Abstract
The SARS-CoV-2 epidemic, which has spread to many countries around the world, has hit Europe particularly hard. From our point of view, in a rural emergency department (with an annual patient census of around 25,000) in northeastern Italy, it is necessary to preserve the hospital and prevent it from becoming an outbreak of infection. In our experience, we reevaluated the negative predictive value of lung ultrasound to rule out lung involvement. Since severe acute respiratory failure appears to be the leading cause of death for COVID-19 patients, it is essential to focus on this clinical feature. We currently believe that a patient suspected of COVID-19, if he has a normal ultrasound examination (a so-called "A-profile"), can be discharged home to continue isolation and be treated without being hospitalized.
Keywords: COVID-19, Lung ultrasound, Accuracy, Sensitivity, Rule out
The SARS-CoV2 outbreak spreads quickly through droplets and, therefore, through close contact between people. Isolation of the people is the primary strategy to avoid the spread of this infection. Unfortunately, small outbreaks are easy to develop in small communities such as long-term care facilities or hospitals. COVID-19 (the disease caused by SARS-CoV2) seems to be mainly related to lung involvement. Although other organs may be involved (the infection can cause diarrhea, myocarditis, and encephalitis as well), the cause of death for many patients appears to be a profound and severe respiratory failure [1]. Unfortunately, in many countries, the number of beds in intensive care units (ICUs), ventilators, doctors, and nurses trained in critical care medicine is not sufficient for the number of patients. If many people got infected and required ICU level of care concurrently, there might be a paucity of supplies. Early recognition of infected patients at an early stage of the disease and discharge of patients without COVID-19 pneumonia could avoid extensive ICU hospitalization [2].
In this epidemic, lung ultrasound seems to confirm the diagnostic performances highlighted for other lung pathologies. In particular - at least from the first reports - the sensitivity appears to be adequate, even if the ultrasound findings are not specific [[3], [4], [5]–5]. On the other hand, the high pre-test probability determined by the high number of infections makes the presumptive diagnosis not so tricky. However, even computed tomography is afflicted by the same limits: a sensitivity close to 100% but a significantly lower specificity (even less than 25%) [[6], [7]–8]. It is difficult to establish the diagnostic accuracy of an imaging technique if the presumed gold standard, i.e., the reverse-transcription polymerase chain reaction (RT-PCR) via nasopharyngeal swab, seems to have an accuracy of about 70% [9].
So, it seems that the main quality of lung ultrasound is to allow us an early diagnosis and, therefore, an initial treatment, right? Wrong. The terms of the matter must be reversed.
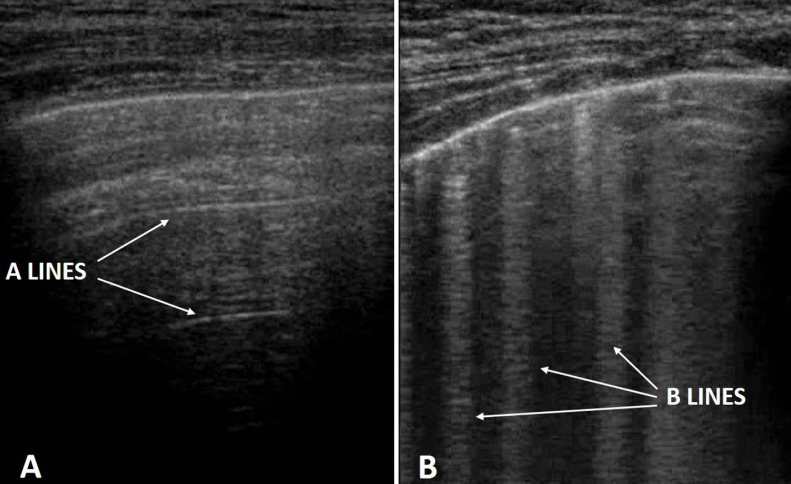
Italy has been particularly affected by the SARS-CoV-2 epidemic. Since we practice in a rural emergency department (with an annual patient census of around 25,000) in northeastern Italy, we have had the opportunity to evaluate several COVID-19 patients and people exposed to SARS-CoV2. What we have learned from this epidemic is the significant negative predictive value of lung ultrasound. Our preliminary data have taught us that through lung ultrasound, we can exclude lung involvement in high pre-test probability patients. We can establish that these are patients at low risk of developing respiratory failure within hours. Of course, this does not exempt us from checking their health, but it allows us a quick ruling out and rapid discharge. If these patients are SARS-CoV2 infected, their hospitalization would only increase the likelihood that the infection will spread to the hospital, without bringing any therapeutic benefit to the patients themselves. A normal image on the lung ultrasound examination, a so-called "A-profile" (i.e., the presence of A-lines and the absence of B-lines) (Fig. 1 ), precisely because of the high sensitivity, allows excluding lung involvement from COVID-19. From our preliminary data, no patient with a normal pattern on lung ultrasound had subsequent lung involvement from COVID-19. In fact, in about 100 cases of healthcare operators involved in the management of COVID-19 patients, only two were infected (one case of mild respiratory failure and one asymptomatic). Lung ultrasound (12-area anterior and posterior chest scan with convex or linear probe) was positive in three cases: one false positive and two true positives. None of the remaining cases with normal lung ultrasound showed a clinical or ultrasound deterioration at the follow-up of a month (weekly ultrasound check).
Fig 1.
Comparison between an "A-profile" (figure A), in which there are horizontal artifacts, called "A-lines", produced by the reverberation of the pleural line; and "B-profile" (figure B), in which the B-lines prevail, i.e., vertical hyperechoic artifacts, determined by complex reverberation phenomena if the density of the lung parenchyma increases.
If the larger case series confirm these data, we can say that the strength of the lung ultrasound lies precisely in its ability to rule out. When the peak of the infection decreases, but we will still be involved in the epidemic, the screening role of lung ultrasound - thanks to its ability to rule out - will become even more appreciable [10].
We are deeply convinced that this lesson should direct all future studies on the role of lung ultrasound in this global epidemic, rather than scrambling to look for highly specific signs and findings. First, there is A and then comes B.
Authors' contributions
RC and DO conceived the study; RC and GA collected the data; CCDG and DO wrote the first draft; RC and DO wrote the final draft; all authors approved the final draft.
Role of funding source
No funds have been used for this article.
Ethics committee approval
Not required.
Declaration of Competing Interest
Nothing to declare for all authors.
Footnotes
This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
References
- 1.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. Mar 13Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent JL, Slutsky AS. Coronavirus: just imagine. Crit Care. 2020;24(1):90. doi: 10.1186/s13054-020-2824-8. Mar 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound. 2008;6:16. doi: 10.1186/1476-7120-6-16. Apr 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buonsenso D, Pata D, Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30120-X. Mar 20pii: S2213-2600(20)30120-XEpub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith MJ, Hayward SA, Innes SM, Miller A. Point-of-care lung ultrasound in patients with COVID-19 - a narrative review. Anaesthesia. 2020 Apr 10 doi: 10.1111/anae.15082. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. Feb 26:200642Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.22954. Mar 4Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 8.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie F, Li S, Healey T, Atalay MK, Liao WH. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. Mar 10Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan JF, Yip CC, To KK, Tang TH, Wong SC, Leung KH, Fung AY, Ng AC, Zou Z, Tsoi HW, Choi GK, Tam AR, Cheng VC, Chan KH, Tsang OT, Yuen KY. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol. 2020 doi: 10.1128/JCM.00310-20. Mar 4pii: JCM.00310-20Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, Schluger NW, Volpi A, Yim JJ, Martin IBK, Anderson DJ, Kong C, Altes T, Bush A, Desai SR, Goldin J, Goo JM, Humbert M, Inoue Y, Kauczor HU, Luo F, Mazzone PJ, Prokop M, Remy-Jardin M, Richeldi L, Schaefer-Prokop CM, Tomiyama N, Wells AU, Leung AN. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Chest. 2020 doi: 10.1016/j.chest.2020.04.003. Apr 7. pii: S0012-3692(20)30673-5Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]