Abstract
Extensive heterogeneity in autism spectrum disorder (ASD) has hindered the characterization of consistent biomarkers, which has led to widespread negative results. Isolating homogenized subtypes could provide insight into underlying biological mechanisms and an overall better understanding of ASD. A total of 1093 participants from the population-based “Healthy Brain Network” cohort (Child Mind Institute in the New York City area, USA) were selected based on score availability in behaviors relevant to ASD, aged 6–18 and IQ >= 70. All participants underwent an unsupervised clustering analysis on behavioral dimensions to reveal subgroups with ASD traits, identified by the presence of social deficits. Analysis revealed three socially impaired ASD traits subgroups: (1) high in emotionally dysfunctional traits, (2) high in ADHD-like traits, and (3) high in anxiety and depressive symptoms. 527 subjects had good quality structural MRI T1 data. Site effects on cortical features were adjusted using the ComBat method. Neuroimaging analyses compared cortical thickness, gyrification, and surface area, and were controlled for age, gender, and IQ, and corrected for multiple comparisons. Structural neuroimaging analyses contrasting one combined heterogeneous ASD traits group against controls did not yield any significant differences. Unique cortical signatures, however, were observed within each of the three individual ASD traits subgroups versus controls. These observations provide evidence of ASD traits subtypes, and confirm the necessity of applying dimensional approaches to extract meaningful differences, thus reducing heterogeneity and paving the way to better understanding ASD traits.
Subject terms: Diagnostic markers, Human behaviour, Neuroscience, Prognostic markers, Autism spectrum disorders
Introduction
Autism spectrum disorder (ASD) is a complex array of neurodevelopmental conditions typically characterized by social interaction and communication impairments, and restricted and repetitive behaviors1. The heterogeneity of ASD, reflected in its etiology, development, and biological phenotypes, presents an enormous challenge in the delineation and understanding of the disorder. It is therefore fundamental to define distinct subgroups of ASD, and dimensional approaches have been proposed as one way to perform this.
It has been suggested that autistic traits, in particular social and communication deficits, are distributed along a continuum extending into the general population2–5. Core autistic traits are often concomitant with behavioral traits varying in type and degree, thus further complicating the characterization of ASD. Common symptoms reported in ASD patients include anxiety6, depressive symptoms7, aggression8, attention deficits9, hyperactivity10, and sleep difficulties11. ASD patients are also more likely to present medical issues including seizures12, immune system abnormalities13, and gastrointestinal disorders14. Behavioral symptoms often indicate the presence of comorbid psychiatric disorders such as attention-deficit/hyperactivity disorder (ADHD), major depressive disorder, anxiety disorders, and conduct disorders. This complexity enforces the legitimacy of implementing a dimensional approach to examine continuous autistic traits and fluctuating behavioral symptoms as inter-correlated constructs varying in expression. A dimensional approach can promote stratification according to behavioral and biological features as suggested by the Research Domain Criteria15.
A prominently studied biological feature in ASD is cortical morphometry. In particular, ASD is accompanied by a range of aberrant cortical patterns present in both volumetric and surface-based morphology studies16,17. Several case-control studies have reported various changes in thickness including increases16,18 and decreases19,20. Surface area in ASD has been less investigated, with most results reporting no differences16,21,22. Studies have also reported significant global increases in surface area at younger ages23,24, as well as decreases in later stages of life24. Gyrification observations within ASD on the other hand have greatly reported increases17,21,25,26, with few showing decreases27,28. Though neuroanatomical investigations in ASD have remained largely unreplicated, few observations have persisted. This includes early brain overgrowth in frontal and temporal lobes29–31, causing children to achieve a nearly developed brain volume earlier than controls. Also, longitudinal studies in cortical thickness have shown a general trajectory of accelerated thinning with age in ASD patients versus controls in frontal, temporal, and parietal areas22,32. We presume that the general variability and lack of reproducibility is due to the frequently encountered practice of combining heterogeneous ASD patients into one group within case-control studies.
The objective of the present study is to thus disentangle and better understand the behavioral heterogeneity in ASD by using subjects with autistic traits to extract refined cortical morphometry features. To observe how behavioral dimensions distribute in a general population of children and adolescents that vary in degree of social impairment spreading across the spectrum, we designed the following experiment. We chose a broad age range (5–18), including males and females, within a large-scale multidimensional population-based cohort in order to capture a larger effect variance (compared to a purely ASD cohort) by focusing on behavioral constructs, and not an ASD diagnosis. We then conducted an unsupervised clustering analysis on the z-scores of several behaviors, especially chosen due to their manifestation in ASD, in order to isolate data-driven subgroups high in our dimension of interest: social impairment, which is a surrogate of autistic traits3,33. Extracted subgroups were subsequently combined into one autistic traits group and compared in cortical surface features (thickness, gyrification, and surface area) to the remainder of the population (i.e., the remaining subgroups that do not exhibit high social impairments, serving as our controls), thus mimicking a case-control study. We show that the case-control paradigm does not extract meaningful cortical features and that behavioral stratification is required. Therefore, in order to achieve clinically relevant morphometric signatures, we ran morphological analyses comparing each of our isolated socially impaired subgroups to controls. This should provide us with a better understanding of underlying heterogeneity present in the physiology of autistic traits, and ultimately ASD.
Materials and methods
Part 1: Clinical profiles
HBN cohort and participants
The Healthy Brain Network (HBN) cohort initiative within the Child Mind Institute began in 2015 with the goal of collecting brain imaging, cognitive/behavioral, and genetic data for 10,000 children and adolescents (5–21 years old) to investigate the heterogeneity behind neuropsychiatric and neurocognitive development34. It comprises a population of individuals at-risk for developing psychiatric disorders and typically developing participants. Subjects were recruited through flyer dissemination and subsequently assessed on clinical questionnaires at three sites in New York City, USA: Staten Island, Mobile Van, Midtown.
In the status of the HBN cohort, consensus diagnostics are not available for most of the subjects enrolled; however, this does not preclude the possibility to carry out our dimensional study since subjects were not selected based on an ASD diagnosis, but rather on the presence of behavioral constructs relevant in the field of ASD. There were 1800 subjects participating at the time of this study, of which 1093 remained based on available overlap in behavioral scores assessing social deficits, hyperactivity, anxiety, irritability, depression, aggression, and attention problems, and having a full-scale Intelligence Quotient (FSIQ) >= 70. We selected these seven behaviors due to their presence in comorbid psychiatric disorders commonly reported in ASD patients, and therefore their frequent emergence along the autistic behavioral spectrum, implicating them in the understanding of ASD behavioral neuropathology35–39. Full-scale IQ was measured using the Wechsler Adult Intelligence Scale (WAIS-III, for those over 16) or the Wechsler Intelligence Scale for Children (WISC-III). Written informed consent was obtained from legal guardians and from participants themselves. This cohort study initiative was approved by the Chesapeake Institutional Review Board.
Behavioral assessments
One of the most prominent dimensions in ASD patients is social impairment. Here, we used data from the widely used 65-item parent social responsiveness scale (SRS) as a quantitative measure of clinical autistic traits, making it the central variable of interest in our study and in fact the score from which we separate out our autistic traits individuals. The SRS has been proven as a valid measure of autistic traits and thus has been used as a measure of autistic traits (for the purpose of understanding ASD) in several behavioral, genetic, and neuroimaging studies3,28,32,33,40–44. Though not a diagnostic tool, the SRS exhibits high inter-rater and cross-cultural reliability, and correlates greatly with the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview—Revised (ADI-R) diagnostic assessments for ASD from the DSM-5, making it a robust measure to use in the dimensional study of ASD behaviors3,33,40,45. Similarly, for the remaining behaviors we did not use diagnostic assessments but rather scales measuring behavioral trait severity. Hyperactivity levels were determined using the hyperactivity subscale within the Strengths and Difficulties Questionnaire (SDQ)46; anxiety was measured using the total score from the Screen for Child Anxiety Related Disorders Parent-Report (SCARED-P)47; irritability was defined using the total score of the Affective Reactivity Index Parent-Report (ARI-P)48; and lastly, levels of depression, aggression, and attention problems were determined using subscales of the same names within the Child Behavioral Checklist (CBCL)49.
Unsupervised clustering analysis (K-means)
We conducted a k-means analysis on scaled z-scores of the previously mentioned 7 behaviors. This extracted subgroups varying in SRS and other accompanying behavioral characteristics. Briefly, k-means is an algorithm identifying mean cluster centroids, which serves to partition a sample into k subgroups50. A substantial challenge in such analyses lies in determining the number of clusters, which is a user-defined parameter. To address this problem, the chosen number of clusters k was determined using a Bayesian Information Criterion (BIC) distribution (Supplementary Fig. 1)51.
Mean behavioral scores, FSIQ and age were compared between subgroups using non-parametric 2-sided Mann–Whitney U tests, while gender differences were determined using a chi-square test. Python version 2.7 and R 3.4.0 were used on a Linux platform to perform all analyses in this study. Python packages used include Pandas (version 0.19.2), SciPy (version 1.1.0), and Matplotlib (version 1.5.1).
Part 2: Neuroimaging analysis of cortical surface features
Structural MRI acquisition and processing
MRI acquisition took place at three different sites: mobile 1.5T Siemens Avanto in Staten Island, 3T Siemens Tim Trio at Rutgers University Brain Imaging Center, and 3T Siemens Prisma at the CitiGroup Cornell Brain Imaging Center (acquisition protocols are extensively described in Alexander et al. 34).
T1-weighted images were processed using the FreeSurfer software version 6.0.0 (https://surfer.nmr.mgh.harvard.edu/). For more information on precise methods of image analysis and the construction of anatomical information for each individual done by this software, refer to52,53. Briefly, the FreeSurfer analysis stream includes intensity normalization, skull stripping, and segmentation of gray (pial) and white matter surfaces52. Subsequent tessellation, as well as various topology corrections and inflation, leads to 3D meshes of cortical surfaces in different resolutions. Our work is based on a tessellation with ~160,000 vertices per hemisphere and used the FreeSurfer fsaverage template. We focused on three morphological measures of which the processing stream created vertex-wise maps for analysis: cortical thickness (CT), surface area (SA), and gyrification (lGI). The local gyrification index is measured as the ratio between buried and visible cortex54. All images were manually inspected in-house, in addition to using the Euler number as a metric of quality by retaining images at a threshold of -217, as specified in Rosen et al. 55.
Elimination of site effects on cortical features using ComBat
A harmonization process was performed to account for the multiple acquisition sites. Features extracted from structural MR images are prone to technical variability across acquisition centers such as differences in scanning parameters, scanner manufacturers and field strengths. In order to remove cortical feature bias and variability caused by the unwanted site effects, the ComBat technique was applied to harmonize feature data along our three acquisition centers. This method adjusts the mean value and variance of feature measures across sites56.
Statistical analysis
Vertex-wise statistical analyses were conducted using the command-line group analysis stream in FreeSurfer. Cortical surfaces for each participant were first registered to a study-specific template, then smoothed using a full-width-at-half maximum (FWHM) kernel of 10 mm for CT and SA, and 5 for lGI. A general linear model was fit at each vertex i to compare the three morphological measures between groups, using gender as a categorical covariate, and age and FSIQ as continuous covariates (site effects were already accounted for at the vertex level), and including the residual error:
We performed a cluster-level analysis using a cluster-forming threshold of p = 0.01. We report clusters with cluster-wise p-value (cwp) of cwp <0.05. These p-values were corrected for multiple comparisons using the mri_glmfit-sim precomputed MonteCarlo simulation.
Results
Part 1: Clinical profiles
Data-driven behavioral subgroups in HBN cohort
Based on the computed BIC value distribution, a k value of 9 was retained as our supervised partitioning for this study (Supplementary Fig. 1). Thus, upon running the clustering analysis, we obtained nine subgroups with various behavioral profiles (Table 1). The average SRS levels were used to decide which subgroups represented high autistic traits participants and which were controls. From these nine subgroups, three expressed high levels of SRS, representing our socially impaired “high autistic traits” subgroups. The SRS levels of these three subgroups fall within the “severe” or at least upper “moderate” classification of the SRS scale (an SRS value above ~80), thus indicating a high level of social impairment, providing us with greater confidence that subjects within these subgroups have “autistic-like” traits (Supplementary Fig. 2). Additionally, mean SRS values in these three subgroups are comparable to the average SRS level of ~86 reported in diagnosed ASD patients33,57,58. Regarding the behavioral compositions of our three high autistic traits subgroups, one subgroup showed high levels of reactivity, aggression, and ADHD-like symptoms (hyperactivity and attention issues), n = 107 (described as emotional dysregulation—Emot); the second maintained normal levels in all behavioral scores except for attention problems and hyperactivity, n = 82 (described as attention problems—Attn); and the third showed high levels of anxiety and depression, as well as attention deficits, n = 61 (described as anxiety depression—AnxDep) (Fig. 1). Clinically high levels were determined for each behavioral measure according to the literature3,47,48,59–61. Though the remaining six subgroups contained subjects with SRS values ranging from low to high, each of these subgroups maintained an overall low SRS mean and were thus combined as our control group (n = 843) with the aim of creating a representative general population without autistic traits subjects. Studies often barely obtain additional behavioral information on their controls other than a “non-diagnosis” or “low SRS”. By combining these remaining six subgroups into one control group, we smooth out several behavioral heterogeneities and yield a control group composed of a wide behavioral spectrum, while still maintaining low mean levels of SRS (our target variable of interest to be contrasted in subsequent analyses) (Supplementary Fig. 3).
Table 1.
Nine resultant subgroups from clustering analysis.
| Subgroups | n (Total = 1093) | SRS (s.d.): Social Deficits | SCARED-p (s.d.): Anxiety | ARI-p (s.d.): Reactivity | SDQ-Hyperactivity (s.d.) | CBCL-AB (s.d.): Aggression | CBCL-AP (s.d.): Attention Problems | CBCL-WD (s.d.): Depression | Mean Age (s.d.) | Gender Ratio | Mean FSIQ (s.d.) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Subgroup 1 (AnxDep) | 61 | 88.7* (26.0) | 40.0* (13.0) | 6.1 (3.0) | 5.9 (1.9) | 12.6 (3.8) | 10.8* (3.4) | 8.4* (3.1) | 12.7 (2.7) | 35:26 | 96.9 (14.2) |
| Subgroup 2 | 221 | 24.4 (13.8) | 6.7 (5.1) | 0.8 (1.4) | 2.0 (1.5) | 1.9 (2.3) | 2.1 (2.1) | 0.8 (1.2) | 11.2 (2.9) | 114:107 | 101.9 (15.2) |
| Subgroup 3 | 124 | 45.6 (16.2) | 22.8 (10.2) | 2.8 (2.1) | 3.1 (1.7) | 5.4 (3.6) | 4.9 (3.0) | 4.5 (2.5) | 12.3 (3.1) | 59:65 | 100.1 (15.6) |
| Subgroup 4 (Attn) | 82 | 93.5* (22.5) | 20.0 (9.4) | 2.2 (1.9) | 7.5* (1.9) | 7.4 (4.0) | 12.6* (2.7) | 5.5 (2.4) | 11.7 (3.1) | 57:25 | 93.3 (15.3) |
| Subgroup 5 | 130 | 53.3 (18.3) | 11.6 (7.7) | 7.5 (1.9) | 6.0 (1.9) | 14.0 (5.0) | 8.7 (2.8) | 2.6 (2.0) | 10.6 (2.9) | 90:40 | 99.5 (14.5) |
| Subgroup 6 | 141 | 30.6 (11.5) | 5.9 (5.0) | 1.1 (1.5) | 6.2 (1.6) | 3.9 (3.1) | 8.0 (2.6) | 0.9 (1.0) | 10.8 (2.9) | 99:42 | 98.7 (15.1) |
| Subgroup 7 (Emot) | 107 | 98.3* (20.7) | 24.7 (11.8) | 8.7* (2.3) | 8.4* (1.5) | 20.1* (5.0) | 13.3* (3.4) | 5.9 (3.0) | 10.7 (2.8) | 71:36 | 95.7 (15.4) |
| Subgroup 8 | 104 | 55.5 (17.9) | 14.3 (9.6) | 3.0 (2.0) | 8.6* (1.4) | 10.1 (4.6) | 12.9* (2.3) | 1.7 (1.5) | 10.1 (2.3) | 78:26 | 98.3 (15.0) |
| Subgroup 9 | 123 | 63.3 (16.9) | 14.0 (7.4) | 1.7 (1.7) | 5.9 (1.4) | 4.4 (2.9) | 6.9 (2.1) | 2.0 (1.6) | 10.6 (2.8) | 77:46 | 96.1 (15.6) |
*Values surpassing high clinical levels of each score.
Ranges for each score: SRS: 0 to 123+; SCARED-p: 0 to 82; ARI-p: 0 to 12; SDQ-Hyperactivity: 0 to 10; CBCL-AB: 0 to 40+; CBCL-AP: 0 to 22+; CBCL-WD: 0 to 17+. Age ranges: Subgroup 1 (AnxDep): 6.9 to 17.1; Subgroup 2: 6.0 to 17.7; Subgroup 3: 5.8 to 17.9; Subgroup 4 (Attn): 6.6 to 17.7; Subgroup 5: 5.8 to 17.6; Subgroup 6: 6.0 to 17.7; Subgroup 7 (Emot): 6.1 to 17.3; Subgroup 8: 6.2 to 16.4; Subgroup 9: 6.1 to 17.6.
Mean behavioral scores and demographic data for each subgroup, including our three high autistic traits subgroups of interest (highlighted). Behavioral scores with a clinically high threshold were bolded and denoted with a “*” superscript (s.d = Standard Deviation).
Fig. 1. Radar plot of high autistic traits subgroups.
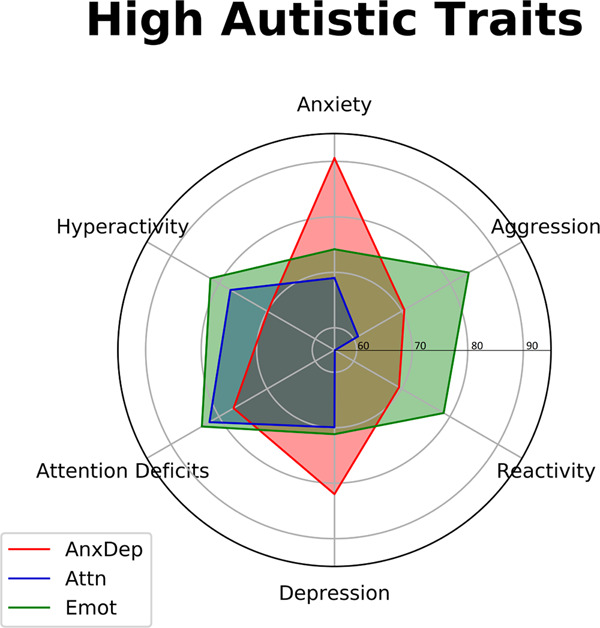
A clustering analysis yielded nine subgroups varying in behavioral composition. From these, three exhibited high SRS levels. The first subgroup (Emot), colored in green, had strong emotional dysregulation (aggression and reactivity) with ADHD-like symptoms. The second subgroup (Attn), colored in blue, showed ADHD-like tendencies. Lastly, the third subgroup (AnxDep), colored in red, exhibited high levels of anxiety and depression, as well as attention deficits. This plot was built upon normalized scores that were converted to a scale of 1 to 100 (as indicated by each encircling gray line) for simplification.
Upon comparing the three socially impaired subgroups to one another, several significant differences in behavioral scores were found (Table 2a, “Comparisons between subgroups”). We also compared each autistic traits subgroup to controls and observed significant differences in all behavioral scores, except for reactivity in the Attn subgroup. Lastly, we decided to combine all three high autistic traits subgroups into one “autistic-like” group (combined high SRS, hSRS) to compare against controls, which yielded highly significant differences in every behavioral score (Table 2a, “Comparisons to controls”).
Table 2.
Between-group behavioral score and demographic comparisons.
| SRS: Social Deficits | SCARED-p: Anxiety | ARI-p: Reactivity | SDQ-Hyperactivity | CBCL-AB: Aggression | CBCL-AP: Attention Problems | CBCL-WD: Depression | Age | Gender (X2) | FSIQ | |
|---|---|---|---|---|---|---|---|---|---|---|
| A. Behavioral data cohort (n=1093) | ||||||||||
| Comparisons between subgroups | ||||||||||
| Emot vs. Attn | 0.07 | 4.21 × 10−3* | 7.30 × 10−30* | 5.43 × 10−4* | 1.85 × 10−29* | 0.053 | 0.15 | 0.014* | 0.32 | 0.13 |
| Emot vs. AnxDep | 0.01* | 1.77 × 10−11* | 3.52 × 10−8 * | 4.58 × 10−14* | 3.80 × 10−17* | 2.03 × 10−5* | 1.43 × 10−6* | 6.80 × 10−6* | 0.76 | 0.25 |
| Attn vs. AnxDep | 0.16 | 2.72 × 10−16* | 4.72 × 10−14* | 1.41 × 10−6* | 8.13 × 10−12* | 1.70 × 10−3* | 5.92 × 10−9* | 0.02* | 0.19 | 0.056 |
| Comparisons to controls | ||||||||||
| Emot | 3.71 × 10−56* | 1.68 × 10−26* | 3.33 × 10−50* | 8.07 × 10−34* | 1.26 × 10−54* | 1.19 × 10−39* | 3.17 × 10−36* | 0.15 | 0.37 | 8.94 × 10−3* |
| Attn | 3.75 × 10−41* | 3.57 × 10−14* | 0.37 | 3.48 × 10−17* | 1.15 × 10−4* | 2.49 × 10−30* | 5.38 × 10−31* | 0.03* | 0.18 | 2.01 × 10−4* |
| AnxDep | 4.92 × 10−27* | 8.92 × 10−34* | 8.47 × 10−17* | 7.51 × 10−4* | 7.58 × 10−19* | 9.30 × 10−14* | 2.68 × 10−34* | 2.69 × 10−6* | 0.64 | 0.13 |
| hSRS (Emot + Attn + AnxDep) | 1.68 × 10−102* | 1.19 × 10−56* | 2.44 × 10−38 * | 5.40 × 10−40* | 1.91 × 10−53* | 2.15 x 10−67* | 4.18 x 10−81* | 7.14 x 10−3* | 0.3 | 7.06 x 10−5* |
| B. Neuroimaging cohort (n = 527; subset of behavioral data cohort) | ||||||||||
| Comparisons between subgroups | ||||||||||
| Emot vs. Attn | 0.09 | 0.49 | 1.81 × 10−14* | 4.01 × 10−3* | 5.95 × 10−15* | 0.35 | 0.24 | 4.49 × 10−3* | 0.76 | 0.21 |
| Emot vs. AnxDep | 0.02* | 3.27 × 10−7* | 2.28 × 10−5* | 2.96 × 10−7* | 1.08 × 10−10* | 4.61 × 10−2* | 3.93 × 10−4* | 4.36 × 10−4* | 0.99 | 0.29 |
| Attn vs. AnxDep | 0.12 | 1.88 × 10−7* | 2.38 × 10−7* | 4.14 × 10−3* | 8.12 × 10−8* | 0.08 | 5.83 × 10−4* | 0.06 | 0.66 | 0.11 |
| Comparisons to controls | ||||||||||
| Emot | 2.41 × 10−26* | 3.03 × 10−9* | 1.93 × 10−23* | 8.93 × 10−17* | 2.05 × 10−26* | 3.19 × 10−18* | 1.23 × 10−15* | 0.09 | 0.31 | 0.04* |
| Attn | 9.22 × 10−20* | 1.26 × 10−8* | 0.31 | 8.18 × 10−9* | 1.15 × 10−3* | 2.19 × 10−15* | 8.80 × 10−17* | 4.93 × 10−3* | 0.12 | 1.86 × 10−3* |
| AnxDep | 4.32 × 10−13* | 5.01 × 10−17* | 1.84 × 10−9* | 2.35 × 10−3* | 3.01 × 10−12* | 1.94 × 10−9* | 2.14 × 10−17* | 5.34 × 10−5* | 0.61 | 0.16 |
| hSRS (Emot + Attn + AnxDep) | 2.33 × 10−47* | 3.10 × 10−25* | 4.53 × 10−19* | 1.75 × 10−20* | 6.96 × 10−29* | 1.09 × 10−33* | 1.15 × 10−38* | 8.25 × 10−3* | 0.07 | 1.15 × 10−3* |
*Significant p-values.
Demographic and behavioral score comparisons, presented as p-values, between autistic traits subgroups, and between each autistic traits subgroup and controls. The top section shows these comparisons in the behavioral cohort (“A. Behavorial data cohort (n = 1093)”, with autistic traits subgroups (i.e. Emot, Attn, AnxDep) compared to each other (under “Comparisons between subgroups”), each autistic traits subgroup compared to controls, and finally a combination of all three autistic traits subgroups (hSRS) compared to controls (under “Comparisons to controls”). The bottom section (B. Neuroimaging cohort (n = 527; subset of behavioral data cohort)) presents the same comparisons in the neuroimaging cohort, which is composed of a subset of subjects from the behavioral cohort with usable structural MRI data. Significant p-values are bolded with a “*” superscript.
With respect to demographic information, there were no significant differences in gender and FSIQ between all subgroups. However, there were reported differences in age, though age ranges were similar (mean age = 10.8, SD = 3.4) (Table 2a, “Comparisons between subgroups”). Upon comparing each subgroup to controls, we again found no differences in gender. We did however find differences in age between all subgroups and controls, except for Emot. Although age differences were present, age ranges were again similar. FSIQ differed between all subgroups and controls, except for AnxDep, which is to be expected since autistic traits are generally accompanied by differences in FSIQ. Lastly, the comparison between the hSRS group and controls yielded significant differences in age and FSIQ, but not gender (Table 2a, “Comparisons to controls”). Due to these differences, we deemed it important to control for FSIQ, age and gender in the subsequent neuroimaging analysis.
Part 2: Neuroimaging analysis of cortical surface features
Morphological comparisons
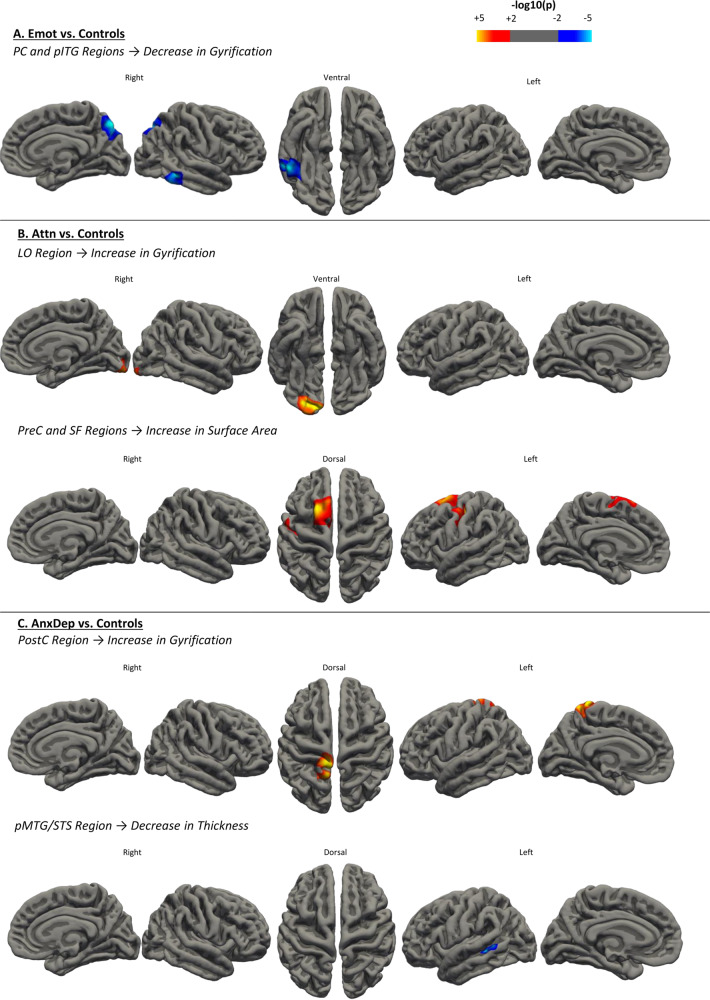
After removing subjects that have not undergone MRI acquisition and/or did not pass the T1 image quality check, as well as those removed during the outlier detection step (Supplementary Fig. 4), we obtained a sample of: n = 47 in the “Emot” group, n = 39 in the “Attn” group, n = 31 in the “AnxDep” group, and n = 410 controls (Supplementary Table 1), producing a total of 527 subjects with available T1 data participating in the study. Behavioral score and demographic information comparisons were nearly identical to the behavioral cohort (Table 2b, “Neuroimaging cohort’”). To delineate the interest and significance of subtyping in an autistic traits population, we first combined all three subgroups into one large group (hSRS, n = 117) and compared cortical thickness, local gyrification and surface area against controls. Indeed, this comparison did not yield significant differences in any of the measured surface features. We then compared the same surface features between each of our three subgroups against controls. After correction for multiple comparisons, the Emot subgroup exhibited decreases in gyrification in the right hemisphere in two separate clusters, one spanning the precuneus (including parts of the superiorparietal area) (p < 0.01, Cohen’s d = 0.51), and another in the temporal lobe (including the posterior inferior temporal gyrus and the middletemporal) (p < 0.01, Cohen’s d = 0.48)(denoted as PC and pITG) (Fig. 2a). The Attn subgroup displayed elevated local gyrification peaking in the lateraloccipital area of the right hemisphere (denoted as LO) (p < 0.01, Cohen’s d = 0.41). Additionally, the Attn subgroup also exhibited two separate clusters in the left hemisphere showing increases in surface area in the precentral cortex (along the central sulcus) (p < 0.01, Cohen’s d = 0.61), and superiorfrontal regions (p < 0.01, Cohen’s d = 0.58) (denoted as PreC and SF) (Fig. 2b). Lastly, the AnxDep subgroup showed increases in gyrification spanning the left postcentral and precuneus regions (PostC) (p < 0.01, Cohen’s d = 0.33), and decreases in thickness in the left posterior middletemporal gyrus lining the superior temporal sulcus (pMTG/STS) (p < 0.01; Cohen’s d = 0.55) (Fig. 2c) (Table 3).
Fig. 2. Surface feature comparisons between each subgroup and controls.
a The Emot subgroup yielded decreases in gyrification in the right precuneus and temporal regions (cwp = 0.0004 and 0.005, respectively). b The Attn subgroup exhibited increases in gyrification in the left lateraloccipital region (cwp = 0.002), and increases in surface area in the left precentral and superiorfrontal regions (cwp = 0.02 and 0.02, respectively). c The AnxDep subgroup showed increases in gyrification in the left postcentral area (cwp = 0.02), and decreases in thickness in the left middletemporal gyrus/superior temporal sulcus (cwp = 0.04). Colors represent the –log10(p-value), with red(+) indicating an increase and blue(−) indicating a decrease compared to controls in affected morphological features.
Table 3.
Neuroimaging cluster coordinates information.
| Subgroups | Feature | Hemisphere | Cluster name | All areas included in cluster | Peak region | Peak MNI coordinates | Size of region (mm²) | Cluster-wise p-value (cwp) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| X | Y | Z | ||||||||
| Emot | ↓ Gyrification | Right | PC (Precuneus) | Precuneus, Superiorparietal | Precuneus | 14 | −71.4 | 40.9 | 1860.87 | 0.0004 |
| ↓ Gyrification | Right | pITG (Posterior Inferior temporal) | Inferiortemporal, Middletemporal | Middletemporal | 59 | −42.4 | −10.4 | 1237.64 | 0.005 | |
| Attn | ↑ Gyrification | Right | LO (Lateraloccipital) | Lateraloccipital, Lingual | Lateraloccipital | 26.5 | −87.2 | −10.7 | 1395.61 | 0.002 |
| ↑ Surface Area | Left | PreC (Precentral) | Precentral, Central Sulcus | Precentral | −32 | −18.1 | 44.2 | 960.47 | 0.02 | |
| ↑ Surface Area | Left | SF (Superiorfrontal) | Superiorfrontal | Superiorfrontal | −18.1 | 10.5 | 60.8 | 985.47 | 0.02 | |
| Anxdep | ↑ Gyrification | Left | PostC (Postcentral) | Postcentral, Central Sulcus | Postcentral | −8.2 | −38.8 | 74.1 | 969.46 | 0.02 |
| ↓ Thickness | Left | pMTG/STS (posterior Middletemporal/Superior Temporal Sulcus) | Middletemporal, Superior Temporal Sulcus | Middletemporal | −49.1 | −39 | −5.6 | 399.23 | 0.04 | |
The type of morphological feature (↑ indicating an increase, and ↓ indicating a decrease), hemisphere, and affected brain regions are indicated above for each autistic traits subgroup. Additional information on MNI coordinate data, region size, peak region and cluster-wise p-value for each result within each autistic traits subgroup are also reported.
Discussion
ASD studies have unceasingly demonstrated heterogeneity, warranting a shift in focus towards initially characterizing these differences before subsequent analysis, and steering away from case-control studies. To this end, a dimensional approach proves most relevant. To the best of our knowledge, this is the first study using an unsupervised clustering analysis on a population-based cohort to investigate how autistic traits cluster with other behavioral dimensions into subgroups, with subsequent isolation of subgroup cortical signatures. Recent evidence advocates that autistic traits fall along a continuum within the general population, which was why this study was not limited to diagnosed individuals, but rather focused on autistic traits as absolute constructs in order to avoid potential selection or environmental biases often accompanying diagnosed patients. We obtained three autistic traits subgroups in our unsupervised clustering analysis with the following behavioral profiles: (1) high aggression, reactivity, and ADHD-like traits (Emot), (2) high in attention deficits and hyperactivity (Attn), and (3) high in anxiety and depression, as well as attention deficits (AnxDep). Furthermore, upon neuroanatomical investigation, we found that comparing each subgroup to controls uncovers unique cortical signatures. Namely, after correcting for multiple comparisons, the Emot subgroup showed decreased gyrification in precuneus and posterior inferior temporal regions (PC and pITG); the Attn subgroup displayed increases in gyrification in the lateraloccipital (LO) and increases in surface area in the precentral and superiorfrontal regions (SF); and lastly, the AnxDep subgroup exhibited an increase in gyrification in the postcentral cortex (PostC), as well as a decrease in thickness in the posterior middletemporal and superior temporal sulcus area (pMTG/STS). Most interestingly, we found that by comparing the structural brain features of one heterogeneous autistic traits group (composed by combing all three subgroups) to controls, we were unable to uncover any cortical signatures. Simply comparing behaviorally diverse ASD-like cases to controls proved far too rudimentary to yield consistent features.
Though several case-control studies have reported neuroanatomical differences in ASD populations, these studies have remained grossly inconsistent, possibly due to ASD heterogeneity. Here, we showed that by running a direct comparison between subjects having high versus low/absent autistic traits, no cortical differences were reported. In a study by Haar et al., authors compared cortical thickness differences between ASD and controls and ran both univariate and multivariate comparisons62. Results were strikingly weak and were attributed to the considerable heterogeneity of the ASD population. The authors ultimately suggested that previously reported neuroanatomical differences between cases and controls held low clinical significance, and advocated the necessity of subdividing ASD groups by genetic, clinical and/or behavioral traits in the identification of unique neuroanatomical abnormalities62. Further studies in animal research have also encouraged subtyping in ASD, namely a study by Ellegood et al., which ran a clustering analysis on ASD neuroanatomy in a cohort comprising several varieties of mouse models, and subsequently observed resulting clusters’ corresponding gene and behavior patterns63. The mentioned studies, along with several others, promote a shift towards subtyping ASD and autistic traits populations in order to better understand and treat the disorder.
Compared to our high vs. low/absent autistic traits contrast that yielded no results, by isolating behaviorally refined autistic traits subgroups we observed cortical signatures despite having lower statistical power than the combined sample. Decreased gyrification detected in the right PC and pITG region in the Emot subgroup is consistent with studies in ASD27,64. In general, the precuneus is highly implicated in the default mode network (DMN) as well as in visuospatial processing, empathy and memory, while the temporal lobe correlates to memory, audition, theory of mind and visual processes65–68. Considering that this group bears high in aggression, studies have also reported a general decrease in gyrification in aggressive patients69,70, as well as decreased functional connectivity between the precuneus and other brain regions in patients exhibiting higher aggression traits, possibly due to its role in the DMN and empathy71,72. Additionally, this subgroup exhibited high ADHD-like symptoms which have also shown links to precuneus regions of the brain73,74. In our second subgroup, Attn, we observed increases in surface area in the precentral (primary motor) cortex, which is involved in voluntary motor control75,76, and the superiorfrontal gyrus, which is part of the motor control network and also harbors functions in attention, working memory, executive functioning and in the default mode network74,77,78. A study has even suggested that early motor impairments are predictors of future social communication delays, further indicating the importance of understanding this region in relation to ASD risk79. Specifically, within ASD, atypical motor functioning has been measured in patients from infancy until well into adulthood80,81. Seeing as how we observed extensive structural alterations throughout the motor control network in the Attn subgroup, this warrants further investigation into the relationship between ADHD-like traits and motor control in ASD and autistic traits populations. The Attn subgroup also presented decreases in gyrification in the lateraloccipital region, which is heavily implicated in visual perception, and specifically in face recognition, which greatly influences social communication25,82,83. The last subgroup, AnxDep, exhibited increases in gyrification in the postcentral region (primary somatosensory cortex), which functions as the main sensory receptive area of the brain84,85. In ASD, atypical sensory reception, more specifically over-responsivity to tactile sensory inputs, is a very prevalent symptom86–88. This suggests that autistic individuals could easily be overwhelmed, perhaps forging a link to the development of anxious and depressive behaviors, as observed in this subgroup. The AnxDep subgroup additionally showed a decrease in thickness in the pMTG/STS region, which has been greatly implicated in language and social aspects, and thus an extremely important cortical region of interest in ASD behavioral studies89–91. Therefore, taking into account dimensional constructs of behavior in ASD can better prepare subgroups for the identification of biological mechanisms. Further investigation is warranted into the relationship between affected regions and corresponding subgroup behaviors in the context of ASD since these regions have been consistently reported within the ASD literature.
The behaviors observed in our subgroups enforce the fact that ASD is highly concurrent with several psychiatric conditions in up to 80–95% of patients35,39. Reported comorbid disorders include ADHD, depression disorders, anxiety disorders, obsessive compulsive disorder (OCD), and conduct disorders35–39. This high degree of comorbidity (based on diagnostic information) corresponds to our dimensional results, which describe these associations in an even more descriptive and spectral manner using behavioral constructs. Having access to a multidimensional cohort containing assessments of behaviors reported in ASD allowed us to explore how core autistic traits inherently distribute with other symptoms in a dimensionally continuous population. By running a data-driven clustering analysis on a population-based cohort, we isolated three main autistic traits subgroups. The AnxDep subgroup is composed of subjects high in anxiety, depression and attention deficits. This is in line with findings reported in the literature where anxiety and depression appear to be some of the most common psychiatric comorbidities in ASD patients38,39. The Attn subgroup could represent an isolated population consisting purely of ADHD and autistic traits in an otherwise behaviorally muted subclass. This may perhaps become the optimal subgroup for studying the overlap between ADHD and ASD. Lastly, the Emot subgroup has ADHD-like traits in combination with emotional regulation abnormalities as evidenced by high degrees of aggression and reactivity. The Emot subgroup suggests a third combination of behavioral traits showing that the aggressive behaviors often observed in autistic traits participants can in effect co-occur with ADHD-like traits. The diverse behavioral profile of each subgroup highlights the importance of combining independent behaviors into one multivariate analysis to observe how they distribute. For example, as mentioned previously, both the Attn and Emot subgroups show high levels of attention problems and hyperactivity, and remain relatively close in anxiety and depression levels. The Emot subgroup, however, exhibits exceptionally high levels of aggression and reactivity, a factor that separates one ADHD-like autistic traits subgroup into two (i.e. Attn and Emot), thus increasing behavioral homogeneity and the likelihood of extracting biological features from cortical images.
Notably, the unsupervised clustering analysis yielded high autistic traits subgroups with gender ratios (averaging 2:1, male to female) differing from those usually reported ASD populations (averaging 4:1, male to female)92. However, this gender disequilibrium is not entirely surprising as this difference can be explained by the fact that studies sampling from the general population often show a lower ratio (3:1)93, and that overall variability may play a role. Moreover, several studies have reported ratios ranging from 2:1 to 7:194–97, indicating a heterogeneity that warrants further exploration as well as a diversity in gender ratio that depends on how cohorts are built. Most importantly, within the current investigation gender differences were controlled for in the neuroimaging analysis.
This study has several potential limitations. Firstly, though the SRS included a repetitive behavior subscale, it would have been interesting to include an independent repetitive behavior component within the clustering analysis. Concerning the unsupervised clustering, inherent limitations include the somewhat arbitrary determination of the number of clusters, and difficulties to reproduce the same partitioning in another dataset. Also, it is challenging to account for covariates in unsupervised clustering analyses. Alternative approaches could also have been applied on this dataset that would prove interesting in future studies including clustering based on SRS subscales (with subsequent study of behavioral and morphological traits), or clustering on a broader range of scales (not only pertaining to behaviors central in ASD) with subsequent isolation of subgroups high in SRS. Additionally, the present study used a general population-based cohort, and not one tailored for ASD studies, thus warranting the careful isolation of behavioral variables relevant to our objective. Within the morphometric results, it is possible we did not observe further thickness differences due to the wide age range of our cohort. Thickness changes more with age and environment and may thus present larger heterogeneities than does gyrification (which is typically developed in-utero and shortly after birth), leading us to observe greater gyrification alterations within our results98,99. Also, the average age of subjects in the current study (~11.4 years old) could indicate that our cortical results are consequences of differential child development, a hypothesis however that can only be confirmed using a longitudinal, prospective design. Clinical diversity in autistic traits may be further explained by other modalities, thus next steps would involve considering genetic, volumetric, diffusion, and functional differences between the acquired subgroups.
In conclusion, we showed that subtypes of autistic traits yield refined signatures and therefore stress the importance of stratification using a dimensional approach. Several studies, including the current one, have demonstrated the difficulty in yielding significant biological features in case-control comparisons, leading to large-scale inconsistencies within ASD literature. Since several of the behavioral associations and affected cortical regions discussed in this study have similarly been implicated in ASD studies, our findings maintain the growing assumption that outcomes in autistic traits are related to variations observed in ASD patients. By uncovering better-defined subtypes of ASD, studies can finally begin to truly understand the underlying genetic, biological and behavioral mechanisms of this syndrome.
Supplementary information
Acknowledgements
The authors acknowledge the Healthy Brain Network (HBN) initiative at the Child Mind Institute in New York City, NY, USA. The HBN cohort provided us with the multidimensional data used in this study, namely MRI T1 images, clinical, psychiatric and behavioral assessments.
Author contributions
Experimental design and statistical analyses were conducted by A.M., V.F., J.H., C.Ph., and A.Gl. Neuroimaging data was processing by A.Gr. and A.M. Quality control of the structural neuroimaging data was done by A.M., V.F., and C.P. The manuscript was prepared by A.M., V.F., J.H., and C.Ph. All authors contributed to the interpretation of the results, as well as to the editing and approval of the manuscript content.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41398-020-00894-3).
References
- 1.Wing L. The autistic spectrum. Lancet. 1997;350:1761–1766. doi: 10.1016/S0140-6736(97)09218-0. [DOI] [PubMed] [Google Scholar]
- 2.Whitehouse AJO, Hickey M, Ronald A. Are autistic traits in the general population stable across development? PLoS ONE. 2011;6:e23029. doi: 10.1371/journal.pone.0023029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Constantino JN, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J. Autism Dev. Disord. 2003;33:427–433. doi: 10.1023/a:1025014929212. [DOI] [PubMed] [Google Scholar]
- 4.Robinson E, et al. The stability of autistic traits in the general population: further evidence for a continuum of impairment. J. Am. Acad. Child Adolesc. Psychiatry. 2011;50:376–384. doi: 10.1016/j.jaac.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Constantino JN, Todd RD. Autistic traits in the general population: a twin study. Arch. Gen. Psychiatry. 2003;60:524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- 6.White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin. Psychol. Rev. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wijnhoven LA, et al. Prevalence of comorbid depressive symptoms and suicidal ideation in children with autism spectrum disorder and elevated anxiety symptoms. J. Child Adolesc. Ment. Health. 2019;31:77–84. doi: 10.2989/17280583.2019.1608830. [DOI] [PubMed] [Google Scholar]
- 8.Kanne SM, Mazurek MO. Aggression in children and adolescents with ASD: prevalence and risk factors. J. Autism Dev. Disord. 2011;41:926–937. doi: 10.1007/s10803-010-1118-4. [DOI] [PubMed] [Google Scholar]
- 9.Dawson G, et al. Early social attention impairments in autism: social orienting, joint attention, and attention to distress. Dev. Psychol. 2004;40:271–283. doi: 10.1037/0012-1649.40.2.271. [DOI] [PubMed] [Google Scholar]
- 10.Murray MJ. Attention-deficit/hyperactivity disorder in the context of autism spectrum disorders. Curr. Psychiatry Rep. 2010;12:382–388. doi: 10.1007/s11920-010-0145-3. [DOI] [PubMed] [Google Scholar]
- 11.Mayes SD, Calhoun SL. Variables related to sleep problems in children with autism. Res. Autism Spectr. Disord. 2009;3:931–941. [Google Scholar]
- 12.Bolton PF, et al. Epilepsy in autism: features and correlates. Br. J. Psychiatry. 2011;198:289–294. doi: 10.1192/bjp.bp.109.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mostafa GA, Al-Ayadhi LY. The possible link between the elevated serum levels of neurokinin A and anti-ribosomal P protein antibodies in children with autism. J. Neuroinflammation. 2011;8:180. doi: 10.1186/1742-2094-8-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaidez V, Hansen RL, Hertz-Picciotto I. Gastrointestinal problems in children with autism, developmental delays or typical development. J. Autism Dev. Disord. 2014;44:1117–1127. doi: 10.1007/s10803-013-1973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Insel T, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 16.Ecker C, et al. Brain surface anatomy in adults with autism: the relationship between surface area, cortical thickness, and autistic symptoms. JAMA Psychiatry. 2013;70:59–70. doi: 10.1001/jamapsychiatry.2013.265. [DOI] [PubMed] [Google Scholar]
- 17.Libero LE, DeRamus TP, Deshpande HD, Kana RK. Surface-based morphometry of the cortical architecture of autism spectrum disorders: volume, thickness, area, and gyrification. Neuropsychologia. 2014;62:1–10. doi: 10.1016/j.neuropsychologia.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 18.Khundrakpam BS, Lewis JD, Kostopoulos P, Carbonell F, Evans AC. Cortical thickness abnormalities in autism spectrum disorders through late childhood, adolescence, and adulthood: a large-scale MRI study. Cereb. Cortex N. Y. N. 1991. 2017;27:1721–1731. doi: 10.1093/cercor/bhx038. [DOI] [PubMed] [Google Scholar]
- 19.Laidi C, et al. Decreased cortical thickness in the anterior cingulate cortex in adults with autism. J. Autism Dev. Disord. 2019;49:1402–1409. doi: 10.1007/s10803-018-3807-3. [DOI] [PubMed] [Google Scholar]
- 20.Wallace GL, Dankner N, Kenworthy L, Giedd JN, Martin A. Age-related temporal and parietal cortical thinning in autism spectrum disorders. Brain. 2010;133:3745–3754. doi: 10.1093/brain/awq279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace GL, et al. Increased gyrification, but comparable surface area in adolescents with autism spectrum disorders. Brain J. Neurol. 2013;136:1956–1967. doi: 10.1093/brain/awt106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallace GL, et al. Longitudinal cortical development during adolescence and young adulthood in autism spectrum disorder: increased cortical thinning but comparable surface area changes. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:464–469. doi: 10.1016/j.jaac.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hazlett HC, et al. Early brain development in infants at high risk for autism spectrum disorder. Nature. 2017;542:348–351. doi: 10.1038/nature21369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mak-Fan KM, Taylor MJ, Roberts W, Lerch JP. Measures of cortical grey matter structure and development in children with autism spectrum disorder. J. Autism Dev. Disord. 2012;42:419–427. doi: 10.1007/s10803-011-1261-6. [DOI] [PubMed] [Google Scholar]
- 25.Kohli, J. S. et al. Local cortical gyrification is increased in children with autism spectrum disorders, but decreases rapidly in adolescents. Cereb. Cortex N. Y. N 199110.1093/cercor/bhy111 (2018). [DOI] [PMC free article] [PubMed]
- 26.Ecker C, et al. Relationship between cortical gyrification, white matter connectivity, and autism spectrum disorder. Cereb. Cortex. 2016;26:3297–3309. doi: 10.1093/cercor/bhw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schaer, M. et al. Decreased frontal gyrification correlates with altered connectivity in children with autism. Front. Hum. Neurosci. 7, 750 (2013). [DOI] [PMC free article] [PubMed]
- 28.Blanken LME, et al. Cortical morphology in 6- to 10-year old children with autistic traits: a population-based neuroimaging study. Am. J. Psychiatry. 2015;172:479–486. doi: 10.1176/appi.ajp.2014.14040482. [DOI] [PubMed] [Google Scholar]
- 29.Courchesne E. Abnormal early brain development in autism. Mol. Psychiatry. 2002;7:S21–S23. doi: 10.1038/sj.mp.4001169. [DOI] [PubMed] [Google Scholar]
- 30.Courchesne E, Campbell K, Solso S. Brain growth across the life span in autism: age-specific changes in anatomical pathology. Brain Res. 2011;1380:138–145. doi: 10.1016/j.brainres.2010.09.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hazlett HC, et al. Early brain overgrowth in autism associated with an increase in cortical surface area before age 2 years. Arch. Gen. Psychiatry. 2011;68:467–476. doi: 10.1001/archgenpsychiatry.2011.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prigge MBD, et al. Social responsiveness scale (SRS) in relation to longitudinal cortical thickness changes in autism spectrum disorder. J. Autism Dev. Disord. 2018;48:3319–3329. doi: 10.1007/s10803-018-3566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kamio Y, et al. Quantitative autistic traits ascertained in a national survey of 22 529 Japanese schoolchildren. Acta Psychiatr. Scand. 2013;128:45–53. doi: 10.1111/acps.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alexander LM, et al. An open resource for transdiagnostic research in pediatric mental health and learning disorders. Sci. Data. 2017;4:170181. doi: 10.1038/sdata.2017.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joshi G, et al. The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: a large comparative study of a psychiatrically referred population. J. Autism Dev. Disord. 2010;40:1361–1370. doi: 10.1007/s10803-010-0996-9. [DOI] [PubMed] [Google Scholar]
- 36.Lai M-C, Lombardo MV, Baron-Cohen S. Autism. Lancet. 2014;383:896–910. doi: 10.1016/S0140-6736(13)61539-1. [DOI] [PubMed] [Google Scholar]
- 37.Leyfer OT, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J. Autism Dev. Disord. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- 38.Salazar F, et al. Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J. Autism Dev. Disord. 2015;45:2283–2294. doi: 10.1007/s10803-015-2361-5. [DOI] [PubMed] [Google Scholar]
- 39.Simonoff E, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 40.Bölte S, Poustka F, Constantino JN. Assessing autistic traits: cross-cultural validation of the social responsiveness scale (SRS) Autism Res. 2008;1:354–363. doi: 10.1002/aur.49. [DOI] [PubMed] [Google Scholar]
- 41.Page J, et al. Quantitative autistic trait measurements index background genetic risk for ASD in Hispanic families. Mol. Autism. 2016;7:39. doi: 10.1186/s13229-016-0100-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frazier TW, et al. Quantitative autism symptom patterns recapitulate differential mechanisms of genetic transmission in single and multiple incidence families. Mol. Autism. 2015;6:58. doi: 10.1186/s13229-015-0050-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blanken LME, et al. White matter microstructure in children with autistic traits. Psychiatry Res. Neuroimaging. 2017;263:127–134. doi: 10.1016/j.pscychresns.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 44.Tu P-C, et al. Structural and functional correlates of a quantitative autistic trait measured using the social responsive scale in neurotypical male adolescents. Autism Res. 2016;9:570–578. doi: 10.1002/aur.1535. [DOI] [PubMed] [Google Scholar]
- 45.Aldridge FJ, Gibbs VM, Schmidhofer K, Williams M. Investigating the clinical usefulness of the social responsiveness scale (SRS) in a tertiary level, autism spectrum disorder specific assessment clinic. J. Autism Dev. Disord. 2012;42:294–300. doi: 10.1007/s10803-011-1242-9. [DOI] [PubMed] [Google Scholar]
- 46.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the strengths and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br. J. Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 47.Birmaher B, et al. The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 48.Stringaris A, et al. The affective reactivity index: a concise irritability scale for clinical and research settings. J. Child Psychol. Psychiatry. 2012;53:1109–1117. doi: 10.1111/j.1469-7610.2012.02561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Achenbach TM, Edelbrock C, Howell CT. Empirically based assessment of the behavioral/emotional problems of 2- and 3- year-old children. J. Abnorm. Child Psychol. 1987;15:629–650. doi: 10.1007/BF00917246. [DOI] [PubMed] [Google Scholar]
- 50.Jain, A. K. & Dubes, R. C. Algorithms for Clustering Data (Prentice-Hall, Inc., 1988).
- 51.Schwarz G. Estimating the dimension of a model. Ann. Stat. 1978;6:461–464. [Google Scholar]
- 52.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage. 1999;9:179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- 53.Fischl B, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–355. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- 54.Schaer M, et al. A surface-based approach to quantify local cortical gyrification. IEEE Trans. Med. Imaging. 2008;27:161–170. doi: 10.1109/TMI.2007.903576. [DOI] [PubMed] [Google Scholar]
- 55.Rosen AFG, et al. Quantitative assessment of structural image quality. NeuroImage. 2018;169:407–418. doi: 10.1016/j.neuroimage.2017.12.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fortin J-P, et al. Harmonization of cortical thickness measurements across scanners and sites. NeuroImage. 2018;167:104–120. doi: 10.1016/j.neuroimage.2017.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coon H, et al. Genome-wide linkage using the social responsiveness scale in Utah autism pedigrees. Mol. Autism. 2010;1:8. doi: 10.1186/2040-2392-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pan, P.-Y., Tammimies, K. & Bölte, S. The association between somatic health, autism spectrum disorder, and autistic traits. Behav. Genet. 10.1007/s10519-019-09986-3 (2019). [DOI] [PMC free article] [PubMed]
- 59.Tehrani-Doost M, Shahrivar Z, Pakbaz B, Rezaie A, Ahmadi F. Normative data and psychometric properties of the child behavior checklist and teacher rating form in an iranian community sample. Iran. J. Pediatr. 2011;21:331–342. [PMC free article] [PubMed] [Google Scholar]
- 60.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: Dept. of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 61.Carballo JJ, Rodríguez-Blanco L, García-Nieto R, Baca-García E. Screening for the ADHD phenotype using the strengths and difficulties questionnaire in a clinical sample of newly referred children and adolescents. J. Atten. Disord. 2018;22:1032–1039. doi: 10.1177/1087054714561858. [DOI] [PubMed] [Google Scholar]
- 62.Haar S, Berman S, Behrmann M, Dinstein I. Anatomical abnormalities in autism? Cereb. Cortex N. Y. N. 1991. 2016;26:1440–1452. doi: 10.1093/cercor/bhu242. [DOI] [PubMed] [Google Scholar]
- 63.Ellegood J, et al. Clustering autism: using neuroanatomical differences in 26 mouse models to gain insight into the heterogeneity. Mol. Psychiatry. 2015;20:118–125. doi: 10.1038/mp.2014.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pereira AM, et al. Differences in cortical structure and functional MRI connectivity in high functioning autism. Front. Neurol. 2018;9:539. doi: 10.3389/fneur.2018.00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Utevsky AV, Smith DV, Huettel SA. Precuneus Is a functional core of the default-mode network. J. Neurosci. 2014;34:932–940. doi: 10.1523/JNEUROSCI.4227-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bruner E, Preuss TM, Chen X, Rilling JK. Evidence for expansion of the precuneus in human evolution. Brain Struct. Funct. 2017;222:1053–1060. doi: 10.1007/s00429-015-1172-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Margulies DS, et al. Precuneus shares intrinsic functional architecture in humans and monkeys. Proc. Natl. Acad. Sci. 2009;106:20069–20074. doi: 10.1073/pnas.0905314106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jackson RL, Bajada CJ, Rice GE, Cloutman LL, Lambon Ralph MA. An emergent functional parcellation of the temporal cortex. NeuroImage. 2018;170:385–399. doi: 10.1016/j.neuroimage.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 69.Wallace GL, et al. Cortical and subcortical abnormalities in youths with conduct disorder and elevated callous-unemotional traits. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53:456–65.e1. doi: 10.1016/j.jaac.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hyatt CJ, Haney-Caron E, Stevens MC. Cortical thickness and folding deficits in conduct-disordered adolescents. Biol. Psychiatry. 2012;72:207–214. doi: 10.1016/j.biopsych.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bzdok D, et al. Parsing the neural correlates of moral cognition: ALE meta-analysis on morality, theory of mind, and empathy. Brain Struct. Funct. 2012;217:783–796. doi: 10.1007/s00429-012-0380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhu W, Zhou X, Xia L-X. Brain structures and functional connectivity associated with individual differences in trait proactive aggression. Sci. Rep. 2019;9:7731. doi: 10.1038/s41598-019-44115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Di Martino A, et al. Relationship between cingulo-insular functional connectivity and autistic traits in neurotypical adults. Am. J. Psychiatry. 2009;166:891–899. doi: 10.1176/appi.ajp.2009.08121894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nagahama Y, et al. Transient neural activity in the medial superior frontal gyrus and precuneus time locked with attention shift between object features. NeuroImage. 1999;10:193–199. doi: 10.1006/nimg.1999.0451. [DOI] [PubMed] [Google Scholar]
- 75.Thach WT. Correlation of neural discharge with pattern and force of muscular activity, joint position, and direction of intended next movement in motor cortex and cerebellum. J. Neurophysiol. 1978;41:654–676. doi: 10.1152/jn.1978.41.3.654. [DOI] [PubMed] [Google Scholar]
- 76.Georgopoulos AP, Kalaska JF, Caminiti R, Massey JT. On the relations between the direction of two-dimensional arm movements and cell discharge in primate motor cortex. J. Neurosci. 1982;2:1527–1537. doi: 10.1523/JNEUROSCI.02-11-01527.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chouinard PA, Paus T. What have we learned from ‘perturbing’ the human cortical motor system with transcranial magnetic stimulation? Front. Hum. Neurosci. 2010;4:173. doi: 10.3389/fnhum.2010.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 79.Bhat AN, Galloway JC, Landa RJ. Relation between early motor delay and later communication delay in infants at risk for autism. Infant Behav. Dev. 2012;35:838–846. doi: 10.1016/j.infbeh.2012.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brian J, et al. Clinical assessment of autism in high-risk 18-month-olds. Autism Int. J. Res. Pract. 2008;12:433–456. doi: 10.1177/1362361308094500. [DOI] [PubMed] [Google Scholar]
- 81.Landa R, Garrett-Mayer E. Development in infants with autism spectrum disorders: a prospective study. J. Child Psychol. Psychiatry. 2006;47:629–638. doi: 10.1111/j.1469-7610.2006.01531.x. [DOI] [PubMed] [Google Scholar]
- 82.Pierce K, Müller RA, Ambrose J, Allen G, Courchesne E. Face processing occurs outside the fusiform ‘face area’ in autism: evidence from functional MRI. Brain J. Neurol. 2001;124:2059–2073. doi: 10.1093/brain/124.10.2059. [DOI] [PubMed] [Google Scholar]
- 83.Zhao Y, et al. Altered spontaneous neural activity in the occipital face area reflects behavioral deficits in developmental prosopagnosia. Neuropsychologia. 2016;89:344–355. doi: 10.1016/j.neuropsychologia.2016.05.027. [DOI] [PubMed] [Google Scholar]
- 84.Rausch M, Spengler F, Eysel UT. Proprioception acts as the main source of input in human S-I activation experiments: a functional MRI study. Neuroreport. 1998;9:2865–2868. doi: 10.1097/00001756-199808240-00034. [DOI] [PubMed] [Google Scholar]
- 85.Chudler EH, Anton F, Dubner R, Kenshalo DR. Responses of nociceptive SI neurons in monkeys and pain sensation in humans elicited by noxious thermal stimulation: effect of interstimulus interval. J. Neurophysiol. 1990;63:559–569. doi: 10.1152/jn.1990.63.3.559. [DOI] [PubMed] [Google Scholar]
- 86.Green SA, et al. Overreactive brain responses to sensory stimuli in youth with autism spectrum disorders. J. Am. Acad. Child Adolesc. Psychiatry. 2013;52:1158–1172. doi: 10.1016/j.jaac.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liss M, Saulnier C, Fein D, Kinsbourne M. Sensory and attention abnormalities in autistic spectrum disorders. Autism Int. J. Res. Pract. 2006;10:155–172. doi: 10.1177/1362361306062021. [DOI] [PubMed] [Google Scholar]
- 88.Cascio CJ, et al. Perceptual and neural response to affective tactile texture stimulation in adults with autism spectrum disorders. Autism Res. 2012;5:231–244. doi: 10.1002/aur.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Redcay E. The superior temporal sulcus performs a common function for social and speech perception: implications for the emergence of autism. Neurosci. Biobehav. Rev. 2008;32:123–142. doi: 10.1016/j.neubiorev.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 90.Iidaka T, Miyakoshi M, Harada T, Nakai T. White matter connectivity between superior temporal sulcus and amygdala is associated with autistic trait in healthy humans. Neurosci. Lett. 2012;510:154–158. doi: 10.1016/j.neulet.2012.01.029. [DOI] [PubMed] [Google Scholar]
- 91.Mensen VT, et al. Development of cortical thickness and surface area in autism spectrum disorder. NeuroImage Clin. 2016;13:215–222. doi: 10.1016/j.nicl.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fombonne E. Epidemiology of autistic disorder and other pervasive developmental disorders. J. Clin. Psychiatry. 2005;66:3–8. [PubMed] [Google Scholar]
- 93.Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? a systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry. 2017;56:466–474. doi: 10.1016/j.jaac.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 94.Idring S, et al. Changes in prevalence of autism spectrum disorders in 2001-2011: findings from the Stockholm youth cohort. J. Autism Dev. Disord. 2015;45:1766–1773. doi: 10.1007/s10803-014-2336-y. [DOI] [PubMed] [Google Scholar]
- 95.Frazier TW, Georgiades S, Bishop SL, Hardan AY. Behavioral and cognitive characteristics of females and males with autism in the simons simplex collection. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53:329–340.e3. doi: 10.1016/j.jaac.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ozonoff S, et al. A prospective study of the emergence of early behavioral signs of autism. J. Am. Acad. Child Adolesc. Psychiatry. 2010;49:256–266.e1–2. [PMC free article] [PubMed] [Google Scholar]
- 97.Nag HE, Nordgren A, Anderlid B-M, Nærland T. Reversed gender ratio of autism spectrum disorder in Smith-Magenis syndrome. Mol. Autism. 2018;9:1. doi: 10.1186/s13229-017-0184-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li G, Lin W, Gilmore JH, Shen D. Spatial patterns, longitudinal development, and hemispheric asymmetries of cortical thickness in infants from birth to 2 years of age. J. Neurosci. 2015;35:9150–9162. doi: 10.1523/JNEUROSCI.4107-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Li G, et al. Mapping longitudinal development of local cortical gyrification in infants from birth to 2 years of age. J. Neurosci. 2014;34:4228–4238. doi: 10.1523/JNEUROSCI.3976-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.