Abstract
Court-involved youth exhibit high rates of psychiatric symptoms, substance use, and delinquency, yet little is known about the contributing roles of caregiver and family factors. The current study examined whether family functioning and parental monitoring mediate the relationship between caregiver and youth psychiatric symptoms (at first court contact) and youth substance use and delinquency (two years later). Participants were 400 first-time offending court-involved youth (Mage = 14.5 years; 57.3% male; 45.6% non-Latinx White, 42.0% Latinx) and an involved caregiver (Mage = 41.0 years; 87.2% female; 53.0% non-Latinx White, 33.8% Latinx). Structural equation modeling revealed that caregiver and youth psychiatric symptoms were prospectively associated with worse family functioning, which was in turn related to higher levels of youth delinquency and greater likelihood of substance use. The results support the notion of addressing the needs of justice-involved youth and families holistically rather than treating youth as “the problem” in isolation.
Keywords: Court-involved Youth, Delinquency, Family Functioning, Juvenile Justice, Psychiatric Symptoms, Substance Use
Introduction
Court-involved youth engage in substance use (Belenko et al. 2017; Teplin et al. 2002) and delinquent behaviors (Cottle et al. 2001) at alarmingly high rates. Since the vast majority of court-involved youth are not incarcerated (Hyland 2018) and often live in the community with family, it is critical to understand how family dynamics (e.g., family functioning, parenting practices) may mitigate or contribute to youth substance use and delinquency. Prior research with court-involved youth has examined the relationships between caregiver psychiatric symptoms, family functioning, and parental monitoring (Tolou-Shams et al. 2018), key factors which may contribute to youth substance use and delinquency. This work however was cross-sectional, used only caregiver report, included both first-time offending and repeat court-involved youth, and did not account for youth psychiatric symptoms or include youth substance use and delinquent behaviors as outcomes. The current study expands upon this prior work by utilizing a prospective design, focusing on first-time offending youth only, including both caregiver and youth perspectives, and including youth psychiatric symptoms, substance use, and delinquency in the model. Since youth who have any type of justice involvement are likely to have continued legal contact due to increased monitoring by the legal system following their initial contact, it is critical to understand ways to offset this trajectory as quickly as possible.
Psychiatric Symptoms as a Risk Factor for Youth Substance Use and Delinquency
Court-involved youth may be at particularly high risk for substance use and delinquent behavior because of clinically significant psychiatric symptoms, which are highly prevalent in these youth and their families. An estimated 70% of justice-involved youth have been diagnosed with psychiatric disorders (Skowyra and Cocozza 2007) and nearly one-third of caregivers of court-involved youth report psychiatric symptoms (Brown et al. 2018). The link between youth psychiatric symptoms and substance use (Abram et al. 2003; Teplin et al. 2002) and delinquent behavior (Carswell et al. 2004; Skowyra and Cocozza 2007; Vermeiren 2003) is well-documented, and often explained by theories such as the self-medication hypothesis (Khantzian 1997). It is also possible, however, that the relationship between youth and caregiver psychiatric symptoms and youth substance use and delinquency can be explained by family dynamics.
Family dynamics are complex and include family functioning (Epstein et al. 1983) and parenting practices (Sheidow et al. 2014). Family functioning involves the overall health of the family environment, including the structural and organizational properties of the family (e.g., management of daily roles and responsibilities) and interactions between family members (e.g., communication, emotional connection; Epstein et al. 1983; Rhee 2008). Parenting practices encompass discipline and monitoring efforts. Parental monitoring (i.e., a caregiver’s knowledge of and involvement in their child’s day-to-day activities and relationships) has been widely studied as a key practice related to youth substance use and delinquency.
Caregiver psychiatric symptoms are consistently related to poor family functioning (Daches et al. 2018; Tolou-Shams et al. 2018; Van Loon et al. 2014). According to both parent and youth report, poor family functioning, including lower rates of family expressiveness (Horwitz et al. 2007; Van Loon et al. 2014), cohesion (Fendrich et al. 1990; Pilowsky et al. 2006; Van Loon et al. 2014) and general family functioning (Daches et al. 2018), is often observed in families where a parent has a psychiatric disorder. Caregivers struggling with their own psychiatric symptoms may have limited capacity to promote positive family functioning through engaging their children on an emotional level (Goodyear et al. 2015). Furthermore, poor family functioning has been observed in families with adolescents with depression (Tamplin 1998), attention-deficit hyperactivity disorder (Schei et al. 2013), and internalizing symptoms (Simpson et al. 2018). Similar to caregivers with psychiatric problems, youth experiencing psychiatric symptoms may struggle to engage with their family in a healthy manner in areas such as parent-child communication, problem-solving, and affective involvement (Epstein et al. 1983).
In addition to contributing to poor family functioning, caregiver psychiatric symptoms are linked with less parental monitoring. Caregivers with higher levels of psychiatric symptoms tend to monitor their children less frequently than caregivers with fewer symptoms do (Borre and Kliewer 2014; Van Loon et al. 2014). This may be because caregivers’ symptoms impede their ability to effectively solicit information and/or track their children’s whereabouts, as well as connect with their children and instill necessary trust to promote voluntary disclosure of information.
Family Functioning and Parental Monitoring Influence Youth Substance Use and Delinquency
Research shows family functioning and parental monitoring influence youth engagement in substance use and delinquent behaviors. Of note, poor family functioning is associated with greater youth substance use among girls (Ohannessian et al. 2016; Shek 2002). Higher levels of parental monitoring are associated with less substance use among youth who are detained (Voisin et al. 2012), from low-income neighborhoods (DiClemente et al. 2001), are Hispanic/Latino (Wagner et al. 2010), or are racially and ethnically diverse and in middle school (Fosco et al. 2012) or high school (Parker and Benson 2004). Less parental monitoring also predicts earlier onset of alcohol use (Ryan et al. 2010), greater alcohol misuse (e.g., binge drinking, drunkenness) and increases in problem drinking over time (Barnes et al. 2006) among community samples of adolescents. Regarding delinquency, less parental monitoring (Barnes et al. 2006; Caldwell et al. 2006; DiClemente et al. 2001; Parker and Benson 2004) and poor family functioning (Gorman-Smith et al. 1998) are associated with more frequent delinquent behavior.
For parental monitoring, however, these effects are not universal. In a nationally representative sample of adolescents in the United States (Gault-Sherman 2012), parental monitoring was unrelated to delinquency. Although parental monitoring is protective against marijuana use at the bivariate level for urban high schoolers, there is no significant relationship once controlling for demographic factors (e.g., age, gender, ethnicity) in multivariate analyses (Borawski et al. 2003). There is also some evidence for gender differences in the relationship between parental monitoring and youth alcohol use. Of note, in multivariate analyses, parental monitoring is related to less alcohol use (Borawski et al. 2003; Griffin et al. 2000) for males, but not females. It is unclear whether the effects of parental monitoring and family functioning generalize to court-involved youth, as empirical investigations in this area are lacking.
To our knowledge, only one prior study has examined the relationships between caregiver psychiatric symptoms, family functioning, and parenting practices among court-involved youth in a single model (Tolou-Shams et al. 2018). Results of Tolou-Shams et al. (2018) indicated family functioning mediates the relationship between caregiver psychiatric symptoms and parental monitoring. Caregivers with higher levels of psychiatric symptoms tended to report worse family functioning, which in turn was related to less parental monitoring. It is likely that similar to caregiver psychiatric symptoms, poor family functioning (characterized by difficulty with communication and interaction patterns), inhibits youth’s spontaneous disclosure to their caregivers as well as caregivers’ ability to solicit information from their youth. The current study extends this research by using a prospective design, focusing on first-time offending court-involved youth only, using caregiver and youth report, and including youth psychiatric symptoms, substance use, and delinquency in the model.
Current Study
The current study examined the prospective relationships between caregiver and youth psychiatric symptoms at youth’s first court contact and youth’s substance use and delinquency two years later, as mediated by family functioning and parental monitoring. The conceptual model is shown in Fig. 1. It was hypothesized that family functioning and parental monitoring would sequentially mediate the relationships between caregiver and youth psychiatric symptoms and youth substance use and delinquency. Higher levels of youth and caregiver psychiatric symptoms (independent variables) were expected to result in poor family functioning (mediator), and in turn less parental monitoring (mediator) and more youth substance use and delinquency (dependent variables). In addition to a mediational effect by family functioning, caregiver psychiatric symptoms were also expected to directly relate to less parental monitoring. Further, in addition to a mediational effect by parental monitoring, poor family functioning was expected to relate to more youth substance use and delinquency.
Fig. 1.
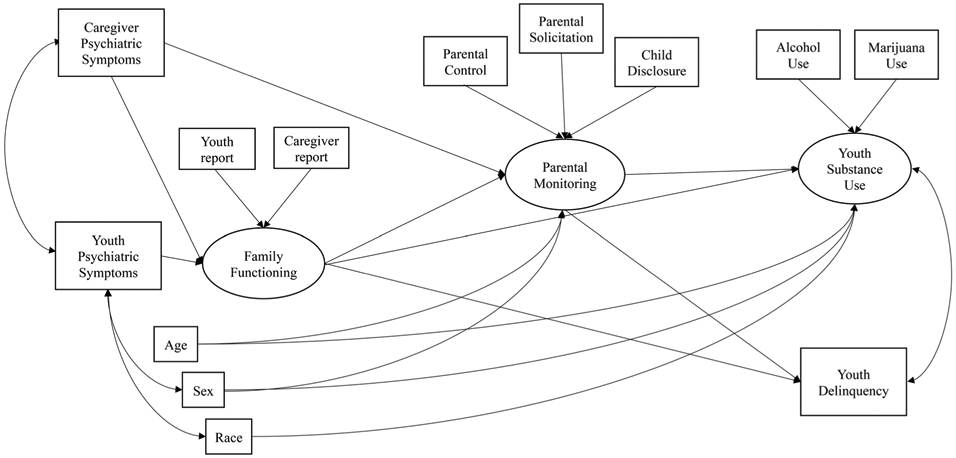
Conceptual model
Methods
Participants and Procedure
Participants were 400 first-time offending court-involved youth and an involved caregiver. Demographic characteristics of the youth and caregiver dyads are displayed in Table 1. Youth were on average 14.5 years old (SD = 1.5 years), predominately male (57.3%), and racially and ethnically diverse. Caregivers were on average 41.0 years old (SD = 7.2 years), predominately female (87.2%) and racially and ethnically diverse. According to caregivers, over 60% of families earned less than $30,000 annually, with an average of four people dependent upon this income; 65% reported receiving public assistance (e.g., food stamps, SNAP, WIC, SSI).
Table 1.
Demographic characteristics of court-involved youth and caregiver dyads recruited from a family court in the northeastern region of the United States
| Variable | Adolescents (n = 400) |
Caregivers (n = 400) |
|---|---|---|
| Mean age at baseline, in years (SD) | 14.5 (1.5) | 41.0 (7.2) |
| Female, n (%) | 170 (42.7) | 348 (87.2) |
| Latinx, n (%) | 168 (42.0) | 135 (33.8) |
| Race, n (%) | ||
| White | 182 (45.6) | 212 (53.0) |
| Black | 70 (17.5) | 48 (12.0) |
| Multi-racial | 68 (17.0) | 35 (8.8) |
| Other | 80 (20.0) | 105 (26.3) |
| Charge type, n (%) | ||
| Status offense | 194 (48.6) | – |
| Delinquent offense | 205 (51.4) | – |
| Employment, n (%) | ||
| Part-time | 30 (7.5) | 63 (15.8) |
| Full-time | 8 (2.0) | 144 (36.1) |
| Unemployed | 347 (87.0) | 192 (48.1) |
| Relationship to youth, n (%) | ||
| Birth parent | – | 371 (93.0) |
| Step-parent | – | 6 (1.5) |
| Adoptive parent | – | 10 (2.5) |
| Aunt/uncle | – | 3 (0.8) |
| Grandparent | – | 7 (1.8) |
| Other | – | 2 (0.6) |
| Marital status, n (%) | ||
| Single, never married | – | 152 (38.1) |
| Married | – | 104 (26.1) |
| Separated/divorced | – | 102 (25.5) |
| Living with partner | – | 25 (6.3) |
| Other | – | 15 (3.8) |
Enrolled youth had been in contact with the court for the first time within the past 30 days and were living in the community. To be eligible for study participation, youth had to have a first-time, open status (e.g., truancy, curfew, alcohol use) and/or delinquent petition (e.g., assault, breaking and entering) filed through a large family court in the northeastern region of the United States. Study exclusion criteria included being younger than 12 years or older than 18 years of age, having a prior offense at time of initial recruitment, cognitive impairment that would impede juvenile or caregiver ability to complete assessments, caregiver’s unwillingness to participate, and/or if the caregiver and youth had not lived in the same household for at least the prior six months. Court staff estimates and records indicated that approximately 50% of the 4,800 juveniles seen at the court setting during the enrollment time period were potentially eligible. The Principal Investigator’s university and collaborating sites’ Institutional Review Boards (and Office for Human Research Protections) approved all study procedures.
Participants received a study flyer with their court appointment date notification letter and research assistants then approached potentially eligible participants at the time of their first appointment to determine interest and eligibility for study participation. Interested youth and families were then screened in a private setting at the court and for those eligible, assent and consent was subsequently obtained from youth and caregivers off-site at the home, private community space, or research lab.
Youth and caregiver assessments (less than 2 h in duration) were conducted in private spaces using tablet-based, audio-assisted computerized assessment in English and Spanish (caregiver only). Audio-assisted computerized assessment has been shown to improve reliability of self-report (Romer et al. 1997), is easy to administer and is time and cost-effective. Follow-up assessments were conducted every four months post-baseline for two years. The current report uses data from the baseline, 8-month, 16-month, and 24-month follow-up assessments (see Fig. 2 for retention); data from the 4-, 12-, and 20-month assessments were not used because not all constructs of interest were measured at these time-points.
Fig. 2.
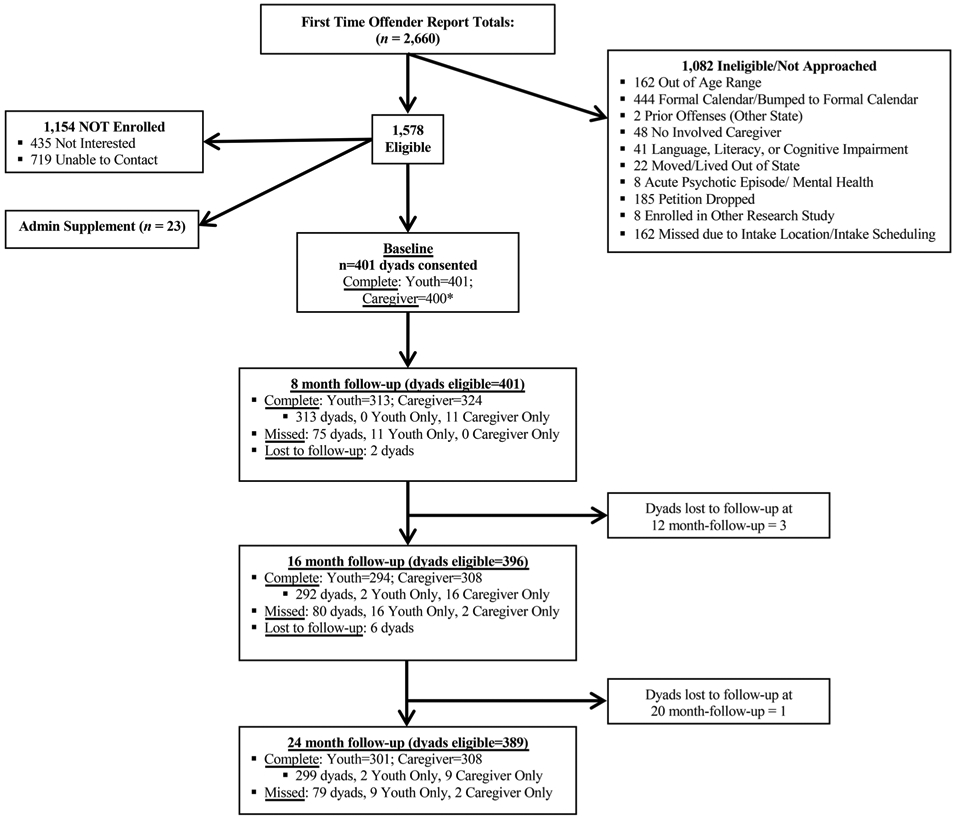
Participant retention flowchart. Note. dyad = youth and caregiver completed or missed assessment; youth only = youth completed or missed assessment but caregiver did not; caregiver only = caregiver completed or missed assessment but youth did not. Asterisk indicates baseline assessment was not completed for one caregiver, so this dyad is not part of the longitudinal sample for the current study
Measures
Demographic characteristics (baseline)
Standard demographic characteristics of youth and caregivers were assessed at baseline, including age, sex, race, and ethnicity.
Caregiver psychiatric symptoms (baseline)
Caregivers completed the 51-item Global Severity Index derived from the Brief Symptom Inventory (Derogatis and Melisaratos 1983). Two items related to harming oneself or others were removed from the assessment (because these assessments were conducted in the community where immediately accessible clinical resources were not available), which is typically 53 items. The Global Severity Index captures psychiatric symptoms across nine dimensions: Somatization (7 items; α = 0.96; e.g., Nausea or upset stomach), Obsessive-compulsive (6 items; α = 0.97; e.g., Having to check and double check what you do), Interpersonal sensitivity (4 items; α = 0.96; e.g., Your feelings being easily hurt.), Depression (5 items; α = 0.97; e.g., Feeling blue), Anxiety (6 items; α = 0.96; e.g., Suddenly scared for no reason), Hostility (5 items; α = 0.96; e.g., Having urges to break or smash things), Phobic anxiety (5 items; α = 0.97; e.g., Feeling afraid in open spaces or on the streets), Paranoid ideation (5 items; α = 0.94; e.g., Feeling that you are watched or talked about by others), Psychoticism (5 items; α = 0.95; e.g., The idea that someone else can control your thoughts), and 3 additional items not included in a specific subscale (i.e., Poor appetite; Trouble falling asleep; Feelings of guilt). Caregivers rated the severity of their psychiatric symptoms in the past week on a Likert scale where 1 = not at all and 5 = extremely. Responses are averaged and higher scores represent greater overall psychiatric symptoms. Repeated studies have established reliability and validity of the Brief Symptom Inventory, with the initial report (Derogatis and Melisaratos 1983) providing internal consistency coefficients for primary symptom dimensions ranging from 0.68 for Somatization to 0.85 for Depression and test re-test for the Global Severity Index as 0.90. In this study, internal consistency for the Global Severity Index was 0.99.
Youth psychiatric symptoms (baseline)
Youth completed the internalizing composite scale of the 176-item Behavior Assessment System for Children, Second Edition (BASC-2; Reynolds and Kamphaus 2006). This composite scale is a broad index of inwardly directed distress and combines seven subscales: Atypicality (9 items; α = 0.89; e.g., I see weird things), Locus of Control (9 items; α = 0.85; e.g., What I want never seems to matter), Social Stress (10 items; α = 0.90; e.g., I feel out of place around people), Anxiety (13 items; α = 0.91; e.g., I worry but I don't know why), Depression (12 items; α = 0.92; e.g., I feel depressed), Sense of Inadequacy (10 items; α = 0.87; e.g., I fail at things), and Somatization (7 items; α = 0.81; e.g., I often have headaches) subscales. Youth self-report of internalizing symptoms responses was used because youth tend to more accurately capture and report their internal states than their caregivers do (De Los Reyes et al. 2015). Responses were captured using 2-point true or false responses and 4-point Likert scales where 1 = never and 4 = almost always. The summation of points provided a raw score, which was converted to a T-score. The BASC-2 T-score (standardized scores with a mean of 50 and standard deviation of 10) is based on a general adolescent sample. Internal consistency for the overall internalizing composite was 0.98.
Family functioning (eight month follow-up)
Youth and caregivers completed the 60-item Family Assessment Device (Epstein et al. 1983). The Family Assessment Device includes six subscales that assess the six dimensions of the McMaster Model of Family Functioning (i.e., affective involvement, affective responsiveness, behavioral control, communication, problem solving, and roles). The General Family Functioning Scale, which includes 12 statements about family communication and support (e.g., “In times of crisis we can turn to each other for support”; “We are able to make decisions about how to solve problems”.), was included in the current study. Caregivers and youth rate how well statements describe their family on a 4-point Likert scale of 1 = strongly disagree to 4 = strongly agree. Higher scores represent better family functioning (i.e., less dysfunction). Adequate reliability (α = 0.72–0.92; r = 0.66–0.76) and validity have been established (Miller et al. 1985). For the current sample, internal consistency for the General Functioning scale was α = 0.98 (caregiver) and α = 0.96 (youth).
Parental monitoring (sixteen month follow-up)
Youth completed three subscales from the 24-item Parental Monitoring Questionnaire (Stattin and Kerr 2000). Subscales used in the current study include: (1) parental control (i.e., caregivers controlling children’s ability to do things without permission); (2) parental solicitation (i.e., caregivers asking children and their friends for information); and (3) child disclosure (i.e., children spontaneously sharing information with caregivers). Youth rated how well statements describe their family on a 5-point Likert scale (1 = no, never and 5 = yes, always). Higher scores reflect higher levels of parental monitoring. Youth report of parental monitoring was used because it tends to be more closely related to youth outcomes such as substance use (Abar et al. 2015) and delinquency (Augenstein et al. 2016), compared to caregiver report of parental monitoring. Adequate reliability (α = 0.77–0.86) has been established for youth report of parental monitoring (Stattin and Kerr 2000). In the current sample, internal consistencies were α = 0.93 for Parental Control, α = 0.93 for Parental Solicitation scale, and α = 0.92 for Child Disclosure.
Alcohol and marijuana use (twenty-four month follow-up)
Youth reported recent (past 120 days) alcohol and marijuana use on the Adolescent Risk Behavior Assessment (Donenberg et al. 2001). The frequency of the alcohol use variable was highly skewed (9.42) and kurtotic (103.82) due to the majority of youth endorsing no alcohol use (77.6%) during the past 120 days; the variable was transformed into a dichotomous indicator (0 = no use and 1 = use). Marijuana use was coded in the same manner.
Delinquency (twenty-four month follow-up)
Youth completed the National Youth Survey Self-Reported Delinquency (Thornberry and Krohn 2000) scale, a well-validated 40-item self-report measure of delinquent acts (e.g., larceny, fighting, selling drugs). Scores were used from the General Delinquency subscale ranging from 0–23 with higher scores indicating greater number of delinquent acts (in the past 120 days) endorsed (α = 0.98).1
Plan of Analysis
Preliminary analyses consisted of descriptive statistics and bivariate correlations between all study variables. We also examined whether there were differences in key study variables based on demographic characteristics (age, sex, race, status vs. delinquent offense). Next, path analysis was conducted using Mplus statistical software to test study hypotheses. Latent variables were created to represent family functioning, parental monitoring, and youth substance use; all other variables in the model were observed. Family Functioning was composed of caregiver and youth report on the general functioning scale from the Family Assessment Device. Parental Monitoring was composed of youth report on the parental control, parental solicitation, and child disclosure subscales from the Parental Monitoring Questionnaire; only youth report of parental monitoring was used because adolescent reports of parenting behaviors tend to be more closely related to youth outcomes than caregiver reports (Abar et al. 2015; Fleming et al. 2016). Youth substance use was composed of dichotomous indicators of alcohol and marijuana use during the past four months. Missing data were handled using Full Information Maximum Likelihood (Graham 2009; Kline 2005; Muthén and Muthén 1998; Schafer and Graham 2002).
Results
Descriptive Statistics, Bivariate Relationships, and Demographic Differences
Descriptive statistics for primary study variables are presented in Table 2; all variables were normally distributed and ranges were within expected values. The number and proportion of participants who completed each follow-up is shown in Fig. 2; the overall retention rate over 24 months was above 78% at all follow-ups used in the current manuscript.
Table 2.
Descriptive statistics for psychiatric symptoms, family functioning, parental monitoring, and youth substance use and delinquency
| Variable | N | Mean | S.D. | Skewness | Kurtosis | Range |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| Caregiver psychiatric symptoms | 383 | 0.58 | 0.64 | 1.54 | 2.07 | 0–3 |
| Youth psychiatric symptoms | 383 | 52.54 | 14.07 | 0.90 | 0.10 | 34–98 |
| Eight month follow-up | ||||||
| Family functioning (caregiver) | 288 | 3.36 | 0.50 | −0.68 | 0.56 | 1–4 |
| Family functioning (youth) | 280 | 2.86 | 0.55 | 0.14 | 0.57 | 1–4 |
| Sixteen month follow-up | ||||||
| Parental control | 264 | 13.40 | 7.71 | 0.32 | −1.42 | 5–25 |
| Parental solicitation | 263 | 15.60 | 7.12 | −0.19 | −1.26 | 5–25 |
| Child disclosure | 267 | 13.97 | 3.85 | −0.74 | 0.43 | 5–24 |
| Twenty-four month follow-up | ||||||
| Alcohol use (yes = 1) | 295 | 0.24 | – | – | – | 0–1 |
| Marijuana use (yes = 1) | 290 | 0.39 | – | – | – | 0–1 |
| Delinquency | 283 | 0.33 | 1.04 | 4.52 | 25.02 | 0–9 |
Assessments: Caregiver psychiatric symptoms = brief symptom inventory (Derogatis and Melisaratos 1983); youth psychiatric symptoms = behavior assessment system for children, second edition (Reynolds and Kamphaus 2006); family functioning = family assessment device (Epstein et al. 1983); parental monitoring = parental monitoring questionnaire (Stattin and Kerr 2000); youth substance use = adolescent risk behavior assessment (Donenberg et al. 2001); youth delinquency = national youth survey self-reported delinquency (Thornberry and Krohn 2000).
Intercorrelations between variables in the structural model are shown in Table 3. Caregiver psychiatric symptoms were associated with more youth psychiatric symptoms (r = 0.13, p < 0.05) and worse family functioning per caregiver (r = −0.15, p < 0.05) and youth (r = −0.27, p < 0.05) report. Caregiver and youth reports of family functioning were modestly related (r = 0.18, p < 0.01) and on the parental monitoring subscales, correlations were substantial (rs = 0.52–0.75, p < 0.001). Youth report of stronger family functioning was associated with less parental monitoring (rs = −0.17 to −0.29, p < 0.05) and less delinquency (r = −0.17, p < 0.05). Child disclosure was associated with all youth outcomes (rs = 0.19, p < 0.001). Correlations between youth outcomes were all significant (rs = 0.20 to 0.44, p < 0.01).
Table 3.
Intercorrelations between psychiatric symptoms, family functioning, parental monitoring, and youth substance use and delinquency
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | |||||||||||
| 1. Youth age | – | −0.13* | −0.00 | −0.08 | 0.09 | 0.29*** | 0.15* | 0.19** | 0.26*** | 0.22*** | 0.02 |
| 2. Caregiver psychiatric symptoms | – | 0.13* | −0.15* | −0.27*** | 0.00 | −0.06 | −0.11 | −0.01 | −0.01 | −0.01 | |
| 3. Youth psychiatric symptoms | – | −0.35*** | −0.06 | 0.02 | 0.02 | 0.18** | 0.13* | 0.11 | 0.10 | ||
| Eight month follow-up | |||||||||||
| 4. Family functioning (caregiver) | − | 0.18** | −0.05 | −0.03 | −0.07 | −0.12 | −0.07 | −0.05 | |||
| 5. Family functioning (youth) | − | −0.17* | −0.17* | −0.29*** | −0.11 | −0.12 | −0.17* | ||||
| Sixteen month follow-up | |||||||||||
| 6. Parental control | – | 0.75*** | 0.52*** | 0.11 | 0.09 | 0.06 | |||||
| 7. Parental solicitation | – | 0.61*** | 0.06 | 0.07 | 0.13 | ||||||
| 8. Child disclosure | – | 0.19** | 0.19** | 0.19** | |||||||
| Twenty-four month follow-up | |||||||||||
| 9. Alcohol use | – | 0.44*** | 0.23*** | ||||||||
| 10. Marijuana use | – | 0.20** | |||||||||
| 11. Delinquency | – | ||||||||||
p < 0.05
p < 0.01
p < 0.001
Significant demographic differences were found in key study mediators and dependent variables. Age was significantly associated with higher levels of parental monitoring on all subscales (rs = 0.15– 0.29, p < 0.001). Older youth were significantly more likely to endorse using alcohol (t (291) = −4.52, p < 0.001) and marijuana (t (286) = −3.79, p < 0.001). Males reported significantly higher rates of parental monitoring on all subscales (parental control: t (259) = 2.02, p = 0.04; parental solicitation: t (258) = 2.63, p = 0.01; child disclosure: t (262) = 2.14, p = 0.03). Females were significantly more likely to use marijuana than males (χ2 = 4.41, p = 0.04). A marginally significant racial difference emerged, whereby White, non-Latinx youth were more likely and Latinx youth were less likely to report using marijuana than expected by chance (χ2 = 7.43, p = 0.06). Regarding charge type, youth with delinquent offenses reported significantly higher rates of child disclosure (t (256.17) = −2.36, p = 0.02). No other demographic differences emerged. Based on these results, age, sex, and race were accounted for in the structural model, with control pathways only to variables where there were significant differences based on the demographic characteristics. Status versus delinquent offense is not included in the model because there was only a single subscale difference based on this factor; although racial differences emerged only related to marijuana use, this is a key outcome of interest and given there are racial disparities in justice involvement, race was accounted for in the model.
Primary Analyses: Structural Model Testing
The full model (Fig. 3; Table 4) fit the data acceptably (χ 2 (51) = 95.08, p < 0.001; RMSEA = 0.05 with 95% CI 0.03–0.06, CFI = 0.92, SRMR = 0.05). Higher levels of youth (β = −0.44, p < 0.001) and caregiver (β = −0.24, p = 0.017) psychiatric symptoms were prospectively related to worse family functioning, which in turn was related to lower levels of parental monitoring (β = −0.30, p = 0.002), and greater likelihood of substance use (β = −0.25, p = 0.021), and more delinquency (β = −0.19, p = 0.038). Parental monitoring was not related to youth substance use or delinquency. The indirect effect from youth psychiatric symptoms to youth substance use through family functioning was significant (β = 0.11, p = 0.037); the indirect effect from youth psychiatric symptoms to youth delinquency through family functioning was also significant (β = 0.08, p = 0.044). No other indirect pathways were significant.
Fig. 3.
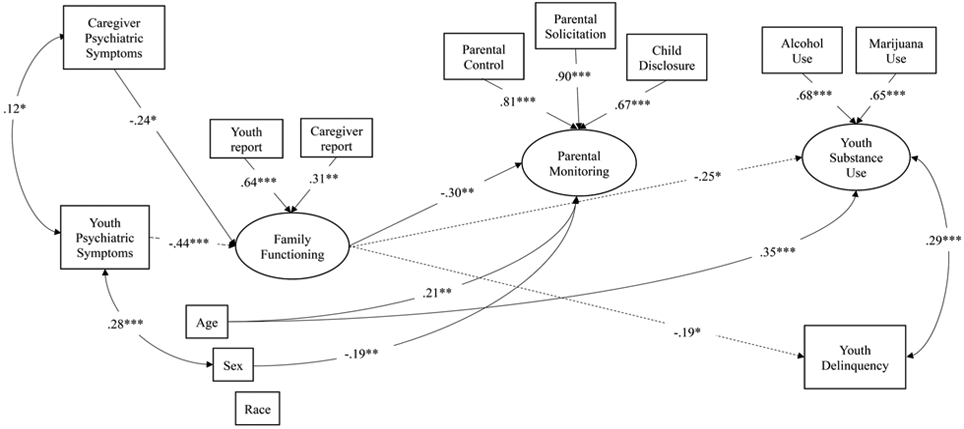
Results of structural model. note. *p < 0.05; **p < 0.01; ***p < 0.001; Non-significant paths have been removed for visual purposes only. Numbers are standardized Betas. Dashed line represents a significant indirect effect
Table 4.
Structural model results
| Parameter | B (SE) | β |
|---|---|---|
| Latent variables | ||
| Family functioning | ||
| Youth report | 1.00 (0.00) | 0.64*** |
| Caregiver report | 0.45 (0.16) | 0.31** |
| Parental monitoring | ||
| Parental control | 1.00 (0.00) | 0.81*** |
| Parental solicitation | 1.03 (0.08) | 0.90*** |
| Child disclosure | 0.41 (0.04) | 0.67*** |
| Substance use | ||
| Alcohol use | 1.00 (0.00) | 0.68*** |
| Marijuana use | 1.09 (0.20) | 0.65*** |
| Structural paths | ||
| Caregiver psychiatric symptom→family functioning | −0.13 (0.05) | −0.24* |
| Youth psychiatric symptoms→family functioning | −0.11 (0.02) | −0.44*** |
| Caregiver psychiatric symptoms→parental monitoring | −1.26 (0.74) | −0.13 |
| Family functioning→parental monitoring | −5.33 (2.08) | −0.30** |
| Family functioning→substance use | −0.21 (0.11) | −0.25* |
| Parental monitoring→substance use | 0.00 (0.00) | 0.07 |
| Family functioning→delinquency | −0.57 (0.28) | −0.19* |
| Parental monitoring→delinquency | 0.01 (0.01) | 0.08 |
| Control paths | ||
| Age→parental monitoring | 0.86 (0.28) | 0.21** |
| Sex→parental monitoring | −2.40 (0.80) | −0.19** |
| Age→substance use | 0.07 (0.02) | 0.35*** |
| Sex→substance use | 0.08 (0.04) | 0.14 |
| Race→substance use | −0.02 (0.02) | −0.09 |
| Correlated error terms | ||
| Caregiver and youth psychiatric symptoms | 0.10 (0.05) | 0.12* |
| Substance use and delinquency | 0.07 (0.02) | 0.29*** |
| Youth psychiatric symptoms with sex | 0.19 (0.04) | 0.28*** |
| Youth psychiatric symptoms with race | −0.06 (0.09) | −0.03 |
p < 0.05
p < 0.01
p < 0.001
Sensitivity Analyses
In sensitivity analyses, the structural model was modified to determine whether results were consistent when including direct pathways from youth psychiatric symptoms to youth substance use and delinquency. The revised model fit the data acceptably (χ 2 (49) = 94.44, p < 0.001; RMSEA = 0.05 with 95% CI 0.03–0.06, CFI = 0.92, SRMR = 0.05). Consistent with the initial model, higher levels of youth (β = −0.42, p < 0.001) and caregiver (β = −0.23, p = 0.030) psychiatric symptoms were prospectively related to worse family functioning, which in turn was related to lower levels of parental monitoring (β = −0.30, p = 0.002). However, the pathways between family functioning and youth substance use (β = −0.17, p = 0.238) and delinquency (β = −0.18, p = 0.142), although similar in direction and magnitude to the original model, were no longer statistically significant. Youth psychiatric symptoms were not significantly related to youth substance use or delinquency. None of the indirect pathways were significant.
Discussion
Court-involved youth exhibit high rates of psychiatric symptoms, substance use, and delinquency. Family dynamics (e.g., family functioning, parental monitoring) are linked with these behavioral health and legal outcomes, and understanding the ways in which these relationships operate at point of first-time justice contact is critical to improving public health and legal outcomes. The current prospective study of first-time offending court-involved youth examined the mediating role of family functioning and parental monitoring between caregiver and youth psychiatric symptoms and youth risk behavior (substance use, delinquency) over a two-year period.
Consistent with study hypotheses, when caregivers and youth reported higher levels of psychiatric symptoms, families tended to experience worse family functioning, which in turn was related to higher levels of delinquency and a higher likelihood of substance use among youth two years after their first contact with the juvenile court system. Caregiver psychiatric symptoms were unrelated to parental monitoring, and parental monitoring was unrelated to youth substance use or delinquency.
Consistent with prior research on court-involved youth (Tolou-Shams et al. 2018) and broader samples of adolescents (Krug et al. 2016; Simpson et al. 2018), caregiver psychiatric symptoms were prospectively related to worse family functioning, as were youth internalizing problems. Caregivers of court-involved youth (Brown et al. 2018) and court-involved youth themselves (Carswell et al. 2004; Cocozza and Skowyra 2000) have elevated psychiatric symptoms relative to non-court-involved youth and families. When even one family member is depressed, for example, family functioning can be compromised (Du et al. 2014). Further, youth legal involvement places a significant burden on caregivers, who may not be prepared to manage the stress of court and treatment mandates; this could increase strain on caregivers and within the family environment, resulting in impaired family functioning.
Consistent with a prior study involving court-involved youth (Tolou-Shams et al. 2018), but not more general samples of adolescents (Van Loon et al. 2014), caregiver psychiatric symptoms were not related to parental monitoring. It is unclear why the relationship between caregiver psychiatric symptoms and parental monitoring is not present when examining a first-time offending court-involved sample. One possibility is that, since it is the first time youth are having contact with the juvenile court, caregivers may be more highly aware of the need, and feel more pressured to engage in parental monitoring, regardless of their mental health status. Caregivers may also be receiving new resources for their youth and family, which may be a moderating factor in this relationship; understanding more about this association would be an important area for future research.
Caregiver psychiatric symptoms were, however, related to worse family functioning. This relationship is highly relevant for clinicians because most family-based treatments for justice-involved youth do not directly target caregiver psychiatric symptoms (National Institute of Justice 2011). One exception is Multisystemic Therapy (Huey et al. 2000), which involves providing evidence-based treatment to caregivers for their specific psychiatric concerns (e.g., Myers et al. 2011). Caregivers experiencing psychiatric symptoms who receive appropriate treatment may be better able to engage in youth-focused and family-based treatment, which may improve overall family functioning and allow them to use parenting skills learned in treatment to mitigate future youth delinquency (Huey et al. 2000). Even if caregivers do not have a pre-existing psychiatric condition (which many do), caring for an adolescent who has recently become court-involved can be stressful and increase caregiver psychiatric symptoms. As such, programs for first-time court-involved youth and their families that directly address caregiver stress and psychiatric problems, in addition to youth psychiatric problems, may be most effective in improving family functioning and thereby preventing future delinquency and justice involvement.
Contrary to hypotheses, better family functioning was prospectively related to less parental monitoring. This may be due to the nature of the assessments and the imposition of an external monitoring system on youth’s behavior (i.e., juvenile justice system). The general family functioning scale used in the current study involves perceptions of communication (e.g., make decisions about how to solve problems) and support (e.g., turn to each other for support in times of crisis). When family functioning is better, youth may perceive less parental monitoring because open communication is more natural within the family. Conversely, when families have less functional patterns of communication and support, youth may be more aware of parental monitoring, which conflicts with the lack of communication characteristic of the family. Court-involved youth are likely in greater need of parental monitoring than non-court-involved youth, as they have become justice-involved due to problematic behavior. It is possible that factors, such as caregivers’ reliance on monitoring related to the youth’s court involvement (e.g., court hearings, probation, diversion programs) and youth’s perceptions of the court monitoring, impact the relationship between family functioning and perceptions of parental monitoring; this should be explored in future research.
Parental monitoring was not related to substance use or delinquency in the structural model. Prior research with boys on probation (Caldwell et al. 2006), detained youth (Voisin et al. 2012), Black females from low-income neighborhoods (DiClemente et al. 2001), diverse general population adolescents (i.e., living in the community and not sampled based on court involvement) (Barnes et al. 2006; Parker and Benson 2004), and Hispanic/Latino adolescents (Wagner et al. 2010) has demonstrated a protective effect of parental monitoring against adverse outcomes including substance use and delinquency. This was not the case in the current sample of first-time offending court-involved youth. In fact, at the bivariate level, there was a positive association between child disclosure and youth substance use and delinquency. Having become involved in the legal system for the first time, first-time offending court-involved youth may be more forthcoming with their caregivers when using substances or engaging in delinquent behavior due to external factors like ongoing court hearings and drug testing by juvenile drug court programs and/or probation officers. This newly imposed external monitoring, an experience which is universal for the current sample, may be attenuating the relationship between parental monitoring and youth substance use and delinquency.
Moreover, some research has found parental monitoring to be unrelated to marijuana use and sexual activity when considering other family factors (e.g., parental trust; Borawski et al. 2003). It may be that among first-time offending court-involved youth, other family factors captured by the general family functioning construct are stronger influences on youth substance use and delinquency. Further research is needed to understand the relationships among different parenting practices and youth substance use and delinquency among justice-involved youth.
Results of the current study have important implications for understanding how family factors contribute to youth delinquency and substance use over time. Strengths of the study include the use of a prospective design, empirically validated assessments, and a multi-informant approach. The uniqueness of the sample is also a strength; youth participants were newly justice-involved and had just experienced their first court contact. Little is known about what happens immediately after a youth becomes court-involved; this study sheds light on important family processes during the first two years following initial court contact.
The study also has several noteworthy limitations. First, despite the sample’s racial, ethnic, and sex diversity, youth were sampled from a single family court in the northeastern region of the United States; future research is needed to understand whether these findings generalize to youth in other regions of the United States and internationally. Additional family factors (e.g., caregiver marital status) should also be taken into account in future research.
Second, due to limited power given the number of variables in the study and available sample size, bidirectional or recursive impacts of the variables over time were not examined. A more sophisticated causal analysis assessing the degree to which changes in one variable result in changes in the other variable (and vice versa) would likely be a promising future direction holding relevant implications for intervention. Limitations to power may also be influencing the findings from sensitivity analyses, as each additional pathway added reduces one’ s ability to detect significant effects. Specifically, although of similar magnitude to the original structural model testing, the pathways from family functioning to youth substance use and delinquency are no longer significant when pathways between youth psychiatric symptoms and these outcomes are included. Although of value, there is much debate in the field about the use of statistical significance as a metric for interpreting results (Wasserstein et al. 2019). Given the theoretical justification for the relationships between family functioning and youth substance use and delinquency, as well as youth psychiatric symptoms and these outcomes, future research should continue to explore these pathways.
Third, self-report of substance use and delinquency were used rather than official records. Within the court context, there is always a concern that respondents will be less likely to disclose sensitive or illicit behaviors, as disclosure could have legal implications. The current data revealed substantial rates of self-reported substance use and delinquent behavior (e.g., 39% used marijuana in the past 4 months), suggesting youth were comfortable reporting these behaviors and this bias was not an overwhelming concern. Future research should consider utilizing self-report and official records of delinquent behavior (e.g., arrest records, probation violations) and substance use (e.g., urine toxicology screen results) to corroborate and mitigate the potential biases of self-report.
Additionally, only youth report of parental monitoring was used in the current study. Youth reports of parental monitoring tend to be more strongly linked with youth substance use (Abar et al. 2015) and delinquency (Augenstein et al. 2016) than caregiver reports, and offer a potential point of intervention (e.g., altering adolescents’ perceptions). A growing body of research, however, documents the predictive role of the discrepancy between youth and caregiver report of parental monitoring (De Los Reyes et al. 2010). This is an important area for future research among justice-involved youth.
Conclusion
First-time offending court-involved youth are at high-risk for adverse outcomes including substance use and ongoing delinquent behavior. Since many of these youth (and all in the current study) reside with their families, understanding how caregiver and family factors contribute to youth’s substance use and delinquency is vital. The current prospective study examined whether family functioning and parental monitoring mediate the relationships between youth and caregiver psychiatric symptoms and youth substance use and delinquency. The results of the current study demonstrate that family functioning, which is influenced by caregiver and youth psychiatric symptoms, has critical implications for youth substance use and delinquency. As such, viewing court-involved youth as “the problem” in isolation of caregiver and family functioning is inherently problematic. This is a paradigm shift for many juvenile courts, though in line with decades of research documenting the effectiveness of family-based treatment modalities. Addressing the needs of the family more holistically will likely be beneficial in reducing youth substance use and delinquency in this population.
Acknowledgements
Many thanks to the members of the Juvenile Justice Behavioral Health Lab for their assistance with this research, and to the youth and families who participated.
Funding This research was supported by grants from the National Institute on Drug Abuse (R01DA034538) and National Institute of Mental Health (T32MH018261).
Biography
Johanna B. Folk is a Postdoctoral Fellow at the University of California, San Francisco. Her major research interests include understanding how best to improve behavioral health outcomes for justice-involved populations, focusing on the role of interpersonal relationships and family support.
Larry K. Brown is the Director of the Division of Child and Adolescent Psychiatry at Bradley and Hasbro Children’s Hospitals; Professor and Vice Chair in the Department of Psychiatry and Human Behavior, Alpert Medical School of Brown University. His research interests include HIV prevention for at-risk youth and clinical interventions for those living with HIV.
Brandon D. L. Marshall is an Associate Professor of Epidemiology at the Brown University School of Public Health and also serves as an Associate Editor for the International Journal of Drug Policy. His research interests include substance use epidemiology, infectious diseases, and the social, environmental, and structural determinants of health of urban populations.
Lili M. C. Ramos is a Clinical Research Coordinator at the University of California, San Francisco. Her major research interests include improving child and adolescent mental health, with a specific focus on justice-involved youth, early childhood trauma, and family processes.
Lakshmi Gopalakrishnan is a Clinical Research Coordinator at the University of California, San Francisco. Her research interests include integrated community-based interventions to promote child and adolescent mental health, improve family functioning, and reduce substance abuse.
Daphne Koinis-Mitchell is a Professor in the Departments of Psychiatry and Human Behavior and Pediatrics, Alpert Medical School of Brown University; Director of the Community Asthma Program and The Faculty Development and Research Mentoring Program in the Department of Pediatrics. Her research interests include pediatric health disparities with a focus on asthma and sleep health.
Marina Tolou-Shams is a UCSF Professor in the Department of Psychiatry, Division Director of Infant, Child and Adolescent Psychiatry, Deputy Vice Chair for Research, and Chief Psychologist at the Zuckerberg San Francisco General Hospital. Her research interests have primarily focused on the development and testing of empirically supported integrated mental health, substance use and sexual health interventions for justice-involved youth.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Data Sharing and Declaration The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Ethical Approval All recruitment and study procedures were approved by the Principal Investigator’s university and collaborating sites’ Institutional Review Board (and Office for Human Research Protections) and conducted in accordance with the ethical standards of the American Psychological Association.
Informed Consent All caregivers enrolled in the study provided informed consent and adolescents provided assent.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original subscale includes 24 items. Due to an error in the audio-assisted computerized assessment development, item 24 of the National Youth Survey Self-Reported Delinquency general delinquency scale, “Have you had sexual intercourse with a person who was not your serious partner when involved in a relationship?” was not administered to study participants; therefore, subscale scores range from 1-23 but still accurately indicate that greater scores represent greater number of delinquent acts.
References
- Abar CC, Jackson KM, Colby SM, & Barnett NP (2015). Parent-child discrepancies in reports of parental monitoring and their relationship to adolescent alcohol-related behaviors. Journal of Youth and Adolescence, 44(9), 1688–1701. 10.1007/s10964-014-0143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abram KM, Teplin LA, McClelland GM, & Dulcan MK (2003). Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 60, 1097–1108. 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augenstein TM, Thomas SA, Ehrlich KB, Daruwala S, Reyes SM, Chrabaszcz JS, & De Los Reyes A (2016). Comparing multi-informant assessment measures of parental monitoring and their links with adolescent delinquent behavior. Parenting,Science and Practice, 16(3), 164–186. 10.1080/15295192.2016.1158600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes GM, Hoffman JH, Welte JW, Farrell MP, & Dintcheff BA (2006). Effects of parental monitoring and peer deviance on substance use and delinquency. Journal of Marriage and Family, 68(4), 1084–1104. 10.1111/j.1741-3737.2006.00315.x. [DOI] [Google Scholar]
- Belenko S, Knight D, Wasserman GA, Dennis ML, Wiley T, Taxman FS, & Sales J (2017). The juvenile justice behavioral health services cascade: a new framework for measuring unmet substance use treatment services needs among adolescent offenders. Journal of Substance Abuse Treatment, 74, 80–91. 10.1016/j.jsat.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borawski EA, Ievers-Landis CE, Lovegreen LD, & Trapl ES (2003). Parental monitoring, negotiated unsupervised time, and parental trust: The role of perceived parenting practices in adolescent health risk behaviors. The Journal of Adolescent Health, 33(2), 60–70. 10.1016/S1054-139X(03)00100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borre A, & Kliewer W (2014). Parental strain, mental health problems, and parenting practices: a longitudinal study. Personality and Individual Differences, 68, 93–97. 10.1016/j.paid.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Tarantino N, Tolou-Shams M, Esposito-Smythers C, Healy MG, & Craker L (2018). Mental health symptoms and parenting stress of parents of court-involved youth. Journal of Child and Family Studies, 27(3), 843–852. 10.1007/s10826-017-0923-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell RM, Beutler LE, An Ross S, & Clayton Silver N (2006). Brief report: an examination of the relationships between parental monitoring, self-esteem and delinquency among Mexican American male adolescents. Journal of Adolescence, 29 (3), 459–464. 10.1016/j.adolescence.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Carswell K, Maughan B, Davis H, Davenport F, & Goddard N (2004). The psychosocial needs of young offenders and adolescents from an inner city area. Journal of Adolescence, 27(4), 415–428. 10.1016/j.adolescence.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Cocozza JJ, & Skowyra KR (2000). Youth with mental health disorders: Issues and emerging responses. Juvenile Justice, 7(1), 3–13. [Google Scholar]
- Cottle CC, Lee RJ, & Heilbrun K (2001). The prediction of criminal recidivism in juveniles: a meta-analysis. Criminal Justice and Behavior, 28(3), 367–394. 10.1177/0093854801028003005. [DOI] [Google Scholar]
- Daches S, Vine V, Layendecker KM, George CJ, & Kovacs M (2018). Family functioning as perceived by parents and young offspring at high and low risk for depression. Journal of Affective Disorders, 226, 355–360. 10.1016/j.jad.2017.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. 10.1037/a0038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Goodman KL, Kliewer W, & Reid-Quiñones K (2010). The longitudinal consistency of mother-child reporting discrepancies of parental monitoring and their ability to predict child delinquent behaviors two years later. Journal of Youth and Adolescence, 39(12), 1417–1430. 10.1007/s10964-009-9496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The brief symptom inventory: an introductory report. Psychological Medicine, 13(3), 595 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Crosby R, Sionean C, Cobb BK, Harrington K, & Oh MK (2001). Parental monitoring: association with adolescents’ risk behaviors. Pediatrics, 107(6), 1363–1368. 10.1542/peds.107.6.1363. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, & Weber-Shifrin E (2001). Understanding AIDS-risk behavior among adolescents in psychiatric care: links to psychopathology and peer relationships. Journal of the American Academy of Child and Adolescent Psychiatry, 40(6), 642–653. 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du N, Ran M-S, Liang S-G, Situ M-J, Yi J, Mansfield AK, & Keitner G (2014). Comparison of family functioning in families of depressed patients and nonclinical control families in China using the family assessment device and the family adaptability and cohesion evaluation scales II. Annals of Clinical Psychiatry, 26(1), 47–56. [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, & Bishop DS (1983). The McMaster family assessment device. Journal of Marital and Family Therapy, 9(2), 171–180. 10.1111/j.1752-0606.1983.tb01497.x. [DOI] [Google Scholar]
- Fendrich M, Warner V, & Weissman MM (1990). Family risk factors, parental depression, and psychopathology in offspring. Developmental Psychology, 26(1), 40–50. 10.1037/0012-1649.26.1.40. [DOI] [Google Scholar]
- Fleming CB, Mason WA, Thompson RW, Haggerty KP, & Gross TJ (2016). Child and parent report of parenting as predictors of substance use and suspensions from school. Journal of Early Adolescence, 36(5), 625–645. 10.1177/0272431615574886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosco GM, Stormshak EA, Dishion TJ, & Winter CE (2012). Family relationships and parental monitoring during middle school as predictors of early adolescent problem behavior. Journal of Clinical Child and Adolescent Psychology, 41(2), 202–213. 10.1080/15374416.2012.651989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gault-Sherman M (2012). It’s a two-way street: the bidirectional relationship between parenting and delinquency. Journal of Youth and Adolescence, 41(2), 121–145. 10.1007/s10964-011-9656-4. [DOI] [PubMed] [Google Scholar]
- Goodyear M, Hill T-L, Allchin B, McCormick F, Hine R, Cuff R, & O’Hanlon B (2015). Standards of practice for the adult mental health workforce: meeting the needs of families where a parent has a mental illness. International Journal of Mental Health Nursing, 24(2), 169–180. 10.1111/inm.12120. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan PH, Loeber R, & Henry DB (1998). Relation of family problems to patterns of delinquent involvement among urban youth. Journal of Abnormal Child Psychology, 26(5), 319–333. 10.1023/A:1021995621302. [DOI] [PubMed] [Google Scholar]
- Graham JW (2009). Missing data analysis: making it work in the real world. Annual Review of Psychology, 60, 549–576. 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Scheier LM, Diaz T, & Miller NL (2000). Parenting practices as predictors of substance use, delinquency, and aggression among urban minority youth: moderating effects of family structure and gender. Psychology of Addictive Behaviors, 14(2), 174–184. 10.1037/0893-164X.14.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, & Carter AS (2007). Prevalence, correlates, and persistence of maternal depression. Journal of Women’s Health, 16(5), 678–691. 10.1089/jwh.2006.0185. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Henggeler SW, Brondino MJ, & Pickrel SG (2000). Mechanisms of change in multisystemic therapy: Reducing delinquent behavior through therapist adherence and improved family and peer functioning. Journal of Consulting and Clinical Psychology, 68(3), 451–467. 10.1037/0022-006X.68.3.451. [DOI] [PubMed] [Google Scholar]
- Hyland N (2018). Delinquency Cases in Juvenile Court, 2014. https://www.ojjdp.gov/pubs/251107.pdf. [Google Scholar]
- Khantzian EJ (1997). The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kline RB (2005). Principles and practice of structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Krug S, Wittchen H-U, Lieb R, Beesdo-Baum K, & Knappe S (2016). Family functioning mediates the association between parental depression and low self-esteem in adolescents. Journal of Affective Disorders, 203, 184–189. 10.1016/j.jad.2016.06.008. [DOI] [PubMed] [Google Scholar]
- Miller IW, Epstein NB, Bishop DS, & Keitner GI (1985). The McMaster family asessment device: reliability and validity. Journal of Marital and Family Therapy, 11(4), 345–356. 10.1111/j.1752-0606.1985.tb00028.x. [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus: Statistical analysis with latent variables, User’s Guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Myers RJ, Roozen HG, & Smith JE (2011). The community reinforcement approach: an update of the evidence. Alcohol Research and Health, 33(4), 380–388. [PMC free article] [PubMed] [Google Scholar]
- National Institute of Justice. (2011). All programs and practices. https://www.crimesolutions.gov/Programs.aspx. May 27, 2019. [Google Scholar]
- Ohannessian CM, Flannery KM, Simpson E, & Russell BS (2016). Family functioning and adolescent alcohol use: a moderated mediation analysis. Journal of Adolescence, 49, 19–27. 10.1016/j.adolescence.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker JS, & Benson MJ (2004). Parent-adolescent relations and adolescent functioning: self-esteem, substance abuse, and delinquency. Adolescence, 39(155), 519–530. [PubMed] [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Nomura Y, & Weissman MM (2006). Family discord, parental depression, and psychopathology in offspring: 20-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 45(4), 452–460. 10.1097/01.chi.0000198592.23078.8d. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2006). BASC-2: Behavior Assessment System for Children 2nd Edn. Upper Saddle River, NJ: Pearson Education, Inc. [Google Scholar]
- Rhee K (2008). Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. Annals of the American Academy of Political and Social Science, 615(1), 12–37. 10.1177/0002716207308400. [DOI] [Google Scholar]
- Romer D, Hornik R, Stanton B, Black M, Li X, Ricardo I, & Feigelman S (1997). “Talking” computers: a reliable and private method to conduct interviews on sensitive topics with children. Journal of Sex Research, 34(1), 3–9. 10.1080/00224499709551859. [DOI] [Google Scholar]
- Ryan SM, Jorm AF, & Lubman DI (2010). Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Australian and New Zealand Journal of Psychiatry, 44(9), 774–783. 10.1080/00048674.2010.501759. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: our view of the state of the art. Psychological Methods, 7(2), 147–177. 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Schei J, Jozefiak T, Nøvik TS, Lydersen S, & Indredavik MS (2013). The impact of coexisting emotional and conduct problems on family functioning and quality of life among adolescents with ADHD. Journal of Attention Disorders, 20(5), 424–433. 10.1177/1087054713507976. [DOI] [PubMed] [Google Scholar]
- Sheidow AJ, Henry DB, Tolan PH, & Strachan MK (2014). The role of stress exposure and family functioning in internalizing outcomes of urban families. Journal of Child and Family Studies, 23(8), 1351–1365. 10.1007/s10826-013-9793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shek DTL (2002). Family functioning and psychological well-being, school adjustment, and problem behavior in Chinese adolescents with and without economic disadvantage. The Journal of Genetic Psychology, 163(4), 497–502. 10.1080/00221320209598698. [DOI] [PubMed] [Google Scholar]
- Simpson EG, Vannucci A, & Ohannessian CM (2018). Family functioning and adolescent internalizing symptoms: a latent profile analysis. Journal of Adolescence, 64, 136–145. 10.1016/j.adolescence.2018.02.004. [DOI] [PubMed] [Google Scholar]
- Skowyra KR, & Cocozza JJ 2007). Blueprint for change: a comprehensive model for the identification and treatment of youth with mental health needs in contact with the juvenile justice system Office of Juvenile Justice and Delinquency Prevention. New York, NY: Delmar; http://www.umt.edu/sociology/faculty_staff/burfeind/documents/Soc438_SkowyraCocozza2007_s08.pdf. [Google Scholar]
- Stattin H, & Kerr M (2000). Parental monitoring: a reinterpretation. Child Development, 71(4), 1072–1085. 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Tamplin A (1998). Family functioning and parent general health in families of adolescents with major depressive disorder. Journal of Affective Disorders, 48(1), 1–13. 10.1016/S0165-0327(97)00105-5. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, & Mericle AA (2002). Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 59(12), 1133–1143. 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, & Krohn MD (2000). The self-report method for measuring delinquency and crime In Duffee D (Ed.), Measurement and analysis of crime and justice: Criminal justice (pp. 33–84). Washington, DC: U.S. Department of Justice. [Google Scholar]
- Tolou-Shams M, Brogan L, Esposito-Smythers C, Healy MG, Lowery A, Craker L, & Brown LK (2018). The role of family functioning in parenting practices of court-involved youth. Journal of Adolescence, 63, 165–174. 10.1016/j.adolescence.2017.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Loon LMA, Van de Ven MOM, Van Doesum KTM, Witteman CLM, & Hosman CMH (2014). The relation between parental mental illness and adolescent mental health: the role of family factors. Journal of Child and Family Studies, 23(7), 1201–1214. 10.1007/s10826-013-9781-7. [DOI] [Google Scholar]
- Vermeiren R (2003). Psychopathology and delinquency in adolescents: a descriptive and developmental perspective. Clinical Psychology Review, 23, 277–318. 10.1016/S0272-7358(02)00227-1. [DOI] [PubMed] [Google Scholar]
- Voisin DR, Tan K, Tack AC, Wade D, & DiClemente R (2012). Examining parental monitoring as a pathway from community violence exposure to drug use, risky sex, and recidivism among detained youth. Journal of Social Service Research, 38(5), 699–711. 10.1080/01488376.2012.716020. [DOI] [Google Scholar]
- Wagner KD, Ritt-Olson A, Chou C-P, Pokhrel P, Duan L, Baezconde-Garbanati L, & Unger JB (2010). Associations between family structure, family functioning, and substance use among Hispanic/Latino adolescents. Psychology of Addictive Behaviors, 24(1), 98–108. 10.1037/a0018497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserstein RL, Schirm AL, & Lazar NA (2019). Moving to a World Beyond “p < 0.05”. American Statistician, 73(sup1), 1–19. 10.1080/00031305.2019.1583913. [DOI] [Google Scholar]


