Dear Editor,
Central retinal artery or ophthalmic artery occlusion is a rare complication of facial filler injection, which causes irreversible blindness. Studies have reported failed attempts of retrobulbar, peribulbar, or intraarterial (inside the ophthalmic artery) injections of hyaluronidase to restore retinal arterial perfusion and vision[1]–[4]. However, the efficacy of this treatment approach remains inconclusive[2],[4]. Herein, we report a case of loss of vision following facial filler injection, which did not show improvement after three subtenon retrobulbar injections of hyaluronidase. Informed consent was obtained from the patient and this report adhered to the Declaration of Helsinki.
A 32-year-old woman visited our emergency room complaining of painful vision loss in her left eye after injection of hyaluronic acid gel (HAG) filler at the glabella. She could not perceive light with her left eye. Ptosis, ophthalmoplegia, and corneal edema were observed (Figure 1A, 1B). Skin around the nose and glabella showed discoloration that might be due to ischemia of dorsal nasal artery and angular artery that construct anastomoses with ophthalmic artery. On fundus photography, multiple retinal arterial emboli and ischemic white retina with a cherry red spot was observed (Figure 1C). Fundus fluorescein angiography (FA) showed severely delayed retinal and choroidal perfusion consistent with ophthalmic artery occlusion (Figure 1D). On MR angiography for brain and carotid artery to evaluate the thrombotic cause of ophthalmic artery occlusion, there was no significant finding, and it supported that ophthalmic artery occlusion was resulted from HAG filler, which was injected intra-arterially. After obtaining informed consent from the patient, we injected hyaluronidase (1500 units/3.5 mL normal saline) into the retrobulbar space via transconjunctival subtenon route using a 23-gauge long-curved needle, three hours after the onset of symptoms. Two additional retrobulbar injections of hyaluronidase were administered on the following day and after one week. However, no improvement was noticed in the patient's vision.
Figure 1. Clinical findings at initial presentation.
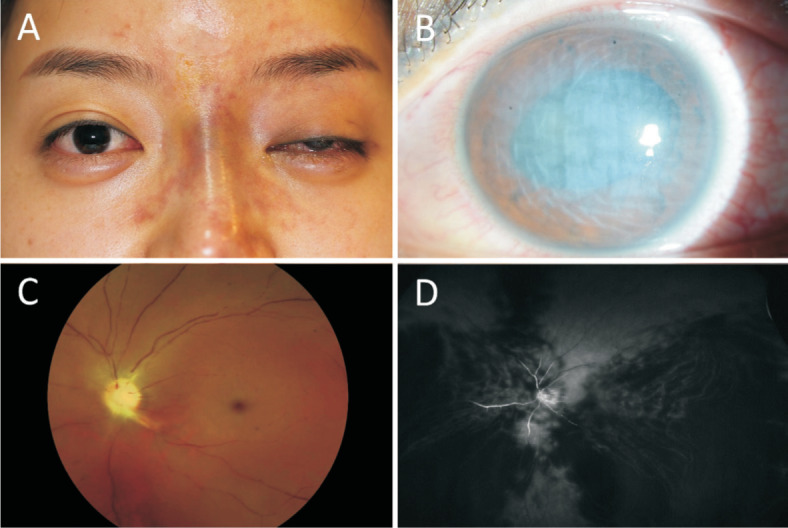
A: Ptosis with incomplete ophthalmoplegia in the left eye and nasal skin discoloration; B: Corneal edema with anterior chamber inflammation on slit lamp biomicroscopy; C: Multiple emboli in arterial vascular arcade and whitened retina with cherry red spot on fundus photography; D: FA showing severely diminished retinal and choroidal perfusion with diffuse non-perfused area, even in the late phase.
Three months later, near complete recovery was achieved in ptosis, ophthalmoplegia, and corneal edema, and partially improved retinal and choroidal perfusion were confirmed on FA (Figure 2). The patient still did not have light perception; ocular hypotony, slightly decreased eyeball size, and sensory exotropia were observed. She underwent surgery for correction of enophthalmos and strabismus. Three years later, atrophy of the iris and cataract developed (Figure 3). Phacoemulsification was performed without implantation of intraocular lens to remove the white cataract for the cosmetic purpose. Diffuse retinal atrophy with thick tractional membrane was observed at the latest fundus examination (Figure 3).
Figure 2. Fundus photography and FA 3mo post treatment.
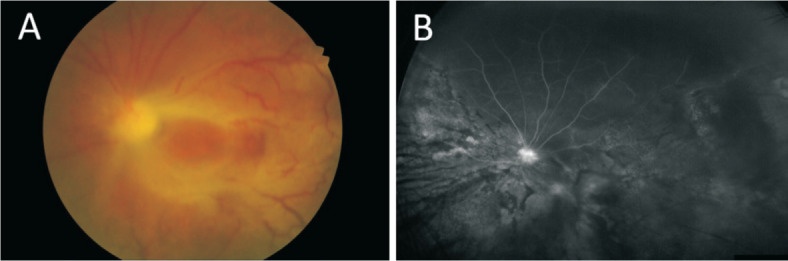
Despite three subtenon retrobulbar injections of hyaluronidase, the patient had no light perception. A: Pale disc and retinal degeneration are shown on fundus photography; B: Partially improved retinal and choroidal perfusion on FA were observed.
Figure 3. Fundus and anterior segment findings 3y post treatment.
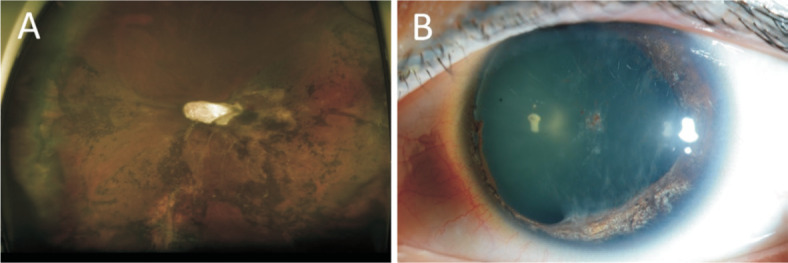
A: Diffuse retinal atrophy with thick tractional membrane are observed on fundus photography; B: Iris atrophy and cataract, which resulted from anterior segment ischemia, were aggravated.
The retrograde arterial embolism is suspected for the main mechanism of blindness after filler injection. Filler injected into subcutaneous arteries during cosmetic procedures accidently can migrate to the proximal site of the arterial system when injection force is higher than arterial pressure, and it can be propagated to other peripheral branches after the injection force is removed. Injection into glabella or nasal dorsum area, which is supplied by supratrochlear artery and dorsal nasal artery from ophthalmic artery, or angular artery and lateral nasal artery anastomosing with ophthalmic artery can cause of retrograde embolism resulting ophthalmic arterial occlusion[5]. Injection of filler materials into deep subcutaneous layers, injecting a large volume of filler into one area and the use of small-gauge sharp needles may increase the risk of vascular complications. In addition, the presence of deep tissue scar is also a risk factor because it stabilizes and fixes arteries in place and make them easier to be penetrated with needles[6]. Autologous fat is also known to be associated with a higher risk of vascular adverse events than hyaluronic acid. To prevent arterial occlusion, practitioners should have sufficient knowledge about detailed anatomy and injection techniques, and they should inject slowly with minimal pressure not to inject bolus in one location. Use of blunt cannula may reduce the risk of accidental intra-arterial injection, and aspiration prior to injection is recommended though it does not guarantee blood to flash back into the syringe in cases of arterial puncture due to the highly viscous filler materials inside the syringe[7]. Our group previously attempted intra-arterial injection of hyaluronidase to treat iatrogenic embolic blindness due to injection of hyaluronic acid filler. However, we failed to recanalize the ophthalmic artery and to restore vision, though partial recanalization was confirmed on angiography during the procedure[3].
Carruthers et al[1] showed that hyaluronidase can hydrolyze intravascular HAG across the vascular wall of the facial artery in an ex vivo human cadaveric model, and this was considered the basis for retrobulbar or peribulbar hyaluronidase injections in filler-associated retinal and ophthalmic arterial occlusion[8].
However, the actual clinical results after injection of hyaluronidase in patients with filler-associated retinal arterial occlusion are unsatisfactory. According to a report by Zhu et al[4], none of the four patients treated with retrobulbar injection of hyaluronidase within 4 to 32h after the events showed improvement in vision. The reasons for lack of improvement in vision are thought to be the short retinal survival time and the possibility of lack of action of hyaluronidase on intravascular HAG in humans. Considering the absence of perfusion restoration on FA in our case, retrobulbar injection of hyaluronidase has little effect in dissolving HAG in the retinal and ophthalmic arteries, in contrast to the in vitro study. It was suggested that the vascular wall in a living patient would be less permeable than cadaver-sourced free artery and that the blood stasis resulting from the filler material may impede the delivery of hyaluronidase to the proximity of the HAG[4]. Most recent study using a rabbit model of ophthalmic artery occlusion by HAG also showed that retrobulbar hyaluronidase injection failed to reverse obstruction or restore function[9].
Two cases have been reported in the literature wherein restoration of vision was achieved after retrobulbar injection of hyaluronidase[2],[8]. The studies proposed that the favorable prognosis compared to previous reports could be attributed to a very short lag time after the event. They emphasized on immediate injection of hyaluronidase in cases of vision loss after filler injection. However, the assessment of vision was based only on subjective statements of the patient, and no data on ophthalmic examinations or angiography were reported to prove reperfusion after the treatment.
Based on results of our case and those reported previously, retrobulbar injection of hyaluronidase appears to have no effect in restoring retinal arterial perfusion and vision in cases with facial filler-associated retinal or ophthalmic artery occlusion.
Acknowledgments
Foundation: Supported by the NRF Bio & Medical Technology Development Program (No.2018M3A9B5021319) funded by the Korean government (MSIP and MSIT).
Conflicts of Interest: Choe HR, None; Woo SJ, None.
REFERENCES
- 1.Carruthers JD, Fagien S, Rohrich RJ, Weinkle S, Carruthers A. Blindness caused by cosmetic filler injection: a review of cause and therapy. Plast Reconstr Surg. 2014;134(6):1197–1201. doi: 10.1097/PRS.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 2.Goodman GJ, Clague MD. A rethink on hyaluronidase injection, intraarterial injection, and blindness: is there another option for treatment of retinal artery embolism caused by intraarterial injection of hyaluronic acid? Dermatologic Surgery. 2016;42(4):547–549. doi: 10.1097/DSS.0000000000000670. [DOI] [PubMed] [Google Scholar]
- 3.Oh BL, Jung C, Park KH, Hong YJ, Woo SJ. Therapeutic intra-arterial hyaluronidase infusion for ophthalmic artery occlusion following cosmetic facial filler (hyaluronic acid) injection. Neuroophthalmology. 2014;38(1):39–43. doi: 10.3109/01658107.2013.830134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu GZ, Sun ZS, Liao WX, Cai B, Chen CL, Zheng HH, Zeng L, Luo SK. Efficacy of retrobulbar hyaluronidase injection for vision loss resulting from hyaluronic acid filler embolization. Aesthet Surg J. 2017;38(1):12–22. doi: 10.1093/asj/sjw216. [DOI] [PubMed] [Google Scholar]
- 5.Park SW, Woo SJ, Park KH, Huh JW, Jung C, Kwon OK. Iatrogenic retinal artery occlusion caused by cosmetic facial filler injections. Am J Ophthalmol. 2012;154(4):653–662.e1. doi: 10.1016/j.ajo.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 6.DeLorenzi C. Complications of injectable fillers, part 2: vascular complications. Aesthet Surg J. 2014;34(4):584–600. doi: 10.1177/1090820X14525035. [DOI] [PubMed] [Google Scholar]
- 7.Loh KT, Chua JJ, Lee HM, Lim JT, Chuah G, Yim B, Puah BK. Prevention and management of vision loss relating to facial filler injections. Singapore Med J. 2016;57(8):438–443. doi: 10.11622/smedj.2016134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chesnut C. Restoration of visual loss with retrobulbar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44(3):435–437. doi: 10.1097/DSS.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 9.Hwang CJ, Mustak H, Gupta AA, Ramos RM, Goldberg RA, Duckwiler GR. Role of retrobulbar hyaluronidase in filler-associated blindness: evaluation of fundus perfusion and electroretinogram readings in an animal model. Ophthalmic Plast Reconstr Surg. 2019;35(1):33–37. doi: 10.1097/IOP.0000000000001132. [DOI] [PubMed] [Google Scholar]


