Abstract
Background
Food preparation interventions are an increasingly popular target for hands-on nutrition education for adults, children and families, but assessment tools are lacking. Objective data on home cooking practices, and how they are interpreted through different data collection methods are needed.
Objective
The goal of this study was to explore the utility of the Healthy Cooking Index in coding multiple types of home food preparation data and elucidating healthy cooking behavior patterns.
Design
Parent-child dyads were recruited between October 2017 and June 2018 in Houston and Austin, Texas for this observational study. Food preparation events were observed and video recorded. Participants also wore a body camera (eButton) and completed a questionnaire during the same event.
Participants/setting
Parents with a school-aged child were recruited as dyads (n=40). Data collection procedures took place in participant homes during evening meal preparation events.
Main outcome measures
Food preparation data were collected from parents through direct observation during preparation as well as, eButton, and paper questionnaires completed immediately after the event.
Statistical analyses performed
All data sets were analyzed using the Healthy Cooking Index coding system, and compared for concordance. A paired sample t-test was used to examine significant differences between the scores. Cronbach’s alpha and principal components analysis (PCA) were conducted on the observed Healthy Cooking Index items to examine patterns of cooking practices.
Results
Two main components of cooking practices emerged from the PCA: one focused on meat products and another on health and taste enhancing practices. The eButton was more accurate in collecting Healthy Cooking Index practices than the self-report questionnaire. Significant differences were found between participant reported and observed summative Healthy Cooking Index scores (p < .001), with no significant differences between scores computed from eButton images and observations (p=.187).
Conclusions
This is the first study to examine nutrition optimizing home cooking practices by observational, wearable camera and self-report data collection methods. By strengthening cooking behavior assessment tools, future research will be able to elucidate the transmission of cooking education through interventions, and the relationships between cooking practices, disease prevention and health.
Keywords: Food preparation, behavior assessment, family meals, cooking
Introduction
Diet is a modifiable risk factor for several major diseases including obesity, diabetes, and cardiovascular disease. 1 Although the United States Department of Agriculture has been issuing dietary recommendations for 40 years 2, adherence to them is low, especially among children. 3 This disconnect highlights the need for practical family interventions that bridge the gap between recommendations and sustainable behavior change. 4,5 As part of this effort, food preparation resources are increasingly part of both academic research and community nutrition interventions.6–8 Cooking classes are delivered in K- 12 education, hospitals, community-based organizations as well as graduate-level medical and dietetics training, highlighting the breadth of investment and interest in cooking as a public health initiative. 6,8,9
Home cooking, as opposed to eating out, has been associated with better diet quality and lower food costs in cross-sectional research. 10–13 Three reviews of experimental cooking interventions reported modest positive impact on adult self-efficacy and diet, and mixed impact on child food-related attitudes and preferences. 6–8 Methodological weaknesses in these studies included evaluation using non-validated metrics. 6–8 Current assessment tools used in cooking program evaluation tend to focus on psychosocial aspects of cooking such as confidence, perceived skills, and attitudes. 14–16 Validations of these self-report tools are typically limited to test-retest and internal consistency reliability of items. 7,17,18 While helpful, it is unclear how well these instruments reflect actual home cooking practices with the potential to impact the nutritional content of meals or downstream biological correlates of health. Thus, the relationship between cooking practices and health outcomes remains in need of further study. 6–8 Given the expansion of cooking interventions across sectors, there is a critical need for novel methods to accurately quantify nutrition optimizing home cooking behaviors.
Direct observation has been used to objectively assess behavior related to cooking such as parent feeding and family meal interactions. 19–21 Observational data may serve as a ground truth measure for behavioral assessment, but requires substantial time and staff resources. Conversely, self-report assessments are relatively inexpensive to conduct and analyze, but often suffer from recall or desirability bias. 22 Further, broad interpretations of cooking practices may result in self-report items that are not clearly operationalized, leading participants to interpret questions using dissimilar criteria.
Novel wearable technologies offer an alternative, and potentially more objective, approach for the evaluation of cooking practices. Although not widely used, wearables may support or supplant self-report tools as this technology becomes lower cost and increasingly automated. 23–25 One such device is the Sun eButton, a passive, chest-worn camera that takes a picture directly in front of the wearer at four-second intervals. 26 The eButton has shown promise in supplementing dietary recall and activity data in controlled settings 27,28, but the ability of the eButton to collect food preparation data in a natural, home setting has not yet been explored.
Existing research on the effectiveness of cooking interventions is limited by lack of 1) a standardized system to quantify nutrition optimizing cooking practices and 2) an understanding of which data collection method accurately captures these practices in the home food environment. The current study utilizes a novel, evidence-based system for quantifying nutrition optimizing home cooking practices, the Healthy Cooking Index (HCI), and explores the utility of this system in coding multiple data types and elucidating relevant behavior patterns. The performance of two data collection methods (the eButton wearable camera and a self-report Healthy Cooking Questionnaire) is compared to observations of a home-based food preparation event as the validation method (Figure 1). Observational data of the event serves as the ground truth measure for independently examining the accuracy of these measures in a family home setting.
Figure 1:
Graphical representa9on of study design and data collec9on method. Each square represents a data collec9on method including observa9on, or ground truth, measure on the far leD; a par9cipant’s percep9on/recall of their own behavior on the top right; and the use of a wearable body camera, eBuIon, on the boIom right. The data collec9on methods on the right were compared to the ground truth assessment on the leD for accuracy.
Materials and Methods
This observational study was conducted between October 2017 and June 2018 in Houston and Austin Texas. Recruitment and data collection were conducted on a rolling basis throughout the study period.
Participants
A convenience sample of 40 parents, with one child aged 5 to 17 years, was recruited. School-aged children were targeted given the likelihood that they still ate evening meals in the home. Paper and digital flyers were used to recruit families over the nine-month study. Parents were told the goal of the study was to better understand family cooking practices and how they can be measured. Inclusion criteria were: child aged 5 – 17 years, parents and children able to speak and read in English, no severe food allergies in the home, and parent reports cooking a meal for the child at least once a week on average. All study procedures took place in the participants’ homes. The University of Texas MD Anderson Cancer Center Institutional Review Board reviewed and approved the protocol (PA16–0995). Families were offered $50 gift cards as compensation at the end of their study participation. Parental consent, permission and child assent were obtained. A total of 80 potential participants responded to recruitment efforts; 8 were deemed ineligible due to food allergies or lack of ability to speak English, 32 declined to participate after learning more about the study details. Main reasons for declining participation included discomfort with being filmed, general disinterest and recovery from recent storm damage that impacted the Houston area two months prior to study initiation.
Study Procedures
The study consisted of five steps including recruitment/prescreening, scheduling the video sessions, conducting video observation sessions, completing questionnaires as well as height/weight measures and compensating. During recruitment, parents completed pre-screening questions to ensure their eligibility, reported their top five most commonly made meals and proposed convenient times and dates for the video observation session in their home. Interested participants were emailed or mailed copies of the informed consent form for their review. Video observation sessions were scheduled for evening meal preparation times at the participant’s convenience, and confirmed one week prior. During confirmation, participants were requested to make one of the common meals noted from the pre-screener or an alternative typical meal of their choice. Prior to arranging the video equipment, participants completed the informed consent process with research staff. All data were collected in homes by specially trained research staff members hereinafter referred to as “observers”.
Video Observation Session
During the observation session, a digital video camera on a tripod was situated to capture the entire kitchen area and to ensure overall practices, environment, and assistance by children or others were adequately captured. Parent participants wore a wireless lapel microphone and explained their actions as they performed them, and also wore the eButton on their shirt collars. One or two observers, expert in nutrition, took notes and asked questions and clarifications as needed. Observer notes included all ingredients and amounts used during the observation. Participants were asked to report the number of servings yielded from each recipe. Self-report questionnaires and anthropometric measurements were completed directly after the recording session in the participant’s home. The participant was compensated for their time and offered kid-friendly recipe cards and nutritional information upon completion of the session as a thank you.
eButton Procedures
The eButton is a wireless camera device worn on the collar or lapel and consists of a camera, 9-axis motion sensor, barometer, temperature sensor, and light sensor (no audio). Data storage (8GB of flash memory) and a lithium-ion battery are built into the unit. 28 The eButton images are encrypted upon being taken, and thereby safely stored until analyzed. During the video observation sessions, eButton units were activated; parents were asked to place the unit on their shirt collar before they began cooking; and to leave the unit on until food preparation was complete. Parents were instructed to remove the eButton if it was uncomfortable or obstructive during cooking, and all issues with the eButton were documented. The eButton images were analyzed using specialized activity categorization software developed for the unit, detailed elsewhere. 26 Briefly, the software allows researchers to view the images in clusters of events. When reviewing the images in the viewer, the researcher cut strings of images into smaller sets and drop image clusters into specified categories. In this study, the categories were set to match a pre-determined coding system of food preparation behavior, the Healthy Cooking Index Score. 29 A single session’s participant images required between fifteen minutes to one hour to analyze. This variability mirrored the range of preparation times of participants (8 to 120 min), and was similar to the time needed to analyze the observational data.
Anthropometric Measures
Height/weight measurements were collected from child participants by study observers on a single occasion. Given the relationship between eating habits and excessive adiposity, these measures were taken to better characterize the study group relative to current overweight/obesity prevalence. Weight was recorded in kilograms (kg) to the nearest single decimal, using the Seca 869 digital scale. Height was recorded in centimeters (cm) to the nearest single decimal using a Seca 0123 stadiometer. Height and weight measures were conducted with shoes, heavy outerwear and large hair accessories removed. Two height and two weight measures were taken for each child and averaged. BMI was calculated according to the formula kg/m2 based on the height and weight measurements, and were compared to Center for Disease Control (CDC) growth charts for children based on age and sex. Children were characterized by BMI into healthy, overweight and obese as per CDC guidelines. 30
Questionnaires
Demographic questionnaires included items on parent age, sex, education, income level, marital status, and child age, race/ethnicity and sex. The Healthy Cooking Questionnaire (HCQ) examined key nutrition optimizing home cooking practices (Table 1) used during the observation session. The HCQ was completed immediately after the food preparation event and items were phrased as “during the observation session did you...”, in order to capture the same practices as the observational and eButton methods. The HCQ items mirrored the HCI coding system described below (Table 1) and also included items regarding usual cooking frequency to better characterize the sample. The HCQ also included questions on number of children and adults for whom the participants cooked during the observation session as well as estimated number of leftovers (as indicated by participant), which were combined to determine meal serving size. These items were used to calculate a total number of servings for the prepared meal, and allowed for the calculation of per serving nutrition information.
Table 1:
Nutrition optimizing cooking practice items and their respective point distribution from the Healthy Cooking Index Codebook
| Item | Description | Points |
|---|---|---|
| Basic Ingredients | Uses only: fresh, dry or frozen fruits or vegetables, grains, legumes, meat, fish and/or milk, salt, spices, and unflavored oilsa | +1 |
| Low Fat Method | Any instance of the following: bake, grill, boil, microwave, steam, slow cook | +1 |
| Measure Fat | Uses measuring spoon or describes measurement of oil or fat used, or does not add any/negligible amount of fat | +1 |
| Measure Salt | Uses measuring spoon or describes measurement of salt or salty seasoning used or adds no/negligible amount of salt or salty seasoning | +1 |
| Fruit & Vegetables | Adds any fresh or frozen (pure / unseasoned / unsweetened) fruits or vegetables | +1 |
| Olive Oil | Uses olive oil | +1 |
| Alliums | Uses garlic, onions, leeks, or shallots in any form (frozen, fresh, powder) | +1 |
| Herbs & Spices | Uses any fresh or dried herbs or spices / salty seasoning mixes (i.e. seasoned salt) are not counted | +1 |
| Citrus | Fresh or concentrated orange, lemon, grapefruit, lime in any form (fruit, juice or zest) | +1 |
| Whole Grains | Brown rice, whole wheat flour/bread, quinoa, oats, corn, farro or other whole grains | +1 |
| Cook with processed foods | Uses any foods that have undergone substantial processing including canned, jarred, or packaged products that are seasoned or sweetened. This includes salad dressings, seasoning mixes, canned soups, bottled sauces, ready to heat meals and side dishes and the like. This does not include minimally processed foods such as tortillas, breads, cheese, sour cream, jarred garlic, unseasoned, unsalted, and unsweetened canned/jarred products. | −1 |
| Deep Fry | Any meal component is fully submerged in hot oil or grease | −1 |
| Red Meat | Uses any beef, lamb, pork, veal | −1 |
| Red Meat at High Temp | Red meat (above) is cooked by boiling, BBQ, grilling, broiling or pan sauté | −1 |
| Red Meat to Well Done | Red meat cooked to well done (no pink in center) and/or dark browned if fried | −1 |
| Sweetener | Adds sugar, honey, agave, stevia or other sweetener while cooking | −1 |
| Animal Fat | Butter, chicken fat, lard, full fat cheese, bacon fat, cream or other animal fat | −1 |
| Processed Meat | Any processed meat including pepperoni, salami, sausage, lunch meat, bacon, or similar | −1 |
| Vegetables with Creamy Sauce | Prepares vegetables with creamy sauce including creamy dressing for salad, cheese sauce or other white sauce | −1 |
Unflavored oils are those extracted from olive, corn, avocado, etc. or a combination. This is in comparison to flavored oils, which may be made through botanical or spice infusion, addition of artificial flavorings, sweeteners or salt.
Healthy Cooking Index
The HCI offers a system for quantifying nutrition optimizing home cooking practices, and was used in this study to independently code the observational, eButton, and self report (HCQ) data sets. The HCI does not represent an exhaustive list of cooking practices, but rather focuses on food preparation practices specified in the extant literature that likely impact the nutritional quality of prepared meals. 29 The HCI is based on a previously published, evidence-based conceptual framework of nutrition optimizing cooking practices. 29 The framework was developed from a systematic literature review of peer-reviewed articles examining food preparation and health across multiple disciplines. Food preparation practices were assembled into five overarching constructs (frequency, techniques/methods, minimal usage, additions/replacements, and flavoring) specified as individual practices. Face validity of the framework was assessed with a focus group of experts. 29 Subsequent community-based participatory cooking classes based on the framework were undertaken to examine the real-world application of framework constructs in diverse communities. 31 The HCI operationalizes this framework into a data coding system. Food preparation behaviors are items in the HCI coding system, with −1 applied to less healthy practices demonstrated and +1 applied to healthier practices demonstrated (Table 1). This point system offers a simple way to calculate a summative HCI score (range = −9 to +10). The +1/−1 rating was used, due to lack of research to inform accurate item weighting.
Research Staff Training
Two observers were trained to conduct the observation sessions and record ingredients used during cooking. A manual of procedures detailing equipment set-up and a script for the video sessions was developed. Two practice sessions were conducted in volunteer homes during evening meal preparation times, during which observers reviewed setting up equipment, taking notes on ingredients and amounts used, and asking volunteer participants script questions for clarification, as necessary. Videos and notes of the practice sessions were reviewed to ensure compliance with manual of procedure guidelines. Inconsistencies between the two observers were discussed and resolved, mediated by the principal investigator when necessary. Two observers were present for 25 percent of the video sessions and agreement between them was high (95%) with regard to ingredients used. A practice height and weight collection was completed by both observers with six volunteers, and calculated BMI measurements were within .12 kg/m2 between the two data collectors.
Two researchers, one present during the observation sessions (an observer) and the other absent, were trained in applying the HCI coding system to the three data types: Observational data (including video and audio), eButton (images only), and HCQ (self-report) data sets. These were independently coded by one researcher. Forty percent of the observational and eButton data sets were coded by both researchers with the HCI as a quality control procedure. Inter-coder reliability as concordance and percent agreement was acceptable: observational data (k = .875, 92.8% agreement), eButton data (k = .775, 89.8% agreement). 32
Statistical Analysis
Participant demographics were analyzed using descriptive statistics. Ingredient and amount information collected by observers during the video observation sessions were analyzed using the Nutrient Data System for Research software Version 2017. 33 The self report, eButton image, and observational data sets were coded separately using the HCI coding system described above. A summative HCI score was calculated from each data set for each participant. As there is limited extant literature on patterns of modern home cooking practices, an exploratory principal components analysis (PCA) 34 was conducted on the observational HCI data to examine the structure of potential interdependencies in cooking behavior that may inform future research. The number of components extracted was based on Cattell’s scree plot. Orthogonal varimax rotation was used to maximize factor loadings and facilitate interpretability of the factors. The Kaiser-Meyer-Olkin (KMO) test was examined to estimate sampling adequacy. The PCA was exploratory and limited by the sample size (n=40, KMO= .489); however this analysis offers a preliminary introduction into the potential inter-relation between observed food preparation practices. Component scores were calculated and Spearman correlation coefficients used to examine total HCI scores, and component scores, relative to meal nutrient compositions. Cronbach’s alpha 35was calculated for the observed summative scores to examine internal consistency of measure.
The eButton and self-reported HCQ data sets were examined for accuracy through comparison to the direct observational data. Independent one-sample t-tests were used to determine differences between the observed, eButton, and self-report data sets and Bland Altman plots constructed to estimate agreement. The Bland Altman approach quantifies the agreement between two paired measurements (in this case observed and either self-reported or ebutton HCI scores) by examining differences between them against their respective means. 36 One researcher reviewed the coded data sets and classified individual HCI items into matches (recorded by both observational and non-observational methods) and non-matches (observed but not captured by the non-observational methods). Totals of each category formed the percentage groups, with the denominator as the sum of all items, as adapted from previous studies. 37. All statistical analysis was conducted in IBM SPSS Statistics Version 24.0. 38
Results
Participants
A total of 40 parent-child dyads completed this study. Participant characteristics are shown in Table 2. The majority of child participants were under 14 years, female and non-Hispanic White or Hispanic. Most parents were highly educated, completing college or post-graduate study, and socioeconomically stable with the majority owning their homes and earning above 60,000 per year (median household income in Houston = $49,399; Austin = $63,717). 39 Although participants made a variety of main dishes during the observation sessions, all fell into eleven distinct categories (Figure 2a), and ranged widely in both overall calorie content per serving and, likewise, in summative HCI score (Figure 2b).
Table 2:
Demographic Characteristics of 40 parent/child dyads participating in in-home cooking behavior observation study in Houston/Austin Texas (10/2017 – 06/2018).
| Child Characteristics %(n) | ||
| Age (years) | 5 to 8 | 42.5 (17) |
| 9 to 13 | 45 (18) | |
| 14 to 18 | 12.5 (5) | |
| Sex | Male | 35 (14) |
| Female | 65 (26) | |
| Child Race / Ethnicity | Non-Hispanic White | 40 (16) |
| Hispanic | 27.5 (11) | |
| Non-Hispanic Black | 17.5 (7) | |
| Other | 10 (4) | |
| Asian | 5 (2) | |
| BMI Classificationa,b | Healthy | 69.2 (27) |
| Overweight | 17.9 (7) | |
| Obese | 12.8 (5) | |
| Parent and Household Characteristics %(n) | ||
| Female | 95 (38) | |
| Education | High School | 2.5 (1) |
| Some College | 15 (6) | |
| Tech School | 2.5 (1) | |
| College Grad | 32.5 (13) | |
| Post Grad | 40 (16) | |
| Other | 7.5 (3) | |
| Marital Statusa | Married | 75 (30) |
| Owns Homea | Yes | 77.5 (31) |
| Annual Household Incomea | < $60,000 | 25 (10) |
| Parent Age in years mean (range) | 39.9 (28 – 56) | |
| # Children in Home mean (range) | 2.28 (1–5) | |
missing (n=1) data point, n=39 tor these variables
overweight = BMI ≥85th percentile by age and sex. Obesity = BMI ≥ 95th percentile by age and sex.
Figure 2:
a)Bar graph showing category of dishes made by participants as percentage of total group, in 11 categories. b) Scheme showing mean (represented by middle circles) and range (represented by whiskers) of total calorie content per serving of prepared meal by category (black) and healthy cooking index score indica9ng the quality of meal preparation behaviors (grey ).
HCI Scores, Component Scores, and Associations with Prepared Meal Nutrient Content
An exploratory PCA of the observed HCI data was conducted in order to better understand how the HCI items were potentially inter-related. Less healthy practice items were reverse coded so all would have the same directionality and indicate a higher score as favorable. A scree plot revealed two main components (Table 3), although 8 components showed Eigenvalues over 1.0. As this analysis was exploratory, several extractions were attempted but more interpretable components were not revealed. One component (Health and Taste Enhancing) was broad, but included adding fruit and vegetables, using alliums, citrus, herbs and spices, whole grains, processed foods, and using deep-frying cooking methods, while avoiding sweeteners and measuring salt (negative correlations). The combination of less healthy and healthier behaviors in this component may potentially be due to the limited sample size or differences in locally perceived healthy practices from guidelines propounded in the research literature. The other component (Meat Focused) included cooking red meat at high temperatures to well-done, using animal fat and processed meat, and measuring fat. Measuring fat may have loaded onto this component as the most common animal fat used in the sample was butter. Modern packaged butter commonly comes in stick form with tablespoon measurements pre-marked on the packaging, thus potentially giving butter-using participants a better sense of fat measurement than those using oil. Using basic ingredients, serving vegetables with creamy sauce and low fat cooking methods did not load on either factor. Using olive oil loaded similarly on both factors.
Table 3:
Rotated Component Matrixa showing two main components of observed cooking behaviors from Principal Component Analysis.
| Component | ||
|---|---|---|
| Healthy Cooking Index Item (Observed) | Health and Taste Enhancing | Meat Focused |
| Add Fruit and Veg | 0.697 | 0.215 |
| Use Alliums | 0.679 | 0.064 |
| Deep Fry | 0.6 | 0.14 |
| Use Citrus | 0.543 | −0.165 |
| Use Herbs and Spices | 0.498 | 0.155 |
| Use Processed Foods | 0.494 | −0.115 |
| Use Whole Grain | 0.482 | −0.201 |
| Add Sweetener | −0.468 | 0.146 |
| Measure Salt | −0.354 | −0.143 |
| Use Red Meat | 0.326 | 0.877 |
| Cook Red Meat at High Temp | 0.107 | 0.845 |
| Cook Red Meat to Well Done | 0.364 | 0.71 |
| Use Animal Fat | −0.235 | 0.499 |
| Use Processed Meat | 0.231 | 0.453 |
| Measure Fat | −0.043 | 0.313 |
| Cook from Basic Ingredients | −0.072 | 0.179 |
| Use Low Fat Methods | 0.016 | −0.068 |
| Use Olive Oil | 0.355 | 0.341 |
| Serve Veg with Creamy Sauce | −0.221 | −0.001 |
| % variance accounted for | 16.89 | 15.31 |
Rotation converged in 3 iterations. Extraction Method: Principal Component Analysis. Rotation Method: Varimax with Kaiser Normalization.
Two component scores were calculated based on the observed HCI item scores for each participant, a “Health and Taste Enhancing” score and a “Meat Focused” score. Component scores and summative HCI scores were compared to the nutrient composition of prepared meals. The saturated fat content of prepared meals was negatively associated with total observed summative HCI score (rs=−315, p=.047) and, unexpectedly, the Meat Focused component score (rs=−.376, p = .017). The Health and Taste Enhancing component score was positively associated with fiber (rs=.435, p=.006), total servings of fruit in meal (rs=.365, p=.02) and servings of whole grains in meal (rs=.374, p=.017). These preliminary correlations provide proof of concept that HCI practices influence meal nutrient composition, highlighting the potential use of the HCI in cooking program curriculum and evaluation development. The Cronbach’s alpha was .628, for the summative HCI score, .383 for the Health and Taste Enhancing score and .749 for the Meat Focused score.
Performance of Self-report and eButton Data Collection Methods
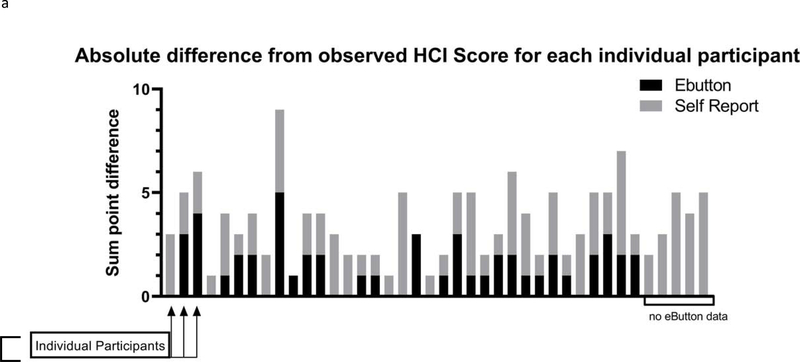
With observation values as the criterion, the eButton was more accurate than the self-report HCQ (Figure 3a–3d) in identifying HCI practices (.40 mean HCI point difference from observed vs −2.15 mean HCI point difference respectively), although both methods reflected some disagreement with the observational data across individual HCI items (Figure 3b).
Figure 3:
Set of schemes depictng differences between observed, eButton and self-report HCI scores. a) Bar graph showing the absolute point difference in summative Healthy Cooking Index score from observed for both self-reported HCQ data (grey ) and eBuIon data ( black); each bar on x-axis represents one individual participant, the five bars on the far right represent participants with missing eButton data. b) Graph showing crosswalk of Healthy Cooking Index behaviors by each data type. Each box represents percentage of participants that demonstrated a behavior by observation/ground truth (white), self report (grey), and eButton (black ). Closer boxes represent more agreement between the three measures. c) Bland Altman plot showing the difference between the observational and eButton summative Healthy Cooking Index Scores and d) the observational and self-report Healthy Cooking Index scores. The horizontal axis represents the average of the scores measured by each method (possible range = −9 to +10). The vertical axis represents the difference between the two measurements. The middle solid line represents the mean difference, the other horizontal lines represent the limits of agreement, defined as the mean difference +/− 1.96 of the standard deviation. The middle dashed line represents the regression of the difference between measures. The two outer slanted grey lines represent the upper and lower bounds of the 95% confidence interval of the regression. Measures repeated at the same point are represented by a single marker. e) the percentage of participants perfectly matching self report and observational HCI scores (far left) or within one, two or three or more points moving from left to right.
eButton vs Observed
Summative HCI scores for observed and eButton data sets were calculated for each participant with usable images (n=35). In five cases, eButton data were not usable. This was due to scrambled images (n=2) or the eButton producing no photos (n = 3). The eButton generally captured fewer HCI practices than the direct observation data; although the majority (77%) of cases showed less than perfect agreement, differences were generally small. A one-sample t-test of differences showed no significant differences between the eButton vs observed HCI scores (t = 1.346, p=.187). A Bland Altman plot (Figure 3c) was constructed and analysis showed a mean difference of .40 index points (95% CI −.21, 1.05) with a SD of 1.973. Thus, virtually all of the paired points were within two index points of the mean score. No significant proportional bias using simple linear regression of the differences between the two paired measurements (r2=.07, SE = 1.817) was found.
Self Report HCQ vs Observed
Differences between self-reported and observed HCI scores were significant, (t = −8.363, p < .001), with a mean difference of −2.15 index points as shown in the Bland Altman plot (Figure 3d). Levels of discordance varied across HCI items (Figure 3b), and in summative scores (Figure 3e) with 30 percent of participants’ self-reporting scores falling within one index point of their observational score; 25 percent falling within two points of their observational score; and 40 percent falling within three or more points different than observed scores. Five percent of self-reported scores were perfect matches with the observational summative HCI score. No significant proportional bias was detected.
To better understand which elements of the HCI were impacting score variability, each item was examined with regard to matches and non-matches between the data sets (Table 4) The eButton had the most error in capturing low fat cooking methods (31% unmatched), processed food usage (34%), measurement of salt (40%) or fat (40%), and use of animal fat (40%) or olive oil (37%). Self-report errors were similar, with larger errors regarding the HCI items processed foods usage (50%), basic ingredients (50%), and measurement of salt (57%) or fat (47%) (Table 4).
Table 4:
Healthy Cooking Index items and the percent matches between observed and eButton / self-reported data as well as self-report intrusions and omissions (Houston/Austin, Texas; 10/2017 – 06/2018).
| Ebutton | Self Report | |||
|---|---|---|---|---|
| Item Content | Match (%) | Match (%) | Intrusiona | Omissionb |
| Deep Fry Method (-) | 100 | 100 | 0 | 0 |
| Used Red Meat (-) | 97 | 98 | 0 | 2 |
| Red Meat at High Temp (-) | 94 | 100 | 0 | 0 |
| Red Meat Well Done (-) | 80 | 85 | 10 | 5 |
| Used Sweetener (-) | 91 | 95 | 3 | 3 |
| Used Processed Meat (-) | 97 | 95 | 0 | 5 |
| Used Processed Foods (-) | 66 | 50 | 3 | 48 |
| Prep Veg w/Creamy Sauce (-) | 74 | 80 | 5 | 15 |
| Used Animal Fat (-) | 60 | 70 | 3 | 28 |
| Measured Salt | 60 | 43 | 58 | 0 |
| Used Alliums | 71 | 95 | 3 | 3 |
| Used Citrus | 89 | 95 | 3 | 3 |
| Used Low Fat Methods | 69 | 93 | 3 | 5 |
| Added Fruit/Veg | 86 | 93 | 0 | 8 |
| Used Olive Oil | 63 | 90 | 5 | 5 |
| Used Whole Grains | 89 | 85 | 8 | 8 |
| Used Herbs and Spices | 86 | 83 | 5 | 13 |
| Measured Fat/Oil | 60 | 53 | 45 | 3 |
| Cooked from Basic Ingredients | 77 | 50 | 50 | 0 |
Intrusion occurs when behaviors are self-reported by participants but not observed by research staff during the event
Omission occurs when behaviors are observed by research staff during event but not self-reported by participants
Self-report non-matches were further examined in terms of intrusions and omissions in order to identify trends in self-reporting errors (Table 4, right side). Unhealthy practices were more likely to be omissions, meaning the practices were observed in the home but were not reported by participants on the HCQ. For healthy practices, errors were more likely to be intrusions, meaning the practices were reported by participants on the HCQ, but not observed during the cooking sessions. This suggests some social desirability bias and/or inappropriate operationalization of the index item.
Discussion
This study examined the quantification of healthy home cooking practices using the HCI across multiple data collection methods. The accuracy of self-report (HCQ) and wearable camera (eButton) data collection methods were assessed against recorded audio/visual observations of meal preparation events in 40 parent-child dyads. The eButton was more accurate, with no significant difference between HCI scores computed from unit images and observations. The self-report data had significant differences between participant reported and observed summative HCI scores and more error by item.
The structure of the relationships among cooking practices is poorly understood, and has not been the subject of current nutrition research. Two main components, or patterns, of cooking practices were determined by the exploratory PCA: one focused on meat products and another on health and taste enhancing practices. Doing a behavior from one component implied a higher likelihood of doing another behavior within the component, and not doing a behavior from the other component. Fiber and whole grain content was positively associated with higher Health and Taste Enhancing scores, which was expected. Saturated fat content was negatively associated with Meat Focused scores, which was unexpected but may potentially be due to the use of leaner red meats by the sample. The Cronbach’s alpha scores, indicators of internal consistency and reliability, were modest. This was expected as the HCI measures represented meal preparation behaviors, not latent psychosocial constructs such as confidence in preparing meals. 35 Although these analyses were exploratory, they do provide preliminary unique insight into the potential inter-relatedness of cooking practices, which, like dietary practices, do not function independently. These PCAs will need to be replicated with larger data sets. 40
One of the main sources of self-reporting error was participant interpretation of terms including “basic ingredients” and “processed foods”, which are not well defined in the current literature. 41 These two items measure a related construct, the use of processed versus non-processed foods, with slight variability in definition (Table 1). Despite the inclusion of definitions and examples on the HCQ, approximately half of participants misreported cooking from basic ingredients and processed food usage. The term “basic ingredients” has variability in meaning, even with a definition provided. Likewise, processed foods exist on a spectrum that may make it difficult for home cooks to report overall usage. The NOVA system offers a method for categorizing processed foods, and helped inform the definitions used in this study. 42However, the NOVA is typically used to code dietary recalls. It remains unclear how to modern home cooks interpret these processed food categories without the use of a full dietary recall. Qualitative and survey studies on the concept of “basic ingredients” and “from scratch” cooking have shown variability in personal definitions of scratch versus processed ingredients. 41,43,44 Despite this inconsistency, many existing evaluations of cooking behavior rely on items examining “from scratch” or “basic ingredients”, often with minimal definition provided. 6,45 These terms need to be clearly defined for participants if used in cooking evaluation. In order for the HCI to be used to evaluate self-reported behavior, alternative question structures regarding basic ingredients and processed foods will need to be developed with end-users and carefully pilot tested in a larger population.
Assessment tools of home cooking behavior have been lacking, leading to variability in cooking program evaluation and, in turn, challenging attempts to compare findings in this growing area of research. 6,7 Robust measures of cooking behavior should be both valid and equivalent in multiple contexts 46,47, yet existing assessment tools of cooking behavior have relied on test-retest reliability and internal consistency of self-report for validation. 15,16,48 To our knowledge, this is the first study to assess the accuracy of a cooking assessment tool relative to a ground truth measure (observed audio/wide angle video of cooking practices).
Participant reported HCI practices revealed significant error when compared to observations of home cooking events. This discord may be due to the fact that cooking is a multi-faceted behavior that lacks a universal definition, and may vary considerably in practice. 41,44 It is worth noting that the self-report was conducted right after the meal preparation performance without time for memory to decay. In dietary assessment, error is greater as time from the event increases, further highlighting the need for improvement in self-report tools in this area. 49 Future self-report tools should avoid overly broad items, which are difficult to interpret during analysis given the diversity of participant experience in food preparation. Further, self-report assessments must consider participant socio-ecological context when operationalizing items (e.g. regional/cultural food nomenclature). The eButton image data were reasonably close, but not perfectly matched, with the observational data. Given the eButton’s ability to approximate video camera type observational data, low resistance to using the technology among parents, and the modest amount of time needed to process the images per participant (15 to 60 minutes), the eButton could be utilized as a primary data collection method or to evaluate self-report items relative to demonstrated home practices.
Limitations to this study include the limited sample size and use of a convenience sample that was predominantly female and of high socioeconomic status. Age ranges and inclusion criteria were kept broad to maximize recruitment potential for this study. This study did not have adequate power to examine reporting errors by demographic characteristics, or cooking scores by demographics or child BMI status. Future research with larger, demographically diverse populations will help elucidate factors that may influence HCI behaviors and reporting. The PCA was limited by sample size. Future studies should consider conducting PCA with larger samples of preferably observed or eButton (i.e. minimal error) data. In-home observations may have influenced usual food preparation practices and multiple, concurrent data collection procedures may have impacted participant recall and eButton usage. Even with observer instruction, five out of 40 participants produced unusable eButton data. This could be problematic as researchers will likely want to capture multiple days of cooking in the home environment. Unfortunately, it is not possible to determine if the eButton collects usable images until they are downloaded for analysis. Finally, individual HCI item matching was conducted by a single researcher and the HCI itself only measures a specific set of possible food preparation practices. Together, these issues limit the generalizability of results.
This work provides a baseline for the further development of tools to assess family cooking habits, and evaluate cooking interventions. This is the first study of which we are aware to compare self-reported and wearable camera data to observational cooking behavior data collected directly from family homes. This offers a new perspective on existing research on the subject, which has, up to this point, depended on focus groups and/or exploratory surveys. 41,50
Conclusions
Novel findings were obtained regarding nutrition optimizing home cooking practices that support the development of more robust cooking program evaluation tools. The eButton demonstrated potential as an accurate primary or reference measure of home cooking behaviors. As wearable technology further develops, automatic identification of food preparation practices may be wired into image-analyzing software to increase the wider utility of these devices in research and community program evaluation. Although the self-report questionnaire, HCQ, showed significant error compared to observational data, this analysis offers insight into the underlying social desirability and reporting issues which may guide an improved self-report assessment tool. Tools based on the HCI will enable future researchers to elucidate the transmission of cooking education through interventions, and the relationships between cooking practices, disease prevention and health.
Research Snapshot.
Research Question
How can the Healthy Cooking Index be used to quantify different types of home food preparation data and are there patterns of healthy cooking behaviors among parents of school-aged children in Houston/Austin, Texas?
Key Findings
In this study, the Healthy Cooking Index was used to examine self-report, wearable camera, and observational data collected from 40 in-home food preparation events. Summative Healthy Cooking Index Scores were significantly different between the self-report and observational data, but not between the wearable camera and observational data. Two distinct patterns of index practices were observed, “Health and Taste Enhancing” and “Meat Focused”; these summative component scores were associated with the nutritional composition of prepared meals.
Acknowledgements
We would like to acknowledge all participants that took part in this research. We would also like to acknowledge Dr. Michael Roth, Grace Yang, Allison Marshall, Emily Kelly and Mike Pomeroy, who assisted with study recruitment and data collection.
Funding / Financial Disclosures: This research was funded by a grant from the National Institutes of Health, National Cancer Institute (5 R21 CA172864) (R01CA165255) (R25CA057730) and Cancer Center Support Grant (P30-CA16672); National Heart, Lung and Blood Institute (U01HL91736); institutional support from the U.S. Department of Agriculture, Agricultural Research Service (Cooperative Agreement 58-3092-5-001); the MD Anderson Center for Energy Balance in Cancer Prevention and Survivorship, and the James and Lois Archer Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest Disclosures:
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Margaret Raber, Department of Pediatrics Research, University of Texas MD Anderson Cancer Center, Box 853, 1515 Holcombe, Houston, TX, 77030.
Tom Baranowski, Department of Pediatrics, USDA/ARS Children’s Nutrition Research Center, Baylor College of Medicine, 1100 Bates St, Houston, TX, 77030.
Karla Crawford, Department of Pediatrics Research, University of Texas MD Anderson Cancer Center, Box 853, 1515 Holcombe, Houston, TX, 77030.
Shreela V. Sharma, Department of Epidemiology University of Texas School of Public Health, 1200 Pressler Dr, Houston, TX, 77030.
Vanessa Schick, Department of Community Health Practice, University of Texas School of Public Health, 1200 Pressler Dr, Houston, TX, 77030.
Christine Markham, Department of Health Promotion and Behavioral Science, 7000 Fannin, Houston, TX, 77030.
Wenyan Jia, Department of Neurological Surgery, University of Pittsburgh, UPMC Presbyterian, Suite B-400, 200 Lothrop Street, Pittsburgh, PA 15213.
Mingui Sun, Department of Neurological Surgery, University of Pittsburgh, UPMC Presbyterian, Suite B-400, 200 Lothrop Street, Pittsburgh, PA 15213.
Emily Steinman, Department of Pediatrics Research, University of Texas MD Anderson Cancer Center, Box 853, 1515 Holcombe, Houston, TX, 77030.
Joya Chandra, Department of Pediatrics Research, University of Texas MD Anderson Cancer Center, Box 853, 1515 Holcombe, Houston, TX, 77030.
References:
- 1.Micha R, Kalantarian S, Wirojratana P, et al. Estimating the global and regional burden of suboptimal nutrition on chronic disease: Methods and inputs to the analysis. European journal of clinical nutrition. 2012;66(1):119–29. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Dietary guidelines for americans 2015–2020. Skyhorse Publishing Inc.; 2017. [Google Scholar]
- 3.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. Journal of the Academy of Nutrition and Dietetics. 2016;116(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun Y, You W, Almeida F, Estabrooks P, Davy B. The effectiveness and cost of lifestyle interventions including nutrition education for diabetes prevention: A systematic review and meta-analysis. Journal of the Academy of Nutrition and Dietetics. 2017;117(3):404–421. e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiMaria-Ghalili RA, Mirtallo JM, Tobin BW, Hark L, Van Horn L, Palmer CA. Challenges and opportunities for nutrition education and training in the health care professions: Intraprofessional and interprofessional call to action. Am J Clin Nutr. 2014;99(5 Suppl):1184S–93S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reicks M, Kocher M, Reeder J. Impact of cooking and home food preparation interventions among adults: A systematic review (2011–2016). Journal of nutrition education and behavior. 2017. [DOI] [PubMed] [Google Scholar]
- 7.Reicks M, Trofholz AC, Stang JS, Laska MN. Impact of cooking and home food preparation interventions among adults: Outcomes and implications for future programs. J Nutr Educ Behav. 2014;46(4):259–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hersch D, Perdue L, Ambroz T, Boucher JL. The impact of cooking classes on food-related preferences, attitudes, and behaviors of school-aged children: A systematic review of the evidence, 2003–2014. Preventing chronic disease. 2014;11:E193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polak R, Phillips EM, Nordgren J, et al. Health-related culinary education: A summary of representative emerging programs for health professionals and patients. Global Advances in Health and Medicine. 2016;5(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiwari A, Aggarwal A, Tang W, Drewnowski A. Cooking at home: A strategy to comply with US dietary guidelines at no extra cost. Am J Prev Med. 2017;52(5):616–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolfson JA, Bleich SN. Fruit and vegetable consumption and food values: National patterns in the united states by supplemental nutrition assistance program eligibility and cooking frequency. Prev Med. 2015;76:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Archuleta M, Vanleeuwen D, Halderson K, et al. Cooking schools improve nutrient intake patterns of people with type 2 diabetes. J Nutr Educ Behav. 2012;44(4):319–25. [DOI] [PubMed] [Google Scholar]
- 13.Chen RC, Lee MS, Chang YH, Wahlqvist ML. Cooking frequency may enhance survival in Taiwanese elderly. Public Health Nutr. 2012;15(7):1142–9. [DOI] [PubMed] [Google Scholar]
- 14.Utter J, Larson N, Laska MN, Winkler M, Neumark-Sztainer D. Self-perceived cooking skills in emerging adulthood predict better dietary behaviors and intake 10 years later: A longitudinal study. Journal of nutrition education and behavior. 2018;50(5):494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lahne J, Wolfson JA, Trubek A. Development of the cooking and food provisioning action scale(CAFPAS): A new measurement tool for individual cooking practice. Food Quality and Preference. 2017;62:96–105. [Google Scholar]
- 16.Lavelle F, McGowan L, Hollywood L, et al. The development and validation of measures to assess cooking skills and food skills. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartmann C, Dohle S, Siegrist M. Importance of cooking skills for balanced food choices. Appetite. 2013;65:125–131. [DOI] [PubMed] [Google Scholar]
- 18.Laska MN, Larson NI, Neumark-Sztainer D, Story M. Does involvement in food preparation track from adolescence to young adulthood and is it associated with better dietary quality? findings from a 10-year longitudinal study. Public Health Nutr. 2012;15(07):1150–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tovar A, Vaughn AE, Fallon M, et al. Providers’ response to child eating behaviors: A direct observation study. Appetite. 2016;105:534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moens E, Braet C, Soetens B. Observation of family functioning at mealtime: A comparison between families of children with and without overweight. J Pediatr Psychol. 2006;32(1):52–63. [DOI] [PubMed] [Google Scholar]
- 21.Hughes SO, Patrick H, Power TG, Fisher JO, Anderson CB, Nicklas TA. The impact of child care providers’ feeding on children’s food consumption. J Dev Behav Pediatr. 2007;28(2):100–107. [DOI] [PubMed] [Google Scholar]
- 22.Schoeller DA. Limitations in the assessment of dietary energy intake by self-report. Metab Clin Exp. 1995;44:18–22. [DOI] [PubMed] [Google Scholar]
- 23.Stumbo PJ. New technology in dietary assessment: A review of digital methods in improving food record accuracy. Proc Nutr Soc. 2013;72(01):70–76. [DOI] [PubMed] [Google Scholar]
- 24.Boushey CJ, Kerr DA, Wright J, Lutes KD, Ebert DS, Delp EJ. Use of technology in children’s dietary assessment. Eur J Clin Nutr. 2009;63:S50–S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gemming L, Utter J, Mhurchu CN. Image-assisted dietary assessment: A systematic review of the evidence. Journal of the Academy of Nutrition and Dietetics. 2015;115(1):64–77. [DOI] [PubMed] [Google Scholar]
- 26.Sun M, Burke LE, Baranowski T, et al. An exploratory study on a chest-worn computer for evaluation of diet, physical activity and lifestyle. J Healthc Eng. 2015;6(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beltran A, Dadabhoy H, Chen T, et al. Adapting the eButton to the abilities of children for diet assessment. Proceedings of Measuring Behavior 2016 – 10th International Conference on Methods and Techniques in Behavioral Research, May 25–27, 2016 2016:72–81. [PMC free article] [PubMed] [Google Scholar]
- 28.Sun M, Fernstrom JD, Jia W, et al. A wearable electronic system for objective dietary assessment. J Am Diet Assoc. 2010;110(1):45–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raber M, Chandra J, Upadhyaya M, et al. An evidence-based conceptual framework of healthy cooking. Preventive Medicine Reports. 2016;4:23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for disease control and prevention 2000 growth charts for the united states: Improvements to the 1977 national center for health statistics version. Pediatrics. 2002;109(1):45–60. [DOI] [PubMed] [Google Scholar]
- 31.Raber M, Crawford K, Chandra J. Healthy cooking classes at a children’s cancer hospital and patient/survivor summer camps: Initial reactions and feasibility. Public Health Nutr. 2017;20(9):1650–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McHugh ML. Interrater reliability: The kappa statistic. Biochemia medica. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 33.Center NC. Nutrition data system for research (NDSR) software. University of Minnesota: Minneapolis, MN, USA: 2017. [Google Scholar]
- 34.Jolliffe I Principal component analysis. Springer; 2011. [Google Scholar]
- 35.Tavakol M, Dennick R. Making sense of cronbach’s alpha. International journal of medical education. 2011;2:53–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giavarina D Understanding bland altman analysis. Biochemia medica: Biochemia medica. 2015;25(2):141–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baranowski T, Islam N, Baranowski J, et al. Comparison of a web-based versus traditional diet recall among children. J Acad Nutr Diet. 2012;112(4):527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.IBM Corp. SPSS statistics for windows, version 24.0. armonk, NY. 2016;24.0. [Google Scholar]
- 39.U.S. Census Bureau. American fact finder. http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Updated 2016.
- 40.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: Policy and environmental approaches. Annual review of public health. 2008;29:253–72. [DOI] [PubMed] [Google Scholar]
- 41.Wolfson JA, Bleich SN, Smith KC, Frattaroli S. What does cooking mean to you?: Perceptions of cooking and factors related to cooking behavior. Appetite. 2016;97:146–154. [DOI] [PubMed] [Google Scholar]
- 42.Monteiro CA, Cannon G, Moubarac J, Levy RB, Louzada MLC, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavelle F, McGowan L, Spence M, et al. Barriers and facilitators to cooking from ‘scratch’using basic or raw ingredients: A qualitative interview study. Appetite. 2016;107:383–391. [DOI] [PubMed] [Google Scholar]
- 44.Wolfson JA, Smith KC, Frattaroli S, Bleich SN. Public perceptions of cooking and the implications for cooking behaviour in the USA. Public Health Nutr. 2016;19(09):1606–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Condrasky MD, Williams JE, Catalano PM, Griffin SF. Development of psychosocial scales for evaluating the impact of a culinary nutrition education program on cooking and healthful eating. J Nutr Educ Behav. 2011;43(6):511–6. [DOI] [PubMed] [Google Scholar]
- 46.Gleason PM, Harris J, Sheean PM, Boushey CJ, Bruemmer B. Publishing nutrition research: Validity, reliability, and diagnostic test assessment in nutrition-related research. J Am Diet Assoc. 2010;110(3):409–419. [DOI] [PubMed] [Google Scholar]
- 47.Frongillo EA, Baranowski T, Subar AF, Tooze JA, Kirkpatrick SI. Establishing validity and cross-context equivalence of measures and indicators. Journal of the Academy of Nutrition and Dietetics. 2018. [DOI] [PubMed] [Google Scholar]
- 48.Flego A, Herbert J, Waters E, et al. Jamie’s ministry of food: Quasi-experimental evaluation of immediate and sustained impacts of a cooking skills program in australia. PloS one. 2014;9(12):e114673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shim J, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiology and health. 2014;36:e2014009; e2014009–e2014009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murray DW, Mahadevan M, Gatto K, et al. Culinary efficacy: An exploratory study of skills, confidence, and healthy cooking competencies among university students. Perspect Public Health. 2016;136(3):143–151. [DOI] [PubMed] [Google Scholar]