Abstract
AIM
To investigate the outcomes of adaptive conjunctival flap advancement surgical techniques with or without scleral graft for patients undergoing revision surgery after trabeculectomy.
METHODS
This retrospective study included 28 eyes of 28 subjects from December 2015 to April 2018. A group of 15 eyes underwent conjunctival advancement only while the other 13 eyes did conjunctival advancement with partial thickness scleral graft. In both study groups, we considered the intraocular pressure (IOP) as our primary outcome and visual acuity (VA) as our secondary outcome. Both were assessed pre- and post-operatively till the last follow-up possible point. Additionally, we classified the patients according to complete and qualified success criteria.
RESULTS
The mean age of the conjunctival advancement group was 36.87±19.25y, while it was 44.08±18.04 in the other group. In both study groups, the mean IOP significantly increased after revision surgery at 1, 2, 3mo and the last follow-up visit when compared to prior the surgery (P<0.001). Moreover, VA was significantly improved (P=0.03) in the final follow-up for both surgical techniques. When we compared the change from baseline in both groups, there was no significant difference between IOP improvement in 1mo (P=0.263), while the difference was significant in 2mo (P=0.03), 3mo (P=0.02) and in the final follow-up visit postoperatively. However, this difference was not significant regarding VA (P=0.5).
CONCLUSION
The both adaptive techniques of conjunctival advancement and conjunctival advancement with scleral graft are effective for treating patients with late-onset hypotony. Yet, more prospective studies are needed to assert upon these results.
Keywords: trabeculectomy, scleral melting, revision surgery, hypotony maculopathy
INTRODUCTION
Trabeculectomy has been regarded the dark horse for surgical management of glaucoma maintaining more than 50% of all the surgical procedures that are used in glaucoma treatment since its introduction in 1968; being a relatively easy and short procedure that is showing efficacy, cost-effectiveness as well as long-term intraocular pressure (IOP) control[1]–[2]. However, there are many limitations for trabeculectomy that make ophthalmologists seek a better surgical procedure. Among those, scarring and bleb failure are the most common postoperative complications. Introduction of the antimetabolites, namely mitomycin C and 5-fluorouracyl, to the world of glaucoma was associated with increased success rate in IOP control with the enhancement of postoperative sight-threatening complications namely bleb leakage, blebitis which can lead to endophthalmitis[3]–[8]. Hypotony is usually defined as an IOP of 5 mm Hg or less. Hypotony can lead to severe visual impairment from hypotonic maculopathy, accelerated cataract formation, corneal decompensation and associated retinal, choroidal and corneal folds[3]–[15]. In addition to visual symptoms, the patients usually suffer from ocular discomfort. Clinically significant changes occur more frequently as the IOP approaches 0.
The best management of postoperative hypotony should consider repairing leaks and hypotony while preserving filtration function and maintaining the target IOP. Achieving this goal is a complete success. However, reaching the goal with the aid of medications or other surgical procedures is still a success that is qualified. Several medical and surgical techniques have been used to try to decrease the late excessive bleb leakage and hypotony. In mild cases, measures such as acetazolamide, trichoracetic acid, cryotherapy, argon laser or injection of autologous blood can be helpful but in more advanced stages, surgical measures are mainly needed[11],[16]–[18].
The main surgical techniques used in literature include conjunctival advancement with or without excision of the pre-existing bleb, free conjunctival or amniotic membrane grafts scleral flap re-suturing, patch grafting with donor pericardium or sclera, placement of compression sutures and trans-conjunctival suturing of the scleral flap. The best surgical intervention should treat the problem of hypotony with bleb leakage while maintaining a good control of IOP as well as the anatomical configuration of the bleb[19]–[27]. Conjunctival advancement flaps as well as scleral grafts are among the commonest surgical interventions used in Egypt to treat hypotony from late bleb leakage. This is due to the ease of material availability and the cost-effectiveness of the procedure. Therefore, in this study, we aimed to assess the IOP and visual acuity (VA) changes after adaptive conjunctival advancement flap alone or with scleral graft for patients undergoing revision surgery after trabeculectomy.
SUBJECTS AND METHODS
Ethical Approval
All procedures performed in studies were in accordance with the ethical standards of Alexandria Faculty of Medicine Research Committee (No.0303979) and with the 1964 Helsinki declaration and its later amendments. Patients signed an informed consent for the surgery after being informed about the surgical procedure in details. Moreover, the patient's data remained anonymous for analysis.
This was a retrospective interventional clinical study that included all patients who underwent conjunctival advancement surgery alone or a combined conjunctival advancement surgery with scleral graft to treat bleb leaks or hypotony after trabeculectomy during the period from December 2015 to April 2018. We excluded cases with VA of no perception of light and cases of active endophthalmitis or any other case who underwent a different procedure other than the two techniques described in this study or performed with another surgeon. The first group included 15 eyes of patients who underwent conjunctival advancement alone while the second group included 13 eyes of patients who underwent a combined conjunctival advancement with partial scleral graft. All of the cases who underwent partial scleral graft had a degree of scleral melting with uveal tissue exposure. One author (Elhofi AS) performed the surgeries and both authors (Elhofi AS, AbouSamra A) shared the follow up.
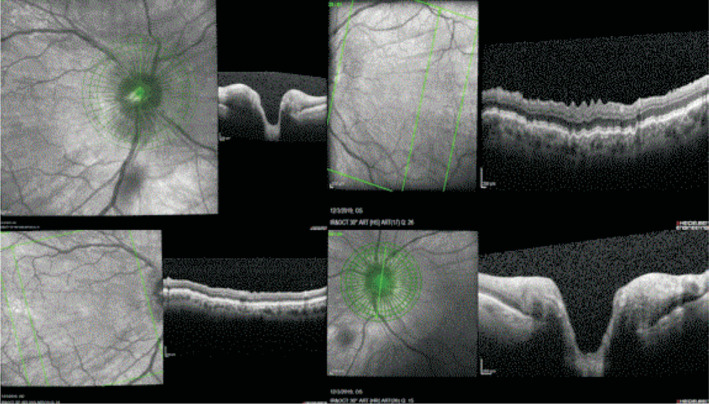
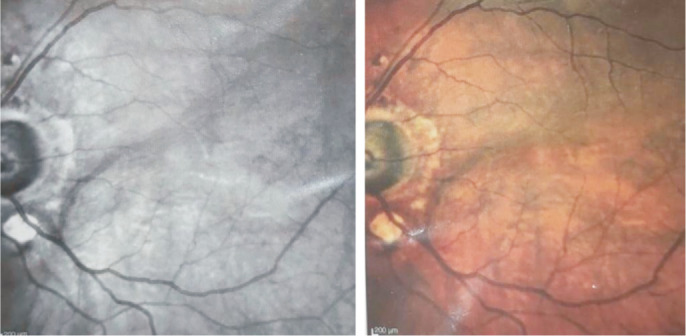
The medical records were revised to obtain a detailed medical history for all patients involved in the study. The ophthalmological examination sheets of patients were obtained and essential data were recorded. Those included the best corrected VA being recorded using logMAR, any important information regarding anterior segment, posterior segment examination as well as IOP measurement using the Goldman's applanation tonometry. Signs of hypotony and blebitis were recorded. Blebitis was considered with or without bleb leakage with conjunctival or ciliary injections or necrotized conjunctiva. Hypotony was considered when there was low pressure (IOP ≤5 mm Hg) in an eye with pathologic functional (decrease in VA) and/or structural changes (corneal folds, flat anterior chamber, macular or choroidal striae, choroidal detachment, optic disc edema or decrease of axial bulbus length). For the enrolled eyes, slit lamp biomicroscopy was done in all patients involved in the study while macular imaging with optical coherence tomography (OCT) was done in three patients only to confirm hypotonic maculopathy (Figures 1–3). Ultrasound biomicroscopy (UBM) was done for only one patient (Figure 4).
Figure 1. OCT of the optic disc and retina for the right and left eyes with OCT of the retina showing retinal folds denoting hypotony.
Figure 3. OCT findings of left hypotony maculopathy with retinal folds.
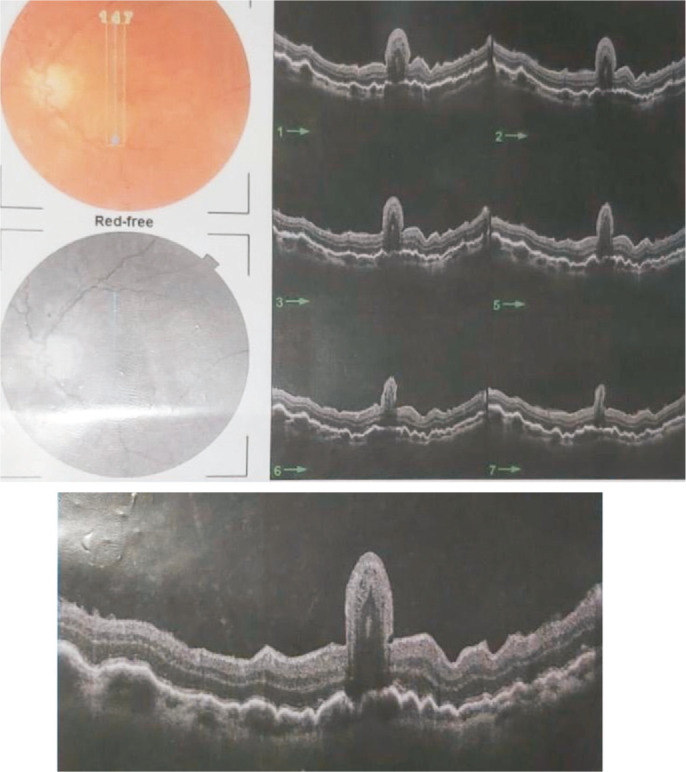
Figure 4. UBM for only one patient showing edematous cornea.
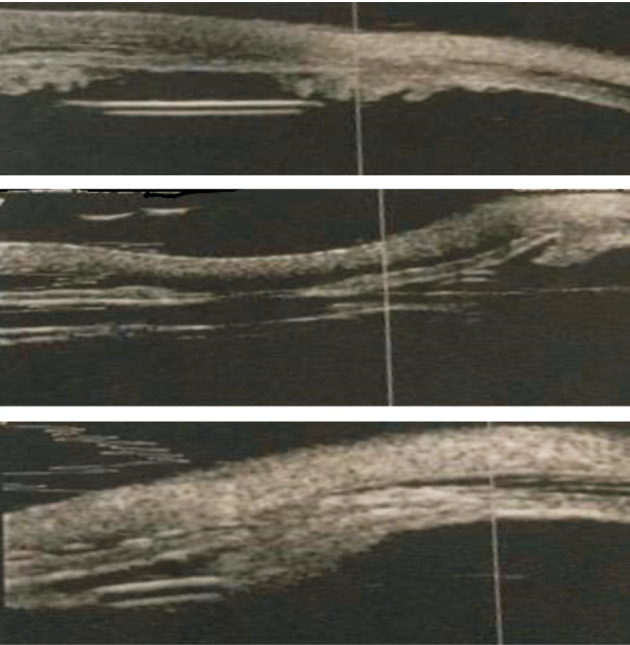
Anterior and posterior chamber are very narrowed due to hypotony resulting in shallowing of the angel.
Figure 2. Red free and colored photos of the left fundus showing hypotony signs with hypotony maculopathy.
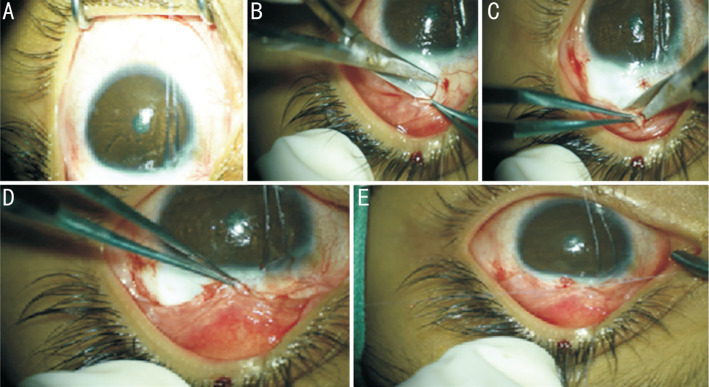
Surgical Technique
Our revision surgery was performed under general anesthesia. After sterilization of the surgical field and draping, traction corneal suture with 8/0 silk was taken at 12 o'clock to rotate the globe inferiorly to expose the superior field. According to the site of the bleb leakage, a 3 o'clock hour horizontal limbal peritomy incision was done in the superior conjunctiva. The bleb was then dissected backward, away from the underlying sclera and excised flush with the limbus. Good scrapping at the limbus was done with No.15 surgical blade to allow for better adhesion of the conjunctiva. Two horizontal conjunctival relaxing incisions were created at the 2 and 10 o'clock positions to allow for conjunctival advancement in 40% of the cases while the rest 60% did not need it (Figure 5).
Figure 5. Surgical technique for conjunctival advancement placement of traction suture (A), conjunctival opening and removal of necrotic tissue (B), conjunctival release (C), conjunctival advancement (D) and closure (E).
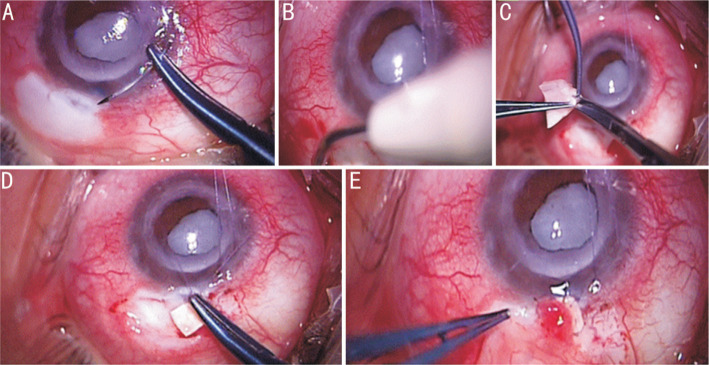
Resuturing of the scleral flap with 8/0 vicryl was done if a shallow anterior chamber or excessive aqueous humour leakage through the sclerostomy was seen during the procedure. In cases with scleral melting with exposed uvea, a partial scleral graft from a dead donor corneo-scleral button was taken by cutting it flush of the corneal remnants with a circumference of 2 clock hours and a width of the whole available scleral rim around the cornea. This scleral tissue was then divided into 2 vertical sheets by using a conjunctival scissor as seen in Figure 6.
Figure 6. Surgical technique for conjunctival advancement and scleral graft approach placement of traction suture (A), cauterization when needed after conjunctival opening (B), scleral fashioning into half thickness partial scleral graft (C), scleral placement over the area of scleral melting with 2 cardinal stitches (D) and conjunctival approximation and closure over the scleral graft (E).
The scleral graft was prepared by the same surgeon during the revision operation. It was taken from the scleral rim that surrounds the corneal grafts so it was preserved in the same preservative media as the donor cornea and it came sterilized in the bottle of donation from the eye bank. The scleral graft was fashioned so that it covers the scleral melted area in such a way that it was possible to take a good stitch bite into non-friable scleral tissue. Four cardinal stitches with 8/0 vicryl were taken each at one corner of the graft. This was creating a new healthy roof to the area of scleral melting without affecting the aqueous seepage through the subscleral pathway. Figure 6 is showing a real life example of conjunctival advancement alone and conjunctival advancement flap with partial thickness corneal grafting.
Our primary outcome measure was IOP change measured at 1, 2, 3mo and at the final follow up visit after surgery while our secondary outcome was the change in VA in the last follow up visit comparing them to prior to the revision surgery and comparing one approach to the other. Complete success was defined as resolution of the pre-existing leak or hypotony, with the maintenance of IOP between 6 and 21 mm Hg, in the absence of further glaucoma surgery and without any glaucoma medications. Moreover, qualified success met the above criteria with or without the use of glaucoma medications[28]. The follow up period ranged from 4 to 16mo with a mean of 8.3mo in the first group and 5 to 15mo in the other group with a mean of 7.6mo. Postoperatively, all cases received moxifloxacin eye drops five times per day for one week. Fixed dose combination of tobramycin and dexamethazone was used four times per day for the first week and tapered gradually over four weeks. Cyclopentolate drops were used in the first day only four times per day. Brimonidine was used every eight hours for the first day and reevaluation of the IOP was done in the first, second days then after 1wk, 1mo and then every 3mo till the last follow up visit. If the IOP was less than 10 mm Hg, brimonidine was stopped and the case was followed up. The cases were divided then into qualified and total success according to the use of antiglaucoma medications or not as mentioned before following revision.
Data were analyzed using SPSS for Windows, version 25.0 (SPSS Inc, Chicago, IL, USA). Number and percent were used for qualitative data while quantitative data were described using the mean and standard deviation. Pre- and post-operatively IOP and VA were compared using a paired t-test. P values of less than 0.05 were considered significant.
RESULTS
Twenty-eight patients (18 males, 10 females) were included in this study with 15 eyes were included in the conjunctival advancement group and 13 eyes were included in the conjunctival advancement with scleral graft group. The mean age of the conjunctival advancement group was 36.87±19.25y while it was 44.08±18.04y in the other group. The mean time from initial trabeculectomy to bleb revision was 14.39±6.58mo for the conjunctival advancement group and 12.31±5.88mo for the other group while the mean follow-up period was 8.3mo with range from 4 to 16mo for the conjunctival advancement group and 7.6mo with a range from 5 to 15mo in the other group. There was a significant difference in the baselines values of IOP between the two groups (P<0.001). However, the VA was comparable (P=0.23). More details about the diagnosis for trabeculectomy and follow up time for revision surgery are summarized in Table 1.
Table 1. The baseline characteristics for the included patients.
| Parameters | Conj. ADV (n=15) | Conj. ADV+graft (n=13) |
| Sex (male:female) | 9:6 | 9:4 |
| Age (y) | 36.87±19.25 | 44.08±18.04 |
| Indication of trabeculectomy | ||
| COAG | 7 | 5 |
| Juvenile | 3 | 1 |
| Traumatic | 1 | 3 |
| Neovascular | 2 | 1 |
| Steroid | 1 | 2 |
| CNAG | 1 | 1 |
| Time after trabeculectomy to revision surgery (mo) | 14.39±6.58 | 12.31±5.88 |
| Follow-up after revision surgery (mo) | 8.3 (4-16) | 7.6 (5-15) |
| Preop. IOP (mm Hg) | 2.73±1.16 (2-5) | 0.23±0.6 (0-2) |
| Preop. VA (logMAR) | 1.27±0.23 (1-1.78) | 1.37±0.19 (1.18-1.78) |
Values are presented as mean±standard deviation or mean (range) or n (number). Conj. ADV: Conjunctival advancement; COAG: Chronic open angle glaucoma; CNAG: Chronic narrow angle glaucoma; VA: Visual acuity.
In both study groups, the mean IOP significantly increased after revision surgery at one, two, three months and the final follow up visit when compared to prior revision surgery (P<0.001). According to the aforementioned criteria of success, throughout the follow up period, complete success was achieved in 6 eyes (40%) and 9 eyes (60%) had a qualified success in the conjunctival advancement group while complete success was achieved in 5 eyes (38.5%) and 8 eyes (61.5%) had a qualified success in the conjunctival advancement with scleral graft group. Moreover, VA was significantly improved (P=0.03) at the final follow-up visit after revision compared to before revision surgery for both groups. Mean IOP and VA of patients prior to and after revision surgery are summarized in Table 2.
Table 2. Mean IOP and VA of patients prior to and after revision surgery.
| Outcomes | Preoperative | 1mo | 2mo | 3mo | Last follow up |
| Mean IOP (mm Hg) | |||||
| ADV | 2.73±1.16 | 10.6±2.69 | 12.33±1.95 | 14±2.67 | 13.27±3.01 |
| ADV+scleral graft | 0.23±0.6 | 9.08±2.06 | 12.46±3.78 | 17.7±8.52 | 14.42±4.64 |
| Mean VA (logMAR) | |||||
| ADV | 1.27±0.23 | - | - | - | 0.79±0.32 |
| ADV+scleral graft | 1.37±0.19 | - | - | - | 0.99±0.35 |
ADV: Advancement; IOP: Intraocular pressure; VA: Visual acuity.
mean±SD
When both groups were compared to find out if there is any difference in the change from baseline for both surgical approaches, there was no significant difference between IOP improvement in 1mo (P=0.263) while the difference was significant in 2mo (P=0.03), 3mo (P=0.02) and at the last follow-up (P=0.02) postoperatively. However, the difference was not significant regarding VA (P=0.5). The difference of improvements in measurements of both groups is summarized in Table 3. Moreover, there were no spikes or other complications in any patient of both groups.
Table 3. The difference of improvements in measurements of both groups.
| Outcomes | Conj. ADV | Conj. ADV with scleral graft | P |
| Mean IOP (mm Hg) | |||
| Baseline-1mo | 7.87±2.5 | 8.85±1.95 | 0.263 |
| Baseline-2mo | 9.6±2.53 | 12.23±3.49 | 0.03 |
| Baseline-3mo | 11.27±3.08 | 17.53±8.25 | 0.02 |
| Baseline-last follow up | 10.53±3.34 | 14.15±4.6 | 0.02 |
| Mean VA (logMAR) | |||
| Baseline-last follow-up | 0.47±0.35 | 0.38±0.36 | 0.5 |
Conj. ADV: Conjunctival advancement; IOP: Intraocular pressure; VA: Visual acuity.
mean±SD
DISCUSSION
There are different reported options for bleb revision in the literature including bleb excision and conjunctival advancement, amniotic membrane transplant, the use of autologous free conjunctival graft, sclera patch graft, and pericardial graft[19]–[23]. In this retrospective study, we reported the follow up for both IOP and VA comparing conjunctival advancement and conjunctival advancement with scleral graft for the patients having late-onset hypotony. Our results showed that both approaches can lead to a significant improvement for IOP and VA. Additionally, conjunctival advancement and scleral graft approach was effective to increase IOP in advanced cases with scleral melting and uveal exposure at the baseline. The improvement was gradual over the first three months follow up period and found to be stable at the last follow-up period. Complete success was achieved 40% of conjunctival advancement group and 38.5% of the other group. Moreover, 60% could only achieve a qualified success in the conjunctival advancement group while 61.5% could achieve a qualified success in the other group.
These results are consistent with the previously published studies[26],[28]–[32]. For instance, a study reported by Tannenbaum et al[28] using bleb excision and scleral flap re-suturing with conjunctival advancement showed an excellent qualified success rate in terms of IOP increase and hypotony resolution after glaucoma filtering surgery. The study showed that 33 eyes out of 49 eyes (83%) achieved at least qualified success while there are 40% classified as complete success. However, the rate of complete success or qualified success did not differ significantly between the group of patients who underwent bleb excision and conjunctival advancement alone versus those who also had re-suturing of sclera and/or placement of a pericardial graft. Morever, Bitrian et al[29] reported a promising success rate of advancement of a conjunctival flap with preservation the preexisting bleb. In their study, 33 eyes were followed for 4.68±3.56y. They found an improvement in the logMAR VA from at 6 and 12mo after bleb revision (P<0.001) and there was an IOP increase from 3.51±2.27 mm Hg to 12.06±4.06 mm Hg (P<0.001) at 12mo. The same was found in Catoira et al[32] and Burnstein et al[26] studies with a qualified success rate of 80%. Furthermore, a larger study including 177 eyes showed a convenient overall success rates of less than 63% using different surgical techniques according to the intraoperative findings in cases with conjunctival leakage and hypotony included variations on excision of thin or leaking conjunctiva with advancement[20]. Despite the results of this large study could be considered a lower success rate, the long follow up period could explain these results.
In our study, the causes of hypotony were mostly due to microleakage from the over-filtering bleb due to the previous use of antimetabolites. The 13 candidates who underwent scleral grafting had scleral melting with uveal exposure that needed scleral resuturing during the revision procedure. Being a retrospective study and knowing that the surgeon performing the revision is not the one who performed the trabeculectomy, there was a limitation to obtain all of the information about the cases but mostly the onset of leak was 1-2y following the previous trabeculectomy. As has been stated before, the mean time of revision for the conjunctival group was 14.39±6.58mo and for that of the scleral graft group was 12.31±5.88mo following the initial procedure.
Although the main aim of the study was to describe the surgical outcomes of both adaptive techniques to investigate their efficacy, we furtherly compared both to assess which approach was the best in terms of improving IOP and VA. To avoid the limitation of both groups being not comparable for IOP at the baseline, we compared only the change in the IOP from baseline to the final follow up points.
As for our aforementioned surgical technique, we used relaxing incisions which is the same as what is done by Tannenbaum et al[28] and different from the placement of a mattress suture or running suture at the limbus provided in other studies[20]–[21]. Additionally, we have no complications for surgery in our study unlike Tannenbaum et al[28] study in which three patients (8%) required repeated bleb revision for persistent hypotony. Catoira et al[32] showed 10% incidence of recurrent bleb leaks and a 7% incidence of persistent hypotony and Burnstein et al[26] study which showed a 6% incidence of recurrent bleb leaks and bleb dysaesthesia. We speculate that we may got a lower incidence of complication due to the use of general anesthesia, expert surgeon, meticulous follow up, short follow up period which is still a limitation to our study, the type of glaucoma for which the initial surgery was done and the selection of surgery according to the severity of the case, so that all cases with scleral melting were managed with a healthy donor scleral grafting.
The rate of post trabeculectomy complications due to hypotony with its related complications due to the unjustified use of anti-fibrotics is increasing causing severe complications. This problem must be addressed in several studies as it is an important issue and even more studies must share in the management of such serious complication. To our knowledge, only one study was present in literature that was nearly the same to ours[28]. In this study the authors did not use a donor sclera but used the pericardium which is not available in our region. The conjunctival advancement flap procedure was not done in the same way as ours. Also, multiple surgeons preformed the revision in the other study. In our study, we described a new stitching technique of the scleral graft using only 4 cardinal 8/0 vicryl stitches to fix the graft to the healthy sclera around the area of scleral melting so that the graft is not too tight to prevent the seepage of aqueous underneath the scleral graft aiming at keeping a total success following this procedure. To our knowledge, this was the first study in the Middle East to address this problem and management according to our capabilities in this region of the world. It took about three years to come to existence in addition to about one year of postoperative follow up. In contrast to other studies, a single surgeon performed the operations so that there is less bias in the results. The other surgeon did only the follow up and recruitment of the cases with the scientific work related to the study. Only the two most used procedures for revision in Egypt as an example of a developing country were discussed and they were divided into conjunctival advancement for cases with no scleral melting and scleral graft with conjunctival advancement in cases with scleral melting. This can be a guide to other countries to solve a serious problem where the pericardium is not available. In our study we included real life microscope images to help others to adopt our techniques in the futures.
We have encountered several limitations in this study such as the retrospective design, limiting our ability of selecting comparable groups and the small number of the included patients also the short time of follow up period. However, for such kind of procedure, the included number was enough to give insights about both surgical options effect since the prospective design is difficult considering the nature of this study. We highly encourage future prospective comparative studies to consider both surgical options as their objective.
In conclusion, to recapitulate, our study showed that both conjunctival advancement and conjunctival advancement with scleral graft are effective for treating patients with late onset hypotony favoring the effect of conjunctival advancement with scleral graft for cases with scleral melting and lower IOP. Yet, more prospective studies are needed to assert upon these results.
Acknowledgments
Authors' contributions: Elhofi AS: revised and edited the manuscript, revised the statistical analysis, data collection and writing the manuscript; AbouSamra A: the idea and concept of the study, revised and edited the manuscript and collection of data; Doheim MF: writing the manuscript and analysis of the data.
Conflicts of Interest: Elhofi AS, None; Doheim MF, None; AbouSamra A, None.
REFERENCES
- 1.Broadway DC, Grierson I, O'Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol. 1994;112(11):1446–1454. doi: 10.1001/archopht.1994.01090230060021. [DOI] [PubMed] [Google Scholar]
- 2.Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66(4):673–679. [PubMed] [Google Scholar]
- 3.Bindlish R, Condon GP, Schlosser JD, D'Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology. 2002;109(7):1336–1341. discussion 1341–1342. doi: 10.1016/s0161-6420(02)01069-2. [DOI] [PubMed] [Google Scholar]
- 4.Wang D, Jampel HD. Imprecision medicine: the use of mitomycin C in trabeculectomy surgery. Ophthalmology Glaucoma. 2018;1(3):149–151. doi: 10.1016/j.ogla.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Ji Q, Qi B, Liu L, Guo X, Zhong J. Efficacy and safety of ologen implant versus mitomycin C in primary trabeculectomy: a Meta-analysis of randomized clinical trials. J Glaucoma. 2015;24(5):e88–e94. doi: 10.1097/IJG.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 6.Fontana H, Nouri-Mahdavi K, Lumba J, Ralli M, Caprioli J. Trabeculectomy with mitomycin C: outcomes and risk factors for failure in phakic open-angle glaucoma. Ophthalmology. 2006;113(6):930–936. doi: 10.1016/j.ophtha.2006.01.062. [DOI] [PubMed] [Google Scholar]
- 7.Tseng VL, Kim CH, Romero PT, Yu F, Robertson-Brown KW, Phung L, Raygoza D, Caprioli J, Coleman AL. Risk factors and long-term outcomes in patients with low intraocular pressure after trabeculectomy. Ophthalmology. 2017;124(10):1457–1465. doi: 10.1016/j.ophtha.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Olayanju JA, Hassan MB, Hodge DO, Khanna CL. Trabeculectomy-related complications in Olmsted County, Minnesota, 1985 through 2010. JAMA Ophthalmol. 2015;133(5):574–580. doi: 10.1001/jamaophthalmol.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dada T, Midha N, Sidhu T. Bleb-related infections. Ocular Infections: Prophylaxis and Management. 2017:128. [Google Scholar]
- 10.Abramowitz B, Moster MR. Management of conjunctival bleb leaks. Adv Ophthalmol Optom. 2017;2(1):279–300. [Google Scholar]
- 11.Okada K, Tsukamoto H, Masumoto M, et al. Autologous blood injection for marked overfiltration early after trabeculectomy with mitomycin C. Acta Ophthalmol Scand. 2001;79(3):305–308. doi: 10.1034/j.1600-0420.2001.790320.x. [DOI] [PubMed] [Google Scholar]
- 12.Wang Q, Thau A, Levin AV, Lee D. Ocular hypotony: a comprehensive review. Surv Ophthalmol. 2019;64(5):619–638. doi: 10.1016/j.survophthal.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Thomas M, Vajaranant TS, Aref AA. Hypotony maculopathy: clinical presentation and therapeutic methods. Ophthalmol Ther. 2015;4(2):79–88. doi: 10.1007/s40123-015-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenfield DS, Liebmann JM, Jee J, Ritch R. Late-onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol. 1998;116(4):443–447. doi: 10.1001/archopht.116.4.443. [DOI] [PubMed] [Google Scholar]
- 15.Anand N, Arora S, Clowes M. Mitomycin C augmented glaucoma surgery: evolution of filtering bleb avascularity, transconjunctival oozing, and leaks. Br J Ophthalmol. 2006;90(2):175–180. doi: 10.1136/bjo.2005.077800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gehring JR, Ciccarelli EC. Trichloracetic acid treatment of filtering blebs following cataract extraction. Am J Ophthalmol. 1972;74(4):622–624. doi: 10.1016/0002-9394(72)90821-5. [DOI] [PubMed] [Google Scholar]
- 17.Blok MD, Kok JH, van Mil C, Greve EL, Kijlstra A. Use of the megasoft bandage lens for treatment of complications after trabeculectomy. Am J Ophthalmol. 1990;110(3):264–268. doi: 10.1016/s0002-9394(14)76342-1. [DOI] [PubMed] [Google Scholar]
- 18.Leen MM, Moster MR, Katz LJ, Terebuh AK, Schmidt CM, Spaeth GL. Management of overfiltering and leaking blebs with autologous blood injection. Arch Ophthalmol. 1995;113(8):1050–1055. doi: 10.1001/archopht.1995.01100080102036. [DOI] [PubMed] [Google Scholar]
- 19.Cardakli N, Weinreb SF, Jefferys ScM JL, Quigley HA. Long-term functional outcomes of trabeculectomy revision surgery. Ophthalmol Glaucoma. 2019;2(4):240–250. doi: 10.1016/j.ogla.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Budenz DL. Conjunctival advancement for late-onset filtering bleb leaks. Arch Ophthalmol. 1999;117(8):1014. doi: 10.1001/archopht.117.8.1014. [DOI] [PubMed] [Google Scholar]
- 21.Myers JS, Yang CB, Herndon LW, Allingham RR, Shields MB. Excisional bleb revision to correct overfiltration or leakage. J Glaucoma. 2000;9(2):169–173. doi: 10.1097/00061198-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Perez CI, Oportus MJ, Mellado F, Valenzuela F, Cartes C, López-Ponce D, Salinas-Toro D, López-Solís R, Traipe L. Algorithm approach for revision surgery following late-onset bleb complications after trabeculectomy: long-term follow-up. Arq Bras Oftalmol. 2017;80(1):25–29. doi: 10.5935/0004-2749.20170008. [DOI] [PubMed] [Google Scholar]
- 23.B Scoralick AL, Almeida I, Ushida M, et al. Hypotony management through transconjunctival scleral flap resuturing: analysis of surgical outcomes and success predictors. J Curr Glaucoma Pract. 2017;11(2):58–62. doi: 10.5005/jp-journals-10028-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Canut MI, Cobián R, Fernández-Vega A, Julio G, Barraquer RI. Long-term follow-up of partial bleb excision in late-onset bleb-related complications by a single surgeon using conjunctival advancement. J Glaucoma. 2019;28(6):546–549. doi: 10.1097/IJG.0000000000001236. [DOI] [PubMed] [Google Scholar]
- 25.Wadhwani RA, Bellows AR, Hutchinson BT. Surgical repair of leaking filtering blebs. Ophthalmology. 2000;107(9):1681–1687. doi: 10.1016/s0161-6420(00)00282-7. [DOI] [PubMed] [Google Scholar]
- 26.Burnstein AL, WuDunn D, Knotts SL, Catoira Y, Cantor LB. Conjunctival advancement versus nonincisional treatment for late-onset glaucoma filtering bleb leaks. Ophthalmology. 2002;109(1):71–75. doi: 10.1016/s0161-6420(01)00838-7. [DOI] [PubMed] [Google Scholar]
- 27.Wilson MR, Kotas-Neumann R. Free conjunctival patch for repair of persistent late bleb leak. Am J Ophthalmol. 1994;117(5):569–574. doi: 10.1016/s0002-9394(14)70060-1. [DOI] [PubMed] [Google Scholar]
- 28.Tannenbaum DP, Hoffman D, Greaney MJ, Caprioli J. Outcomes of bleb excision and conjunctival advancement for leaking or hypotonous eyes after glaucoma filtering surgery. Br J Ophthalmol. 2004;88(1):99–103. doi: 10.1136/bjo.88.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bitrian E, Song BJ, Caprioli J. Bleb revision for resolution of hypotony maculopathy following primary trabeculectomy. Am J Ophthalmol. 2014;158(3):597–604.e1. doi: 10.1016/j.ajo.2014.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prokosch-Willing V, Lamparter J, Ul Hassan SN, Toshev AP, Pfeiffer N, Hoffmann EM. Results of an adaptive surgical approach for managing late onset hypotony after trabeculectomy with mitomycin C. J Glaucoma. 2018;27(4):307–314. doi: 10.1097/IJG.0000000000000886. [DOI] [PubMed] [Google Scholar]
- 31.Radhakrishnan S, Quigley HA, Jampel HD, Friedman DS, Ahmad SI, Congdon NG, McKinnon S. Outcomes of surgical bleb revision for complications of trabeculectomy. Ophthalmology. 2009;116(9):1713–1718. doi: 10.1016/j.ophtha.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Catoira Y, Wudunn D, Cantor L. Revision of dysfunctional filtering blebs by conjunctival advancement with bleb preservation. Am J Ophthalmol. 2000;130(5):574–579. doi: 10.1016/s0002-9394(00)00653-x. [DOI] [PubMed] [Google Scholar]