Abstract
Purpose
The aim of this study was to investigate and identify the main causes of periodontal tissue change associated with labial gingival recession by examining the anterior region of patients who underwent orthodontic treatment.
Methods
In total, 45 patients who had undergone orthodontic treatment from January 2010 to December 2015 were included. Before and after the orthodontic treatment, sectioned images from 3-dimensional digital model scanning and cone-beam computed tomography images in the same region were superimposed to measure periodontal parameters. The initial labial gingival thickness (IGT) and the initial labial alveolar bone thickness (IBT) were measured at 4 mm below the cementoenamel junction (CEJ), and the change of the labial gingival margin was defined as the change of the distance from the CEJ to the gingival margin. Additionally, the jaw, tooth position, tooth inclination, tooth rotation, and history of orthognathic surgery were investigated to determine the various factors that could have affected anterior periodontal tissue changes.
Results
The mean IGT and IBT were 0.77±0.29 mm and 0.77±0.32 mm, respectively. The mean gingival recession was 0.14±0.57 mm. Tooth inclination had a significant association with gingival recession, and as tooth inclination increased labially, gingival recession increased by approximately 0.2 mm per 1°.
Conclusions
In conclusion, the IGT, IBT, tooth position, tooth rotation, and history of orthognathic surgery did not affect labial gingival recession. However, tooth inclination showed a significant association with labial gingival recession of the anterior teeth after orthodontic treatment.
Keywords: Alveolar ridge, Bone, Gingiva, Gingival recession, Incisor, Orthodontic tooth movement
Graphical Abstract
INTRODUCTION
Gingival recession is defined as displacement of the marginal tissue apical to the cementoenamel junction (CEJ). The root exposure caused by gingival recession is not esthetically pleasing and may lead to tooth hypersensitivity and root caries [1]. A few studies have claimed that orthodontic treatment is among the causes of gingival recession, and some studies have reported deepening of the gingival recession after orthodontic treatment [2,3]. However, other studies found no evidence of the development of gingival recession due to the presence of a fixed orthodontic retainer, which maintains the condition of the area after orthodontic treatment [4,5]. Therefore, the role of orthodontic tooth movement in the development of gingival recession is still a debatable topic [6,7,8]. Several factors have been suggested to influence the occurrence of gingival recession following orthodontic treatment, including congenital gingival biotype, innate alveolar bone characteristics, total orthodontic tooth movement, and oral hygiene status [9,10].
According to the proposed concept of the “periodontal biotype,” the gingiva can be classified into thin and thick biotypes, especially on the labial side [11]. The thin biotype features a minimal amount of delicate soft tissue, with a gingival thickness of <1.5 mm, while the thick biotype features dense and fibrotic soft tissue with a large amount of attachment and a gingival thickness of ≥2mm [12,13]. Patients with the thin biotype have been considered to be more susceptible to gingival recession than those with the thick biotype [14,15,16]. Thus, a proper clinical assessment of the periodontal biotype is needed to avoid muco-gingival defects after orthodontic treatment, and to ensure accurate decision-making for planned anterior teeth inclination.
Alveolar bone deficiency around the teeth is an etiological factor associated with gingival recession [17]. Bony dehiscence and fenestration are often associated with a thin alveolar bone plate compared to a normal or thick bone plate. Thus, a thin alveolar bone plate can be susceptible to alveolar bone resorption and to subsequent gingival recession [18].
Orthodontic treatment is another possible etiological factor contributing to gingival recession. The labial or lingual movement of teeth during orthodontic treatment may cause thinning, dehiscence, and fenestration of the supporting alveolar bone plate. If the gingival margin is insufficiently supported by the alveolar bone, apical migration can occur, eventually leading to gingival recession [19]. An increased risk of gingival recession after orthodontic treatment was observed when the thickness of the free gingiva margin was less than 0.5 mm, and especially when the anterior teeth tilted forward [2].
Several methods have been proposed as ways to assess the periodontal biotype, but their accuracy remains controversial [20,21,22]. Recently, digital methods of scanning and assessment have been introduced to measure the periodontal biotype. These non-invasive and more accurate methods have been successfully applied to measure the volume of soft and hard tissues [23].
For diagnostic and evaluation purposes, cone-beam computed tomography (CBCT) and digital model scanning have been widely used in orthodontic treatment. These methods can be used to assess periodontal parameters such as thickness of the gingiva and alveolar bone, as well as changes of the position of the gingival margin.
However, few studies have investigated the correlations of the initial and final conditions of periodontal tissues and anterior teeth with the occurrence of gingival recession after orthodontic treatment. In particular, studies in Koreans are even more limited. Therefore, this study was designed to assess the effect of changes of the location of periodontal tissues and the anterior teeth on gingival recession in the anterior teeth after orthodontic treatment. In this study, we analyzed a broad range of factors that potentially affect gingival recession during orthodontic treatment.
MATERIALS AND METHODS
This study was reviewed and approved by the Institutional Review Board of the Ewha Medical Center (approval No. 2016-05-032-002).
Patient and site selection
This study included patients who had undergone orthodontic treatment with fixed appliances on the upper and lower incisors from January 2010 to December 2015 at the Department of Orthodontics of Ewha Medical Center. Patients in a physically healthy condition, with no gingival recession or restorations of the anterior teeth, and with available clinical records before and after orthodontic treatment were selected. The exclusion criteria were previous periodontal surgery or orthodontic treatment, dental trauma, drug-induced gingival enlargement, periodontitis of the anterior teeth, and missing teeth.
Initially, 137 records were collected, but only 57 patients possessed complete sets of pre- and post-treatment study models and CBCT images. Superimposing sectioned images of digital model scanning and CBCT was an essential component of this study. Therefore, after excluding patients with anterior alveolar bone segment fractures, which may cause alveolar bone remodeling and deformation due to trauma, and poor-quality anterior CBCT images, a final total of 45 patients were selected as the study subjects. The examinations were focused on the 8 maxillary and mandibular incisors, yielding a total of 360 incisors, of which 180 were central and 180 were lateral. One professional dentist objectively evaluated the data for all patients.
Site analysis
Digital model scanning
Pre- and post-treatment orthodontic study models were scanned using a TRIOS intraoral scanner (3Shape Dental Systems, Copenhagen, Denmark), and sectioned images for each incisor were made using the Ortho Analyzer software (3Shape Dental Systems). The sections were made along the long axes of teeth by a line connecting the mid-point of the incisor tip and the mid-point of the clinical CEJ.
CBCT images
A trained dentist obtained CBCT images before and after treatment using the Dinnova3 device (HDXWILL, Cheongju, Korea), at 90 KVp and 10 mA for 10 seconds. The sectioned images were generated using 3D imaging software (OnDemand 3D; Cybermed Co., Seoul, Korea). Sections were made along the axis of each tooth.
Superimposition of digital model scanning and CBCT images
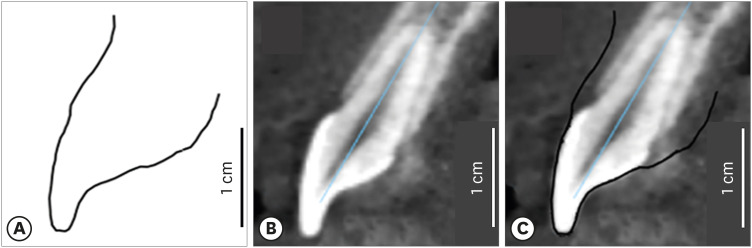
The sectioned images of digital model scanning and CBCT were superimposed in the same ratio using Adobe Photoshop 7.0 (Adobe Systems Inc., San Jose, CA, USA). A 1-cm line was drawn on each sectioned image of digital model scanning, and then calibrated to the same length of the CBCT image scale. The outline of a clinical crown was used as a reference to match both sectioned images (Figure 1).
Figure 1. Superimposition of cross-sectioned images of a digital scanned model and a cone-beam computed tomography (CBCT) image. (A) Cross-sectioned image of the digital scanned model, (B) cross-sectioned image of the CBCT image, (C) superimposition of (A) and (B).
Measurement of periodontal tissue parameters
The periodontal parameters presented below were measured on the superimposed image of the cross-sectioned images of digital model scanning and CBCT.
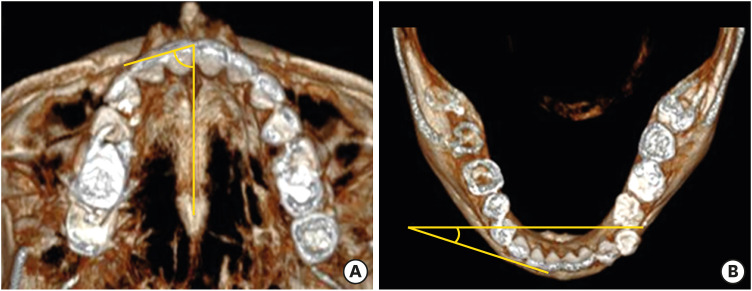
Pre-treatment gingival and alveolar bone thickness
Periodontal parameters such as the pre-treatment initial labial gingival thickness (IGT) and the initial labial alveolar bone thickness (IBT) were measured. Cook et al. [24] reported that the distance from the CEJ to the alveolar crest ranged from 2.5 to 3.5 mm (71.4%). In other words, the alveolar bone crest often does not exist up to 3.5 mm below the CEJ. Therefore, we measured gingival and alveolar bone thickness at 4 mm apical from the anatomical CEJ. In the orthodontic diagnostic model casts, the gingiva of all study subjects was confirmed to be keratinized at this depth. A perpendicular line to the long axis of the tooth (i.e., E-F) was drawn at 4 mm apical of the anatomical CEJ. The points where the E-F line met the outline of the digital model scanning, alveolar bone, and tooth were defined as points G, H, and I, respectively. The distance between G and H was considered to be the gingival thickness (GT), while the distance between H and I was considered to be the alveolar bone thickness (BT) (Figure 2).
Figure 2. Measurements of periodontal parameters on the superimposed image. A–B: perpendicular line from the most coronal position of marginal gingiva to the long axis of the tooth; C–D: perpendicular line from the cementoenamel junction to the long axis of the tooth; E–F: parallel line with the C–D line positioned 4 mm apically from the C–D line; G–H: gingival thickness; H–I: alveolar bone thickness.
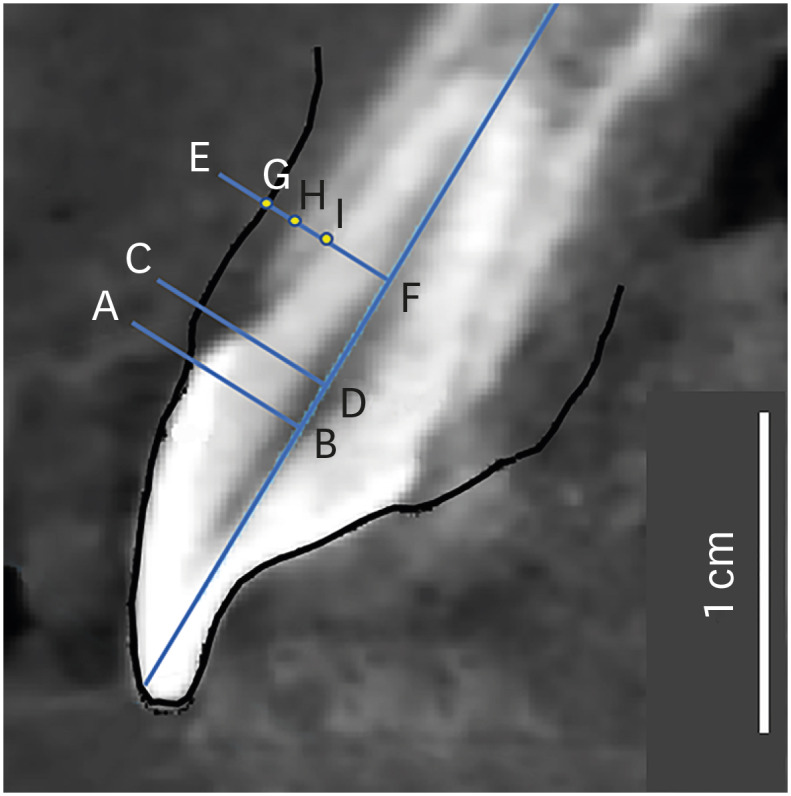
Changes of the gingival margin
The pre- and post-treatment position of the labial gingival margin were measured as the distance between the CEJ and the most coronal position of the gingival margin (i.e., A-C or B-D), and the change of the gingival margin was calculated by subtracting the post-treatment value from the pre-treatment value (Figure 2). A positive value indicated the occurrence of gingival recession, while a negative value showed coronal movement of the gingival margin.
Measurements of anterior teeth parameters
Orthognathic surgery history
For each tooth, it was assessed whether orthognathic surgery had been performed on the jaw on which the tooth was located. Only orthognathic procedures associated with movement of the anterior teeth were included, meaning that orthognathic surgery was limited to Le Fort I osteotomy or anterior segmental osteotomy (ASO) on the maxilla and genioplasty or ASO on the mandible.
Inclination of anterior teeth
Changes in the inclination (i.e., proclination [forward tilting] or retroclination [backward tilting]) of the incisors were assessed using 3D imaging software (OnDemand 3D). All the reference points were projected to the midsagittal plane of the skull. The reference points, lines, and planes used to determine tooth inclination were as follows: 1) the crista galli, basion, and anterior nasal spine for setting the midsagittal plane; 2) the menton and gonion for the mandibular plane; 3) the porion and orbitale for the Frankfurt horizontal (FH) plane; 4) the midbuccal cusp of the upper first molars, middle of the upper incisors, midbuccal cusp of the lower first molars, and middle of the lower incisors for the occlusal plane; and 5) the mid-point of the incisor tip and apex of the incisor tip for the long axis of the incisor [25,26].
For patients with no history of orthognathic surgery, the angle between the FH plane and the long axis of the upper incisors projected to the midsagittal plane were measured to assess the inclination of the upper incisors. The angle between the mandibular plane and the long axis of the lower incisors projected to the midsagittal plane were also measured to evaluate the inclination of the lower incisors.
For patients who had a history of orthognathic surgery, the angle between the occlusal plane and the long axis of the incisors was measured to investigate changes of the reference line after surgery. The inclination of the tooth was calculated by subtracting the post-orthodontic treatment angle from the pre-orthodontic treatment angle for patients who had undergone surgery, and vice versa for patients who had not undergone surgery. A negative value indicated retroclination, while a positive value indicated proclination.
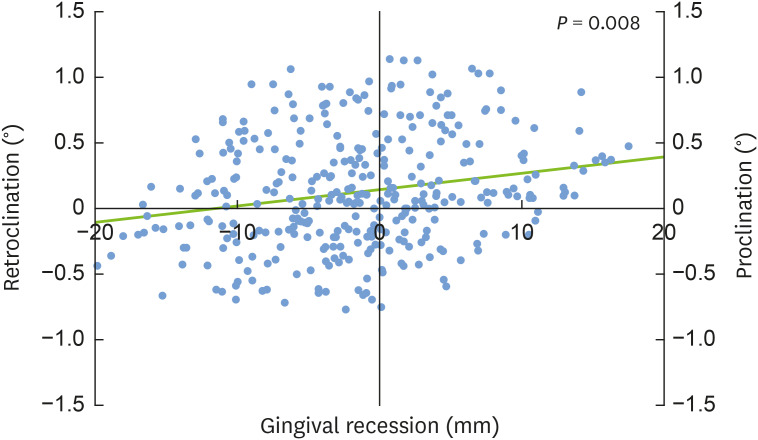
Rotation of the anterior teeth
On the occlusal plane, the rotation of incisors was determined using the reference lines of the mid-palatal suture for the maxilla and the line connecting both mental foramina for the mandible. The angle between the reference line and the tangent line to the incisal edge of each incisor was measured in degrees (Fig. 3). The absolute value of the difference between the pre- and the post-orthodontic treatment angle showed the amount of rotation.
Figure 3. Measurement of the degree of rotation using 3-dimensionally rendered images by calculating the angle between the extension of incisal tip line and the (A) mid-palatal suture or the (B) line connecting both mental foramina.
Factors affecting gingival margin change
The factors associated with gingival margin change were classified into 4 groups: patient-related factors (i.e., age and sex), tooth-related factors (i.e., jaw and position), periodontal factors (i.e., IGT and IBT), and orthodontic factors (i.e., orthognathic surgery history, inclination of the tooth, and rotation of the tooth). Correlations between gingival margin changes and these factors were also investigated.
Statistical analysis
Data were analyzed using SPSS version 20.0 for Mac (IBM Corp., Armonk, NY, USA).
To analyze individual teeth, each incisor in a patient was set as an individual unit.
A linear regression model was applied to assess the factors affecting gingival margin change (i.e., gingival recession). We applied the following key predictors to the linear regression model as confounding variables: age, sex, jaw, tooth position, history of orthognathic surgery, changes of the inclination and rotation of the tooth, and either IGT or IBT. The threshold for statistical significance was a P value less than 0.05.
RESULTS
Patients' characteristics at baseline
The demographic characteristics of the subject population at baseline are presented in Table 1. Forty-five subjects (10 males and 35 females) and 360 anterior teeth were selected. The mean age of the patients in this study was 21.58±8.82 years, with a range of 11 years to 53 years. The mean orthodontic treatment period was 2.11±1.34 years. Twenty-one patients (46.67%) had a history of orthognathic surgery on the maxilla, and 25 patients (55.56%) had a history of orthognathic surgery on the mandible. All the patients who underwent surgery on the maxilla also underwent surgery on the mandible. In total, 158 anterior teeth were forward-tilting (i.e., with a labial inclination), while 202 anterior teeth were backward-tilting (i.e., with a palatal or lingual inclination).
Table 1. Patients' characteristics at baseline.
| Parameters | Values | |
|---|---|---|
| Age (yr) | 21.58±8.82 | |
| Treatment period (yr) | 2.11±1.34 | |
| Sex | ||
| Male | 10 (22.2) | |
| Female | 35 (77.8) | |
| Jaw of the tooth | ||
| Maxilla | 180 (50.0) | |
| Mandible | 180 (50.0) | |
| Position of the tooth | ||
| Central incisor | 180 (50.0) | |
| Lateral incisor | 180 (50.0) | |
| Orthognathic surgery history | ||
| Maxilla | 21 (45.7) | |
| Mandible | 25 (54.3) | |
| Inclination of the tooth | ||
| Proclination | 158 (43.9) | |
| Retroclination | 202 (56.1) | |
Proclination means forward (i.e., labial) tilting, and retroclination means backward (i.e., palatal or lingual) tilting. Values are expressed as mean±standard deviation or number (%).
Periodontal tissue parameters
The IGT and IBT before orthodontic treatment were 0.77±0.29 mm and 0.77±0.32 mm, respectively. The mean distance from the CEJ to the gingival margin was 1.69±1.01 mm before orthodontic treatment and 1.55±1.01 mm after orthodontic treatment. The mean amount of gingival margin change (i.e., gingival recession) was 0.14±0.57 mm (Tables 2 and 3).
Table 2. IGT and IBT according to variables.
| Variables | IGT | IBT | |
|---|---|---|---|
| Overall | 0.77±0.29 | 0.77±0.32 | |
| Sex | |||
| Male | 0.75±0.29 | 0.82±0.31 | |
| Female | 0.77±0.30 | 0.76±0.32 | |
| Jaw of the tooth | |||
| Maxilla | 0.86±0.31 | 0.96±0.28 | |
| Mandible | 0.67±0.24 | 0.59±0.23 | |
| Position of the tooth | |||
| Central incisor | 0.75±0.28 | 0.81±0.33 | |
| Lateral incisor | 0.78±0.31 | 0.74±0.30 | |
| Orthognathic surgery history | |||
| Maxilla | 0.74±0.29 | 0.77±0.32 | |
| Mandible | 0.73±0.28 | 0.76±0.31 | |
| Inclination of the tooth | |||
| Proclination | 0.74±0.26 | 0.72±0.32 | |
| Retroclination | 0.78±0.31 | 0.81±0.31 | |
Proclination means forward (i.e., labial) tilting, and retroclination means backward (i.e., palatal or lingual) tilting. Data are distance (mm) values which expressed as mean±standard deviation except where indicated otherwise.
IGT: initial labial gingival thickness, IBT: initial labial alveolar bone thickness, SD: standard deviation.
Table 3. Changes of the gingival margin according to variables.
| Variables | Pre-orthodontic treatment gingival margin | Post-orthodontic treatment gingival margin | Gingival margin changes (gingival recession) | |
|---|---|---|---|---|
| Overall | 1.69±1.01 | 1.55±1.01 | 0.14±0.57 | |
| Sex | ||||
| Male | 1.72±0.96 | 1.53±0.95 | 0.19±0.50 | |
| Female | 1.69±1.02 | 1.56±1.03 | 0.13±0.58 | |
| Jaw of the tooth | ||||
| Maxilla | 2.01±1.07 | 1.88±0.99 | 0.14±0.60 | |
| Mandible | 1.37±0.83 | 1.22±0.93 | 0.15±0.53 | |
| Position of the tooth | ||||
| Central incisor | 1.61±0.96 | 1.51±0.95 | 0.10±0.58 | |
| Lateral incisor | 1.78±1.05 | 1.59±1.07 | 0.19±0.55 | |
| Orthognathic surgery history | ||||
| Maxilla | 1.69±0.97 | 1.52±1.01 | 0.17±0.56 | |
| Mandible | 1.60±0.96 | 1.44±1.01 | 0.17±0.55 | |
| Inclination of the tooth | ||||
| Proclination | 1.58±1.02 | 1.35±1.03 | 0.23±0.59 | |
| Retroclination | 1.78±0.99 | 1.71±0.96 | 0.08±0.54 | |
All values of gingival margin changes refer to the amount of gingival recession without a ‘-’ sign.
Proclination means forward (i.e., labial) tilting, and retroclination means backward (i.e., palatal or lingual) tilting. Data are distance (mm) values which expressed as mean±standard deviation except where indicated otherwise.
Factors affecting gingival margin change
Univariate and multivariate analyses were performed to evaluate which factors had a significant effect on the relationship of the final labial gingival thickness (FGT) and the final labial alveolar bone thickness (FBT) with gingival recession (Tables 4 and 5).
Table 4. Regression models demonstrating the relationship of FGT with gingival recession.
| Factors | Univariate model | Multivariate model | |||||
|---|---|---|---|---|---|---|---|
| Standardized coefficient β | 95% CI | P | Standardized coefficient β | 95% CI | P | ||
| Patient-related factors | |||||||
| Age | −0.062 | −0.011 to 0.003 | 0.244 | −0.073 | −0.011 to 0.002 | 0.161 | |
| Sex | 0.048 | −0.076 to 0.205 | 0.368 | −0.014 | −0.166 to 0.129 | 0.803 | |
| Tooth-related factors | |||||||
| Jaw of the tooth | −0.009 | −0.128 to 0.107 | 0.862 | 0.011 | −0.110 to 0.134 | 0.847 | |
| Position of the tooth | −0.086 | −0.214 to 0.020 | 0.104 | −0.085 | −0.211 to 0.019 | 0.100 | |
| Periodontal factors | |||||||
| IGT | −0.002 | −0.204 to 0.197 | 0.976 | 0.021 | −0.167 to 0.250 | 0.698 | |
| Orthodontic factors | |||||||
| Orthognathic surgery history | 0.051 | −0.059 to 0.175 | 0.331 | 0.044 | −0.070 to 0.169 | 0.419 | |
| Inclination of the tooth | 0.202 | 0.007 to 0.021 | <0.001a) | 0.232 | 0.005 to 0.027 | 0.004a) | |
| Rotation of the tooth | 0.080 | −0.002 to 0.012 | 0.131 | 0.101 | 0.000 to 0.014 | 0.056 | |
FGT: final labial gingival thickness, CI: confidence interval, IGT: initial labial gingival thickness.
a)Statistically significant difference (P<0.05).
Table 5. Regression models demonstrating the relationship of FBT with gingival recession.
| Factors | Univariate model | Multivariate model | |||||
|---|---|---|---|---|---|---|---|
| Standardized coefficient β | 95% CI | P | Standardized coefficient β | 95% CI | P | ||
| Patient-related factors | |||||||
| Age | −0.062 | −0.011 to 0.003 | 0.244 | −0.071 | −0.011 to 0.002 | 0.176 | |
| Sex | 0.048 | −0.076 to 0.205 | 0.368 | −0.011 | −0.164 to 0.134 | 0.839 | |
| Tooth-related factors | |||||||
| Jaw of the tooth | −0.009 | −0.128 to 0.107 | 0.862 | 0.026 | −0.115 to 0.173 | 0.692 | |
| Position of the tooth | −0.086 | −0.214 to 0.020 | 0.104 | −0.084 | −0.211 to 0.021 | 0.109 | |
| Periodontal factors | |||||||
| IBT | −0.033 | −0.245 to 0.127 | 0.536 | −0.016 | −0.265 to 0.208 | 0.815 | |
| Orthodontic factors | |||||||
| Orthognathic surgery history | 0.051 | −0.059 to 0.175 | 0.331 | 0.041 | −0.073 to 0.166 | 0.442 | |
| Inclination of the tooth | 0.202 | 0.007 to 0.021 | <0.001a) | 0.229 | 0.005 to 0.027 | 0.005a) | |
| Rotation of the tooth | 0.080 | −0.002 to 0.012 | 0.131 | 0.103 | 0.000 to 0.014 | 0.053 | |
FBT: final labial alveolar bone thickness, CI: confidence interval, IBT: initial labial alveolar bone thickness.
a)Statistically significant difference (P<0.05).
The univariate analysis of all variables showed that IGT (P=0.976) and IBT (P=0.536) were not significantly associated with gingival recession after orthodontic treatment. Multivariate analysis using the same variables as in the univariate analysis also showed that IGT (P=0.698) and IBT (P=0.815) were not significantly associated with gingival recession after orthodontic treatment, after adjusting for age, sex, the jaw and position of the tooth, history of orthognathic surgery, and the inclination and rotation of the tooth. No statistically significant differences were found for any variables except for the inclination of the tooth.
Only the inclination of the tooth had a significant association (FGT: P<0.001; FBT: P<0.001) with gingival recession in the univariate model. The multivariate model also showed significant results (FGT: P=0.004; FBT: P<0.001).
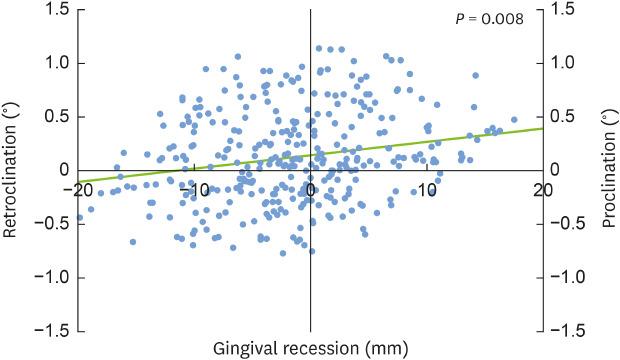
Gingival recession tends to develop in association with proclination of a tooth, rather than retroclination. As the inclination of a tooth increased labially, gingival recession increased by approximately 0.2 mm per 1° (Figure 4).
Figure 4. Scatter plot and trend line of gingival recession (mm) for proclination and retroclination.
DISCUSSION
Understanding the association between orthodontic treatment and gingival recession is important due to the growing demand for orthodontic treatment in children, teenagers, and adults [27]. In orthodontic movement, gingival thickness, proclination, treatment duration and type, and several biological events might influence alveolar bone remodeling around teeth and their periodontal tissues [28]. Bone resorption takes place in the direction of tooth movement, leading to reduction in the alveolar bone volume [13]. A previous study found an increased probability of alveolar bone dehiscence and gingival recession when the tooth root was displaced away from the center of the alveolar bone [2].
Accurately assessing periodontal tissue dimensions before orthodontic treatment is essential because it influences the esthetic outcome of the treatment. Several methods have been suggested for evaluating the gingival biotype (i.e., gingival thickness) [20]. Visual inspection and probe transparency are easily used in clinical practice, but controversial in terms of accuracy [21]. Transgingival probing utilizes a periodontal probe to penetrate and directly measure the gingiva thickness. However, this method is invasive and the results can have errors due to the angulation of the probe during the penetration [22]. Ultrasound devices, which have been proposed as an alternative, are noninvasive; however, it is difficult to determine the position for accurate measurements. Recently, CBCT images and digital model scanning have been applied to measure gingival thickness. These methods are non-invasive, and have been successfully applied to measure the volume of soft and hard tissues [23].
In this study, the assessments of IGT and IBT were restricted to the central and lateral incisors because these teeth are more prone to developing gingival recession. Cook et al. reported that the average distance from the CEJ to the alveolar bone crest was between 2.5 and 3.5 mm (71.4%), so we measured GT and BT at 4 mm apical from the CEJ as the reference point [24].
In relation to orthodontic treatment, the patient-related, site-related, and orthodontic factors may be considered as relevant variables in the analysis of teeth and periodontal tissues. The patient-related factors were age and sex, the site-related factors were tooth-related (jaw and position) and periodontal factors (IGT and IBT), and the orthodontic factors were a history of orthognathic surgery and inclination and rotation of the tooth. Albandar and Kingman reported that the prevalence of 1 mm or more of gingival recession in people aged 30 years and older was 58%, that gingival recession became more common with aging, and that men had more gingival recession than women [29]. Gorman also suggested that gingival recession increases with aging and that it is more severe in men than in women of the same age [30]. However, in contrast with previous studies, we were not able to find any significant differences in gingival recession by age or sex. This may be due to the characteristics of the patients, as most of study subjects were under 30 years old, and the proportion of male subjects was only 22%.
Mandibular incisors are known to have greater gingival recession and bone loss than maxillary incisors, especially in skeletal class III patients [31]. A history of orthognathic surgery was also suggested to cause more alveolar bone loss due to the soft tissue contraction associated with postoperative scar formation in comparison to patients with no history of orthognathic surgery [17]. However, in our study, gingival recession did not show any significant correlations with the jaw of the tooth, position of the tooth, or history of orthognathic surgery. Similarly, previous studies have reported that the gingival recession of incisors after orthodontic treatment, with or without orthognathic surgery, is of minor prevalence and severity [8,10].
Regarding periodontal factors, our results are similar to the findings of previous studies, according to which the initial gingival biotype did not have an influence on the development of gingival recession during orthodontic treatment. Boke et al. [32] also suggested that neither IBT nor gingival biotype is related to gingival recession. Djeu et al. [33] also reported similar results in patients treated with a fixed retainer, in which lower incisors were proclined by 5° after orthodontic treatment.
In orthodontic treatment, bodily movement of the tooth per se does not directly cause gingival recession [34]. Furthermore, the rotational movement of teeth progressed in the same pattern as the bodily movement in our study, and there was no significant association between gingival recession and rotational movement of the tooth.
Of particular note, we found that proclination of a tooth was more likely to cause gingival recession on the labial side than retroclination. In our analysis of all data related to changes in tooth inclination, the scatter plot showed a trend in which if the proclination of a tooth increased by 1°, gingival recession increased by approximately 0.2 mm. Similarly, some previous studies reported that proclined teeth were prone to have a higher occurrence or severity of gingival recession, and Ngan et al. demonstrated that retroclination of mandibular incisors with labial recession resulted in reduced severity of the recession [35]. In addition, Årtun and Krogstad [17] observed that excessive proclination of lower incisors during combined orthodontic and surgical treatment led to apical migration of the gingival margin for 3 years after the treatment.
Since this study was a retrospective study, confounding variables that might affect the gingival recession could not be thoroughly controlled. Furthermore, in this study, the 8 teeth from each patient were considered as separate entities. However, considering those teeth separately is problematic because they share the same patient-related characteristics. Moreover, not all relevant factors that might affect gingival recession were included in this study. Another limitation is that the subjects were drawn from the patient pool of a single medical center, which might have biased the results of the study to a certain extent. Therefore, in order to find a clear relationship between orthodontic tooth movement and gingival recession, more controlled prospective studies should be conducted on patients from various medical centers rather than from a single center. In addition, the study methodology should be improved in future related studies. One periodontist and one orthodontist performed the superimposition of the cross-sectional images of digital model scanning and CBCT for periodontal tissue assessment. In order to avoid errors as much as possible, we used a scale bar and the outline of hard tissue based on the calibration. A limitation of this study is that more accurate and verified measurement methods were not used.
In conclusion, the proclination of a tooth following orthodontic treatment and gingival recession showed a significant positive association. On the other hand, no association was found between IGT or IBT and gingival recession in the anterior teeth. An accurate evaluation of the risk of gingival recession is essential at the time of diagnosis and treatment planning for orthodontic patients. Orthodontists should pay close attention when deciding to procline the incisors, and collaboration with a periodontist is recommended for the pre- and post-orthodontic evaluation of periodontal tissues.
ACKNOWLEDGEMENTS
I certify that this study is academic research from my department and that all information related to this study has been fully acknowledged.
Footnotes
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant No. 2018R1D1A1B07041400) and Research Activation Project for the Interdisciplinary Creative Topic funded by the Ewha Womans University (grant No. 1-2018-000-001-1).
- Conceptualization: Jong-Bin Lee, Soo-Jin Baek, Min-Ji Kim, Eun-Kyoung Pang.
- Data curation: Soo-Jin Baek.
- Formal analysis: Jong-Bin Lee, Soo-Jin Baek, Min-Ji Kim.
- Funding acquisition: Jong-Bin Lee, Eun-Kyoung Pang.
- Investigation: Jong-Bin Lee, Soo-Jin Baek.
- Methodology: Soo-Jin Baek, Min-Ji Kim.
- Project administration: Eun-Kyoung Pang.
- Resources: Soo-Jin Baek, Min-Ji Kim, Eun-Kyoung Pang.
- Software: Jong-Bin Lee, Soo-Jin Baek.
- Supervision: Jong-Bin Lee, Min-Ji Kim, Eun-Kyoung Pang.
- Validation: Jong-Bin Lee, Min-Ji Kim, Eun-Kyoung Pang.
- Visualization: Jong-Bin Lee, Soo-Jin Baek, Min-Ji Kim.
- Writing - original draft: Jong-Bin Lee, Soo-Jin Baek.
- Writing - review & editing: Jong-Bin Lee, Eun-Kyoung Pang.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Rasperini G, Acunzo R, Cannalire P, Farronato G. Influence of periodontal biotype on root surface exposure during orthodontic treatment: a preliminary study. Int J Periodontics Restorative Dent. 2015;35:665–675. doi: 10.11607/prd.2239. [DOI] [PubMed] [Google Scholar]
- 2.Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop. 2006;130:6.e1–6.e8. doi: 10.1016/j.ajodo.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Renkema AM, Fudalej PS, Renkema A, Bronkhorst E, Katsaros C. Gingival recessions and the change of inclination of mandibular incisors during orthodontic treatment. Eur J Orthod. 2013;35:249–255. doi: 10.1093/ejo/cjs045. [DOI] [PubMed] [Google Scholar]
- 4.Allais D, Melsen B. Does labial movement of lower incisors influence the level of the gingival margin? A case-control study of adult orthodontic patients. Eur J Orthod. 2003;25:343–352. doi: 10.1093/ejo/25.4.343. [DOI] [PubMed] [Google Scholar]
- 5.Årtun J, Grobéty D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. Am J Orthod Dentofacial Orthop. 2001;119:2–10. doi: 10.1067/mod.2001.111403. [DOI] [PubMed] [Google Scholar]
- 6.Closs LQ, Grehs B, Raveli DB, Rösing CK. Occurrence, extension, and severity of gingival margin alterations after orthodontic treatment. World J Orthod. 2008;9:e1–6. [PubMed] [Google Scholar]
- 7.Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134:652–656. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- 8.Vasconcelos G, Kjellsen K, Preus H, Vandevska-Radunovic V, Hansen BF. Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatment. Angle Orthod. 2012;82:42–47. doi: 10.2319/021411-108.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127:552–561. doi: 10.1016/j.ajodo.2003.12.026. [DOI] [PubMed] [Google Scholar]
- 10.Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13:127–141. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 11.Seibert J, Lindhe J. Esthetics and periodontal therapy. In: Lindhe J, editor. Textbook of clinical periodontology. 2nd ed. Copenhangen, Denmark: Munksgaard; 1989. pp. 477–514. [Google Scholar]
- 12.Claffey N, Shanley D. Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol. 1986;13:654–657. doi: 10.1111/j.1600-051x.1986.tb00861.x. [DOI] [PubMed] [Google Scholar]
- 13.Zawawi KH, Al-Zahrani MS. Gingival biotype in relation to incisors' inclination and position. Saudi Med J. 2014;35:1378–1383. [PMC free article] [PubMed] [Google Scholar]
- 14.Scheyer ET, Sanz M, Dibart S, Greenwell H, John V, Kim DM, et al. Periodontal soft tissue non-root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86:S73–6. doi: 10.1902/jop.2015.140377. [DOI] [PubMed] [Google Scholar]
- 15.Kim DM, Neiva R. Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86:S56–72. doi: 10.1902/jop.2015.130684. [DOI] [PubMed] [Google Scholar]
- 16.Olsson M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisors. J Clin Periodontol. 1991;18:78–82. doi: 10.1111/j.1600-051x.1991.tb01124.x. [DOI] [PubMed] [Google Scholar]
- 17.Årtun J, Krogstad O. Periodontal status of mandibular incisors following excessive proclination. A study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofacial Orthop. 1987;91:225–232. doi: 10.1016/0889-5406(87)90450-1. [DOI] [PubMed] [Google Scholar]
- 18.Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134:220–225. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- 19.Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14:121–129. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 20.Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81:569–574. doi: 10.1902/jop.2009.090591. [DOI] [PubMed] [Google Scholar]
- 21.Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74:557–562. doi: 10.1902/jop.2003.74.4.557. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg J, Laster L, Listgarten MA. Transgingival probing as a potential estimator of alveolar bone level. J Periodontol. 1976;47:514–517. doi: 10.1902/jop.1976.47.9.514. [DOI] [PubMed] [Google Scholar]
- 23.Sanz Martin I, Benic GI, Hämmerle CH, Thoma DS. Prospective randomized controlled clinical study comparing two dental implant types: volumetric soft tissue changes at 1 year of loading. Clin Oral Implants Res. 2016;27:406–411. doi: 10.1111/clr.12579. [DOI] [PubMed] [Google Scholar]
- 24.Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent. 2011;31:345–354. [PubMed] [Google Scholar]
- 25.Downs WB. Variations in facial relationships; their significance in treatment and prognosis. Am J Orthod. 1948;34:812–840. doi: 10.1016/0002-9416(48)90015-3. [DOI] [PubMed] [Google Scholar]
- 26.Ricketts RM. Cephalometric analysis and synthesis. Angle Orthod. 1961;31:141–156. [Google Scholar]
- 27.Bollen AM, Cunha-Cruz J, Hujoel PP. Secular trends in preadult orthodontic care in the United States: 1942–2002. Am J Orthod Dentofacial Orthop. 2007;132:579–585. doi: 10.1016/j.ajodo.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 28.Henneman S, Von den Hoff JW, Maltha JC. Mechanobiology of tooth movement. Eur J Orthod. 2008;30:299–306. doi: 10.1093/ejo/cjn020. [DOI] [PubMed] [Google Scholar]
- 29.Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70:30–43. doi: 10.1902/jop.1999.70.1.30. [DOI] [PubMed] [Google Scholar]
- 30.Gorman WJ. Prevalence and etiology of gingival recession. J Periodontol. 1967;38:316–322. doi: 10.1902/jop.1967.38.4.316. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y, Park JU, Kook YA. Alveolar bone loss around incisors in surgical skeletal class III patients. Angle Orthod. 2009;79:676–682. doi: 10.2319/070308-341.1. [DOI] [PubMed] [Google Scholar]
- 32.Boke F, Gazioglu C, Akkaya S, Akkaya M. Relationship between orthodontic treatment and gingival health: a retrospective study. Eur J Dent. 2014;8:373–380. doi: 10.4103/1305-7456.137651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Djeu G, Hayes C, Zawaideh S. Correlation between mandibular central incisor proclination and gingival recession during fixed appliance therapy. Angle Orthod. 2002;72:238–245. doi: 10.1043/0003-3219(2002)072<0238:CBMCIP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Wennström JL. Mucogingival considerations in orthodontic treatment. Semin Orthod. 1996;2:46–54. doi: 10.1016/s1073-8746(96)80039-9. [DOI] [PubMed] [Google Scholar]
- 35.Ngan PW, Burch JG, Wei SH. Grafted and ungrafted labial gingival recession in pediatric orthodontic patients: effects of retraction and inflammation. Quintessence Int. 1991;22:103–111. [PubMed] [Google Scholar]