Abstract
Immediate after the official declaration of COVID-19 in Bangladesh on 8 March 2020, it has created public panic which results in price plummeting of the capital market and price hike of many essential commodities. Worldwide, the outbreak of COVID-19 has declared a pandemic. In response, the Government of Bangladesh has initiated some strict measures such as stopping the entry of passengers from Europe, stopping on-arrival visas and self-quarantine for 2 weeks for all passengers return from abroad. Still, many loopholes exist at the entry points of Bangladesh. Most of the people of Bangladesh are yet to aware of the consequences of COVID-19. In this backdrop, this article has attempted to create public awareness about COVID-19, providing some guidelines to restrict this deadly disease, enlisting current challenges of this disease in Bangladesh. This review would be helpful to undertake future management practices against the fearsome COVID-19 in Bangladesh.
Keywords: Coronavirus, outbreak, fatality, pneumonia, Bangladesh
Introduction
The coronavirus was first isolated in 1937, which caused bronchitis in birds [1,2]. However, human coronaviruses (HCoV-229E and HCoV-OC43) were first characterized in the 1960s [3], which were associated with diseases in respiratory tracts such as bronchitis and pneumonia and illnesses in the enteric and central nervous system [3,4]. The virus is named as coronavirus for the crown-like spikes on their surface [5]. According to the Centers for Disease Control and Prevention, Atlanta, USA, the syndrome of coronavirus is called severe acute respiratory syndrome (SARS). The virus SARS-associated coronavirus (SARS-CoV) has received worldwide attention due to its epidemic appearance in 2003. Since then, a total of 8,098 people became sick, which claimed 774 lives across the globe [6]. However, there were no known cases of SARS reported anywhere in the world after 2004 [7]. Recently, a novel coronavirus named SARS-CoV-2 has spread worldwide [8], including Bangladesh, which is one of the most densely populated countries (160 million) in the world [9]. Although overpopulated, the economy of Bangladesh is booming in recent times [8]. Since its independence in 1971, the annual gross domestic product in Bangladesh was 8.75 billion, which is expected to reach 315.00 billion USD by the end of 2020 [8]. In this situation, the emergence of novel coronavirus (COVID-19) in Bangladesh could be a threat to the boosting economy.
Taxonomy, types, origin and evolution of human coronaviruses
Coronaviruses (CoVs) belong to the family Coronaviridae under order Nidovirales. The family Coronoviridae has two subfamilies, such as Orthocoronaviridae and Torovirinae. The subfamily Orthocoronaviridae has four genera, such as alphacoronavirus, betacoronavirus, gammacoronavirus and deltacoronavirus [10]. Until now, seven types of coronaviruses have the ability to infect human. The human coronaviruses are 229E, NL63, OC43 and HKU1, and the rarer strains are SARS-CoV [11] and Middle Eastern respiratory syndrome coronavirus (MERS-CoV) which was first appeared in 2012 in Saudi Arabia [12] and recent SARS-CoV-2 [13]. The virus SARS-CoV-2 has a single-stranded RNA genome ranged from 26 to 32 kilobases (kb) in length, which is one of the largest genomes among RNA viruses [14]. Ten genome sequences of SARS-Cov-2 exhibited 88% identity with two bat-derived SARS-like coronaviruses, bat-SL-CoVZC45 and bat-SL-CoVZXC21; however, they were more distant from SARS-CoV (about 79%) and MERS-CoV about 50% [15]. Usually, the CoVs are commonly harbored in mammals and birds as well as in camels, cattle, cats, bats, and other animals [10]. Genomic characterization of SARS-CoV, MERS-CoV, and SARS-CoV-2 reported that the origination of these viruses was bats. The intermediate hosts of SARS-CoV and MERS-CoV were masked palm civets and dromedary camels, respectively, with human as terminal hosts [16]. However, the intermediate hosts of SARS-CoV-2 are predicted to be the unknown wild animals sold at the seafood market [16,17].
Worldwide severity and outbreak of novel human coronavirus (COVID-19)
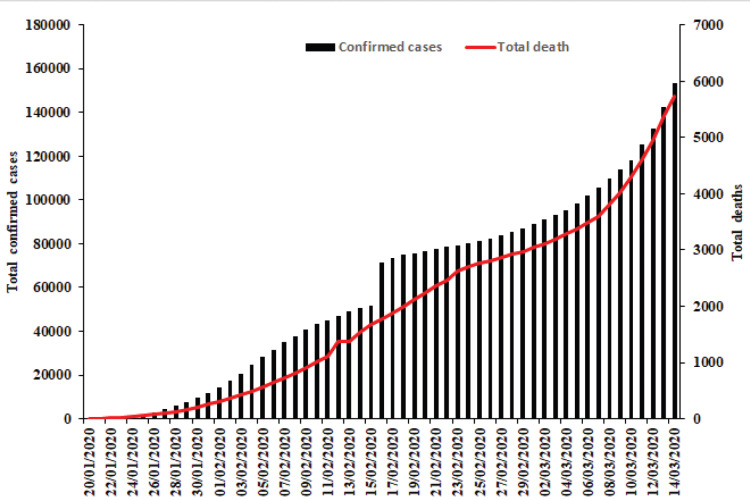
A new type of pneumonia was detected in Wuhan city, Hubei Province of China, on 31 December 2019. Since then, a total of 44 cases with an unknown type of pneumonia were detected until 3 January 2020 [18,19]. The outbreak of this pneumonia was associated with exposures in one seafood market. The unknown case was confirmed as a new type of coronavirus on 7 January 2020. Outside of China, the same kind of novel coronavirus was identified on 13, 15, and 20 January 2020 in Thailand, Japan, and the Republic of Korea, respectively. According to the World Health Organization [20], the cases in Thailand, Japan, and the Republic of Korea were originated from Wuhan City, China. Officially, the WHO has named the novel coronavirus as SARS-CoV-2 causing coronavirus disease-2019 (COVID-19) on 11 February 2020 [10]. Since the first situation report of the WHO published on 21 January 2020, the confirmed case (a person with laboratory confirmation) of COVID-19 was 282 (claimed six lives), which had skyrocketed to 153,517 (claimed 5735 lives) on 15 March 2020 (Fig. 1). Due to the severe outbreak across the globe, the WHO declared the outbreak of COVID-19 is pandemic on 11 March 2020 [8].
Figure 1. Global trend of novel coronavirus (COVID-19) outbreak (situation report 55; data until 16 March 2020 [8]).
According to the current WHO report, the total fatality of COVID-19 is 5,735 with a fatality rate of only 3.73% [8]. However, overall mortality combinedly caused by SARS-CoV and MERS-CoV was 1632 [21,22], with the rate of occurrence of 9.6% [23] and 35.2% [2], respectively. When we wrote this article, new confirmed cases and deaths are recorded every day; therefore, the mortality rate of COVID-19 might be changing, which could not be calculated accurately until the end of this outbreak.
The outbreak of COVID-19 and its consequence in Bangladesh
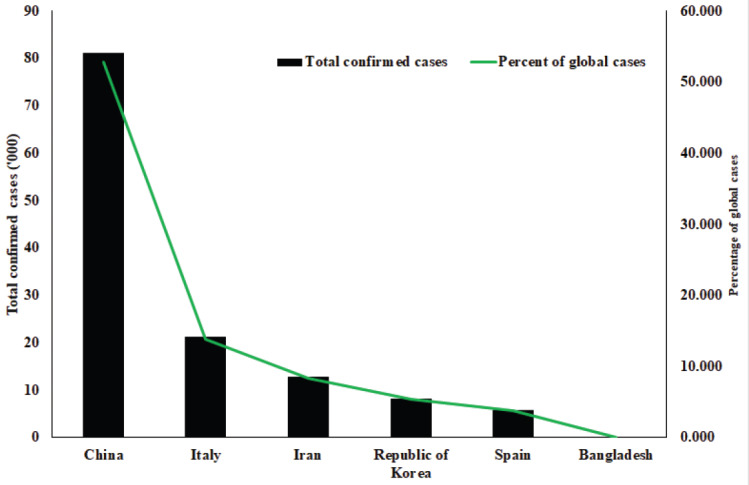
Three confirmed cases of COVID-19 announced for the first time in Bangladesh on 8 March 2020 by the institute of epidemiology, disease control, and research (IEDCR). Subsequently, there were no confirmed cases found on 13 March 2020. However, on 14 March 2020, two more confirmed cases newly detected in Bangladesh. Until now, COVID-19 caused no fatality in Bangladesh. Among the global confirmed cases, Italy, Iran, the Republic of Korea, and Spain ranked 2nd, 3rd, 4th, and 5th, respectively, after China [8] (Fig. 2). In comparison to the global perspective, although the occurrence of COVID-19 is very low (only 0.003%) in Bangladesh, the panic which spreads among the most densely populated country (160 million people) in the world is immense. The first blow of this panic hits into the Bangladesh stock market; due to the fear selling, the general index of the DSE plunged 279.32 points (6.51%) to close the day at 4,008.05 [24]. The panic also affected foreign trade. Qatar temporarily barred travelers from Bangladesh. The Prime Minister of India, Narendra Modi, has canceled his trip to Bangladesh on the occasion of grand inaugural ceremony of Mujib Year [25], and there is excessive price gouging of some essentials such as surgical and face masks, sanitizers, electronics and electrical materials, and so on. [26]. The Government on 14 March 2020 declared that no inbound passengers from European countries except the UK would be allowed in Bangladesh until 31 March 2020. All kinds of on-arrival visas have been suspended for new 2 weeks. Besides, passengers return from any country would be self-quarantined for 14 days [27]. Still, any relaxation on monitoring this disease would be very costly. All kinds of educational institutions would remain close until 31 March 2020 [27]. Moreover, all sports activities to be postponed until 31 March 2020 [27]. Unlike the USA, Spain, Serbia, France, and Lebanon, Bangladesh has yet to declare a state of emergency. The country is now in a state of uncertainty, just watching the global initiatives.
Figure 2. Comparative occurrence of COVID-19 in the top five infected countries and Bangladesh with a percentage share of global cases as of 16 March 2020. (Source: WHO; situation report 55 [8].
The Prime Minister (PM) of Bangladesh has promptly accepted the presence and reality of COVID-19 in Bangladesh. The PM directed all the authorities concerned to closely monitor the situation at all the entry points of Bangladesh and to improve the facilities of all the public hospitals by ensuring enough quarantine facilities. The PM also canceled all the prescheduled meetings, processions, public gatherings, and foreign trips.
Epidemiology of COVID-19
Environmental factors such as temperature, humidity, and wind speed have a significant effect on the survival and transmission of human coronaviruses such as SARS-CoV and MERS-CoV [28]. In general, the survival of viral particles is inversely proportional to air temperature [29]. SARS-CoV could survive for 5 days on a smooth surface at 22°C–25°C and relative humidity 40%–50% [28]. However, it is lost its activity with the increase of temperature and relative humidity at 38°C and 95%, respectively. The possible transmission of SARS-CoV has occurred through airborne droplets. Furthermore, this virus could survive in human feces [30]. Another human coronavirus MERS-CoV could remain active for an extended period as droplets on the solid surface at high temperature (15°C–35°C) and low humidity (<20%). However, with the increase of relative humidity (>35%) and temperatures (5°C–15°C), the survivability and spread of MERS-CoV would be reduced [31]. Although newly emerged novel SARS-CoV-2 virus has similar origin with SARS-CoV and MERS-CoV, the role of temperature and absolute humidity in the transmission is yet to be clearly understood. The contradictory reports have been published in this regard because recently, a group of scientists in China [32] reported that the increased temperature and humidity did not reduce the incidence of COVID-19 [32]. However, according to Wang et al. [29], the increased temperate and relative humidity significantly reduced the transmission of COVID-19 in 100 cities of China. Similarly, another group reported that the COVID-19 virus is sensitive to high temperatures (>30°C) [33]. Using the current statistics available in situation report 55 at the WHO website [8], the cumulative rate of confirmed cases and deaths of COVID-19 is 1.4% and 0.52%, respectively, in tropical or subtropical countries or regions, but it is 98.59% and 99.47%, respectively, in temperate countries or regions (Table 1). Further studies need to be undertaken to confirm whether the variability of incidence and transmission of COVID-19 and deaths in different climatic regions are caused by the variation of temperature and relative humidity in these countries or regions.
Table 1. Comparative analysis of worldwide confirmed COVID-19 cases and deaths between tropical or subtropical and temperate regions/countries.
| Tropical/subtropical countries or regions | Temperate countries or regions | |||||
|---|---|---|---|---|---|---|
| Countries | Confirmed cases | Deaths | Countries | Confirmed cases | Deaths | |
| Afghanistan | 10 | 0 | Australia | 249 | 3 | |
| Bahrain | 211 | 0 | Austria | 800 | 1 | |
| Bangladesh | 3 | 0 | Belgium | 689 | 0 | |
| Bhutan | 1 | 0 | Brazil | 121 | 0 | |
| Cambodia | 7 | 0 | Canada | 244 | 1 | |
| Egypt | 93 | 2 | China | 81048 | 3204 | |
| India | 107 | 2 | Czech | 214 | 0 | |
| Indonesia | 117 | 4 | Finland | 210 | 0 | |
| Iraq | 93 | 9 | France | 4469 | 91 | |
| Jordan | 1 | 0 | Germany | 3795 | 8 | |
| Kuwait | 112 | 0 | Greece | 228 | 2 | |
| Lebanon | 93 | 3 | Ireland | 129 | 2 | |
| Malaysia | 238 | 0 | Italy | 21157 | 1441 | |
| Maldives | 10 | 0 | Japan | 780 | 22 | |
| Nepal | 1 | 0 | Mexico | 41 | 0 | |
| Oman | 20 | 0 | Netherland | 959 | 12 | |
| Pakistan | 28 | 0 | Norway | 907 | 1 | |
| Philippines | 111 | 6 | Poland | 111 | 3 | |
| Qatar | 337 | 0 | Portugal | 112 | 0 | |
| Saudi Arabia | 103 | 0 | Republic of Korea | 8162 | 75 | |
| Sri Lanka | 11 | 0 | Romania | 123 | 0 | |
| Thailand | 75 | 1 | Russia | 34 | 0 | |
| Tunisia | 16 | 0 | Singapore | 212 | 0 | |
| UAE | 85 | 0 | Spain | 5753 | 136 | |
| Vietnam | 53 | 0 | Sweden | 924 | 0 | |
| Subtotal | 1936 | 27 | Switzerland | 1359 | 11 | |
| United Kingdom | 1144 | 21 | ||||
| United States of America | 1678 | 41 | ||||
| Subtotal | 135652 | 5075 | ||||
| Total Confirmed cases | 137,588 | |||||
| Total deaths | 5,102 | |||||
| Percent of confirmed cases in tropical/ subtropical countries/regions | 1.407099456 | |||||
| Percent of confirmed cases in temperate countries/ regions | 98.59290054 | |||||
| Percent of death in tropical/ subtropical countries/regions | 0.529204234 | |||||
| Percent of death in temperate countries/regions | 99.47079577 | |||||
Up to 16 March 2020 [8].
Although the mechanism of transmission of COVID-19 is not fully understood, the recent studies of Huang et al. [34] and Chan et al. [35] have reported human-to-human transmission through the respiratory droplets and surface contact. The droplets are generated from the infected person through his coughs or sneezes, which could potentially infect others remaining in close contact [36]. The virus within the droplets could remain viable on the surface of an object for a few days; thus, the nearby surroundings of an infected person are potential sources of contamination. The symptomatic (sickest) persons are thought to be most contagious. Moreover, recent evidence suggests that a person without symptoms (asymptomatic) could potentially spread the pathogen during the incubation period [37]. Unlike SARS virus, the risk of contamination by COVID-19 virus through feces of an infected person is low [34]. Besides, there is no evidence of airborne dissemination of SARS-CoV-2.
The subtropical monsoon climate in Bangladesh is characterized by heavy summer rainfall and high summer temperature with often excessive humidity. The range of ambient temperature in the summer is 36°C–40°C, and winter temperature is 8°C–15°C [38]. If the studies of Wang et al. [29,33] are true and if the trend of disease occurrence and fatality of Table 1 is sustained, then the cases and fatality of COVID-19 are expected to be very low in Bangladesh particularly in the summer season. Although the mechanism of high temperature and high humidity reduces the transmission of COVID-19 is not known yet, in the case of the influenza virus, two possible reasons have been identified (29). First, the influenza virus is more stable in cold temperatures, and respiratory droplets remain airborne longer in dry air [39,40]. Second, cold and dry weather impairs mucociliary clearance, innate antiviral immunity, and tissue repair and makes them more susceptible to the virus [41,42]. These mechanisms are also likely to applicable for the COVID-19 transmission.
Pathogenesis of COVID-19
The clinical signs and symptoms are almost similar to that of SARS and MERS infections [43]. Hence, although the pathogenesis of COVID-19 is poorly understood, the similar mechanisms of SARS and MERS still can give us a lot of information on the pathogenesis of COVID-19.
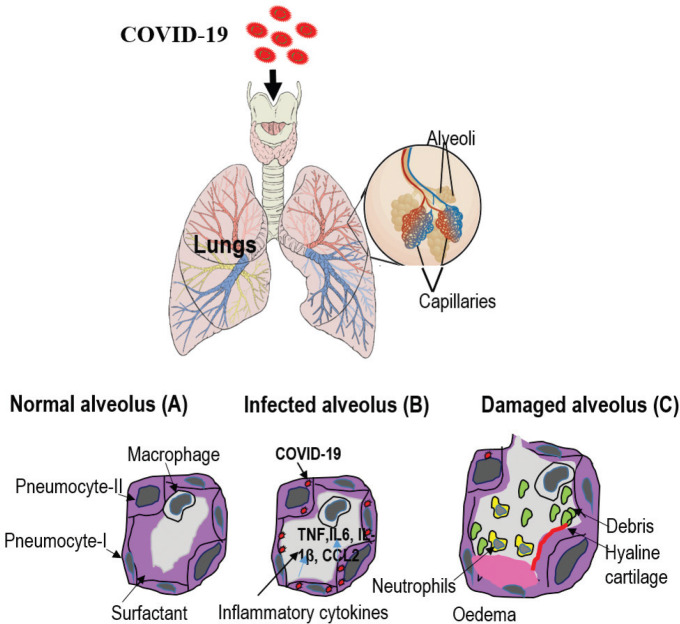
The lungs are made up of a mass of alveoli. The alveoli are responsible for gaseous exchange, providing oxygen to blood flowing through capillaries in the alveolar membrane. The alveolar walls are composed of type I and type II pneumocytes, along with alveolar macrophages (Fig. 3) [44]. Type I pneumocytes are responsible for gaseous exchange with blood in the capillaries of the lungs. Type II pneumocytes are the progenitors of type I pneumocytes and are also responsible for producing surfactant [45]. SARS-CoV infection causes desquamation of pneumocytes by releasing inflammatory cytokine in humans and rats and alveolar swelling, edema, and hemorrhage in the lungs (Fig. 3) [46]. The virus also destroys alveolar macrophages that play an essential role in local immune response [47]. In critical illness, uncontrolled inflammation, fluid accumulation, and developing fibrosis severely compromise gas exchange and lead to respiratory failure [42].
Figure 3. An overview of the pathogenesis of the viral infection in the lungs. Type I and type II pneumocytes make up the alveolar walls, and resident alveolar macrophages and pulmonary surfactant exist in the airspace (A). In the acute phase of SARS-CoV infection (B), type I and type II pneumocytes are infected and secrete inflammatory cytokines, whereas surfactant levels decrease. In severe illness, inflammation, fluid accumulation, and developing fibrosis severely damage alveoli and lead to respiratory failure (C).
Symptoms of COVID-19
The symptoms of COVID-19 are either asymptomatic (no signs) or symptomatic (non-, mild-, or severe pneumonia) [48]. The range of mild disease (i.e., nonpneumonia or mild pneumonia) is about 80% of cases (mostly curable), mild-to-severe pneumonia is about 14%, and critical illness is about 6% of cases [22]. The critical illnesses lead to severe consequences such as a death in the case of the elderly or other people who have severe chronic medical conditions such as heart disease, diabetes, and lung diseases [15]. Other common signs of COVID-19 infection are respiratory symptoms, fever, coughing, sneezing, shortness of breath, and breathing difficulties (Table 2) [14].
Table 2. Similarities and differences among the three coronaviruses transmission, clinical signs, and diagnosis.
| Virus | Zoonotic transmission | Incubation period | Clinical signs and symptoms | Diagnosis | Treatment | Fatality |
|---|---|---|---|---|---|---|
| COVID-19 | Bats harbor the three coronaviruses as a reservoir host. It is still unclear whether the COVID-19 transmitted from bats to humans [10]. Then, human-to-human transmission through droplets, personal (handshaking), and contaminated surface contact [34,35]. It seems to be more transmissible than SARS and MERS. | 2–14 days [10,55] | Mostly respiratory symptoms, such as fever, dry cough, shortness of breath, and in the most severe cases, have pneumonia [10] | Clinical diagnosis based on symptoms, epidemiological history and chest imaging, and confirmation diagnosis by nucleic acid test, such as RT-qPCR, deep sequencing, and ELISA [34,56]. | No antiviral drug yet [57,58]. Oxygen and fluid therapy and antibiotics with oseltamivir [34,57,58]. In severe illness, corticosteroids are used to reduce lung inflammation [59]. | 3.73% [8] |
| SARS | Primarily transmitted from bats to snakes, civet cats, and finally to human [10]. Then, similar transmission to COVID-19, including fecal [34,60]. | 2–10 days, up to 14 days [10] | Besides respiratory symptoms [10], the virus is known to cause enteric symptom, such as diarrhea and abdominal pain, and finally focal necrosis and nephritis in the kidney [60]. | Similar to COVID-19 | Similar to COVID-19 | 9.6% [23] |
| MERS | Primarily transmitted from bats to camels and finally to human [10] and then human to human transmission via direct respiratory secretion contact [34] and also fecal-oral transmission [60]. | Typically, 2–14 days [10] | Severe acute respiratory distress, severe pneumonia, enteric symptoms, and kidney failure [60,61]. | Similar to COVID-19 | Similar to COVID-19 | 35.2% [2] |
Diagnosis of COVID-19 infection
As there are no specific therapeutic drugs or vaccines available for novel COVID-19; therefore, it is essential to detect the disease at an early stage so that immediate isolation of the patient could be undertaken. Thus, the radiological examination is used for the early detection of COVID-19 [49]. Thin-slice chest CT functions are more effectively detecting pneumonia caused by COVID-19 at a very early stage [50]. The sensitivity of CT for COVID-19 infection was 98%, but it was much higher than the sensitivity (71%; p < 0.001) of RT-PCR [49,51]. Although nucleic acid-based detection (real time-qPCR) is used as the standard of reference (Table 2), recently, Xie et al. [52] reported that 5/167 (3%) patients, who had negative RT-qPCR for COVID-19 at the initial stage of COVID-19 but conduction of chest CT, confirmed viral pneumonia at the early stage.
The collection of samples for the detection of the virus is a big challenge for the health workers. The recommended specimens for COVID-19 diagnosis are nasopharyngeal and oropharyngeal swabs; however, the collection of these samples requires close contact with the patients, which poses a risk of transmission of the viruses to the healthcare personnel. Therefore, saliva specimens are suggested because patients could easily spit their saliva into a sterile bottle in a noninvasive way [53]. Meanwhile, real-time RT-PCR using blood samples gave a very low percentage (1%) of the positive results, and urine samples did not give positive results [54].
In Bangladesh, IEDCR is the only approved institute which provides the diagnostic facilities of COVID-19. The detection of COVID-19 is a real-time RT-PCR-based assay that requires skilled human resources and sophisticated laboratory facilities. To avoid false results and risks of biological hazards, the Government is not allowing any other private organizations except IEDCR to perform this [27]. The rapid test kits are although available in Bangladesh, but the WHO does not approve these kits.
Prevention and control of COVID-19
It is popularly said that “prevention is better than cure.” Prevention of COVID-19 should be the prime strategy to restrict this deadly disease from a further outbreak in Bangladesh. The WHO suggested that the transmission of COVID-19 should be prevented by reducing the secondary infections among close contact with persons who suffer from acute respiratory infections. Besides, the hands should be frequently washed after direct contact with a sick person; furthermore, the unprotected contact with wild animals should be avoided. Moreover, the COVID-19-infected person should maintain a good practice of cough etiquettes such as by covering coughs and sneezes with disposable tissues or clean clothes, by washing hands, and by maintaining distance with noninfected persons [15]. In addition to these preventive measures, the Government of Bangladesh should be undertaken stern actions against the passengers, such as strictly measuring their body temperature or keep them in an isolation condition for 14 days at the land, sea, and airports after arrival from COVID-19-infected countries.
Effective vaccines are essential to control the coronavirus outbreaks. There are several vaccination strategies used against SARS-CoV, and MERS-CoV tested in animals, including a live-attenuated virus, inactivated virus, subunit vaccines, recombinant DNA, and protein vaccines [62]. These studies are still underway to develop vaccines for humans.
Unlike SARS-CoV and MERS-CoV, no proven vaccines so far discovered against COVID-19. However, the first trial of evaluating a vaccine against COVID-19 has begun on 15 March 2020 at kaiser permanente washington health research institute in Seattle funded by the national institute of allergy and infectious diseases [63]. There are many promising targets for COVID-19, but more clinical trials still should be needed.
Management of COVID-19 contamination
Evidence suggests that the virus is contaminated from human to human very rapidly [35,64]. Although complete elimination of COVID-19 outbreak seems impossible, several key measures could reduce the possible transmission of SARS-CoV-2 by avoiding the contact opportunities [65], such as avoiding social mass people gathering, transient closure of school and day care for the peak period of outbreak, traveling and trade restrictions, entry screening of the travelers during outbreak period, isolation of infected cases, and maintaining the physical distance within the workspace. In this backdrop, flexible working schedules/shifts for employees, the opportunity of distance working/teleworking, increased use of email and teleconferences to reduce close contacts, reduced contact between employees and customers, reduced contact between employees, promoting the use of other personal protective countermeasures, and avoiding mass gathering, such as sport events, concerts, religious events, conferences, and so on are advised.
According to the WHO, the practice of good personal hygiene is essential [8,66]. Regularly washing hands with soaps and water and avoid touching the face with the hands are some ways to ensure personal hygiene. Wearing a mask is not essential until a person is detected with SARS-CoV-2 to protect spreading the virus to the public [67]. The infected person should take rest at home or admit to the hospital for complete isolation for 14 days. In case of emergency, the infected person should wear a surgical mask to protect others.
Potential treatments against COVID-19
As we know, no effective treatments are available for viral diseases [57,58]. The supportive treatments such as oxygen therapy, conservation fluid management, and the use of broad-spectrum antibiotics to treat secondary bacterial infection are still practiced as important management strategies (Table 2) [34]. In severe illness, corticosteroids are used to reduce lung inflammation [59]. Some of the drugs such as oseltamivir, lopinavir/ritonavir, nucleoside analogs, neuraminidase inhibitors, remdesivir, umifenovir, tenofovir disoproxil and lamivudine (inhibitors), chloroquine, and Shufeng Jiedu or Lianhua Qingwen capsules (traditional medicines of China) are advised to treat COVID-19 [59,68–70]. Moreover, some inhibitors such as 3CLpro (3CLpro-1) and a novel vinyl sulfone protease and angiotensin-converting enzyme 2 (ACE2)-based peptide showed their potentiality against SARS-CoV-2 [71]. Usually, drugs are not effective against viral diseases. Recently, an antiviral drug Favilavir has approved by China’s National Medical Products Administration on 16 February 2020 to treat COVID-19 [72]. This drug has produced by Zhejiang Hisun Pharmaceutical and marketed as brand name Avigan [73].
Current challenges of COVID-19 in Bangladesh
News such as “Coronavirus Outbreak: Screening still lax at Dhaka airport” in the Daily Star on 10 March 2020 [74] has frustrated the government’s efforts to combat the deadly COVID-19 in Bangladesh. Few initiatives have been observed at the Shah Jalal International Airport, such as the setting of some thermal scanners to check the real-time body temperature of the passengers and filling up a health declaration form. However, no disinfection activities and none of the confirmation tests by taking samples from the passenger’s body have performed. According to the WHO, the disease could remain asymptomatic for up to 14 days. Therefore, thermal scanner and travel history are not enough measures to detect COVID-19 among the passengers. Apart from passengers scanning, no initiatives have taken to disinfect the planes and luggage of the passengers.
There is a misconception among the people of Bangladesh that the disease would not sustain in the country due to the onset of summer when the temperature would remain above 30°C. However, the recent study reported that temperature does not change the transmission of COVID-19 [46]; unlike the SARS virus, there is no evidence that the outbreak of COVID-19 would be reduced at higher temperature [75].
Other challenges are (i) lack of laboratory facilities for the early detection of the disease, (ii) scarcity of medical supplies, such as surgical masks and goggles, (iv) lack of personal protective equipment (PPE) for healthcare personnel, (iv) asymptomatic transmission of COVID-19 which could challenge the management strategies at risk [41], (v) lack of quarantine facilities at the hospitals, (v) it is very unfortunate that a good number of people of Bangladesh are not maintaining good hygiene and sanitation practices, and (vi) until now, no specific drugs or vaccines have been proven effective against COVID-19.
Recommendations
Globally, as there are no vaccines discovered against novel coronavirus disease COVID-19; therefore, prevention and management are the best ways to tackle this deadly disease. By comparing the global outbreak, confirmed cases are only 0.003% in Bangladesh [8]. However, stern actions should be taken immediately so that further penetration of any case is not possible through the land-, sea-, and air-ports. Nationally, public awareness is the crucial factor in protecting this disease. The health officials, doctors, and scientists of IEDCR should be worked together with educational institutes, local leaders, and all other professionals to educate them about the protection and safety measures against COVID-19.
Early and quick detection are essential measures to stop the transmission of COVID-19. The diagnostic facilities of Bangladesh should be improved by providing the detection facilities at all the divisional, district, and upazilla hospitals. Once a new case is detected, he should be isolated immediately.
Some general recommendations are suggested as follows:
(i) as per the WHO’s guidelines [23], hand hygiene must be maintained by cleaning hands with soap and water for at least 20 seconds or using alcohol-based hand sanitizer, (ii) avoid contact hands with eyes, nose, and mouth, (iii) the use of disposable tissues or clothing when coughs and sneezes, (iv) health personnel must ensure PPE while working, (v) avoid interpersonal contact such as kissing, handshaking, and so on, (vi) avoid mass gathering and public meetings, (vii) be aware of the latest news circulate by local and international health authorities, (viii) seek medical care when anyone feels fever, cough, and difficulty breathing, (ix) once a person is detected positive with COVID-19, he must be isolated for at least 14 days, (x) operation of public transportations such as local buses, launches, and trains should be limited for 2–3 weeks, and (xi) passengers return from abroad should be self-quarantined for 2 weeks.
Specific recommendations to the government are as follows:
Apart from European flights, passengers from other infected countries such as China, the Republic of Korea, Iran, and the Middle East should undergo extensive screening and, if possible, should be kept in force isolation for 2 weeks. Besides, the planes and luggage arriving from these countries should be disinfected. Compulsory screening of passengers must be maintained at all the entry points of Bangladesh.
Collaborative research between the WHO and government or nongovernment organizations should be carried out immediately to develop a vaccine for SARS-CoV-2.
Providing sufficient funds to conduct research on epidemiology, surveillance, and management of COVID-19 in Bangladesh.
Frequently circulate the news of public awareness and precautions about COVID-19 in mass media.
Acknowledgment
Nothing to disclose.
Conflict of interests
The authors declare that they have no conflict of interests.
Authors’ contribution
Mohammad Shah Alam was involved in the planning and intellectual drafting of the article. Mohammad Zahangeer Alam helped in the drafting of the article, and K. H. M. Nazmul Hussain Nazir and Md. Abdullahil Baki Bhuiyan contributed to revisit the article with potential intellectual content.
References
- [1].Beaudette FR, Hudson CB. Cultivation of the virus of infectious bronchitis. J Am Vet Med Assoc. 1937;90:51–60. [Google Scholar]
- [2].Wang W, Lin XD, Guo WP, Zhou RH, Wang MR, Wang CQ, et al. Discovery, diversity and evolution of novel coronaviruses sampled from rodents in China. Virology. 2015;474:19–27. doi: 10.1016/j.virol.2014.10.017. https://doi.org/10.1016/j.virol.2014.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Gaunt ER, Hardie A, Claas EC, Simmonds P, Templeton KE. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48(8):2940–7. doi: 10.1128/JCM.00636-10. https://doi.org/10.1128/JCM.00636-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kahn JS, McIntosh K. History and recent advances in coronavirus discovery. Pediatr Infect Dis J. 2005;24(11):S223–7. doi: 10.1097/01.inf.0000188166.17324.60. https://doi.org/10.1097/01.inf.0000188166.17324.60. [DOI] [PubMed] [Google Scholar]
- [5].Lin S, Lee CK, Lee SY, Kao CL, Lin CW, Wang AB, et al. Surface ultrastructure of SARS coronavirus revealed by atomic force microscopy. Cell Microbiol. 2005;7(12):1763–70. doi: 10.1111/j.1462-5822.2005.00593.x. https://doi.org/10.1111/j.1462-5822.2005.00593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Peiris JS, Yuen KY, Osterhaus AD, Stöhr K. The severe acute respiratory syndrome. New Engl J Med. 2003;349(25):2431–41. doi: 10.1056/NEJMra032498. https://doi.org/10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention CDC. Outbreak of severe acute respiratory syndrome--worldwide. MMWR-Morbid Mortal W. 2003;52(11):226. [PubMed] [Google Scholar]
- [8].World Health Organization (WHO) [Mar 16;2020 ];Novel coronavirus (2019-nCoV). Situation report-55. Available via https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200315-sitrep-55-covid-19.pdf?sfvrsn=33daa5cb_6 .
- [9].Islam S, Khan MZR. A review of energy sector of Bangladesh. Enrgy Proced. 2017;110:611–8. https://doi.org/10.1016/j.egypro.2017.03.193. [Google Scholar]
- [10].Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA. Insights into the Recent 2019 Novel Coronavirus (SARS-CoV-2) in Light of Past Human Coronavirus Outbreaks. Pathogens. 2020;9(3):pii. doi: 10.3390/pathogens9030186. E186; https://doi.org/10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Matoba Y, Aoki Y, Tanaka S, Yahagi K, Shimotai Y, Matsuzaki Y, et al. An outbreak of human coronavirus OC43 during the 2014–2015 influenza season in Yamagata, Japan. Jpn J Infect Dis. 2015;68(5):442–5. doi: 10.7883/yoken.JJID.2015.292. https://doi.org/10.7883/yoken.JJID.2015.292. [DOI] [PubMed] [Google Scholar]
- [12].Chen X, Chughtai AA, Dyda A, MacIntyre CR. Comparative epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia and South Korea. Emerg Microbes Infec. 2017;6(1):1–6. doi: 10.1038/emi.2017.40. https://doi.org/10.1038/emi.2017.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].World Health Organization (WHO) Novel Coronavirus (2019-nCoV) [Feb 11;2020 ];Situation report-22. Available via https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2 .
- [14].Ahmad T, Rodriguez-Morales AJ. Emergence of COVID-19 (formerly 2019-novel Coronavirus): a new threat from China. Rev Panam Enf Inf. 2020;2(2):37–8. [Google Scholar]
- [15].Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Ag. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. https://doi.org/10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–74. doi: 10.1016/S0140-6736(20)30251-8. https://doi.org/10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Jiang S, Du L, Shi Z. 2020. An emerging coronavirus causing pneumonia outbreak in Wuhan, China: calling for developing therapeutic and prophylactic strategies. Emerg Microbes Infec. 2020;9(1):275–7. doi: 10.1080/22221751.2020.1723441. https://doi.org/10.1080/22221751.2020.1723441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020;35(5):e61. doi: 10.3346/jkms.2020.35.e61. https://doi.org/10.3346/jkms.2020.35.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. New Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. https://doi.org/10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].World Health Organization (WHO) Novel Coronavirus (2019-nCoV) [Jan 21;2020 ];Situation report-1. Available via https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 .
- [21].Chu YK, Ali GD, Jia F, Li Q, Kelvin D, Couch RC, et al. The SARS-CoV ferret model in an infection–challenge study. Virology. 2008;374(1):151–63. doi: 10.1016/j.virol.2007.12.032. https://doi.org/10.1016/j.virol.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Mahase E. Coronavirus: covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. doi: 10.1136/bmj.m641. https://doi.org/10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- [23].World Health Organization. Water, sanitation, hygiene and waste management for COVID-19: technical brief. 03.03/2020 (No. WHO/2019-NcOV/IPC_WASH/2020.1)
- [24].The Prothom alo. DSE, CSE post massive plunge. [Mar 11;2020 ]; Available via https://en.prothomalo.com/business/dse-cse-post-massive-plunge .
- [25].The India Today. PM Modi’s Dhaka trip cancelled after 3 coronavirus cases reported in Bangladesh. [Mar 11;2020 ]; Available via https://www.indiatoday.in/india/story/pm-modi-s-dhaka-trip-cancelled-after-3-coronavirus-cases-reported-in-bangladesh-1653760-2020-03-09 . [Google Scholar]
- [26].The Independent. Panic buying triggers mask, sanitiser crises. [Mar 12;2020 ]; Available via http://www.theindependentbd.com/post/240183 .
- [27].The daily star. [Mar 16;2020 ]; Available via https://www.thedailystar.net/bangladesh-all-educational-institutions-closed-till-march-31-1881541 .
- [28].Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol. 2010;76(9):2712–17. doi: 10.1128/AEM.02291-09. https://doi.org/10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wang J, Tang K, Feng K, Lv W. High temperature and high humidity reduce the transmission of COVID-19. 2020 https://doi.org/10.2139/ssrn.3551767. [Google Scholar]
- [30].Booth TF, Kournikakis B, Bastien N, Ho J, Kobasa D, Stadnyk L, et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis. 2005;191(9):1472–7. doi: 10.1086/429634. https://doi.org/10.1086/429634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Alghamdi IG, Hussain II, Almalki SS, Alghamdi MS, Alghamdi MM, El-Sheemy MA. 2014. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417. doi: 10.2147/IJGM.S67061. https://doi.org/10.2147/IJGM.S67061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Luo W, Majumder MS, Liu D, Poirier C, Mandl KD, Lipsitch M, et al. The role of absolute humidity on transmission rates of the COVID-19 outbreak. medRxiv. 2020 doi: 10.1038/s41598-020-74089-7. https://doi.org/10.1101/2020.02.12.20022467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wang M, Jiang A, Gong L, Luo L, Guo W, Li C, et al. Temperature significant change COVID-19 Transmission in 429 cities. medRxiv. 2020 https://doi.org/10.1101/2020.02.22.20025791. [Google Scholar]
- [34].Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. https://doi.org/10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–23. doi: 10.1016/S0140-6736(20)30154-9. https://doi.org/10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Geneva, Switzerland: World Health Organization; 2020. [Mar 12;2020 ]. Coronavirus disease (COVID-19) advice for the public. Available via https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . [Google Scholar]
- [37].Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019nCoV Infection from an asymptomatic contact in Germany. New Engl J Med. 2020;382(10):970–1. doi: 10.1056/NEJMc2001468. https://doi.org/10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Huda ASN, Mekhilef S, Ahsan A. 2014. Biomass energy in Bangladesh: current status and prospects. Renew Sust Energ Rev. 2014;30:504–17. https://doi.org/10.1016/j.rser.2013.10.028. [Google Scholar]
- [39].Lowen AC, Steel J. Roles of humidity and temperature in shaping influenza seasonality. J Virol. 2010;88:7692–95. doi: 10.1128/JVI.03544-13. https://doi.org/10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface. 2009;6:S783–90. doi: 10.1098/rsif.2009.0302.focus. https://doi.org/10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Eccles R. An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Otolaryngol. 2002;122:183–91. doi: 10.1080/00016480252814207. https://doi.org/10.1080/00016480252814207. [DOI] [PubMed] [Google Scholar]
- [42].Kudo E, Song E, Yockey LJ, Rakib T, Wong PW, Homer RJ, et al. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc Natl Acad Sci USA. 2019;116:10905–10. doi: 10.1073/pnas.1902840116. https://doi.org/10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Peiris JS, Guan Y, Yuen KY. Severe acute respiratory syndrome. Nat Med. 2004;10:S88–97. doi: 10.1038/nm1143. https://doi.org/10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Verma GP. New Delhi, India: New Age International Pvt Ltd Publishers; 2001. Fundamentals of histology. [Google Scholar]
- [45].Fehrenbach H. Alveolar epithelial type II cell: defender of the alveolus revisited. Respir Res. 2001;2:33–46. doi: 10.1186/rr36. https://doi.org/10.1186/rr36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Gralinski LE, Baric RS. Molecular pathology of emerging coronavirus infections. J Pathol. 2015;235:185–95. doi: 10.1002/path.4454. https://doi.org/10.1002/path.4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Zhao J, Zhao J, Van Rooijen N, Perlman S. Evasion by stealth. Inefficient immune activation underlies poor T cell response and severe disease in SARS-CoV infected mice. PloS Pathog. 2009;5:e1000636. doi: 10.1371/journal.ppat.1000636. https://doi.org/10.1371/journal.ppat.1000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. 2020;25(3):278–80. doi: 10.1111/tmi.13383. https://doi.org/10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus Disease 2019 (COVID-19): a perspective from China. Radiology. 2020;200490 doi: 10.1148/radiol.2020200490. https://doi.org/10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;200642 doi: 10.1148/radiol.2020200642. https://doi.org/10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;200432 doi: 10.1148/radiol.2020200432. https://doi.org/10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020;200343 doi: 10.1148/radiol.2020200343. https://doi.org/10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].To KKW, Tsang OTY, Yip CCY, Chan KH, Wu TC, Chan JMC, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;ciaa149 doi: 10.1093/cid/ciaa149. https://doi.org/10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. https://doi.org/10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Guarner J. Three emerging coronaviruses in two decades the story of SARS, MERS, and Now COVID-19. Am J Clin Pathol. 2020;153(4):420–1. doi: 10.1093/ajcp/aqaa029. https://doi.org/10.1093/ajcp/aqaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Xiaowei L, Manman G, Yizhao P, Liesu M, Shemin L. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharmaceut Anal. 2020 doi: 10.1016/j.jpha.2020.03.001. https://doi.org/10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–34. doi: 10.1038/nrmicro.2016.81. https://doi.org/10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY. Coronaviruses - drug discovery and therapeutic options. Nat Rev Drug Discovery. 2016;15:327–47. doi: 10.1038/nrd.2015.37. https://doi.org/10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;pii:dyaa033. doi: 10.1093/ije/dyaa033. https://doi.org/10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5(4):335–7. doi: 10.1016/S2468-1253(20)30048-0. https://doi.org/10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–20. doi: 10.1056/NEJMoa1211721. https://doi.org/10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- [62].Graham RL, Donaldson EF, Baric RS. A decade after SARS: strategies for controlling emerging coronaviruses. Nat Rev Microbiol. 2013;11:836–48. doi: 10.1038/nrmicro3143. https://doi.org/10.1038/nrmicro3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].NIH news. [Mar 16;2020 ]; Available via https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins .
- [64].Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019nCoV), December 2019 to January 2020. Eurosurveillance. 2020;25(4):3. doi: 10.2807/1560-7917.ES.2020.25.4.2000058. https://doi.org/10.2807/1560-7917.ES.2020.25.4.2000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].European Centre for Disease Prevention and Control (ECDC) Technical report. Infection prevention and control for the care of patients with 2019-nCoV in healthcare settings. [Feb 12;2020 ]; Available via https://www.ecdc.europa.eu/sites/default/files/documents/nove-coronavirus-infection-prevention-controlpatients-healthcare-settings.pdf .
- [66].Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. https://doi.org/10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Amodio E, Vitale F, Cimino L, Casuccio A, Tramuto F. Outbreak of Novel Coronavirus (SARS-Cov-2): First evidences from international scientific literature and pending questions. Healthcare. 2020;8(1):51. doi: 10.3390/healthcare8010051. https://doi.org/10.3390/healthcare8010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV) Biosci Trends. 2020;14(1):69–71. doi: 10.5582/bst.2020.01020. https://doi.org/10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- [69].Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–71. doi: 10.1038/s41422-020-0282-0. https://doi.org/10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Wang L, Shi W, Joyce MG, Modjarrad K, Zhang Y, Leung K, et al. Evaluation of candidate vaccine approaches for MERS-CoV. Nat Commun. 2015;6(1):1–11. doi: 10.1038/ncomms8712. https://doi.org/10.1038/ncomms8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Morse JS, Lalonde T, Xu S, Liu WR. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem. 2020;21(5):730–8. doi: 10.1002/cbic.202000047. https://doi.org/10.26434/chemrxiv.11728983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Klein A. Drug trials under way. [Mar 17;2020 ];NewScientist. 2020 245:3270–6. https://doi.org/10.1016/S0262-4079(20)30376-6 Available via https://www.latinpost.com/articles/144190/20200316/facts-about-favilavir-the-first-approved-coronavirus-drug.htm . [Google Scholar]
- [74].The Daily Star. [Mar 14;2020 ]; Available via https://www.thedailystar.net/frontpage/news/coronavirus-outbreak-screening-still-lax-dhaka-airport-1878607 .
- [75].Wang M, Jiang A, Gong L, Luo L, Guo W, Li C, et al. Temperature significant change COVID-19 Transmission in 429 cities. medRxiv. 2020 https://doi.org/10.1101/2020.02.22.20025791. [Google Scholar]