Abstract
Background:
Healthy diet is essential in the management of chronic kidney disease (CKD) and preventing related comorbidities. Food outlet access has been studied in the general population; however, the influence of the local food environment on dietary intake among people with CKD has not been evaluated.
Objectives:
This study examined the associations of food outlet density and type of outlets with dietary intake in a multicenter cohort of racially and ethnically diverse patients with CKD.
Methods:
The Chronic Renal Insufficiency Cohort (CRIC) Study is a multicenter prospective study of patients with CKD that used a validated food frequency questionnaire to capture dietary intake at the baseline visit. This is a cross-sectional analysis of 2,484 individuals recruited in 2003-2006 from seven CRIC Study centers. Food outlet data was purchased to construct a count of the number of fast food restaurants, convenience stores, and grocery stores per 10,000 population for each geocoded census block group. Multivariable linear and logistic regression models were used to evaluate the associations between measures of food outlet availability and dietary factors.
Results:
The proportion of participants living in zero, low, and high food outlet density areas differed by gender, race/ethnicity, and income level. Among males, living in areas with zero or the highest number of outlets was associated with having the highest caloric intakes in multivariable models. Males living in areas with zero outlets consumed the highest levels of sodium and phosphorous. Females living in areas with zero outlets had the lowest average intake of calories, sodium, and phosphorous. Among low-income females, close proximity to more outlets was associated with higher calorie consumption. Among all participants, access to fast food restaurants was not associated with an unhealthy diet score, nor access to grocery stores with a healthy diet score.
Conclusions:
Average caloric and nutrient intakes differed by outlet availability; however, there were no strong associations with type of food outlet. This should be considered when developing food-focused public health policies.
Keywords: chronic kidney disease, chronic renal insufficiency, cohort study, food outlets, food environments, diet, eating behavior, CRIC (Chronic Renal Insufficiency Cohort)
Introduction
Public health messaging has increasingly called for increased access to healthy food. In the context of chronic kidney disease (CKD), access to foods that comprise a healthy diet may be especially relevant given the potential impact that behavioral interventions may have on the increased risk for cardiovascular disease (CVD) and mortality attributed to CKD. Evaluation of the associations between food access, diet and health outcomes has emerged as an area of interest as researchers try to explain health disparities that are not completely explained by individual behaviors. Local food environments vary and may contain grocery stores, convenience stores, and fast food restaurants. Prior studies in the general population have found higher fast food restaurant density to be associated with increased consumption of fast food1,2 and decreased odds of having a healthy diet3. Food purchases from fast food and convenience stores may be unhealthy due to larger portions and high concentrations of sugar, fat, sodium and phosphate additives4–6. Consumption of processed foods has been associated with lower intakes of fruits, vegetables, fiber, and milk7–9. Past studies have shown that having no grocery stores or supermarkets nearby is associated with poor diet among both low-income10 and mixed-income adults11, but little is known about the association between access to food outlets and dietary patterns among individuals with CKD.
The investigation of these associations within a CKD population is particularly warranted given the roles diet and nutritional treatment play in the managing CKD and its comorbidities such as mineral and bone disorders12,13. Processed meats and cheeses, frozen meals, prepackaged baked goods, and colas could be particularly detrimental to health among individuals with CKD due to high concentrations of sodium- and phosphorus-based food additives4,14. Adjusting dietary phosphorus intake is one important aspect of the nutritional management of chronic kidney disease in adults13. In the general population, phosphorus intakes that exceed nutritional thresholds contribute to vascular calcification, impaired kidney function, and bone loss15. Prior studies of patients with CKD have shown high serum phosphate levels to be associated with CVD and increased mortality4,16,17, indicating that high dietary phosphorus intake may be related to even worse health effects among persons with existing CKD.
Lower socioeconomic status has been associated with consumption of nutrient-poor and energy-dense diets18,19, and food consumption and eating behaviors are known to differ by gender20–22. Decreased access to healthy food outlets like grocery stores and increased reliance on fast food outlets due to lower costs may be particularly burdensome on individuals with lower income19,23. Low socioeconomic status has also been associated with disparities among those with CKD24,25 and there are documented differences in CKD prevalence and long-term health outcomes by gender26–28. Evaluation of the association between food outlet density and dietary characteristics overall, in addition to understanding if associations differ by gender or income levels may provide insights into tailored strategies to strengthen healthy eating interventions and encourage healthy living among subgroups of individuals with CKD.
This study uses data from the Chronic Renal Insufficiency Cohort (CRIC) Study to examine the density of different types of food outlets within close proximity to each participant’s census block group among a cohort of individuals with CKD. The study then assessed the association between food outlet density and dietary intake and examined if the relationships between food outlet density and dietary intake differed by gender or income level.
Methods
Study sample
The CRIC Study is a prospective observational multicenter study of risk factors for the progression of CKD and cardiovascular disease in individuals with mild-to-moderate CKD. Details of the study design and baseline characteristics of study participants have been published 29,30 Participants were recruited between 2003 and 2008 from seven U.S. clinical centers in Ann Arbor, Michigan; Baltimore, Maryland; Chicago, Illinois; Cleveland, Ohio; New Orleans, Louisiana; Philadelphia, Pennsylvania; and Oakland, California. The flow diagram for sample exclusions is shown in Figure 1 (online supplementary material). A residential address that could be geocoded to the census block groups in the 2000 US Census was available for 2,930 of the 3,939 participants who completed the baseline visit. Four-hundred forty six participants chose not to report their income level and were excluded. Descriptive analyses were restricted to the 2,484 participants with measures of food outlet density and self-reported income data available. An additional 595 were missing information on dietary intake, either due to incomplete data from diet history questionnaires or exclusion by the data coordinating center due to implausible values. The final analytic sample to evaluate associations with diet included 1,889 participants. The CRIC study was approved by the local institutional review board at each clinical center, and participants provided written informed consent.
Figure 1.
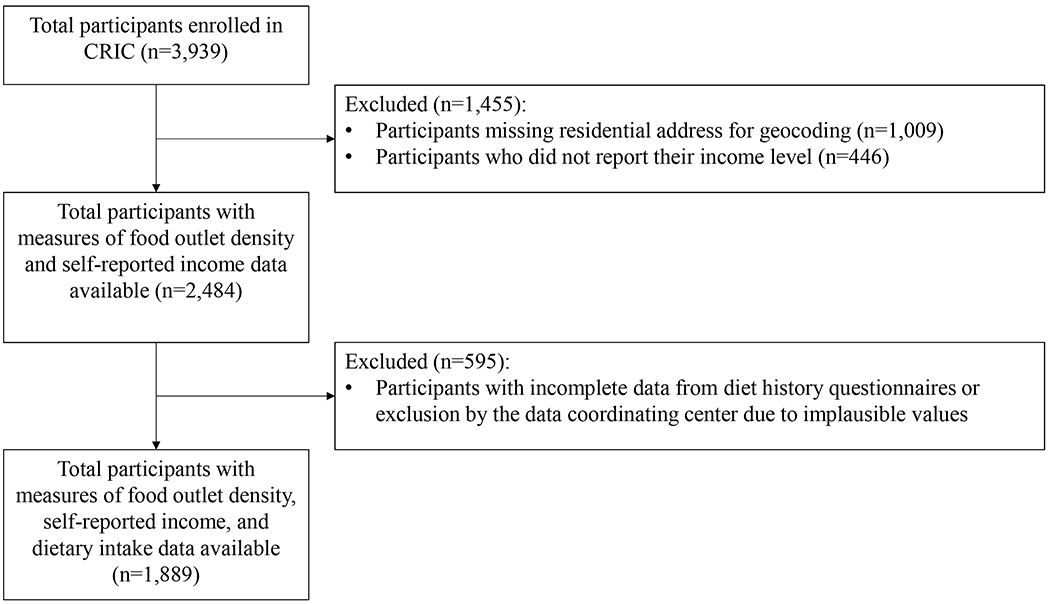
Participant flow diagram showing sample exclusions and final numbers for statistical analysis.
Outcome variables
Information on dietary intake was collected at the baseline CRIC study visit using a validated food frequency questionnaire developed by the National Cancer Institute (NCI)31. Participants recalled portion size and frequency from 124 food items consumed over the preceding 12 months. This information was analyzed using the NCI’s DietCalc software and output as total caloric intake (kcal/day); percentage of calories from carbohydrates, saturated fat, and protein; protein (g/day); saturated fat (g/day); calcium (mg/day); sodium (mg/day); phosphorous (mg/day); cholesterol (mg/day); and sugar-sweetened beverages (ounces/week). Study outcomes also included the number of servings of fruits, vegetables, and whole grains that each participant consumed per day. An overall diet score adapted from the American Heart Association’s recommendations for cardiovascular health32 was calculated by scoring each participant’s diet by assigning one point for having above the median values for 1) fruit/vegetable servings per day, 2) fish servings per week, and 3) whole grain servings per day and below the median values for 4) 24-hour urine sodium excretion, and 5) sweets/sugary beverage portions per week33. The diet score ranged from 0 to 5 and in this study the diet score was dichotomized into a “healthy diet” for those that scored 4 to 5 points and “unhealthy diet” for those that scored 0 to 3 points as has been done in prior studies33.
Exposure variables
Food outlet data for the CRIC enrollment period was obtained from Dun and Bradstreet’s (D&B), and the count of food outlets was matched to the enrollment year for each participant. Standard Industrial Classification (SIC) codes as listed in Table 1 (online supplementary material) were used to classify outlets by type (fast food restaurant, convenience store, or grocery store), to create an annual estimate of each type of outlet for each participant based on their year of their enrollment. Using Geographic Information System software (ArcGIS, version 10.3) each food outlet was geocoded using the address and x and y coordinates provided by D&B and defined 1 kilometer (1km) concentric areas (Euclidean buffer) from each participant’s census block group centroid. Within each buffer, counts of fast food restaurants, convenience stores, and grocery stores were calculated and standardized per 10,000 population using the 2000 US Census block group population data. Prior studies have used scaled measures of food outlets to account for the development of a particular geographic area34,35. When there was overlap between block group buffers, the proportion of each block group area buffer that overlapped with another block group area buffer was calculated and the counts of food outlets were adjusted to address the overlap with other block group buffers.
Table 1.
United States Department of Labor Standard Industrial Classification (SIC)a codes and definitions used to group food outlets into types
| Food Outlet Type | SIC Code | SIC Definition |
|---|---|---|
| Fast Food | 58120300 | Fast Food Restaurants and Stands |
| 58120301 | Box Lunch Stand | |
| 58120302 | Carry-out only | |
| 58120303 | Chili Stand | |
| 58120304 | Coffee Shop | |
| 58120305 | Delicatessen (eating places) | |
| 58120306 | Drive-in Restaurant | |
| 58120307 | Fast-Food Restaurant, Chain | |
| 58120308 | Fast-Food Restaurant, Independent | |
| 58120309 | Food Bars | |
| 58120310 | Grills (eating places) | |
| 58120311 | Hamburgers stand | |
| 58120312 | Hot dogs stand | |
| 58120313 | Sandwiches and Submarines Shop | |
| 58120314 | Snack Bar | |
| 58120315 | Snack Shop | |
| 58120601 | Pizzeria, Chain | |
| 58120602 | Pizzeria, Independent | |
| Grocery stores | 541101 | Grocery stores |
| 541104 | Food products – retail | |
| 541106 | Grocers – retail | |
| 541107 | Markets – kosher | |
| 541108 | Grocers – ethnic foods | |
| 541109 | Grocers – health foods | |
| Convenience stores | 5331 | Variety Stores |
| 541102 | Convenience stores | |
Occupational Safety and Health Administration. Standard Industrial Classification Manual. United States Department of Labor. https://www.osha.gov/pls/imis/sic_manual.html. Published 2019. Accessed 10/28/2019
The food outlet data was used to construct six measures of food outlet availability within 1km. This distance has been used in previous studies to capture food outlets accessible by walking36–39. In addition to separate counts of fast food restaurants, convenience stores, and grocery stores per 10,000 population, the fast food restaurant and convenience store counts were added together to construct a measure of hypothesized “unhealthy” food outlets. To capture total access to food outlets, the counts of fast food restaurants, convenience stores, and grocery stores were summed. The modified retail food environment index (mRFEI)40,41 was calculated as a measure of the mixed retail food environment. This index represents the percentage of food outlets in a given area that are more likely to sell healthy food and is calculated by dividing the number of grocery stores by the sum of fast food restaurants, convenience stores, and grocery stores.
After examining the distribution of each food outlet measure, fast food restaurants, the sum of fast food restaurants and convenience stores, and the total sum of outlets were categorized into quartiles based on their distribution. Due to the smaller number of convenience and grocery stores, those outlets were categorized into tertiles based on their distribution. The proportion with zero outlets was considered the referent group for all measures. The mRFEI was grouped into four categories: 1) no food outlets, 2) only fast food restaurants or convenience stores, 3) ≤20% of outlets are grocery stores, and 4) 21-100% of outlets are grocery stores.
Covariates
At baseline, information was collected on age, gender, race/ethnicity, marital status, annual income, education level, diabetes status, hypertension status, urinary protein level, and estimated glomerular filtration rate (eGFR) measured using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula 42.
Statistical analysis
Descriptive statistics were calculated for demographic and clinical characteristics, overall and stratified by categories of food outlet density. Characteristics were summarized as mean (± standard deviation) or medians with interquartile range (IQR) for continuous variables, and as frequencies (proportions) for categorical variables. Bivariate comparisons between groups utilized analysis of variance or chi-square tests as appropriate. Natural log transformations were applied to skewed dietary outcomes. Individual linear and logistic regression models were used to evaluate the associations between each measure of food outlet availability and the outcomes (e.g., dietary factors and healthy diet score). Model estimates were compared to multilevel linear regression models with a random intercept and logistic models using an exchangeable correlation structure to account for clustering of participants, but estimates did not substantively differ when using multilevel models. Additionally, there were sparse numbers per cluster, resulting in zero estimates for the random intercept variance in multiple instances. Therefore geometric means with 95% confidence intervals (95% CI), or odds ratios (OR) with 95% CI were estimated from simple linear and logistic regression models after controlling for study center, age (continuous), gender (male/female), race (non-Hispanic white, non-Hispanic black and other), annual income (less than $20,000, $20,000 to $50,000, or greater than/equal to $50,000), education level (less than high school, high school graduate, some college, or college graduate or more), and marital status (never, formerly, or currently married). Post-hoc adjustments for multiple comparisons using Tukey’s test did not substantively change the reported results. Effect modification was evaluated by gender and income by adding a cross-product term between the measure of food outlet density within 1km and the effect modifier of interest to the regression model. A p-value of 0.05 was considered statistically significant when evaluating effect modification. When effect modification was detected, estimates are presented stratified by the effect modifier.
Results
Among the 2,484 participants in our study sample, the median age was 60 years (IQR 52-66) and 54% were male (Table 2). Median dietary sodium intake was 2587 mg per day (IQR 1862-3608), and dietary phosphorous intake was 1053 (IQR 746-1415) mg per day. There was a median of 3 (IQR 1-7) fast food restaurants within 1km of the census block groups, and a median of 5 outlets (IQR 1 to 9) when fast food restaurants and convenience stores were combined into a single measure. Within 1km, there were few grocery stores. Over half (n=1,428; 57.5%) of participants had zero grocery stores within 1km of their census block group.
Table 2.
Baseline demographic characteristics of Chronic Renal Insufficiency Cohort (CRIC) Study participants with available data linkage on food density, n=2,484
| Overall (n=2,484) | |
|---|---|
| Characteristic | n (%) |
| Age, years [median (IQRa)] | 60 (52-66) |
| Gender, Male | 1347 (54.2) |
| Race/ethnicity, White, nHb | 1046 (42.1) |
| Black, nH | 969 (39.0) |
| Other | 469 (18.9) |
| Income | |
| <$20,000 | 908 (36.6) |
| $20,001 - $50,000 | 716 (28.8) |
| >$50,001 | 860 (34.6) |
| Education | |
| Less than HSc | 522 (21.0) |
| HS graduate | 439 (17.7) |
| Some college | 715 (28.8) |
| ≥College graduate | 808 (32.5) |
| Marital status, currently married | 1361 (54.8) |
| Formerly married | 764 (30.8) |
| Never married | 359 (14.4) |
| Medical History | |
| Hypertension | 2148 (86.5) |
| Diabetes mellitus | 1235 (49.7) |
| Cardiovascular disease | 812 (32.7) |
| eGFRd, ml/min per 1.73m2 [mean (SDe)] | 43.6 (14.9) |
| Proteinuria, g/day [median (IQR)]f | 0.19 (0.07-0.96) |
| Food outlets per 10,000 people within 1 kilometer [median (IQR)] | |
| Fast food restaurants | 3 (1-7) |
| Convenience stores | 1 (0-2) |
| Fast food restaurants + convenience stores | 5 (1-9) |
| Grocery stores | 0 (0-1) |
| Total food outlets | 5 (1-10) |
IQR=interquartile range
nH=non-Hispanic
HS=high school
eGFR=estimated glomerular filtration rate (Note, eGFR of 60 or higher is considered to be in the normal range.)
SD=standard deviation
n=2782 overall for 24H Urine Protein (g/24Hours)
Relative to males, a smaller proportion of females lived in areas with zero fast food restaurants (p=0.003) or zero convenience stores (p=0.01) within 1km (Table 3; online supplementary material). Overall, a larger proportion of females than males had access to food outlets, but the food outlets that were most available to females included fast food restaurants and convenience stores. The proportion of participants with access to grocery stores did not differ by gender (p=0.28). Compared to black and other race participants, a larger proportion of white participants had zero fast food restaurants (p<0.0001), zero convenience stores (p<0.0001), and zero grocery stores (p<0.0001) within 1km of the census block group. A large proportion of white (40.3%) and black (43.4%) participants lived in areas with only fast food restaurants and convenience stores within 1km; however, a larger proportion of black and other race participants had access to grocery stores compared to whites. Across strata of income, a larger proportion of people with the highest income had zero fast food restaurants (p<0.0001), convenience stores (p<0.0001), and zero grocery stores (p<0.0001) relative to those who reported lower income. As income increased, the proportion living in areas densely populated with fast food restaurants decreased (p<0.0001). The majority with income under $20,000 per year lived in an environment with many food outlets (p<0.0001), which included a mix of fast food restaurants, convenience stores, and grocery stores.
Table 3.
Demographic characteristics among Chronic Renal Insufficiency Cohort (CRIC) Study participants with complete income data (n=2,484) by categories of food density within one kilometer of census block group at baseline
| Gender | Race/ethnicity | Income | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of outlets within one kilometer | Overall | Male | Female | Black, nHa | White, nH | Other | <$20,000 | $20,001 - $50,000 | >$50,001 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Fast food | Zero | 576 (23.2) | 356 (26.4) | 220 (19.3) | 134 (13.8) | 390 (37.3) | 52 (11.1) | 101 (11.1) | 158 (22.1) | 317 (36.9) |
| 1-3 | 694 (27.9) | 360 (26.7) | 334 (29.4) | 305 (31.5) | 297 (28.4) | 92 (19.6) | 245 (27.0) | 207 (28.9) | 242 (28.1) | |
| 4-7 | 657 (26.5) | 331 (24.6) | 326 (28.7) | 299 (30.9) | 174 (16.6) | 184 (39.2) | 330 (36.3) | 179 (25.0) | 148 (17.2) | |
| 8+ | 557 (22.4) | 300 (22.3) | 257 (22.6) | 231 (23.8) | 185 (17.7) | 141 (30.1) | 232 (25.6) | 172 (24.0) | 153 (17.8) | |
| p-value | 0.0003 | <0.0001 | <0.0001 | |||||||
| Convenience stores | Zero | 994 (40.0) | 574 (42.6) | 420 (36.9) | 258 (26.6) | 593 (56.7) | 143 (30.5) | 247 (27.2) | 250 (35.0) | 497 (57.8) |
| 1-2 | 959 (38.6) | 488 (36.2) | 471 (41.4) | 423 (43.7) | 315 (30.1) | 221 (47.1) | 423 (46.6) | 288 (40.2) | 248 (28.8) | |
| 3+ | 531 (21.4) | 285 (21.2) | 246 (21.7) | 288 (29.7) | 138 (13.2) | 105 (22.4) | 238 (26.2) | 178 (24.8) | 115 (13.4) | |
| p-value | 0.01 | <0.0001 | <0.0001 | |||||||
| Fast food + Convenience stores | Zero | 481 (19.4) | 302 (22.4) | 179 (15.7) | 91 (9.4) | 345 (33.0) | 45 (9.6) | 70 (7.7) | 126 (17.6) | 285 (33.1) |
| 1-4 | 715 (28.8) | 379 (28.2) | 336 (29.6) | 294 (30.3) | 328 (31.4) | 93 (19.8) | 243 (26.8) | 210 (29.3) | 262 (30.5) | |
| 5-9 | 719 (28.9) | 357 (26.5) | 362 (31.8) | 334 (34.5) | 193 (18.4) | 192 (40.9) | 352 (38.8) | 201 (28.1) | 166 (19.3) | |
| 10+ | 569 (22.9) | 309 (22.9) | 260 (22.9) | 250 (25.8) | 180 (17.2) | 139 (29.7) | 243 (26.7) | 179 (25.0) | 147 (17.1) | |
| p-value | 0.0001 | <0.0001 | <0.0001 | |||||||
| Grocery stores | Zero | 1428 (57.5) | 793 (58.9) | 635 (55.9) | 507 (52.3) | 750 (71.7) | 171 (36.5) | 416 (45.8) | 424 (59.2) | 588 (68.4) |
| 1 | 593 (23.9) | 315 (23.4) | 278 (24.4) | 269 (27.8) | 196 (18.7) | 128 (27.3) | 255 (28.1) | 167 (23.3) | 171 (19.9) | |
| 2+ | 463 (18.6) | 239 (17.7) | 224 (19.7) | 193 (19.9) | 100 (9.6) | 170 (36.2) | 237 (26.1) | 125 (17.5) | 101 (11.7) | |
| p-value | 0.28 | <0.0001 | <0.0001 | |||||||
| All food outlets | Zero | 455 (18.3) | 286 (21.2) | 169 (14.8) | 86 (8.9) | 329 (31.5) | 40 (8.5) | 66 (7.3) | 122 (17.0) | 267 (31.0) |
| 1-5 | 801 (32.3) | 433 (32.2) | 368 (32.4) | 322 (33.2) | 372 (35.6) | 107 (22.8) | 269 (29.6) | 231 (32.3) | 301 (35.0) | |
| 6-10 | 646 (26.0) | 313 (23.2) | 333 (29.3) | 305 (31.5) | 174 (16.6) | 167 (35.6) | 314 (34.6) | 187 (26.1) | 145 (16.9) | |
| 11+ | 582 (23.4) | 315 (23.4) | 267 (23.5) | 256 (26.4) | 171 (16.3) | 155 (33.1) | 259 (28.5) | 176 (24.6) | 147 (17.1) | |
| p-value | <0.0001 | <0.0001 | <0.0001 | |||||||
| Modified retail food environment index | Zero | 455 (18.3) | 286 (21.2) | 169 (14.8) | 86 (8.9) | 329 (31.4) | 40 (8.5) | 66 (7.3) | 122 (17.0) | 267 (31.1) |
| FFR+CSb only | 973 (39.2) | 507 (37.7) | 466 (41.0) | 421 (43.4) | 421 (40.3) | 131 (27.9) | 350 (38.5) | 302 (42.2) | 321 (37.3) | |
| GSc: FFR+CS≤0.2 | 716 (28.8) | 381 (28.3) | 335 (29.5) | 314 (32.4) | 206 (19.7) | 196 (41.8) | 338 (37.2) | 198 (27.7) | 180 (20.9) | |
| GS: FFR+CS>0.2 | 340 (13.7) | 173 (12.8) | 167 (14.7) | 148 (15.3) | 90 (8.6) | 102 (21.8) | 154 (17.0) | 94 (13.1) | 92 (10.7) | |
| p-value | 0.001 | <0.0001 | <0.0001 | |||||||
nH=non-Hispanic;
FFR+CS= fast food restaurants and convenience stores;
GS= grocery stores;
Compared to the overall sample, the characteristics of the 1,889 study participants with complete diet data were mostly similar. There were small differences with respect to race/ethnicity, income, and educational attainment. A larger proportion of participants with complete diet data were non-Hispanic white (51.1% vs. 42.1% overall) compared to other race/ethnicity (8.9% vs. 18.9% overall), had at least a college education (38.4% vs. 32.5% overall) relative to a less than high school education (13.4% vs. 21.0% overall), and reported an income level greater than $50,000 per year (40.5% vs. 34.6% overall) compared to those that reported an income less than $20,000 per year (29.3% vs. 36.6% overall). In regards to associations between food outlet availability and dietary characteristics, study participants with complete diet data consumed similar average percentages of calories from saturated fats, carbohydrates, or protein regardless of the numbers or types of food outlets within 1km of their census block group. There were no meaningful differences in the average levels of saturated fat (g/day), calcium (mg/day), sugary beverages (ounces/week) consumed by participants living near different densities of food outlet availability, nor did self-reported intakes of fruits, vegetables, and whole grains differ among groups of participants living near different numbers or categorizations of food outlets (data not shown).
In the individual models for daily caloric intake (kcal/day), phosphorous (mg/day), sodium (mg/day), and cholesterol (mg/day) outcomes, many estimates of consumption levels differed by gender. Gender stratified estimates of average daily intake of calories, phosphorous, sodium, and cholesterol by different categorizations of food outlets are shown in Table 4. Among males, daily caloric intake varied by number of fast food outlets available and exhibited a u-shaped distribution where males living within close proximity to zero fast food outlets and eight or more outlets had the highest average daily caloric intakes (1953 kcal/day vs. 1920 kcal/day). Males living in areas with zero food outlets within 1km had high average levels of sodium and phosphorous consumption (3046 mg/day sodium and 1187 mg/day phosphorous). Females living in areas with increasing numbers of fast food restaurants relative to areas with zero food outlets reported consuming higher average levels of dietary cholesterol (140 mg/day among those with zero restaurants vs. 169 mg/day among those with 4 to 7 restaurants). Among females, daily caloric, sodium, and phosphorous intakes were lowest among those living in zero food outlet areas.
Table 4.
Multivariable adjusteda associations between categories of food density within one kilometer of census block group and dietary characteristics among males and females with complete income and diet data in the CRIC cohort (n=1889)
| Caloric intake (kcal/day) | Phosphorous (mg/day) | Sodium (mg/day) | Cholesterol (mg/day) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of outlets within one kilometer | Male | Female | Male | Female | Male | Female | Male | Female | |
| GMb (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | ||
| Fast food | Zero | 1953 (1837-2077) | 1353 (1261-1451) | 1180 (1106-1259) | 844 (782-909) | 3074 (2877-3286) | 2089 (1935-2255) | 245 (223-268) | 140 (126-155) |
| 1-3 | 1770 (1671-1875)* | 1464 (1381-1552)* | 1106 (1040-1176) | 912 (856-970) | 2903 (2727-3090) | 2255 (2116-2404) | 235 (216-256) | 165 (152-180)* | |
| 4-7 | 1880 (1769-1999) | 1503 (1415-1596)* | 1144 (1072-1221) | 949 (889-1012)* | 2876 (2691-3073) | 2317 (2169-2476)* | 236 (215-258) | 169 (154-185)* | |
| 8+ | 1920 (1803-2046) | 1396 (1304-1495) | 1177 (1100-1258) | 876 (814-943) | 3065 (2862-3282) | 2127 (1974-2292) | 245 (223-269) | 156 (141-173) | |
| p-value | 0.02 | 0.06 | 0.25 | 0.06 | 0.19 | 0.08 | 0.77 | 0.02 | |
| Convenience stores | Zero | 1882 (1785-1986) | 1436 (1359-1518) | 1165 (1101-1232) | 911 (858-967) | 2989 (2822-3167) | 2230 (2098-2370) | 245 (227-265) | 153 (141-167) |
| 1-2 | 1840 (1744-1940) | 1464 (1389-1544) | 1115 (1054-1180) | 913 (862-966) | 2871 (2711-3041) | 2247 (2121-2381) | 226 (209-245) | 166 (154-180) | |
| 3+ | 1907 (1790-2032) | 1401 (1307-1501) | 1174 (1097-1255) | 868 (806-935) | 3085 (2880-3304) | 2129 (1974-2296) | 252 (229-277) | 157 (142-175) | |
| p-value | 0.56 | 0.51 | 0.27 | 0.44 | 0.15 | 0.43 | 0.07 | 0.24 | |
| Fast food + convenience stores | Zero | 1949 (1825-2080) | 1345 (1245-1453) | 1188 (1108-1274) | 846 (779-919) | 3060 (2850-3284) | 2102 (1932-2288) | 245 (222-270) | 137 (122-154) |
| 1-4 | 1820 (1719-1927)* | 1487 (1404-1575)* | 1136 (1070-1207) | 920 (864-978) | 2952 (2775-3141) | 2283 (2143-2431) | 239 (219-260) | 166 (152-181)* | |
| 5-9 | 1849 (1742-1963) | 1458 (1375-1545) | 1122 (1053-1196) | 925 (869-985) | 2870 (2690-3062) | 2243 (2104-2391) | 234 (214-256) | 164 (151-179)* | |
| 10+ | 1910 (1795-2033) | 1409 (1316-1508) | 1166 (1092-1245) | 880 (818-947) | 3041 (2843-3252) | 2148 (1994-2314) | 243 (222-267) | 159 (144-176)* | |
| p-value | 0.20 | 0.11 | 0.46 | 0.21 | 0.37 | 0.27 | 0.86 | 0.02 | |
| Grocery stores | Zero | 1853 (1766-1945) | 1436 (1371-1504) | 1140 (1083-1200) | 898 (855-944) | 2948 (2797-3107) | 2207 (2098-2322) | 234 (218-251) | 157 (147-169) |
| 1 | 1873 (1762-1992) | 1400 (1309-1497) | 1142 (1070-1219) | 869 (809-933) | 3014 (2820-3221) | 2185 (2030-2351) | 239 (219-262) | 163 (147-180) | |
| 2+ | 1922 (1786-2067) | 1501 (1393-1618) | 1177 (1089-1271) | 955 (881-1035) | 2960 (2735-3203) | 2281 (2101-2476) | 255 (229-284) | 163 (146-182) | |
| p-value | 0.65 | 0.31 | 0.74 | 0.16 | 0.81 | 0.68 | 0.35 | 0.75 | |
| All food outlets | Zero | 1941 (1816-2074) | 1344 (1243-1453) | 1186 (1105-1273) | 844 (776-918) | 3055 (2843-3283) | 2081 (1911-2267) | 243 (220-268) | 138 (123-155) |
| 1-5 | 1809 (1712-1912)* | 1456 (1377-1540) | 1121 (1057-1189) | 906 (853-962) | 2938 (2768-3120) | 2247 (2114-2389) | 237 (218-257) | 165 (151-179)* | |
| 6-10 | 1857 (1745-1976) | 1504 (1416-1598)* | 1137 (1065-1215) | 948 (889-1012)* | 2876 (2688-3076) | 2328 (2180-2487)* | 235 (214-258) | 169 (155-185)* | |
| 11+ | 1926 (1810-2050) | 1394 (1304-1491) | 1170 (1095-1250) | 873 (813-938) | 3048 (2849-3261) | 2105 (1956-2265) | 246 (224-270) | 153 (139-170) | |
| p-value | 0.13 | 0.06 | 0.39 | 0.08 | 0.39 | 0.05 | 0.81 | 0.01 | |
| Modified retail food environment index | Zero | 1944 (1819-2077) | 1344 (1243-1453) | 1187 (1106-1273) | 844 (776-918) | 3046 (2835-3272) | 2081 (1910-2266) | 242 (219-267) | 138 (123-155) |
| FFR+CSc only | 1819 (1726-1916)* | 1469 (1397-1544)* | 1123 (1062-1187) | 918 (870-969) | 2905 (2746-3075) | 2248 (2127-2375) | 232 (214-250) | 164 (152-177)* | |
| GSd: FFR+CS≤0.2 | 1917 (1808-2032) | 1414 (1328-1507) | 1176 (1105-1251) | 879 (821-941) | 3058 (2871-3258) | 2154 (2010-2309) | 246 (225-268) | 162 (148-179)* | |
| GS: FFR+CS>0.2 | 1850 (1709-2004) | 1491 (1373-1620)* | 1118 (1028-1217) | 952 (871-1040)* | 2868 (2631-3126) | 2359 (2155-2583)* | 245 (218-276) | 162 (143-183)* | |
| p-value | 0.16 | 0.13 | 0.29 | 0.12 | 0.29 | 0.12 | 0.57 | 0.05 | |
Statistically different p≤0.05 compared to zero outlets
Adjusted for age (continuous years), race/ethnicity (non-Hispanic black, non-Hispanic white, other), income (<$20,000, $20,001 - $50,000, >$50,000), education level (less than high school, high school graduate, some college, college graduate or more), marital status (never, formerly, or currently married), and study center
GM= geometric mean (95% CI: 95% confidence interval)
FFR+CS= fast food restaurants and convenience stores
GS= grocery stores
When the associations between food outlets and dietary characteristics were further evaluated to determine if associations additionally differed by income level, associations among males did not differ by income level (p for interaction 0.10 to 0.98). Among females, some associations appeared to differ by income level. Specifically, the association between availability of food outlets and caloric intake among females differed by income level, particularly in respect to fast food restaurants (p-interaction 0.03), and the modified retail food environment index (p-interaction 0.01). The association between grocery store availability and phosphorous consumption differed by income level among females (p-interaction 0.05). Table 5 shows the adjusted associations between food outlet density with total daily caloric and phosphorous intake among females by income level. Females who reported income levels less than $20,000 and had the highest density of grocery stores consumed higher average daily calories relative to females in the same income group with zero grocery stores. Increased availability of grocery stores was also associated with increased phosphorous consumption among females with incomes less than $20,000.
Table 5.
Income stratified multivariable adjusteda associations between categories of food density within one kilometer of census block group and total caloric intake and daily phosphorous intake with among females with complete income and diet data in the CRIC cohort (n=1889)
| Caloric intake (kcal/day) | Phosphorous (mg/day) | ||||||
|---|---|---|---|---|---|---|---|
| Number of outlets within one kilometer | Income <$20,000 | Income $20,000-$50,000 | Income > $50,000 | Income <$20,000 | Income $20,000-$50,000 | Income > $50,000 | |
| GMb (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | GM (95% CI) | ||
| Fast food | Zero | 1291 (1111-1501) | 1396 (1237-1575) | 1509 (1262-1806) | 812 (693-951) | 857 (754-974) | 946 (774-1157) |
| 1-3 | 1574 (1421-1744)* | 1338 (1204-1486) | 1657 (1396-1967) | 965 (866-1075)* | 813 (727-909) | 1066 (880-1292) | |
| 4-7 | 1648 (1491-1820)* | 1335 (1192-1494) | 1640 (1380-1948) | 1009 (909-1121)* | 842 (747-949) | 1070 (881-1298) | |
| 8+ | 1382 (1214-1573) | 1329 (1191-1483) | 1731 (1435-2088)* | 932 (813-1068) | 771 (686-867) | 1121 (908-1383)* | |
| p-value | 0.01 | 0.89 | 0.21 | 0.11 | 0.50 | 0.12 | |
| Grocery stores | Zero | 1486 (1365-1618) | 1374 (1264-1493) | 1647 (1402-1936) | 928 (850-1014) | 837 (766-914) | 1058 (882-1268) |
| 1 | 1474 (1319-1647) | 1284 (1135-1452) | 1656 (1385-1980) | 911 (811-1022) | 755 (663-860) | 1077 (881-1316) | |
| 2+ | 1767 (1541-2027)* | 1309 (1154-1484) | 1597 (1314-1941) | 1141 (989-1316)* | 810 (708-925) | 1034 (830-1288) | |
| p-value | 0.04 | 0.49 | 0.89 | 0.01 | 0.29 | 0.91 | |
| All food outlets | Zero | 1351 (1112-1641) | 1345 (1181-1530) | 1475 (1229-1770) | 842 (686-1034) | 844 (735-969) | 933 (760-1146) |
| 1-5 | 1517 (1378-1669) | 1408 (1268-1562) | 1633 (1377-1936) | 939 (849-1039) | 838 (750-937) | 1050 (867-1272) | |
| 6-10 | 1696 (1526-1886)* | 1286 (1150-1438) | 1657(1398-1963) | 1030 (921-1152) | 813 (722-916) | 1084 (895-1311)* | |
| 11+ | 1377 (1219-1555) | 1333 (1198-1484) | 1755 (1453-2120)* | 917 (807-1042) | 786 (701-881) | 1110 (898-1373)* | |
| p-value | 0.02 | 0.56 | 0.10 | 0.21 | 0.76 | 0.12 | |
| Modified retail food environment index | Zero | 1350 (1112-1640) | 1349 (1186-1535) | 1465 (1222-1756) | 843 (687-1034) | 842 (734-967) | 931 (759-1142) |
| FFR+CSc only | 1507 (1378-1648) | 1388 (1268-1519) | 1720 (1462-2025)* | 939 (855-1032) | 837 (760-922) | 1110 (924-1333)* | |
| GSd: FFR+CS≤0.2 | 1464 (1313-1631) | 1357 (1214-1516) | 1599 (1344-1904) | 937 (836-1050) | 789 (701-889) | 1025 (843-1248) | |
| GS: FFR+CS>0.2 | 1856 (1604-2147)* | 1175 (1013-1362) | 1584 (1297-1934) | 1120 (961-1305)* | 765 (653-896) | 1049 (838-1313) | |
| p-value | 0.02 | 0.21 | 0.07 | 0.08 | 0.60 | 0.08 | |
Statistically different p<0.05 compared to zero outlets
Adjusted for age (continuous years), race/ethnicity (non-Hispanic black, non-Hispanic white, other), income (<$20,000, $20,001 - $50,000, >$50,000), education level (less than high school, high school graduate, some college, college graduate or more), marital status (never, formerly, or currently married), and study center
GM= geometric mean (95% CI: 95% confidence interval)
FFR+CS= fast food restaurants and convenience stores
GS= grocery stores
A total of 408 (21.6%) participants had a diet score that was considered healthy, and 38.0% (n=155) of those with a healthy diet score lived in areas with only fast food and convenience store options (Table 6; online supplementary material). When odds of having a healthy diet were modeled using logistic regression, food outlet availability did not appear to be strongly associated with odds of having a healthy diet. There was no evidence of effect modification by gender or income level.
Table 6.
Multivariable adjusteda associations between categories of food density within one kilometer of census block group and healthy diet score among participants with complete income and diet data in the CRIC cohort (n=1889)
| Number of outlets within one kilometer | Healthy Diet (Diet score ≥4) | |||
|---|---|---|---|---|
| n (%) | ORb (95% CI) | p-value | ||
| Fast food | Zero | 111 (27.2) | 1.0 (ref) | |
| 1-3 | 104 (25.5) | 0.95 (0.69, 1.29) | 0.73 | |
| 4-7 | 108 (26.5) | 1.35 (0.97, 1.86) | 0.07 | |
| 8+ | 85 (20.8) | 1.08 (0.77, 1.51) | 0.67 | |
| Convenience stores | Zero | 188 (46.1) | 1.0 (ref) | |
| 1-2 | 137 (33.6) | 0.92 (0.71, 1.20) | 0.55 | |
| 3+ | 83 (20.3) | 1.16 (0.84, 1.58) | 0.36 | |
| Fast food + convenience stores | Zero | 103 (25.2) | 1.0 (ref) | |
| 1-4 | 100 (24.5) | 0.73 (0.53, 1.00) | 0.05 | |
| 5-9 | 117 (28.7) | 1.14 (0.82, 1.60) | 0.43 | |
| 10+ | 88 (21.6) | 1.00 (0.71, 1.42) | 0.99 | |
| Grocery stores | Zero | 254 (62.2) | 1.0 (ref) | |
| 1 | 93 (22.8) | 1.00 (0.76, 1.32) | 0.98 | |
| 2+ | 61 (15.0) | 1.11 (0.80, 1.55) | 0.52 | |
| All food outlets | Zero | 99 (24.3) | 1.0 (ref) | |
| 1-5 | 111 (27.2) | 0.70 (0.51, 0.96) | 0.03 | |
| 6-10 | 114 (27.9) | 1.25 (0.89, 1.76) | 0.19 | |
| 11+ | 84 (20.6) | 0.93 (0.65, 1.32) | 0.69 | |
| Modified retail food environment index | Zero | 99 (24.3) | 1.18 (0.87, 1.60) | 0.27 |
| FFR+CSc only | 155 (38.0) | 1.0 (ref) | ||
| GSd: FFR+CS≤0.2 | 117 (28.7) | 1.25 (0.95, 1.66) | 0.12 | |
| GS: FFR+CS>0.2 | 37 (9.1) | 0.81 (0.54, 1.21) | 0.30 | |
Adjusted for age (continuous years), gender (male/female), race/ethnicity (non-Hispanic black, non-Hispanic white, other), income (<$20,000, $20,001 - $50,000, >$50,000), education level (less than high school, high school graduate, some college, college graduate or more), marital status (never, formerly, or currently married), and study center; FFR: fast food restaurant; CS: convenience store; GS: grocery store; UF: unhealthy food; HF: healthy food; OR: odds ratio; 95% CI: 95% confidence interval
OR= odds ratio (95% CI: 95% confidence interval)
FFR+CS= fast food restaurants and convenience stores
GS= grocery stores
Discussion
This study is the first to examine the availability of fast food restaurants, convenience, and grocery stores in a diverse cohort of adults with mild-to-moderate CKD. The results show that residential proximity to food outlets varies by gender, race/ethnicity, and income, and may be most influential on dietary behaviors among females with CKD and low income. Most participants had at least one fast food restaurant or convenience store within one kilometer of their census block group. Contrary to expectation, this study did not show strong trends between access to fast food or convenience stores outlets and unhealthy diet, nor did the study find that access to grocery stores is associated with healthy diet among individuals with CKD. The study did; however, detect patterns with specific nutrients, suggesting that the food environment influences dietary choices. Outlet density by gender interactions suggested differences in patterns of calorie and nutrient consumption that may be important to take into consideration when planning interventions or developing health policies aimed at the neighborhood food environment. A large portion of the work surrounding health policies at the neighborhood level has focused on obesity prevention in the general population43–46. The lack of a direct one-to-one correlation between food environment and diet that can be pooled across the population irrespective of differences by gender or socioeconomic status has implications for healthy living policies and community-level interventions aimed at protecting public health. This is an important consideration that may impact public health initiatives such as those led by the Centers for Disease Control and Prevention (CDC) National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity and Obesity47, which are intended to increase access to healthy food by informing health policies aimed at improving food environments.
Prior studies have evaluated gender differences in dietary intakes, reporting increased energy intake among males compared to females48. In the Framingham Study, larger proportions of females relative to males met dietary recommendations for carbohydrate, saturated fat, and cholesterol consumption49. Gender differences in relation to the association between food outlet access and dietary consumption has not been well described. In this study, males living in zero outlet areas consistently had the highest average intakes of calories, phosphorous, and sodium, which were similar to the levels among males living in areas with eight or more fast food restaurants and opposite of what was observed among females. The average daily sodium intake among males exceeded the recommended level of 2,000 mg50. Females in zero outlet areas consistently had low average intakes for dietary components, with additional differences by income level. Despite recommendations that dietary phosphorous intake be restricted to a maximum of 800 to 1,000 mg/day51, females with higher income levels consumed more phosphorous in areas where the number of fast food outlets were greatest (zero outlets 946 mg/day vs. 8+ fast food outlets 1121 mg/day). This contrasts with females with the lowest income, where the highest intake of phosphorous (1141 mg/day) was among those with access to two or more grocery stores. The diversity of these findings may be an indication that one size fits all neighborhood level interventions or policies aimed at improving dietary practices by restricting fast food outlets or increasing the number of grocery stores need careful evaluation before large scale implementation.
Many food environment studies have examined associations of food outlet density with diet individually, focusing on grocery stores or fast food restaurants in isolation without considering the impact of living in a mixed food environment where access to all of these outlets exists in the same space1,3,6,52. While these studies add valuable information to our understanding of the impact the food environment has on health, understanding the implications of the food environment requires us to consider the context of the mixed food environment. Consistent with other multi-center epidemiologic studies11,34,53, this study examined the associations between dietary factors and a diverse food environment that considered a variety of food outlet sources.
Unlike the Multi-Ethnic Study of Atherosclerosis (MESA) study, in this study there was no evidence of an association between the availability of fast food outlets and the odds of a healthy diet3. This may be due to differences between the study groups, small sample size in our sample due to the applied exclusion criteria, or the different metrics used to measure diet. In the Coronary Artery Risk Development in Young Adults (CARDIA) study, greater access to supermarkets was associated with poor quality diet among high-income women, but better quality diet among low-income men34. In the current study access to a higher number of grocery stores was associated with higher consumption of total calories among female participants with the lowest income level. This discordance may be due to differences in age between the two studies; the average age of participants in this study was more than double that of CARDIA. In the Atherosclerosis Risk in Communities (ARIC) study, increased access to supermarkets was associated with increased fruit and vegetable intake among black and white participants53. The current study did produce evidence to support grocery store access being associated with fruit and vegetable intake or better dietary habits, as the majority of dietary intakes measured did not meaningfully differ according to number of grocery stores. To date, findings from other studies have not consistently supported the hypothesis that increased access to grocery stores and supermarkets is associated with better dietary practices54–57. In the context of CKD, this null finding may be due to differences in eating habits among people with CKD that are independent of food outlet availability, such as recommendations from their health care provider to follow a renal diet.
This study has several limitations. It used an ecological approach linking individual behaviors and outcomes with census block group level food outlets, using the geocoded census block group as a proxy for neighborhood. Participants in this study were not asked about fast food eating behavior or about sources of food and beverage. This study is unable to precisely link proximity to food outlets to individual eating behaviors. The food frequency questionnaire may not accurately capture sodium and phosphorous, and the methodology used to estimate individual nutrients does not capture sodium or phosphorus-based additives such as dicalcium phosphate, sodium aluminum phosphate, or sodium phosphate; therefore, this study may be underestimating true consumption levels. The possibility of measurement error in the food frequency questionnaire, or in the food outlet data source cannot be ruled out. This study assumed that proximity to food outlets could be used to infer patronage at surrounding food outlets due to participants’ ability to walk to outlets; however, neighborhood walkability was not measured nor were individual physical limitations that preclude walking to these outlets considered. The assessment of food outlets only occurred at baseline (2003 to 2008), not accounting for changes in neighborhood outlets over time, nor access to food outlets surrounding work places or other communities that participants may frequent. Fast food restaurants and convenience stores were considered to be sources of unhealthy food, but this study cannot account for healthy items that may have been available at these outlets. Numerous participants did not report their income level or dietary characteristics and were excluded from analyses. Although the participants in this study sample had similar levels of kidney function compared to the overall CRIC cohort, the demographics of these participants may not be completely representative of the overall cohort, as participants who were non-Hispanic white, college educated, and had higher income may be overrepresented related to participants of other race or who had less than a high school education or lower income level. Despite these limitations, the CRIC study data provides a unique opportunity for scientific investigation to better understand how neighborhood level food outlet density impacts diet in a well-defined cohort of people with CKD.
Understanding how food outlet density affects dietary consumption and subsequent health outcomes among people of varying socioeconomic backgrounds living with chronic disease is imperative to our work to protect public health. The results from this study indicate that strategies to increase adherence to a healthy diet must go beyond simply advising people with CKD to avoid purchasing food from fast food restaurants. Future investigations may benefit from combining spatial analysis to determine food outlet availability with questions about dietary consumption behaviors, shopping and dining preferences, and awareness of food and drinks that contain unhealthy additives. Ultimately, awareness of the food outlets available at the neighborhood level provides context into how people with CKD access food and may enhance intervention strategies aimed at improving dietary behaviors to promote health in this growing portion of the population living with chronic disease.
Research Snapshot.
Research Question:
How does neighborhood food outlet access impact dietary intake among people with chronic kidney disease? Do these associations differ by gender or income level?
Key Findings:
A U-shaped pattern was observed among males in relation to total caloric consumption. Having zero food outlets nearby was associated with the highest consumption levels of sodium and phosphorous among males. Among females, living in an area with zero food outlets was associated with the lowest average intake of calories, sodium, and phosphorous. Associations between access to outlets and dietary intakes among females differed by income level. Among low-income females, access to more outlets were associated with higher calorie consumption.
Acknowledgments:
We thank Aster Xiang, GIS specialist for the Weight and Veterans’ Environments Study (R01CA172726), for assistance with construction of the food outlet measures. Jessica Madrigal is a trainee supported by the National Institute for Occupational Safety and Health (NIOSH) fellowship under grant number T42 OH008672. Funding for the CRIC Study was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, and U01DK060902). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/NCATS UL1TR000003, Johns Hopkins University UL1 TR-000424, University of Maryland GCRC M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, University of Illinois at Chicago NIDDK K24-DK092290, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20 GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1 RR-024131. The authors have no conflicts of interest to report, and all people named in these acknowledgements have provided permission to be named.
Sources of Support:
Jessica Madrigal is a trainee supported by the National Institute for Occupational Safety and Health (NIOSH) fellowship under grant number T42 OH008672. Funding for the CRIC Study was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, and U01DK060902). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/NCATS UL1TR000003, Johns Hopkins University UL1 TR-000424, University of Maryland GCRC M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, University of Illinois at Chicago NIDDK K24-DK092290, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20 GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1 RR-024131.
Abbreviations:
- CRIC
Chronic Renal Insufficiency Cohort
- CKD
Chronic kidney disease
- NCI
National Cancer Institute
- D&B
Dun and Bradstreet
- SIC
Standard Industrial Classification
- mRFEI
Modified retail food environment index
- eGFR
Estimated glomerular filtration rate
- CKD-EPI
Chronic Kidney Disease Epidemiology Collaboration
- 95% CI
95% confidence interval
- OR
Odds ratios
- IQR
Interquartile range
- MESA
Multi-Ethnic Study of Atherosclerosis Study
- CARDIA
Coronary Artery Risk Development in Young Adults Study
- ARIC
Atherosclerosis Risk in Communities Study
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publisher's Disclaimer: Disclaimers: none
Contributor Information
Jessica M. Madrigal, Division of Epidemiology and Biostatistics, School of Public Health, University of Illinois at Chicago, Chicago, IL, United States, 1603 W. Taylor Street, Room 911, M/C 923, Chicago, IL 60612.
Esteban Cedillo-Couvert, South Texas Renal Care Group, San Antonio, TX, United States, 215 N. San Saba Street, Ste. 301, San Antonio, Texas 78207.
Ana C. Ricardo, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, United States, 1853 West Polk Street, Room 130 CMW, Mail Code 784, Chicago, IL 60612.
Lawrence J. Appel, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States, Welch Center for Prevention, 2024 E. Monument Street, Room 2-600, Baltimore, Maryland 21287.
Cheryl A. M. Anderson, Department of Family Medicine and Public Health, University of California San Diego School of Medicine, La Jolla, CA, United States, 9500 Gilman Drive La Jolla, California 92093.
Rajat Deo, Department of Medicine, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States, 9 Founders Pavilion, 3400 Spruce Street, Philadelphia, PA 19104.
L. Lee Hamm, Tulane University School of Medicine, New Orleans, LA, United States, 1430 Tulane Avenue, New Orleans, LA 70112.
Denise Cornish-Zirker, University of Michigan, Ann Arbor, MI, United States, Domino Farms Lobby M - Suite 3100, Ann Arbor, MI 48105.
Thida C. Tan, Kaiser Permanente Northern California, Division of Research, 2000 Broadway Oakland, CA 94612.
Daohang Sha, Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States, 8th Floor, Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104-6021.
Jesse Y. Hsu, Center for Clinical Epidemiology and Biostatistics and Department of Biostatistics, Epidemiology, and Informatics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States, 629 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104-6021.
Shannon N. Zenk, Department of Health Systems Science, College of Nursing, University of Illinois at Chicago, 845 S. Damen Ave., Rm. 914, Chicago, IL 60612-7350.
Milda R. Saunders, Section of General Internal Medicine, University of Chicago Medicine, Chicago, IL, United States, 5841 S. Maryland Avenue, MC 2007, Chicago, IL 60637.
Victoria Persky, Division of Epidemiology and Biostatistics, School of Public Health, University of Illinois at Chicago, Chicago, IL, United States, 1603 W. Taylor Street, Room 877, M/C 923, Chicago, IL 60612.
James P. Lash, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, United States, 1853 West Polk Street, CMW, Chicago, IL 60612.
References
- 1.Burgoine T, Forouhi NG, Griffin SJ, Wareham NJ, Monsivais P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ (Clinical research ed). 2014;348:g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornton LE, Bentley RJ, Kavanagh AM. Fast food purchasing and access to fast food restaurants: a multilevel analysis of VicLANES. The international journal of behavioral nutrition and physical activity. 2009;6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR, Franco M. Fast-food consumption, diet quality, and neighborhood exposure to fast food: the multi-ethnic study of atherosclerosis. American journal of epidemiology. 2009;170(1):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritz E, Hahn K, Ketteler M, Kuhlmann MK, Mann J. Phosphate additives in food--a health risk. Deutsches Arzteblatt international. 2012;109(4):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annual review of public health. 2001;22:309–335. [DOI] [PubMed] [Google Scholar]
- 6.Caspi CE, Lenk K, Pelletier JE, et al. Food and beverage purchases in corner stores, gas-marts, pharmacies and dollar stores. Public health nutrition. 2017;20(14):2587–2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleischhacker SE, Evenson KR, Rodriguez DA, Ammerman AS. A systematic review of fast food access studies. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12(5):e460–471. [DOI] [PubMed] [Google Scholar]
- 8.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? The international journal of behavioral nutrition and physical activity. 2006;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Satia JA, Galanko JA, Siega-Riz AM. Eating at fast-food restaurants is associated with dietary intake, demographic, psychosocial and behavioural factors among African Americans in North Carolina. Public health nutrition. 2004;7(8):1089–1096. [DOI] [PubMed] [Google Scholar]
- 10.Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public health nutrition. 2004;7(8):1081–1088. [DOI] [PubMed] [Google Scholar]
- 11.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR Jr. Associations of the local food environment with diet quality--a comparison of assessments based on surveys and geographic information systems: the multi-ethnic study of atherosclerosis. American journal of epidemiology. 2008;167(8):917–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson CA, Nguyen HA, Rifkin DE. Nutrition Interventions in Chronic Kidney Disease. The Medical clinics of North America. 2016;100(6):1265–1283. [DOI] [PubMed] [Google Scholar]
- 13.Kalantar-Zadeh K, Fouque D. Nutritional Management of Chronic Kidney Disease. The New Englandjournal of medicine. 2017;377(18):1765–1776. [DOI] [PubMed] [Google Scholar]
- 14.Chang AR, Anderson C. Dietary Phosphorus Intake and the Kidney. Annual review of nutrition. 2017;37:321–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calvo MS, Uribarri J. Public health impact of dietary phosphorus excess on bone and cardiovascular health in the general population. The American journal of clinical nutrition. 2013;98(1):6–15. [DOI] [PubMed] [Google Scholar]
- 16.Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 1998;31(4):607–617. [DOI] [PubMed] [Google Scholar]
- 17.Kestenbaum B, Sampson JN, Rudser KD, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. Journal of the American Society of Nephrology: JASN. 2005;16(2):520–528. [DOI] [PubMed] [Google Scholar]
- 18.Darmon N, Drewnowski A. Does social class predict diet quality? The American journal of clinical nutrition. 2008;87(5):1107–1117. [DOI] [PubMed] [Google Scholar]
- 19.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li KK, Concepcion RY, Lee H, et al. An examination of sex differences in relation to the eating habits and nutrient intakes of university students. Journal of nutrition education and behavior. 2012;44(3):246–250. [DOI] [PubMed] [Google Scholar]
- 21.Li R, Serdula M, Bland S, Mokdad A, Bowman B, Nelson D. Trends in fruit and vegetable consumption among adults in 16 US states: Behavioral Risk Factor Surveillance System, 1990-1996. American journal of public health. 2000;90(5):777–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimakawa T, Sorlie P, Carpenter MA, et al. Dietary intake patterns and sociodemographic factors in the atherosclerosis risk in communities study. ARIC Study Investigators. Preventive medicine. 1994;23(6):769–780. [DOI] [PubMed] [Google Scholar]
- 23.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. American journal of preventive medicine. 2004;27(3):211–217. [DOI] [PubMed] [Google Scholar]
- 24.Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Advances in chronic kidney disease. 2015;22(1):6–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vart P, Gansevoort RT, Joosten MM, Bultmann U, Reijneveld SA. Socioeconomic disparities in chronic kidney disease: a systematic review and meta-analysis. American journal of preventive medicine. 2015;48(5):580–592. [DOI] [PubMed] [Google Scholar]
- 26.Neugarten J, Acharya A, Silbiger SR. Effect of gender on the progression of nondiabetic renal disease: a meta-analysis. Journal of the American Society of Nephrology : JASN. 2000;11(2):319–329. [DOI] [PubMed] [Google Scholar]
- 27.Neugarten J, Golestaneh L. Gender and the prevalence and progression of renal disease. Advances in chronic kidney disease. 2013;20(5):390–395. [DOI] [PubMed] [Google Scholar]
- 28.Silbiger S, Neugarten J. Gender and human chronic renal disease. Gender medicine. 2008;5 Suppl A:S3–s10. [DOI] [PubMed] [Google Scholar]
- 29.Feldman HI, Appel LJ, Chertow GM, et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and Methods. Journal of the American Society of Nephrology : JASN. 2003; 14(7 Suppl 2):S148–153. [DOI] [PubMed] [Google Scholar]
- 30.Lash JP, Go AS, Appel LJ, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clinical journal of the American Society of Nephrology : CJASN. 2009;4(8):1302–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires : the Eating at America’s Table Study. American journal of epidemiology. 2001;154(12):1089–1099. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 33.Ricardo AC, Anderson CA, Yang W, et al. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2015;65(3):412–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Archives of internal medicine. 2011;1V1(13):1162–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hollands S, Campbell MK, Gilliland J, Sarma S. A spatial analysis of the association between restaurant density and body mass index in Canadian adults. Preventive medicine. 2013;57(4):258–264. [DOI] [PubMed] [Google Scholar]
- 36.Yang Y, Diez-Roux AV. Walking distance by trip purpose and population subgroups. American journal of preventive medicine. 2012;43(1):11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Athens JK, Duncan DT, Elbel B. Proximity to Fast-Food Outlets and Supermarkets as Predictors of Fast-Food Dining Frequency. Journal of the Academy of Nutrition and Dietetics. 2016;116(8):1266–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He M, Tucker P, Gilliland J, Irwin JD, Larsen K, Hess P. The influence of local food environments on adolescents’ food purchasing behaviors. International journal of environmental research and public health. 2012;9(4): 1458–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Larsen K, Gilliland J. Mapping the evolution of ‘food deserts’ in a Canadian city: supermarket accessibility in London, Ontario, 1961-2005. International journal of health geographics. 2008;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention (CDC). Census Tract Level State Maps of the Modified Retail Food Environment Index (mRFEI),. Atlanta, GA: U.S. Department of Health and Human Services;2011. [Google Scholar]
- 41.Greer S, Schieb L, Schwartz G, Onufrak S, Park S. Association of the neighborhood retail food environment with sodium and potassium intake among US adults. Preventing chronic disease. 2014;11:E70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009;150(9):604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khan LK, Sobush K, Keener D, et al. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports. 2009;58(Rr-7):1–26. [PubMed] [Google Scholar]
- 44.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annual review of public health. 2008;29:253–272. [DOI] [PubMed] [Google Scholar]
- 45.Cheadle A, Cromp D, Krieger JW, et al. Promoting Policy, Systems, and Environment Change to Prevent Chronic Disease: Lessons Learned From the King County Communities Putting Prevention to Work Initiative. Journal of public health management and practice : JPHMP. 2016;22(4):348–359. [DOI] [PubMed] [Google Scholar]
- 46.Bowen DJ, Barrington WE, Beresford SA. Identifying the effects of environmental and policy change interventions on healthy eating. Annual review of public health. 2015;36:289–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) National Center for Chronic Disease Prevention and Health Promotion DoN, Physical Activity, . Nutrition: Strategies and Resources. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/nutrition.html Published 2019. Accessed 11/01/2019.
- 48.Rolls BJ, Fedoroff IC, Guthrie JF. Gender differences in eating behavior and body weight regulation. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1991;10(2):133–142. [DOI] [PubMed] [Google Scholar]
- 49.Millen BE, Quatromoni PA, Franz MM, Epstein BE, Cupples LA, Copenhafer DL. Population nutrient intake approaches dietary recommendations: 1991 to 1995 Framingham Nutrition Studies. Journal of the American Dietetic Association. 1997;97(7):742–749. [DOI] [PubMed] [Google Scholar]
- 50.Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Annals of internal medicine. 2013;158(11):825–830. [DOI] [PubMed] [Google Scholar]
- 51.Academy of Nutrition and Dietetics Evidence Analysis Library. 2010 Chronic Kidney Disease (CKD) Evidence-Based Nutrition Practice Guideline. Published 2010; Accessed 01-15-2019, 2019. [Google Scholar]
- 52.Suarez JJ, Isakova T, Anderson CA, Boulware LE, Wolf M, Scialla JJ. Food Access, Chronic Kidney Disease, and Hypertension in the U.S. American journal of preventive medicine. 2015;49(6):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. American journal of public health. 2002;92(11):1761–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. American journal of health promotion : AJHP. 2009;23(4):255–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Elbel B, Mijanovich T, Kiszko K, Abrams C, Cantor J, Dixon LB. The Introduction of a Supermarket via Tax-Credits in a Low-Income Area. American journal of health promotion : AJHP. 2017;31(1):59–66. [DOI] [PubMed] [Google Scholar]
- 56.Rogus S, Athens J, Cantor J, Elbel B. Measuring Micro-Level Effects of a New Supermarket: Do Residents Within 0.5 Mile Have Improved Dietary Behaviors? Journal of the Academy of Nutrition and Dietetics. 2018;118(6):1037–1046. [DOI] [PubMed] [Google Scholar]
- 57.Ghosh-Dastidar M, Hunter G, Collins RL, et al. Does opening a supermarket in a food desert change the food environment? Health & place. 2017;46:249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]


