Abstract
Purpose
This pilot study aimed to determine the feasibility of hip corrective taping to improve self-reported knee pain and lower extremity joint kinematics in basketball players with patellofemoral pain.
Patients and Methods
A single group pre-test and post-test design. Collegiate basketball players with patellofemoral pain were recruited. Three-dimensional hip and knee joint kinematics were measured during two tasks, single-leg squat (SLS) and lay-up jump (LUJ), and each task was conducted under no-taping and taping conditions. Subjective report of pain was compared between no-taping and taping conditions only during SLS.
Results
Twelve collegiate basketball players with patellofemoral pain (median age, 22.7 [2.5] years; mean height, 173.8 ± 7.4 cm; mean weight, 72.5 ± 12.8 kg) participated in this study. Compared with no-taping, the use of hip corrective taping significantly increased the hip abduction angle at the instant of the maximal vertical ground reaction force during LUJ (no-taping vs taping: 0.6° ± 6.3° vs 3.3° ± 5.1°, p = 0.029), and also caused a trend of decreased maximal hip internal rotation angle during SLS (no-taping vs taping: 8.0° ± 6.6° vs 4.7° ± 6.9°, p = 0.050). Hip corrective taping also improved self-reported knee pain during SLS (no-taping vs taping: 3.4 ± 1.7 vs 2.6 ± 1.0, p = 0.046).
Conclusion
Hip corrective taping may be used as an effective intervention for athletes with patellofemoral pain during basketball-related tasks.
Keywords: anterior knee pain, kinesio taping, biomechanics, hip joint
Introduction
Basketball is a popular team sport in the United States and around the world.1 Sport participation has many health benefits, but may also increase the risk of injuries.2 Many basketball players suffer from non-traumatic knee pain, with patellofemoral pain (PFP) being one of the most common conditions that affects 25% of the players.3,4 Patellofemoral pain is characterized by retropatellar and/or peripatellar pain that is aggravated by common basketball activities such as jumping, cutting, and pivoting.5 Daily activities like stair climbing, prolonged sitting, and kneeling may also induce anterior knee pain. Patellofemoral pain is not a self-limiting condition; a significant proportion of athletes with PFP limit their sports activities or eventually stop participating in sports because of persistent symptoms.6
A various combination of patho-mechanical factors may lead to the development of PFP.7 Patellar malalignment and/or patellar maltracking had long been considered as the main cause of PFP.8,9 As a result, many previous interventions only emphasized on the anatomical structures in and around the patella and patellofemoral joint, for example, strengthening the vastus medialis oblique, patellar mobilization, and patellar taping.10,11 New evidence showed that altered mechanics at the proximal (trunk and hip) and distal (foot) segments to the knee joint may also contribute to PFP.12,13 Excessive hip adduction and internal rotation during movements and excessive foot pronation have been observed in patients with PFP.12,13 Effective intervention should target these relevant risk factors.
Taping is a commonly used technique for treatment of PFP in clinical practice. The conventional taping technique aims to modify local factors of PFP by improving the patellar alignment. The McConnell taping technique uses rigid tapes to reposition the patella correctively within the femoral trochlea.14 Japanese Chiropractor Dr Kenso Kase invented kinesio taping in the mid-1970s.15 Compared to rigid tapes, the stretchable and breathable kinesio tape can provide support without restricting range of motion and be worn over a longer period. In a recent systematic review comparing the effect of patellar taping using McConnell or Kinesio tape, the 11 included studies showed that both taping techniques had effects in pain reduction for patients with PFP.16 In contrast to McConnell taping, Kinesio taping can improve muscle flexibility, muscle activity, and motor functions but cannot influence patellar alignment.16
Recently, some researchers applied kinesio tape to correct the hip kinematics in patients with PFP.17,18 Kinesio tape was applied spirally on the thigh to restrict hip internal rotation and adduction during lower limb loading. The results showed that hip corrective taping significantly reduced knee pain and altered patellar displacement and rotation during single-leg squat (SLS); however, no significant changes were found in the hip joint excursion angles.17 The researchers explained that the total hip joint excursion may not be a sensitive measurement because the taping might have altered the joint position instead. Whether the reduced PFP was attributed from the reduced hip internal rotation and adduction with hip corrective taping remains unknown. Another limitation of previous studies is that joint kinematics was assessed during a standardized and relatively static task in a general population with PFP,17,18 which may be inadequate in representing how hip corrective taping influences lower extremity joint kinematics during more dynamic sport-specific movement tasks in athletes.
Given the high basketball participation rate and the impact of PFP in basketball players,19,20 it is important to understand whether hip corrective taping is an effective intervention for PFP during performing basketball-related tasks. Prior to determining the effectiveness of hip corrective taping through a randomized controlled trial, this preliminary study was conducted to investigate whether improvements in self-reported knee pain and lower extremity joint kinematics during SLS and lay-up jump (LUJ) could be feasibly achieved through hip corrective taping in basketball players with PFP. We hypothesized that hip corrective taping would reduce knee pain and correct excessive hip internal rotation and adduction during movement tests.
Materials and Methods
Participants
Basketball players with clinically diagnosed PFP were recruited to participate in this study. Participants were screened and recruited from the varsity teams and clubs at the local universities. All participants had at least 3 years of experience playing basketball, currently practiced basketball more than 1 day per week, had no trauma to the lower extremity in the past 6 months, and had no previous surgery in the lower extremity. A licensed physical therapist examined eligible participants and determined if they met the inclusion and exclusion criteria for PFP. The inclusion criteria were (1) experiencing retropatellar and/or peripatellar pain during at least two of the following functional activities: ascending stairs, descending stairs, running, jumping, hopping, and squatting; (2) pain lasting longer than 1 month; (3) pain intensity during above-mentioned activities greater than a 3 on a 10-cm visual analogue scale (VAS). The exclusion criteria were (1) referred pain from the lower back or hips; (2) positive findings on knee examination for meniscus (McMurray and Apley tests), ligament (Lachman’s, anterior/posterior drawer, pivot shift, and valgus/varus stress tests) or interarticular lesions (sweep test). The institutional review board of National Cheng Kung University Hospital approved this study (B-ER-101-168). The study was carried out in compliance with the Declaration of Helsinki, and all participants signed a written informed consent form prior to their inclusion in the study.
Instrumentation
A 6-camera VICON motion analysis system (model MX Giganet, T10, Oxford Metrics, UK) was used to capture the trajectories of reflective markers during SLS and LUJ. The sampling rate was set at 200 Hz. A total of 38 reflective markers were applied to define the body segments based on the Plug-in-Gait model: head (left-front, left-back, right-front, right-back,), bilateral upper extremities (acromion, upper arm, lateral epicondyle, forearm, radial styloid process, ulna styloid process, second knuckle), bilateral lower extremities (lateral femoral epicondyle, thigh, shank, lateral malleolus, heel, second toe), pelvis (bilateral anterior superior iliac spine and posterior superior iliac spine) and trunk (C7, T10, jugular notch, and xiphoid process). An AMTI force plate (Model OR6-6, Watertown, MA) was used to measure ground reaction force data with a sampling rate of 1000 Hz for determining the take-off phase of the LUJ.
The PFP Severity Scale (PSS)21 was used to measure PFP associated with functional activities over the past week. The scale consists of 10 items, including climbing stairs, squatting down, walking, jogging, running/sprinting, participating in a sport, sitting with knees bent (for 20 minutes), kneeling on knee for any time period, pain at rest/sleeping, and pain while resting following activity. The participants rated their pain on a 10-cm VAS, with one end point descriptor as “none” and the other as “unbearable”. The total maximum score for the PSS is 100. The PSS demonstrated strong concurrent validity with the WOMAC (Western Ontario and McMaster Universities) Osteoarthritis index and the Hughston Foundation subjective knee scale, and also has excellent test-retest reliability.21
Procedures
Basic information (age, height, weight, experience of playing basketball) and scores of PSS were collected. Then, participants performed 3 trials of 2 movement tests, SLS and LUJ, each under 2 taping conditions (no-taping and taping). The no-taping condition was performed first and followed by the taping condition in order to assess the immediate effect of pain relief and kinematic changes after taping on the same visit. Sufficient rest was provided between trials to minimize fatigue effects. Before kinematic data were collected, participants performed a 10-min warm-up and practiced each movement test until they were fully familiarized with the requirement. The leg to be tested and taped was the leg with PFP. If both knees were painful, the leg with a greater PPS score was chosen.
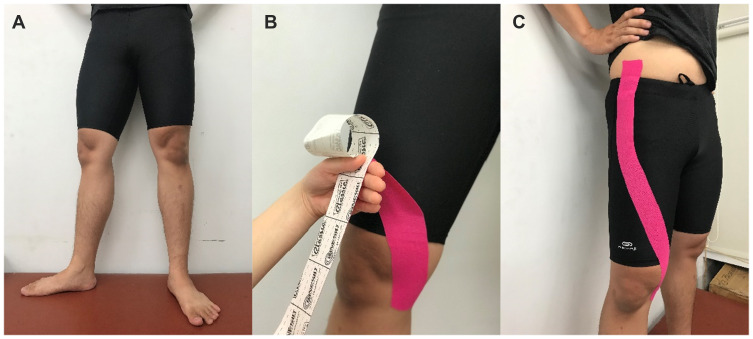
The kinesio tape (Kinesio® Tex Gold) was applied to induce hip external rotation and abduction forces. Before the application of kinesio tape, the skin was cleaned with alcohol swabs. In bare feet standing, the affected limb of each participant was positioned in maximal hip external rotation, slight abduction, and knee extension. An I strip of kinesio tape was anchored at the medial tibial condyle, then applied around anterior thigh with maximal tension, and attached on the anterior superior iliac spine (Figure 1). The hip corrective taping method17,18 was modified from the spiral method described by Dr. Kenso Kase and attempting for mechanical correction. All taping was applied by the same physiotherapist who was an experienced and certified kinesio taping practitioner.
Figure 1.
Illustration of the hip corrective taping using kinesio tape. The tape was placed outside the shorts only for demonstration. (A) The affected limb was positioned in maximal hip external rotation, slight abduction, and knee extension. (B) An I strip of kinesio tape was anchored at the medial tibial condyle and then applied around anterior thigh with maximal tension. (C) The tape was finally anchored on the anterior superior iliac spine.
Single-leg squat is the most common functional test performed in patients with PFP. Participants were asked to keep their arms across the chest, lift up the non-tested leg to 45° of hip and knee flexion, and then performed the squat until the tested knee flexed to at least 60°. Participants were instructed to maintain their trunk upright and the position of the non-tested leg during SLS. Participants were also required to rate their perceived pain intensity after completing 3 trials of the SLS.
Lay-up jump is a common point-scoring maneuver in basketball involving a higher level of power generation and joint loading. Participants were instructed to run from the starting point to the force plate (5.4 m apart) and executed the vertical jump and landing using the tested leg. To ensure that participants’ running speed reached at least 2.7 m/s,22 participants were instructed to complete the run during the 2-second time period signaled with two beep sounds. Participants did not hold a ball when performing LUJ, but they were asked to complete the upper extremity movement as they normally would do with a ball.
Data Analysis
Vicon Nexus 1.6.1 with Plug-In Gait version 1.9 was used to process kinematic data. The output angles of lower extremity were calculated from the YXZ cardan angles derived by comparing the relative orientations between segments. The joint angle was defined by the ordered rotations of flexion-abduction-rotation. All kinematics data of the tested leg were normalized to 100% of ground phase. The starting and take-off points of the LUJ were defined as the time when the ground reaction force was greater than and lesser than 10 N. The starting and ending points of the SLS were defined as the instance when knee started to flex and when the knee flexion angle reached the maximum, respectively. Kinematic variables of interest were three-dimensional hip and knee joint angles at the instant of initial contact and maximal vertical ground reaction force in LUJ. Maximum and minimum hip and knee joint angles as well as angular displacements during SLS and LUJ were also compared.
The normality assumption of all continuous variables was tested using the Shapiro–Wilk test. Mean values and standard deviations were calculated for normally distributed data, and median and interquartile range were calculated for skewed data. Paired t-tests were used to compare differences in pain intensity and joint kinematics between no-taping and taping conditions. The statistical significance level was set as p < 0.05. All data were analyzed using the SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA).
Results
Ten male and 2 female basketball players (median age 22.7 [2.5] years; mean height 173.8 ± 7.4 cm; mean weight 72.5 ± 12.8 kg) with PFP participated in this study. On average, the duration of knee pain was 39.9 ± 21.0 days, and the PSS score was 25.6 ± 13.6 points. Participants had 105.6 ± 37.2 months of experience playing basketball and practiced 4.2 ± 1.6 hours per week.
Single-Leg Squat Test
The mean VAS after 3 trials of SLS was 3.4 (± 1.7) without taping and 2.6 (± 1.0) with taping. Taping significantly reduced pain by 23.8% (p = 0.046). There was a trend of decreased maximum hip internal rotation angle with taping (p = 0.05), and no significant difference was found in all maximum hip and knee joint angles between the two taping conditions (p > 0.05, Table 1).
Table 1.
Maximum Hip and Knee Joint Angles During the Single-Leg Squat
| Joint | Plane of Motion | No-Taping | Taping | p |
|---|---|---|---|---|
| Hip | Sagittal | 69.0 ± 21.4 | 67.2 ± 22.9 | 0.469 |
| Frontal | 11.5 ± 5.5 | 10.2 ± 5.2 | 0.059 | |
| Transverse | 8.0 ± 6.6 | 4.7 ± 6.9 | 0.050 | |
| Knee | Sagittal | 85.3 ± 10.6 | 83.4 ± 11.0 | 0.350 |
| Frontal | 13.3 ± 7.0 | 11.0 ± 6.3 | 0.084 | |
| Transverse | 11.8 ± 5.7 | 10.4 ± 5.1 | 0.413 |
Notes: The data are mean (± standard deviation). Positive values represent flexion in the sagittal plane, adduction in the frontal plane, and internal rotation in the transverse plane.
Lay-Up Jump Test
The duration of LUJ under the no-taping and taping conditions was 0.25 ± 0.04 and 0.25 ± 0.05 seconds, respectively. There was no significant difference between the duration of LUJ under two taping conditions (p = 0.726). Taping significantly decreased the angle of hip flexion by 4.2° (p = 0.038) and knee external rotation by 2.2° (p = 0.038) at the initial contact of LUJ, and increased the angle of hip abduction at the instant of the maximal vertical ground reaction force by 2.7° (p = 0.029) (Table 2). However, taping did not change the maximum and minimum hip and knee joint angles and joint ranges during LUJ (Table 3).
Table 2.
Hip and Knee Joint Angles at the Initial Contact and Maximal Vertical Ground Reaction Force During the Lay-Up Jump
| Joint | Plane of Motion | No-Taping | Taping | p |
|---|---|---|---|---|
| At initial contact | ||||
| Hip | Sagittal | 48.5 ± 7.6 | 44.3 ± 6.9 | 0.038* |
| Frontal | −1.1 ± 4.8 | −2.0 ± 4.6 | 0.392 | |
| Transverse | −5.7 ± 8.4 | −2.0 ± 8.7 | 0.472 | |
| Knee | Sagittal | 22.7 ± 4.6 | 24.0 ± 6.5 | 0.490 |
| Frontal | −2.5 ± 4.4 | −2.1 ± 4.9 | 0.787 | |
| Transverse | −10.2 ± 5.1 | −8.0 ± 5.4 | 0.038* | |
| At maximal vertical ground reaction force | ||||
| Hip | Sagittal | 28.6 ± 11.7 | 23.4 ± 11.8 | 0.103 |
| Frontal | −0.6 ± 6.3 | −3.3 ± 5.1 | 0.029* | |
| Transverse | 1.2 ± 9.1 | −3.1 ± 10.0 | 0.096 | |
| Knee | Sagittal | 44.4 ± 7.3 | 40.7 ± 7.0 | 0.222 |
| Frontal | −2.6 ± 6.1 | −4.6 ± 5.9 | 0.260 | |
| Transverse | 8.6 ± 5.2 | 12.4 ± 4.2 | 0.054 | |
Notes: The data are mean (± standard deviation). Positive values represent flexion in the sagittal plane, adduction in the frontal plane, and internal rotation in the transverse plane. Negative values represent extension in the sagittal plane, abduction in the frontal plane, and external rotation in the transverse plane. *p < 0.05.
Table 3.
Maximum and Minimum Hip and Knee Joint Angles and Joint Ranges During the Lay-Up Jump
| Joint/Plane of Motion | Angle | No-Taping | Taping | p |
|---|---|---|---|---|
| Hip/Sagittal | Maximum | 48.1 ± 5.9 | 47.0 ± 5.9 | 0.380 |
| Minimum | 2.2 ± 6.2 | 2.0 ± 6.3 | 0.871 | |
| Range | 50.3 ± 4.3 | 49.0 ± 7.0 | 0.365 | |
| Hip/Frontal | Maximum | 9.6 ± 4.2 | 8.5 ± 4.9 | 0.323 |
| Minimum | −12.4 ± 4.1 | −12.0 ± 4.4 | 0.132 | |
| Range | 21.6 ± 7.1 | 20.5 ± 7.1 | 0.185 | |
| Hip/Transverse | Maximum | 7.6 ± 7.6 | 8.2 ± 8.9 | 0.800 |
| Minimum | −11.8 ± 8.4 | −12.3 ± 11.8 | 0.861 | |
| Range | 19.3 ± 6.0 | 20.5 ± 7.6 | 0.689 | |
| Knee/Sagittal | Maximum | 52.9 ± 5.7 | 52.9 ± 5.7 | 0.951 |
| Minimum | 10.1 ± 6.0 | 9.7 ± 7.4 | 0.712 | |
| Range | 42.8 ± 4.9 | 43.3 ± 9.4 | 0.773 | |
| Knee/Frontal | Maximum | 3.6 ± 3.2 | 2.8 ± 2.9 | 0.227 |
| Minimum | −8.5 ± 5.2 | −9.7 ± 7.4 | 0.712 | |
| Range | 12.1 ± 4.9 | 12.5 ± 5.4 | 0.659 | |
| Knee/Transverse | Maximum | 17.5 ± 5.1 | 18.2 ± 3.7 | 0.672 |
| Minimum | −13.7 ± 4.4 | −11.6 ± 3.5 | 0.119 | |
| Range | 31.2 ± 7.4 | 29.8 ± 4.9 | 0.472 |
Notes: The data are mean (± standard deviation). Positive values represent flexion in the sagittal plane, adduction in the frontal plane, and internal rotation in the transverse plane. Negative values represent extension in the sagittal plane, abduction in the frontal plane, and external rotation in the transverse plane.
Discussion
Altered hip kinematics has been observed in people with PFP.17,23 Excessive hip internal rotation and adduction can influence relative position between patellar and femur and stress the structures of the patellofemoral joint, which contributes to PFP.7,24 This preliminary study aimed to investigate whether proximal hip control via kinesio taping could improve self-reported knee pain and lower extremity joint kinematics in basketball players with PFP. This study provided preliminary results that hip corrective taping improved self-reported knee pain, and also induced some changes in hip and knee joint kinematics during SLS and LUJ.
The conventional patellar taping techniques like McConnell taping or Kinesio taping attempting to correct abnormal alignment of the patella have been shown to effectively reduce knee pain in patients with PFP.25,26 Based on the findings of dynamic magnetic resonance imaging (MRI), some researchers proposed that the effect of patellar taping on pain reduction resulted from increased patellofemoral joint contact area.27 However, there is evidence to suggest that in people with PFP patellofemoral malalignment and/or maltracking during weight bearing may be the result of internal rotation of the femur as opposed to lateral tilt/displacement of the patella based on a dynamic MRI study.28 The hip corrective taping technique was developed, aiming to correct excessive hip internal rotation and adduction. The current study and the studies of Song et al.17,18 utilized the hip corrective taping in people with PFP, and all three studies demonstrated positive outcome on self-reported knee pain. Song, Huang, Chen, Lin, Chang17 did not find any significant changes in the hip joint excursion angle during SLS with hip corrective taping although the PFP was reduced. The researchers explained that the effect of hip corrective taping on reducing knee pain might have been achieved by decreased quadriceps activity and more posteriorly and distally shifted patella. In contrast to the results of Song, Huang, Chen, Lin, Chang,17 the current study showed that hip corrective taping could alter abnormal hip kinematics in basketball players with PFP. There was a statistically significant increase in the hip abduction angle at the instant of the maximal vertical ground reaction force during LUJ, and also a trend of decreased maximal hip internal rotation angle during SLS. With limited studies examining the effects of hip corrective taping, this is the only study demonstrating its effect on altering lower extremity kinematics during dynamic activities. The preliminary results of the current study suggest that hip corrective taping could be applied to reduce undesired hip internal rotation and knee pain for basketball players with PFP during practice or games. Minimizing such biomechanical risk factors contributing to PFP during activities by maintaining a proper lower extremity alignment in the frontal plane with the hip, knee, and ankle joints aligned in one line might be an important consideration for PFP management.
Previously, a hip stabilization brace has been developed to provide external rotation and abduction forces to the hip joint, with the intent of limiting excessive hip internal rotation and adduction motions during functional activities. Studies have shown that application of a hip stabilization brace in patients with PFP significantly improved mediolateral postural stability during a step-down test29 as well as decreased hip internal rotation and adduction during a drop jump task.30 However, the hip strapping brace is expensive and not easy to wear. In addition, the thick and heavy fabric of the brace may feel muggy and uncomfortable during exercise. The hip corrective taping method using kinesio tape in this study could be an alternative for hip stabilization brace, with the advantages of being inexpensive, light weight, and breathable.
Lay-up jump is one of the most commonly performed movements during a basketball game, and significantly affects point scoring. The LUJ involves a single-leg take-off for maximal height and single-leg landing. Hip corrective taping used in this study might have slightly affected the sagittal hip movement at the initial contact of the LUJ. However, the findings of no statistically significant change in the hip and knee joint excursions in all anatomical planes during the LUJ suggest that hip corrective taping would not affect the overall execution of the task, and thus not influence the performance of LUJ. The slightly decreased knee external rotation angle at the initial contact of the LUJ might be related to altered foot placement during a dynamic movement task or sensory cue from the anchor of the taping at the medial tibia. The above inferences need further investigation.
Besides mechanical explanation, the gate control theory is often discussed for pain control with kinesio taping.31,32 The kinesio tape stimulates mechanoreceptors with light touch in the skin and subsequently inhibits the transmission of pain to the sensory cortex;33 therefore, less pain is perceived. Another possible mechanism is via skin convolutions created by the application of kinesio tape.16,32 Increasing the space of fascia to improve the circulation can remove pain-producing substances, and also reduce the pressure on nociceptors. In addition, applying kinesio tape on the thigh may also influence proprioceptive sense or neuromuscular control, which could contribute to changes in joint kinematics.
There were several limitations in this study. First, the sample size was small with only 12 basketball players with PFP. The participants in the current study were recreational players; hence, the results may not generalize to the population of elite basketball players with PFP. We also did not control some potential confounding factors, for example, excluding participants with pronated foot. Second, as a preliminary study without a control group, this study is unable to determine the effectiveness of hip corrective taping for PFP. Lastly, we only investigated the immediate changes, and did not include other biomechanical measurements like electromyography.
Conclusion
The results of this non-controlled pilot study in a small sample suggest that hip corrective taping may be an effective intervention for athletes with patellofemoral pain during basketball-related tasks.
Acknowledgments
This work was supported by The Ministry of Science and Technology of Taiwan under Grants [MOST 106-2410-H-006 −081 -MY3 and MOST 106-2410-H-006 −083 -MY2]. Ya-Wen Hsu is currently affiliated with Department of Hospital and Health Care Administration, Chia Nan University of Pharmacy and Science, Tainan, Taiwan.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Trojian TH, Cracco A, Hall M, Mascaro M, Aerni G, Ragle R. Basketball injuries: caring for a basketball team. Curr Sports Med Rep. 2013;12(5):321–328. doi: 10.1097/01.CSMR.0000434055.36042.cd [DOI] [PubMed] [Google Scholar]
- 2.Owoeye OBA, Akinbo SRA, Giwa SO. Sport participation and injuries among undergraduate students of a Nigerian University. Afr J Med Med Sci. 2016;45(2):171–178. [PubMed] [Google Scholar]
- 3.Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access J Sports Med. 2017;8:143–154. doi: 10.2147/OAJSM.S133406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith BE, Selfe J, Thacker D, et al. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS One. 2018;13(1):e0190892–e0190892. doi: 10.1371/journal.pone.0190892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halabchi F, Abolhasani M, Mirshahi M, Alizadeh Z. Patellofemoral pain in athletes: clinical perspectives. Open Access J Sports Med. 2017;8:189–203. doi: 10.2147/OAJSM.S127359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rathleff MS, Rasmussen S, Olesen JL. Unsatisfactory long-term prognosis of conservative treatment of patellofemoral pain syndrome. Ugeskr Laeger. 2012;174(15):1008–1013. [PubMed] [Google Scholar]
- 7.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639 [DOI] [PubMed] [Google Scholar]
- 8.Sanchis-Alfonso V, Rosello-Sastre E, Martinez-Sanjuan V. Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. Am J Knee Surg. 1999;12(1):29–40. [PubMed] [Google Scholar]
- 9.Goodfellow J, Hungerford DS, Woods C. Patello-femoral joint mechanics and pathology. 2. Chondromalacia patellae. J Bone Joint Surg Br. 1976;58(3):291–299. doi: 10.1302/0301-620X.58B3.956244 [DOI] [PubMed] [Google Scholar]
- 10.Powers CM. Rehabilitation of patellofemoral joint disorders: a critical review. J Orthop Sports Phys Ther. 1998;28(5):345–354. doi: 10.2519/jospt.1998.28.5.345 [DOI] [PubMed] [Google Scholar]
- 11.Shelton GL. Conservative management of patellofemoral dysfunction. Prim Care. 1992;19(2):331–350. [PubMed] [Google Scholar]
- 12.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd international research retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. doi: 10.2519/jospt.2012.0301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis IS, Powers CM, Davis IS, Powers C. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30–May 2, 2009, fells point, Baltimore, MD. J Orthop Sports Phys Ther. 2010;40(3):A1–16. doi: 10.2519/jospt.2010.0302 [DOI] [PubMed] [Google Scholar]
- 14.Mostamand J, Bader DL, Hudson Z. The effect of patellar taping on joint reaction forces during squatting in subjects with patellofemoral pain syndrome (PFPS). J Bodyw Mov Ther. 2010;14(4):375–381. doi: 10.1016/j.jbmt.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 15.Williams S, Whatman C, Hume PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med. 2012;42(2):153–164. doi: 10.2165/11594960-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 16.Chang WD, Chen FC, Lee CL, Lin HY, Lai PT. Effects of kinesio taping versus McConnell taping for patellofemoral pain syndrome: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2015;2015:471208. doi: 10.1155/2015/471208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song CY, Huang HY, Chen SC, Lin JJ, Chang AH. Effects of femoral rotational taping on pain, lower extremity kinematics, and muscle activation in female patients with patellofemoral pain. J Sci Med Sport. 2015;18(4):388–393. doi: 10.1016/j.jsams.2014.07.009 [DOI] [PubMed] [Google Scholar]
- 18.Song CY, Lin JJ, Chang AH. Effects of femoral rotational taping on dynamic postural stability in female patients with patellofemoral pain. Clin J Sport Med. 2017;27(5):438–443. doi: 10.1097/JSM.0000000000000392 [DOI] [PubMed] [Google Scholar]
- 19.Trojan JD, Treloar JA, Smith CM, Kraeutler MJ, Mulcahey MK. Epidemiological patterns of patellofemoral injuries in collegiate athletes in the United States from 2009 to 2014. Orthop J Sports Med. 2019;7(4):2325967119840712. doi: 10.1177/2325967119886591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foss KD, Myer GD, Magnussen RA, Hewett TE. Diagnostic differences for anterior knee pain between sexes in adolescent basketball players. J Athl Enhanc. 2014;3(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laprade JA, Culham EG. A self-administered pain severity scale for patellofemoral pain syndrome. Clin Rehabil. 2002;16(7):780–788. doi: 10.1191/0269215502cr553oa [DOI] [PubMed] [Google Scholar]
- 22.Brown CN, Padua DA, Marshall SW, Guskiewicz KM. Hip kinematics during a stop-jump task in patients with chronic ankle instability. J Athl Train. 2011;46(5):461–467. doi: 10.4085/1062-6050-46.5.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885 [DOI] [PubMed] [Google Scholar]
- 24.Lee TQ, Morris G, Csintalan RP. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686 [DOI] [PubMed] [Google Scholar]
- 25.Whittingham M, Palmer S, Macmillan F. Effects of taping on pain and function in patellofemoral pain syndrome: a randomized controlled trial. J Orthop Sports Phys Ther. 2004;34(9):504–510. doi: 10.2519/jospt.2004.34.9.504 [DOI] [PubMed] [Google Scholar]
- 26.Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21–28. doi: 10.4085/1062-6050-43.1.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derasari A, Brindle TJ, Alter KE, Sheehan FT. McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010;90(3):411–419. doi: 10.2522/ptj.20080365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Souza RB, Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285. doi: 10.2519/jospt.2010.3215 [DOI] [PubMed] [Google Scholar]
- 29.Lee SP, Souza RB, Powers CM. The influence of hip abductor muscle performance on dynamic postural stability in females with patellofemoral pain. Gait Posture. 2012;36(3):425–429. doi: 10.1016/j.gaitpost.2012.03.024 [DOI] [PubMed] [Google Scholar]
- 30.Selkowitz D, Souza R, Powers C. Effect of femoral strapping on lower extremity kinematics and pain response in females with patellofemoral pain. In: First International Patellofemoral Pain Syndrome Research Retreat; April, 2009; Baltimore, MD. [Google Scholar]
- 31.Artioli DP, Bertolini GRF. Kinesio taping: application and results on pain: systematic review. Fisioter Pesqui. 2014;21(1):94–99. doi: 10.1590/1809-2950/553210114 [DOI] [Google Scholar]
- 32.Wu W-T, Hong C-Z, Chou L-W. The kinesio taping method for myofascial pain control. Evid Based Complement Alternat Med. 2015;2015:950519. doi: 10.1155/2015/950519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moayedi M, Davis KD. Theories of pain: from specificity to gate control. J Neurophysiol. 2013;109(1):5–12. doi: 10.1152/jn.00457.2012 [DOI] [PubMed] [Google Scholar]