Abstract
Emerging studies on radiologic findings in patients with coronavirus disease 2019 (COVID-19) report a high incidence of bilateral lung involvement, with ground-glass opacities imaging being the most common pattern on computed tomography. Cystic lesions, such as pneumatoceles, are rare, although they may occur in 10% of cases. Cyst formation may be explained by a focal pulmonary trauma caused by mechanical ventilation or infection-related damage to the alveolar walls leading to pneumatoceles. The superinfection of pneumatoceles is a potential life-threatening condition for which no standardized therapeutic algorithm has been accepted. We report a case of a COVID-19 patient successfully treated by lung resections for infected pneumatoceles.
In early December 2019, the first cases of pneumonia from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were identified in Wuhan, China.1 Since then, coronavirus disease 2019 (COVID-19) has rapidly become pandemic, causing more than 5,200,000 cases and more than 337,000 deaths worldwide.2 The most common clinical presentation includes fever, cough, and bilateral ground-glass opacities. However, COVID-19 has a wide spectrum of severity, ranging from asymptomatic cases to patients admitted to the intensive care unit (ICU) with acute respiratory distress syndrome (ARDS).
In some patients, pneumatoceles may occur due to damage to the alveolar walls caused by the infection or by lung ventilation.3 , 4 Superinfection of pneumatoceles may represent a potential life-threatening complication; in this case, an urgent surgical approach is recommended.5
A 55-year-old man, who was a nonsmoker, arrived at the emergency department of the Hospital of Cremona (Lombardy Region, Italy) with fever and dyspnea. The patient suffered from arterial hypertension, overweight (body mass index, 27 kg/m2), and impaired glucose tolerance. The nasopharyngeal swab for COVID-19 tested positive. Pulmonary computed tomographic (CT) angiography documented bilateral interstitial changes with smooth interlobular septal thickening (Figure 1 ).
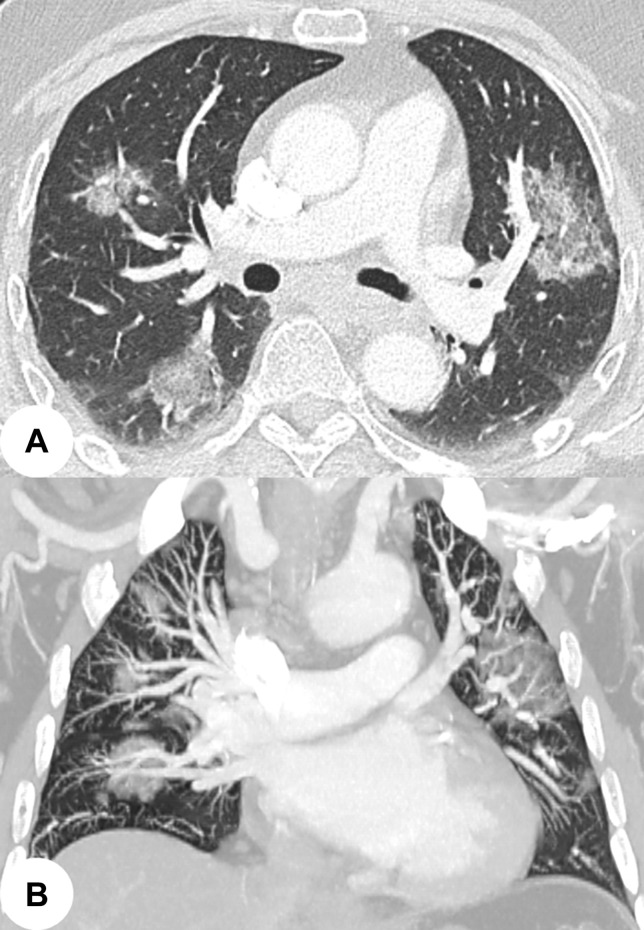
Figure 1.
Computed tomographic images in (A) axial and (B) frontal views document severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) pneumonia on arrival at the emergency department.
As a result of the worsening of respiratory insufficiency despite medical therapy and noninvasive ventilation, the patient was intubated and then transferred to our Institute because of the lack of ICU beds. On admission, laboratory values were white blood cells, 13.980/mm3; neutrophils, 81.1%; lymphocytes, 6.4%; C-reactive protein, 22.50 mg/dL; and D-dimer, 4187 ng/mL. Ventilator settings were mainly as follows: tidal volume, 6 mL/kg; respiratory rate, 21 breaths/min; positive end-expiratory pressure, 8 cm H2O; and fraction of inspired oxygen, 70%.
After 3 weeks, the patient was extubated and noninvasive ventilation was started. The patient was transferred to the Department of Medicine to continue the medical therapy and oxygen support. The patient was readmitted to the ICU 4 days later and intubated for acute respiratory failure and sepsis. Blood culture results revealed Staphylococcus haemolyticus, and specific antibiotics were administered based on the antibiogram report. His clinical condition progressively worsened. The high fever persisted as did the septic state, despite antibiotics.
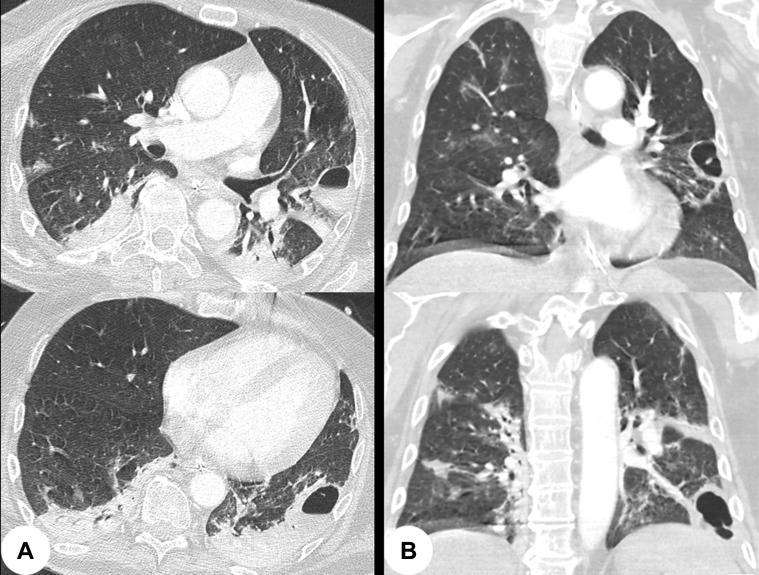
Because no evidence of recurrence of COVID-19 pneumonia was detected with a chest roentgenogram, a CT scan with contrast was requested. Images showed 2 round cystic lesions of 35 and 55 mm with hydro-air level located in the posterior segment of the left upper lobe and in the anterolateral segments of the left lower lobe (Figure 2 ). Furthermore, the CT confirmed the resolution of the bilateral COVID-19 pneumonia.
Figure 2.
Computed tomographic images in (A) axial and (B) frontal views document infected pneumatoceles and show no evidence of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) pneumonia.
Owing to rapid deterioration of the patient’s clinical condition, an urgent surgical procedure was discussed along with intensivists and anesthesiologists. Under general anesthesia, using double-lumen endotracheal intubation, the patient underwent a left lateral muscle-sparing thoracotomy. Video-assisted thoracoscopic surgery was excluded because prolonged single-lung ventilation would not have been tolerated.
After inspection of the lung, the 2 cystic lesions documented by the CT were identified and resected using Endo GIA 45 and 60 mm (Purple 3.0-4.0 mm) Tri-Staple Technology (Medtronic, St Paul, MN). At the end of the procedure no air leaks were noticed, and two 28F chest tubes were inserted. A tracheostomy was also performed.
Within 48 hours, the patient’s clinical condition dramatically improved. Fever and sepsis completely resolved in 1 week. The chest drains were removed in 5 days. The patient was discharged from the ICU on postoperative day 13.
Comment
Emerging reports on radiologic findings in patients with COVID-19 have documented a high incidence of bilateral lung involvement, with ground-glass opacities being the most common pattern on chest CT.1 , 3 Round cystic changes of lung parenchyma are rarely observed in the subclinical period and during the first 2 weeks after the onset of symptoms, although they occur in up to 10% of patients as the disease progresses.4 The formation of cystic lesions might be explained by the infection that causes damage to the alveolar walls, thus leading to pneumatoceles.4 Ventilator-induced lung injury might also play a role. In fact, prolonged ventilation with high-lung volumes may cause barotrauma with alveolar and intraacinar septa rupture; conversely, ventilation with low-lung volumes may cause atelectrauma, especially in patients with ARDS.5 Of note, interstitial involvement observed in COVID-19 seems similar to that observed in ARDS and compromises both compliance and elastance of the lungs.6
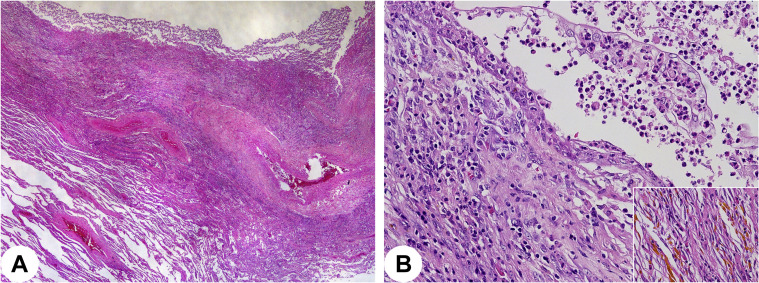
Recent pathologic examinations of lung specimens from patients with COVID-19 have shown a wide range of lung interstitial inflammation, with abundant infiltrating immune cells alongside thickened alveolar septa and interstitial fibrosis.7 , 8 The histologic specimens documented pus collection inside a cystic dilation of the lung parenchyma, which was characterized by acute and chronic inflammation and organizing pneumonia. Remnants of bronchiolar epithelium could be seen along with squamous metaplasia and hemosiderin accumulation (Figure 3 ). These findings favored newly formed cystic dilation in the peripheral lung parenchyma upon infection or barotrauma, or both.
Figure 3.
(A) A cystic space filled by pus was documented, with the wall being composed of inflammatory cells and organizing pneumonia (hematoxylin and eosin ×40). (B) Remnants of the bronchial epithelium with squamous metaplasia were seen to inconsistently cover cystic dilations, alongside hemosiderin accumulation (inset) (hematoxylin and eosin ×100, inset ×200).
Pneumatoceles complicated by infection require urgent treatment. Although there are no widely accepted therapeutic algorithms for the management of complicated pneumatoceles, some authors advocate early percutaneous drainage as a first-line strategy; on failure of this approach, surgical resection should be considered.5 However, an urgent surgical approach may be preferred in patients with critical clinical conditions because it may be lifesaving.
Similarly, we favored an open-approach to the standard thoracoscopy owing to the failure of prolonged single-lung ventilation. Moreover, the presence of adhesions or incomplete fissures due to the inflammatory process were considered preoperatively. Lung resections were performed conservatively on healthy margins. The aim was to preserve maximum pulmonary function and prevent postoperative complications, such as air leaks or peripheral bronchopleural fistula, by excising the infected pneumatoceles completely.
This report describes a COVID-19 patient who was successfully treated by an urgent surgical procedure for 2 infected pneumatoceles causing acute respiratory failure and sepsis that was nonresponsive to antibiotics. Surgical resection of lung lesions as a first-line strategy seems reasonable in a critically ill patient because it may be lifesaving.
References
- 1.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease 2019. Situation Report–125. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200524-covid-19-sitrep-125.pdf?sfvrsn=80e7d7f0_2 Available at:
- 3.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020 Feb 24 doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slutsky A.S., Ranieri V.M. Ventilator-Induced lung injury. N Engl J Med. 2013;369:2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 5.DiBardino D.J., Espada R., Seu P., Goss J.A. Management of complicated pneumatocele. J Thorac Cardiovasc Surg. 2003;126:859–861. doi: 10.1016/s0022-5223(03)00367-2. [DOI] [PubMed] [Google Scholar]
- 6.Aiolfi A., Biraghi T., Montisci A. Management of persistent pneumothorax with thoracoscopy and blebs resection in COVID-19 patients. Ann Thorac Surg. 2020;110:e413–e415. doi: 10.1016/j.athoracsur.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S.Y. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai Y., Hao Z., Gao Y. COVID-19 in the perioperative period of lung resection: a brief report from a single thoracic surgery department in Wuhan, China. J Thorac Oncol. 2020;15:1065–1072. doi: 10.1016/j.jtho.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]