Abstract
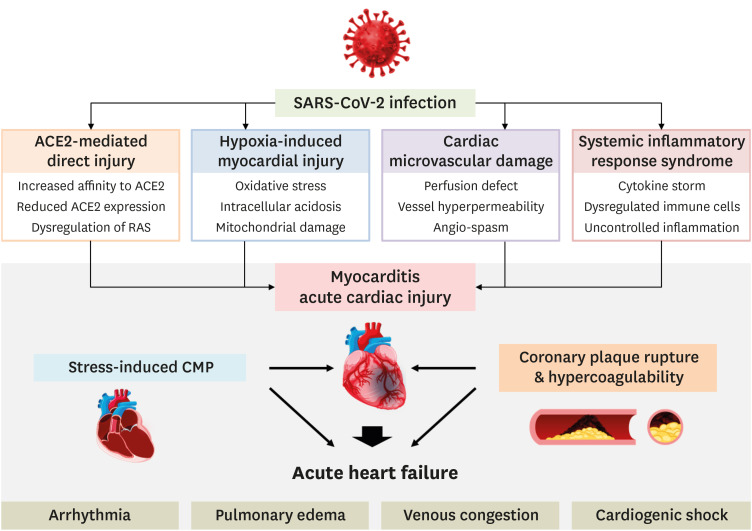
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread worldwide. Not just respiratory complications such as pneumonia and acute respiratory distress syndrome, cardiac manifestations have drawn attention due to the increased risk of mortality and morbidity related to SARS-CoV-2 infections. The mechanisms of the cardiac injury related to SARS-CoV-2 infections have been direct cardiac injury caused by angiotensin converting enzyme 2, hypoxemia, microvascular damage, and a systemic inflammatory response. Stress induced cardiomyopathy in a critically ill condition and acute coronary syndrome due to a vulnerable plaque rupture with coagulopathy can finally lead to acute heart failure with further cardiac manifestations. When dealing with the highly contagious viral disease-related cardiac manifestations, we should carefully apply the diagnostic and therapeutic methods to achieve the best therapeutic results without adding any risk of disease transmission.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, Heart, Cardiac manifestation, Cardiac injury
INTRODUCTION
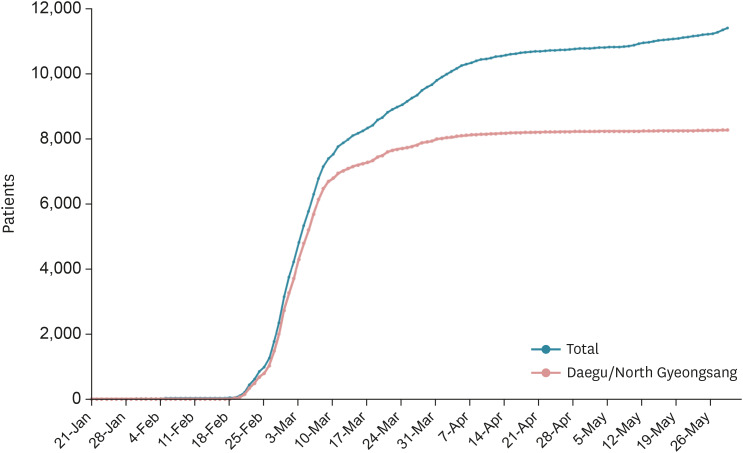
The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread worldwide.1),2),3) After the first case on December 31, 2019, from Wuhan, outbreaks become pandemic within three months with a tremendous socio-economic impact.4),5) In South Korea, the first SARS-CoV-2 infection was confirmed on January 19, 2020.6) After a one-month quiescent period, the outbreak started from a cult in Daegu on February 19, 2020. Most of the cases in South Korea occurred in Daegu and the North Gyeongsang province, which together account for about 10% of the total Korean population (5 million residents—2.4 million in Daegu and 2.6 million in North Gyeongsang province) (Figure 1).
Figure 1. The trend of COVID-19 confirmed patients in South Korea until May 31, 2020. The total numbers in Korea are depicted in the blue line and numbers in Daegu/North Gyeongsang province are depicted in the red line.
COVID-19 = coronavirus disease 2019.
The case fatality rate of COVID-19 worldwide has exceeded 7% with a higher mortality found in patients with an older age (age of >60 years) and history of cardiovascular, respiratory, and metabolic disorders.3),7) Not just respiratory complications such as pneumonia and acute respiratory distress syndrome (ARDS), but cardiac manifestations have drawn attention due to the increased risk of mortality and morbidity related to COVID-19.8),9),10),11)
Underlying cardiovascular disease (CVD) has been common in patients with previous coronavirus infection such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). It has been thought that angiotensin-converting enzyme 2 (ACE2), which is a functional receptor for coronavirus, is responsible for the increased incidence of cardiac involvement.12) In SARS, the prevalence of underlying CVD was 10% with a twelvefold increased risk of death.13),14) In MERS, CVD was present in approximately 30% of patients with also a higher mortality reported in these patients.9),15) The increased presence of cardiovascular comorbidities are also noted in COVID-19 as well, most notably among those with more severe disease.7),16),17) The prevalence of CVD in SARS-CoV-2 infections reported in the previous reports has ranges from 8–40% depending on the patient's characteristics and disease severity.7),12),18) Although the mechanism of the association between CVD and SARS-CoV-2 infection is not clearly identified, it is explained by the fact that the CVD is more prevalent in those with an advancing age, functionally impaired immune system, elevated levels of ACE2, or predisposition to COVID-19 in those with CVD.16)
CARDIAC INJURY IN COVID-19
Definitions of cardiac injury
Cardiac injury was defined by any abnormality observed in the cardiac biomarkers, electrocardiography, or echocardiography from the previous studies (Table 1).7),8),18),19),20) However, the definition in each study varies because there is no unified consensus of the definition in COVID-19 associated cardiac injury. Even though there was a high incidence and substantial impact of cardiac injury, it was not always possible to evaluate the whole set of cardiac injury markers (cardiac biomarkers, electrocardiography, and echocardiography) during the highly infectious virus pandemic. Most of the SARS-CoV-2 infected patients has a milder course with a complete recovery, which would not necessitate an evaluation. It is reasonable to perform those tests in patients with more serious disease course.21)
Table 1. The incidence and the prognosis of cardiac injury in COVID-19 from the previous reports using different definitions.
| Study | Total patients | Incidence | Definition of cardiac injury | Mortality |
|---|---|---|---|---|
| Huang et al.19) | 41 | 5 (12.0%) | Cardiac biomarker (hsTroponin-I) | 15.0% |
| ECG, Echo | ||||
| Wang et al.7) | 138 | 10 (7.2%) | Cardiac biomarker (Troponin-I) | 4.3% |
| ECG, Echo | ||||
| Yang et al.20) | 52 | 12 (23.0%) | Cardiac biomarker (hsTroponin-I>28 pg/mL) | 61.5% (75.0%*) |
| Zhou et al.18) | 191 | 33 (17.0%) | Cardiac biomarker (Troponin-I) | 28.3% (97.0%*) |
| ECG, Echo | ||||
| Guo et al.8) | 187 | 52 (27.8%) | Cardiac biomarker (Troponin-T) | 23.0% (59.6%*) |
COVID-19 = coronavirus disease 2019; ECG = electrocardiogram.
*Mortality of patients with any cardiac injury.
For the critical care patients, an evaluation of cardiac injury is readily feasible. Arentz et al.21) adopted a more specific definition of cardiac injury (more precisely, cardiomyopathy) in COVID-19 patients admitted to the intensive care unit (ICU). Cardiomyopathy was defined as evidence of a new-onset left ventricular systolic dysfunction on transthoracic echocardiogram when any one of following criteria is met: clinical signs of cardiogenic shock; an elevation in the creatinine kinase or troponin I level; a decrease in the central venous oxygen saturation (<70%).
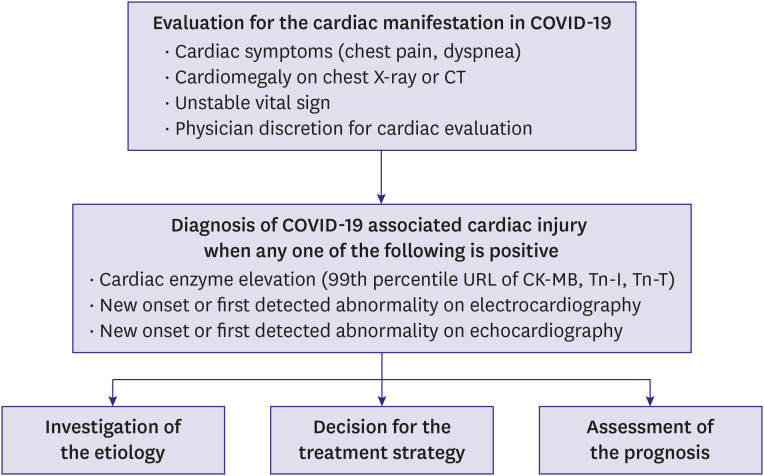
In general, tests for the cardiac manifestation in COVID-19 is performed when the patient has cardiac symptoms such as chest pain or dyspnea, cardiomegaly observed on the chest X-ray or on the chest computed tomography (CT), or when the physician considered the test is necessary in such cases of unstable vital sign. Cardiac injury associated with COVID-19 is diagnosed when any one of the parameters is positive: cardiac enzyme elevation; new-onset or first detected abnormality by electrocardiography; new-onset or first detected abnormality by echocardiography. After the diagnosis of COVID-19 associated cardiac injury, investigation of the etiology, the decision for the future treatment strategy, and assessment of the prognosis need to be proceeded (Figure 2).
Figure 2. Evaluation for the cardiac manifestation in COVID-19 and diagnostic algorithm of COVID-19 associated cardiac injury.
COVID-19 = coronavirus disease 2019; CT = computed tomography; URL = upper reference limit.
The incidence and mortality of cardiac injury in COVID-19
The incidence of cardiac injury associated with the SARS-CoV-2 infection is reported to be 7.2% in the overall patients, 2% in non-ICU patients, and 22% in ICU patients.7) In other reports, the incidence of cardiac injury reach up to 27.8–31% in accordance with the definitions and patient characteristics.8),19) The incidence of cardiomyopathy in ICU patients treated for COVID-19 was 33.3% and the mortality in the study population was 52.4%.21)
The mortality in COVID-19 has been caused mainly by respiratory failure due to severe acute pneumonia. However, a systemic inflammatory response syndrome, including a cytokine storm, and myocardial damage such as acute fulminant myocarditis with arrhythmic manifestations, can lead to sudden cardiac death.7),10),11),16) In this regard, the cardiac injury related to the SARS-CoV-2 infection is considered as an important issue. Patients with a previous history of coronary vascular disease and evidence of cardiac injury by elevated cardiac enzymes (Troponin-T levels) had a higher incidence of mortality.8)
Mechanism of cardiac injury and risk stratification
The cardiac injury related to the SARS-CoV-2 infection can be explained by several mechanisms (Figure 3). The first mechanism is ACE2-mediated direct cardiac damage. ACE2 has been identified as a functional receptor for coronaviruses. The SARS-CoV-2 infection is triggered by binding of the spike protein of the virus to ACE2, which is highly expressed in the heart and lungs. The second one is hypoxia-induced myocardial injury. Oxidative stress, intracellular acidosis, and mitochondrial damage followed by hypoxia might result in cardiac injury. Previously, significantly lower oxygen saturation levels and a higher incidence of dyspneic symptoms was noted in the cardiac injury patients. The third is the cardiac microvascular damage caused by vessel hyperpermeability and angio-spasms under conditions of inflammation. The fourth mechanism is systemic inflammatory response syndrome, such as the cytokine storm, caused by the inadequate responses of type 1 and type 2 helper T cells, which may contribute to the myocardial injury.12) Fulminant myocarditis can be related to the immunologic response during a viral infection.22),23),24) The fifth can be explained by epicardial coronary artery occlusions due to an acute plaque rupture owing to coagulopathy with plaque instability driven by a systemic inflammatory response. The last one is stress-induced cardiomyopathy because of the severe stress during the course of the SARS-CoV-2 infection.12),16),25),26),27) The cardiac injury related to COVID-19 cannot be explained separately by each mechanism. Multiple factors affect the cardiomyocytes, epicardial coronary arteries and coronary microvasculature in a various way at each timepoint of the disease trajectory.9),10),11),12),16),28),29) Evaluation of the major mechanism of cardiac injury in COVID-19 is important to set up further therapeutic strategies.
Figure 3. Mechanism of myocarditis and acute cardiac injury by SARS-CoV-2 leading to acute heart failure.
SARS-CoV-2 = severe acute respiratory syndrome-coronavirus 2; ACE = angiotensin converting enzyme; CMP = cardiomyopathy.
CARDIOVASCULAR MANIFESTATIONS OF COVID-19
Acute coronary syndrome
Although the true incidence is unclear, acute coronary syndrome (ACS) can occur in COVID-19 patients. The risk of ACS in SARS-CoV-2 infected patients may be increased due to an increased thrombotic tendency, evidenced by elevated D-dimer levels in the previous studies.7),18),19) In the inflammatory milieu, endothelial and smooth muscle cell activation, macrophage activation and tissue factor expression in atheromatous plaque, and platelet activation with further elaboration of inflammatory mediators can precipitate plaque rupture resulting in ACS.30) Not just a typical type 1 myocardial infarction (MI), but a type 2 MI related to the increased demand during the virus infection can develop especially in patients with underlying coronary artery disease.31) Frequently, the symptoms of an infection and the signs of non-ischemic cardiac injury can masquerade as ACS, and therefore a high index of suspicion for alternative diagnosis is mandatory by utilizing non-invasive diagnostic methods (cardiac biomarkers, electrocardiography, echocardiography, and cardiac CT).28),32) Given the risk of an infection spreading to other patients and to the healthcare providers during the transportation and procedure, adjusting the protocols for ACS treatment with increasing consideration for thrombolytics is considered in many centers during the virus pandemic.33),34),35),36)
Arrhythmias
Increased evidences has shown that COVID-19 is burdened by a higher risk of arrhythmic events, with a related risk on mortality.37) Palpitations have been reported as one of the most common initial symptoms of this disease (7.3%).37) In 138 hospitalized COVID-19 patients, arrhythmias represented the leading complication (19.6%) after acute respiratory distress syndrome, with an increased risk of up to 44.4% in those admitted to intensive care units. More serious arrhythmic complications such as ventricular tachycardia or ventricular fibrillation were found in 5.9% of cases.37),38) The risk of arrhythmias can be associated with cardiomyopathy caused by cardiac injury, or possibly related to the usage of anti-viral/anti-bacterial medications causing QT-prolongation.28),38) Physicians should keep in mind the risk of increased arrhythmic events in COVID-19 patients, which can significantly affect the overall mortality. Close monitoring for arrhythmic events and careful decision making for anti-viral/anti-bacterial medications is crucial especially in a serious disease status with a vulnerable status.
Myocarditis
There are several reports of SARS-CoV-2 with cardiac involvement as the presentation of acute myocarditis.10),22),24),39) The pathogenesis of cardiac involvement associated with SARS-CoV-2 may reflect a process of a replication and dissemination of the virus through the blood or lymphatic system from the respiratory tract. Tavazzi et al.39) reported the myocardial localization of SARS-CoV-2 with myofibrillar lysis and inflammatory cell infiltration during the acute phase of COVID-19. The general immunologic response in viral myocarditis is as follows: first, there is the viral entry and activation of the innate immune response, which takes 1–7 days after the infection; second, there is the activation of the acquired immune response by natural killer cells, macrophages, and T-lymphocytes which takes 1–4 weeks; and lastly, there is either recovery by the clearance of the virus or disease progression by the delayed and ineffective viral clearance with chronic inflammation, which takes months to years.40),41),42),43) The extent of the local tissue damage and cytokine storm triggered by the host immune response both contribute to the severity of the myocarditis. An exaggerated inflammatory response can be extremely fatal, and immunomodulators such as corticosteroids are considered in selected cases even though the efficacy and safety is questionable.28),44) Combined with these mechanisms related to a host immune response, multiple factors are responsible for the cardiac consequence of COVID-19, such as an oxygen supply and demand imbalance (with or without coronary artery disease), increased right ventricular afterload due to respiratory acidosis, hypoxemia and positive pressure ventilation.29),39) Even though it is difficult to discriminate all the possible mechanisms related to myocarditis, accordingly the effort to identify the dominant cause is necessary for the selection of the proper target treatment.
Heart failure
Patients with SARS-CoV-2 infection related cardiac injury including myocarditis could present with acute decompensated heart failure (HF) (Figure 2). They might have HF with a reduced or preserved ejection fraction.28)
Infection is one of the major precipitating factors of acute decompensation in HF, and patients admitted with acute HF precipitated by an infection had a high 90‐day risk of death.45),46) It is necessary to exert every effort to reduce the risk of SARS-CoV-2 infections in patients with HF—social distancing, hand washing, wearing personal protective equipment, and reducing unnecessary hospital visits.4) Maintaining an optimal guideline directed medical therapy including angiotensin converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB) is also highly recommended since there is no sufficient evidence to discontinue these critical medications for the concern of increased viral invasion due to the increased expression of ACE2.4),47) This issue will be discussed in detail later in a separated part.
Venous thromboembolisms
Thrombosis is a common consequence of an infection and is associated with a poor patient outcome. Many viral infections affect the pathways of hemostasis and coagulation, inducing either thrombotic or hemorrhagic complications.48) In patients with pneumonia caused by an influenza infection, the occurrence of venous thromboembolisms has been shown to be increased.49) Assessing the risk of venous thromboembolisms is essential especially in COVID-19 patients with a critical condition. Early reports from China showed a higher prothrombin time and D-dimer level on admission in ICU patients with COVID-19 as compared to non-ICU patients.19) A retrospective analysis of 183 COVID-19 patients also revealed a higher D-dimer and fibrin degradation product in non-survivals.50) Patients with COVID-19 in a critical condition would have complications such as renal failure, respiratory failure, or liver dysfunction, which can affect both venous thromboembolisms and the bleeding status.3),7) Among the patients with COVID-19 at high risk for venous thromboembolism, 44 (11%) of 407 also had a high risk of bleeding.51) Therefore, anticoagulation should be considered with a balance of the thrombotic risk and bleeding risk. When COVID-19 patients are indicated for anticoagulation therapy, the dose and duration of drug should be adjusted individually, and non-medical prophylactic measures need to be fully utilized such as mechanical compressions with elastic compression stockings or intermittent pneumatic compression.
DIAGNOSTIC CONSIDERATIONS FOR CARDIAC MANIFESTATIONS OF COVID-19
Although the cardiac manifestation of COVID-19 is an important issue, thorough examination of the cardiac injury using advanced diagnostic modalities is often limited owing to the risk of disease transmission during the diagnostic procedures and shortage of medical resources.16),52) Careful planning for the evaluation strategy of cardiovascular manifestations is mandatory in COVID-19 patients to protect both healthcare providers and non-infected patients and at the same time save the infected patients. There are several instructions needed to prevent infection spreading during the diagnostic procedures. Primary evaluation and management procedures, including laboratory tests, electrocardiography, and echocardiography, should be carried out in a negative pressure isolation room. When the patient needs further evaluation at a different location, the hospital administration and infection control departments need to arrange for the patient's transfer routes using a portable isolation bed to minimize the exposure to the facilities. For cardiac CT and magnetic resonance imaging, all rooms should be evacuated during the scan and for 4–5 hours after the sterilization according to the infection control strategy of each hospital.23)
THERAPEUTIC CONSIDERATIONS IN COVID-19 RELATED TO CARDIAC MANIFESTATIONS
The principle for the treatment of cardiac manifestations in COVID-19 is to deliver timely therapeutic modalities with a reduced the risk of disease spread. Cardiac manifestations are mostly urgent, but the prudent approach is crucial to avoid infection transmission to medical staff. If predicted outcomes are not different, selecting a less invasive therapeutic modality is highly recommended.28),35),37) Furthermore, proper utilization of telehealth including telephonic consultations, proxy prescriptions may be considered during the highly contagious virus outbreak.4),53)
Renin-angiotensin-aldosterone system inhibitors and COVID-19
There has been concern about using ACEi or ARB in COVID-19 patients owing to their role in altering the ACE2, which acts as a functional receptor of SARS-CoV-2.12),47) A high incidence of SARS-CoV-2 infections in patients with hypertension, heart failure, or cardiovascular disease who are common renin-angiotensin-aldosterone system (RAAS) blocker users increased the suspicion of their harmful effects.3),7),17),54) Inconsistent results of the previous animal models with respect to the effects of RAAS inhibitors on ACE2 also raised controversy.55),56),57),58),59) The beneficial effect of ACEi or ARB has been suggested by attenuating the local RAAS activation and unopposed angiotensin II accumulation caused by a continued viral infection and replication that contribute to reducing the membrane ACE2 expression.47) There is no concrete evidence or proven benefit to discontinue RAAS blockers and they are well established medications to improve outcomes in various diseases such as hypertension, myocardial infarction, chronic kidney disease, and heart failure. Furthermore, abrupt withdrawal of them in high-risk patients may result in clinical instability and adverse outcomes. Therefore, we need to maintain RAAS inhibitors in COVID-19 patients as previous guidelines recommend.
Heart transplantation
Heart transplant patients are at high risk of an infection and challenges exist regarding the maintenance of immunosuppression therapy after the infection, which can further raise the risk of graft rejection. A case study of two heart transplant patients from the Hubei province of China confirmed with the SARS-CoV-2 infection, revealed typical symptoms in these patients. One had a milder presentation, while the other required hospitalization with cessation of immunosuppression, along with treatment with methylprednisolone and intravenous immunoglobulin.60) When routine preventive measures were well adopted, the incidence of an infection in heart transplant patients can be minimized. A survey of 87 heart transplant recipients in Wuhan, China did not find a higher risk of infection with SARS-CoV-2.61) As of May 31st, there have been no confirmed heart transplant patients reported in South Korea. It is recommended to continue heart transplantations unless the risk of an infection spreading presents during the procedure. Surveillance of both the donor and recipient and related healthcare providers needs to be performed as per the individual organization's protocol and based on the up to date guideline recommendations.62),63) Even though the evidence is lacking, the current consensus for the management of heart transplant recipients who developed COVID-19 is to deliver the best supportive treatment for the viral infection and continuation of immunosuppression for mild disease. In more serious disease, reduction for anti-metabolites (mycophenolate or azathioprine) and further treatment with immunomodulators need to be considered.16)
TREATMENTS FOR SARS-CoV-2 AND FUTURE PERSPECTIVES
Since there is no proven therapy for SARS-CoV-2, the mainstay of the treatment in patients with COVID-19 remains supportive care including symptomatic treatment for minor symptoms and full intensive care support for serious complications. Contemporary candidate drugs are interleukin-6 inhibitors (tocilizumab, sarilumab), type 2 transmembrane serine protease inhibitor (camostat mesylate), membrane fusion and endocytosis inhibitors (chloroquine, hydroxychloroquine, arbidol), 3-chymotrypsin-like protease inhibitors (lopinavir, darunavir), and viral RNA-dependent RNA polymerase inhibitors (ribavirin, remdesivir, favipiravir).64) Among them, chloroquine, hydroxychloroquine, lopinavir/ritonavir, ribavirin are repurposed agents which were previously used to treat SARS and MERS.65),66) Recently, remdesivir showed efficacy for reducing hospitalization compared to the placebo in 1,063 COVID-19 patients from a randomized control trial.67) Compassionate use of remdesivir for 53 patients with severe COVID-19 also revealed 68% of clinical improvement.68) Adjunctive therapies of corticosteroids, anti-cytokine or immunomodulatory agents, and immunoglobulin therapy are also considered in selected cases but they should be applied with caution owing to the serious complications that can cause.64),69),70) More than 300 clinical trials are underway to investigate the effective medications and vaccines to overcome COVID-19, but the most important method at this point would be keeping basic preventive measures of wearing personal protective equipment, hand sanitizing, and social distancing.
CONCLUSIONS
Substantial evidence has suggested a non-negligible incidence of cardiac injury related to COVID-19. Although the clinical significance and exact mechanisms are under investigation, we should be aware of the potentially fatal cardiac manifestations when dealing with patients with COVID-19. Prudent selection of diagnostic and therapeutic methods during the outbreak is crucial to obtain the best therapeutic results without adding a risk of disease transmission.
Footnotes
Funding: This work was supported by the research promoting grant from the Keimyung University Dongsan Medical Center in 2018.
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Kim IC, Kim HA, Park JS, Nam CW.
- Data curation: Kim IC, Kim HA, Park JS.
- Formal analysis: Kim IC.
- Funding acquisition: Nam CW.
- Investigation: Kim IC, Park JS, Nam CW.
- Methodology: Kim IC, Park JS, Nam CW.
- Project administration: Nam CW.
- Resources: Kim IC, Nam CW.
- Supervision: Nam CW.
- Validation: Kim IC, Kim HA, Park JS.
- Visualization: Kim IC.
- Writing - original draft: Kim IC.
- Writing - review & editing: Kim IC, Nam CW.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) outbreak [Internet] Geneva: World Health Organization; c2020. [cited 2020 May 5]. Available from: https://covid19.who.int/ [Google Scholar]
- 2.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Cho DH, Yoo BS, Son JW, Kim IC, Park SM, Choi DJ. COVID-19 — Implications for patients with heart failure: The Korean Society of Heart Failure's clinical recommendations. Int J Heart Fail. 2020;2:111–114. doi: 10.36628/ijhf.2020.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomson B. The COVID-19 pandemic: a global natural experiment. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047538. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Kim JY, Choe PG, Oh Y, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020;35:e61. doi: 10.3346/jkms.2020.35.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1286. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 14.Chan JW, Ng CK, Chan YH, et al. Short term outcome and risk factors for adverse clinical outcomes in adults with severe acute respiratory syndrome (SARS) Thorax. 2003;58:686–689. doi: 10.1136/thorax.58.8.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 17.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa190. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Doremalen N, Bushmaker T, Munster VJ. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18:20590. doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- 24.Kim IC, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020;41:1859. doi: 10.1093/eurheartj/ehaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann Saudi Med. 2016;36:78–80. doi: 10.5144/0256-4947.2016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maisch B, Portig I, Ristic A, Hufnagel G, Pankuweit S. Definition of inflammatory cardiomyopathy (myocarditis): on the way to consensus. A status report. Herz. 2000;25:200–209. doi: 10.1007/s000590050007. [DOI] [PubMed] [Google Scholar]
- 27.Bonow RO, Fonarow GC, O'Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1105. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020;126:1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim IC, Han S. Epicardial adipose tissue: fuel for COVID-19-induced cardiac injury? Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa474. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation. 2001;103:1718–1720. doi: 10.1161/01.cir.103.13.1718. [DOI] [PubMed] [Google Scholar]
- 31.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018) Circulation. 2018;138:e618–51. doi: 10.1161/CIR.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 32.Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with Covid-19 - A case series. N Engl J Med. 2020 doi: 10.1056/NEJMc2009020. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05993-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Welt FGP, Shah PB, Aronow HD, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC's Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daniels MJ, Cohen MG, Bavry AA, Kumbhani DJ. Reperfusion of STEMI in the COVID-19 era - Business as usual? Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047122. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stefanini GG, Azzolini E, Condorelli G. Critical organizational issues for cardiologists in the COVID-19 outbreak: a frontline experience from Milan, Italy. Circulation. 2020;141:1597–1599. doi: 10.1161/CIRCULATIONAHA.120.047070. [DOI] [PubMed] [Google Scholar]
- 37.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lazzerini PE, Boutjdir M, Capecchi PL. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047293. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 39.Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sagar S, Liu PP, Cooper LT., Jr Myocarditis. Lancet. 2012;379:738–747. doi: 10.1016/S0140-6736(11)60648-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper LT., Jr Myocarditis. N Engl J Med. 2009;360:1526–1538. doi: 10.1056/NEJMra0800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis--diagnosis, treatment options, and current controversies. Nat Rev Cardiol. 2015;12:670–680. doi: 10.1038/nrcardio.2015.108. [DOI] [PubMed] [Google Scholar]
- 43.Fung G, Luo H, Qiu Y, Yang D, McManus B. Myocarditis. Circ Res. 2016;118:496–514. doi: 10.1161/CIRCRESAHA.115.306573. [DOI] [PubMed] [Google Scholar]
- 44.Yang Z, Liu J, Zhou Y, Zhao X, Zhao Q, Liu J. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020;81:e13–20. doi: 10.1016/j.jinf.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arrigo M, Gayat E, Parenica J, et al. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur J Heart Fail. 2017;19:201–208. doi: 10.1002/ejhf.682. [DOI] [PubMed] [Google Scholar]
- 46.Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF) Korean Circ J. 2017;47:341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vaduganathan M, Vardeny O, Michel T, McMurray JJ, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beristain-Covarrubias N, Perez-Toledo M, Thomas MR, Henderson IR, Watson SP, Cunningham AF. Understanding infection-induced thrombosis: lessons learned from animal models. Front Immunol. 2019;10:2569. doi: 10.3389/fimmu.2019.02569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Obi AT, Tignanelli CJ, Jacobs BN, et al. Empirical systemic anticoagulation is associated with decreased venous thromboembolism in critically ill influenza A H1N1 acute respiratory distress syndrome patients. J Vasc Surg Venous Lymphat Disord. 2019;7:317–324. doi: 10.1016/j.jvsv.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 50.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang T, Chen R, Liu C, et al. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol. 2020;7:e362–3. doi: 10.1016/S2352-3026(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gao C, Wang Y, Gu X, et al. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza A (H7N9) virus. Crit Care Med. 2020;48:451–458. doi: 10.1097/CCM.0000000000004207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 54.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 56.Burchill LJ, Velkoska E, Dean RG, Griggs K, Patel SK, Burrell LM. Combination renin-angiotensin system blockade and angiotensin-converting enzyme 2 in experimental myocardial infarction: implications for future therapeutic directions. Clin Sci (Lond) 2012;123:649–658. doi: 10.1042/CS20120162. [DOI] [PubMed] [Google Scholar]
- 57.Soler MJ, Ye M, Wysocki J, William J, Lloveras J, Batlle D. Localization of ACE2 in the renal vasculature: amplification by angiotensin II type 1 receptor blockade using telmisartan. Am J Physiol Renal Physiol. 2009;296:F398–405. doi: 10.1152/ajprenal.90488.2008. [DOI] [PubMed] [Google Scholar]
- 58.Sukumaran V, Veeraveedu PT, Gurusamy N, et al. Olmesartan attenuates the development of heart failure after experimental autoimmune myocarditis in rats through the modulation of ANG 1-7 mas receptor. Mol Cell Endocrinol. 2012;351:208–219. doi: 10.1016/j.mce.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 59.Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension. 2004;43:970–976. doi: 10.1161/01.HYP.0000124667.34652.1a. [DOI] [PubMed] [Google Scholar]
- 60.Li F, Cai J, Dong N. First cases of COVID-19 in heart transplantation from China. J Heart Lung Transplant. 2020;39:496–497. doi: 10.1016/j.healun.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ren ZL, Hu R, Wang ZW, et al. Epidemiologic and clinical characteristics of heart transplant recipients during the 2019 coronavirus outbreak in Wuhan, China: a descriptive survey report. J Heart Lung Transplant. 2020;39:412–417. doi: 10.1016/j.healun.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.DeFilippis EM, Farr MA, Givertz MM. Challenges in heart transplantation in the era of COVID-19. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047096. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim IC, Hwang I, Kim YS, Kim JB. Successful heart transplantation to a fulminant myocarditis patient during COVID-19 outbreak — Lessons learned. Korean Circ J. 2020;50:634–637. doi: 10.4070/kcj.2020.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323:1824–1836. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 65.Morra ME, Van Thanh L, Kamel MG, et al. Clinical outcomes of current medical approaches for Middle East respiratory syndrome: a systematic review and meta-analysis. Rev Med Virol. 2018;28:e1977. doi: 10.1002/rmv.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stockman LJ, Bellamy R, Garner P. SARS: systematic review of treatment effects. PLoS Med. 2006;3:e343. doi: 10.1371/journal.pmed.0030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19 — Preliminary report. N Engl J Med. 2020:NEJMoa2007764. doi: 10.1056/NEJMc2022236. [DOI] [PubMed] [Google Scholar]
- 68.Grein J, Ohmagari N, Shin D, et al. Compassionate Use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382:2327–2336. doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zha L, Li S, Pan L, et al. Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19) Med J Aust. 2020;212:416–420. doi: 10.5694/mja2.50577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li H, Chen C, Hu F, et al. Impact of corticosteroid therapy on outcomes of persons with SARS-CoV-2, SARS-CoV, or MERS-CoV infection: a systematic review and meta-analysis. Leukemia. 2020;34:1503–1511. doi: 10.1038/s41375-020-0848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]