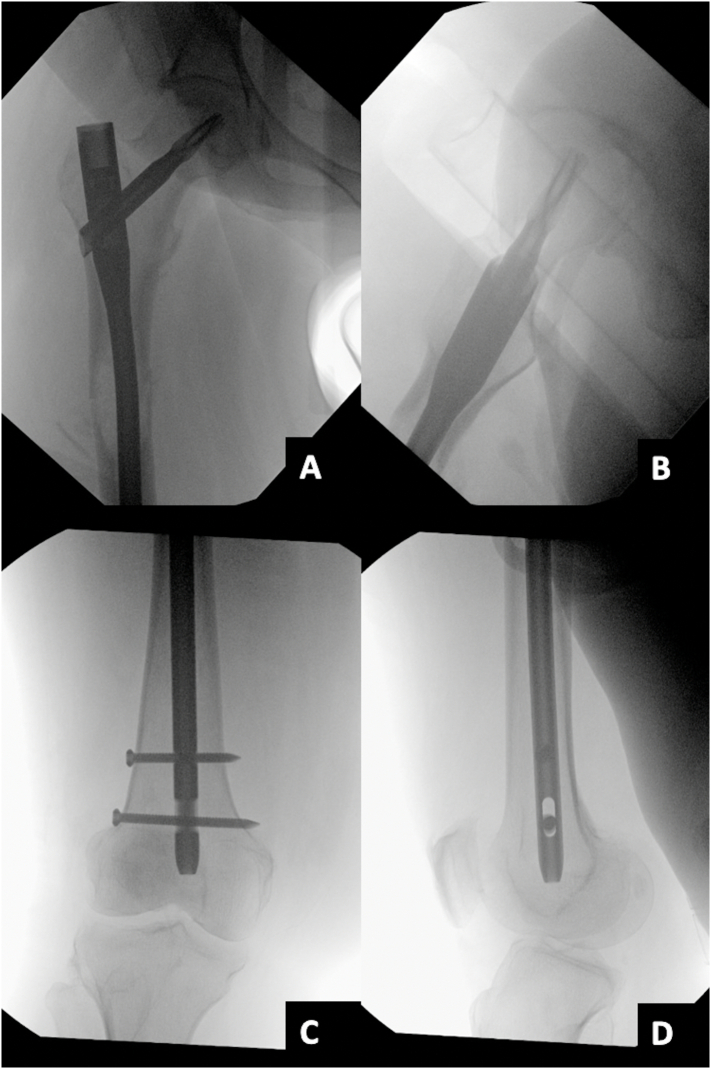
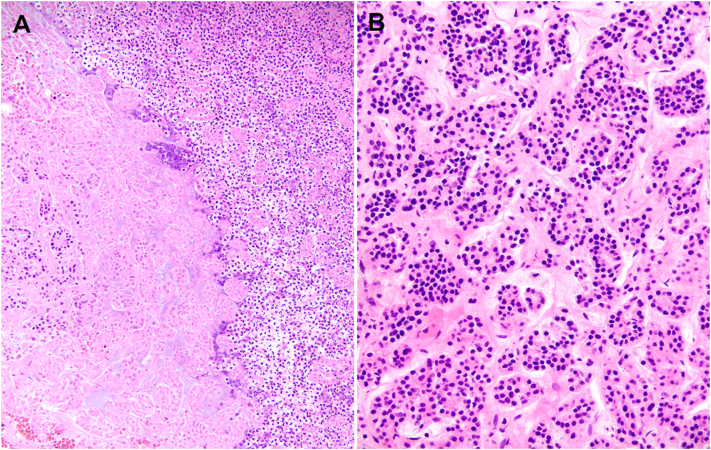
The patient underwent reduction and placement of a cephalomedullary device for fixation of the right femur (Fig. 3). The surgery was un-eventful, and she tolerated it well. During the procedure, a biopsy of the contents of the lytic lesion within the right femur was performed and sent to surgical pathology for gross and microscopic histologic evaluation. This analysis confirmed the diagnosis of metastatic thyroid carcinoma (Fig. 4).
Fig. 3.
Intraoperative fluoroscopy (A–D) of the right femur after fixation of pathologic fracture with cephalomedullary device.
Fig. 4.
Histology of biopsy from femoral lesion obtained at time of reduction and fixation of femur. (A) Infarcted tumor (left) with adjacent marked acute inflammation (right) (H&E stain; original magnification ×200). (B) Foci of viable metastatic follicular thyroid carcinoma. Note the uniform tumor cells with dark nuclei and eosinophilic cytoplasm arranged in nests and small follicles (H&E stain; original magnification ×400).
Radiation oncology was consulted to provide post-operative radiation therapy and medical oncology was consulted for consideration of postoperative chemotherapy. She was mobilized with physical therapy, and was able to walk with the aid of a walker at the time of discharge.
Discussion
In this case report, we illustrate numerous factors associated with a telemedicine visit that resulted in the delayed diagnosis of a skeletal metastasis. This case highlights many of the pitfalls possible with orthopedic surgeons' use of this type of encounter.
One obvious drawback to using telemedicine visits is the limitation placed in conducting a physical examination. Telephonic-only visits are the most limited. These types of visits can detect certain components of the examination (e.g. affect) in the patient's verbal communication. In some unusual circumstances, the physician may be able to evaluate audible findings (e.g. tendon crepitus).
Physical examinations through the video component of eVisits are also limited, albeit less so than with telephonic encounters. eVisits with orthopedic encounters can certainly provide greater information but still prevent adequate examination of tissue character, temperature, sensory function, motor strength, differentiation of pain intensity and certain types of coordination.
With both isolated telephonic encounters and eVisits, there is a very limited ability to obtain synchronous supplemental imaging. For these visits, patients ideally obtain imaging just before the visit itself (e.g. one or a few days before) to allow accurate radiographic diagnosis. When patients are seen in-person in the orthopedic clinic, they are easily sent back to radiology for repeat imaging for those studies that were inadequate or for supplementary studies to show expanded fields of view or non-standard views. In most cases, this option is not available for telephonic or eVisits. Some locales have services that provide mobile imaging at the home of the patient [[3], [4], [5]]. Where available, these services can help improve the quality of the care. However, the imaging equipment such companies are able to bring to the patient's home is limited; specialized studies are not able to be performed. This limits the improvement in diagnostic capabilities.
All patients are not able to use eVisit technology. While smart phones are extremely common, the expertise to conduct a eVisit is not universal. We have found that many geriatric patients have difficulty with eVisit technology. In our case, had an eVisit been possible, it may have tipped-off the treating surgeon to the true nature of the problem. In the hospital, when describing her “knee pain,” she grabbed her thigh. This observation during an eVisit may have led to further questioning or radiographs.
While we have in-person or virtual interpreter services for all in-person patient visits, during the pandemic this has not been possible. This deficit is related to the quick adoption of the eVisit technology as well as the lack of a formal “check-in” where the need for interpreter services is typically ascertained. Although this patient's family spoke fluent English and Spanish, it is likely that communication issues stemming from the lack of professional interpreter services contributed to the delay in diagnosis.
A different outcome would not have been assured if an in-person visit had been conducted. However, the surgeon who conducted the VV is fellowship trained in arthroplasty and musculoskeletal oncology, with over 30 years of experience in practice. We believe it unlikely that this diagnosis would have been initially missed if the clinic encounter had been conducted in-person with a dedicated professional interpreter.
Many practices are embracing both virtual visits and telemedicine to continue to treat patients with musculoskeletal problems while maintaining social distancing during the COVID-19 pandemic. It is important to note the limitations of the technology and take steps to mitigate these problems.
Contributor Information
Eric M. Bluman, Email: ebluman@bwh.harvard.edu.
Matthew S. Fury, Email: MFURY@mgh.harvard.edu.
John E. Ready, Email: jready@bwh.harvard.edu.
Jason L. Hornick, Email: jhornick@bwh.harvard.edu.
Michael J. Weaver, Email: MJWEAVER@PARTNERS.ORG.
References
- 1.AAFP Blog A virtual visit algorithm: how to differentiate and code telehealth visits, e-visits, and virtual check-ins. https://www.aafp.org/journals/fpm/blogs/inpractice/entry/telehealth_algorithm.html
- 2.Mehrotra A., Paone S., Martich G.D., Albert S.M., Shevchik G.J. Characteristics of patients who seek care via eVisits instead of office visits. Telemed J e-Health. 2013;19(7):515–519. doi: 10.1089/tmj.2012.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ricauda N.A., Tibaldi V., Bertone P. The RAD-HOME Project: a pilot study of home delivery of radiology services. Arch. Intern. Med. 2011;171(18):1678–1680. doi: 10.1001/archinternmed.2011.336. [DOI] [PubMed] [Google Scholar]
- 4.Gaitan D. Reuters; Portable X-ray services becoming more common. https://www.reuters.com/article/us-portable-xrays/portable-x-ray-services-becoming-more-common-idUSKBN0KW1ZN20150123
- 5.AARP Amy Goyer Vlog; Mobile X ray services. https://www.youtube.com/watch?v=3ge8llElOgk