Abstract
AIM
To assess physical activity (PA) including its intensity in primary open angle glaucoma (POAG).
METHODS
PA was characterized by the use of questionnaires: Seven-Day Physical Activity Recall and Historical Leisure Activity Questionnaire. A questionnaire of 36 questions, developed by the authors, was used to assess the level of knowledge about glaucoma
RESULTS
The study was conducted among 625 adults. The study group comprised 312 POAG patients aged over 40y, including 238 women (76%) and 74 men (24%). The control group consisted of 313 adults (>40 years old), including 202 (65%) women and 111 men (35%). The duration of current PA with an intensity of 4 metabolic equivalents (METs) was significantly shorter among people with POAG. PA in the past was significantly lower among people from the study group, regardless of gender. The level of glaucoma knowledge in patients with POAG was poor and significantly lower in men.
CONCLUSION
Regular PA is an important and underestimated factor predisposing to the progression of POAG. There is a necessity to undertake educational and preventive actions with a view to modify the health behavior of glaucoma patients.
Keywords: physical activity, intensity, primary open angle glaucoma, metabolic equivalent
INTRODUCTION
Glaucoma belongs to the group of eye diseases which are characterized by progressive damage to the optic nerve and may lead to loss of sight[1]–[2]. It is the second most common cause of blindness after cataract[3]. Moreover, it was recognised by the WHO as a social disease of the 21st century[4]. According to epidemiological data, about 2%-3% of the population aged between 40 and 65y and about 8% of the population aged over 65y are affected by the disease[5]. It is also estimated that about 70 million people worldwide are treated for glaucoma, of whom 14% patients suffer from blindness of both eyes[6].
The most common form of glaucoma is primary open angle glaucoma (POAG), the pathomechanism of which is related to the limitation of the outflow of aqueous humour by conventional route[7]. Increased intraocular pressure (IOP) is considered to be one of the most important risk factors for the occurrence and progression of the disease[8]. The significance of other glaucoma risk factors, including age over 35y, Afro-American race, family history of glaucoma, lipid metabolism disorders and excessive psychological-emotional burden was also proven[9]. There is well-established link between POAG and diabetes mellitus, corneal thickness and high myopia[10]. The correlation between glaucoma and gender as well as cardiovascular diseases, such as cardiomyopathies, heart disease, nocturnal hypotonia, abnormal blood pressure, past stroke or Raynaud's disease, is inconclusive[11].
Some studies point to a link between inappropriate health-related behaviour and incidence of glaucoma. Few studies suggest that low physical activity (PA) as well as limited knowledge of the disease may contribute to the development and progression of glaucoma. However, the results of these studies are often inconsistent and raise considerable controversies[12]–[13]. In addition, opinions on the potential significance of these factors in glaucoma pathomechanism are inconsistent[14]–[15].
The progression of glaucoma observed despite the attempts to eliminate and/or modify the currently known disease risk factors should lead to the search for other predisposing agents and to a better understanding of the pathomechanism of the disease[16]. The aim of this study was to assess PA including its intensity in a group of subjects with POAG and compare it with the control group without POAG.
SUBJECTS AND METHODS
Ethical Approval
The Bioethics Committee of the Lodz Medical University has given its consent for the conduct of the study (No.RNN/35/11/KB). Informed oral consent was obtained from all study participants.
Subjects
Totally 625 adults were enrolled in the study, including 312 with POAG as the study group and 313 without glaucoma as the control group. The inclusion criteria for the study group were age ≥40y as well as the diagnosis of POAG in accordance with the current guidelines for the disease diagnosis by American Glaucoma Society (AGS) and European Glaucoma Society (EGS)[17]. The studied group with POAG consisted of women in 76% (n=238) and in 24% of men (n=74). The control group included adults aged above 40y without POAG, with 64% of women (n=202) and 36% of men (n=111).
Methods
General data of the examined subjects was collected during the interview and it covered, among others, co-existence of systemic diseases. This data was obtained by means of an original questionnaire. Anthropometric indices, including body mass index (BMI; kg/m2), were evaluated during the study. Current physical activity (CPA) was assessed using the Seven-Day Physical Activity Recall taking into account: duration, energy expenditure and intensity[18]. Past physical activity (PPA) was estimated on the basis of the Historical Leisure Activity Questionnaire taking into account its intensity ranging from very low [1.5 metabolic equivalent (METs)] to very high (10 METs)[19]. In this study, the MET of the intensity of PA is the METs number, where 1 METs=3.5 mL O2/(kg·min)[20].
Among the respondents from the POAG group, the scope of their knowledge about glaucoma was evaluated using an original questionnaire of 36 questions, assessed using a 6-point scale, i.e. from excellent level (correct answer to all questions) to insufficient level (lack of answers or incorrect answer to at least 12 questions). The questions focused, among others, on the knowledge of factors predisposing to glaucoma development, its symptoms and the treatment methods.
Statistical Analysis
Statistical analysis used the independence χ2 test and independence χ2 test with Yates' correction, χ2 Pearson test, exact Fischer test and non-parametric U Mann-Witney test. Statistical analysis was performed using the statistical package Statistica 9.0. The significance level of inference was P<0.05.
RESULTS
The general and clinical characteristics of the subjects are presented in Table 1. Women with glaucoma were characterized by higher body weight and BMI values than women without glaucoma (P<0.00). The number of women with normal body weight (BMI 18.5-24.9) was significantly lower in the group of women with glaucoma than in the control group (29.4% vs 56.4%; P<0.00). It was shown that obesity was significantly more common among people with POAG, regardless of gender (P<0.00). Table 2 shows the general and clinical characteristics of the subjects with POAG and control group. The examined glaucoma group demonstrated worse general health condition in comparison to the control group, both in relation to men and women (P<0.00). Among patients with POAG, coexistence of diseases and pathological symptoms was more common than among patients in the control group, among women (81.1% vs 60.4%, P<0.00) and men (82.4% vs 74.8%, P<0.00), respectively.
Table 1. The general and clinical characteristics of the subjects, depending of gender.
| Parameters | Female (n=440) |
P | Male (n=185) |
P | ||
| POAG (n=238) | Control (n=202) | POAG (n=74) | Control (n=111) | |||
| Age (y) | 73.1±11.2 | 71.8±11.2 | 0.18 | 73.5±12.5 | 74.7±10.2 | 0.34 |
| Height of body (cm) | 160.7±7.1 | 162.7±5.7 | 0.49 | 171.6±7.0 | 170.5±6.3 | 0.09 |
| Body mass (kg) | 72.8±14.6 | 66.9±11.4 | <0.001 | 80.5±13.1 | 79.4±13.9 | 0.65 |
| BMI (kg/m2), n (%) | 28.6±5.8 | 25.2±3.9 | <0.001 | 27.4±4.4 | 27.3±4.3 | 0.55 |
| Normal (18.5-24.9) | 70 (29.4) | 114 (56.4) | <0.00 | 21 (28.4) | 33 (29.7) | 0.67 |
| Overweight (25.0-29.9) | 82 (34.5) | 66 (32.7) | 0.37 | 39 (52.7) | 64 (57.7) | 0.16 |
| Obesity (≥30) | 86 (36.1) | 22 (10.9) | 0.00 | 14 (18.9) | 14 (12.6) | 0.00 |
BMI: Body mass index; POAG: Primary open angle glaucoma. P: POAG vs Control.
n=625, mean±SD
Table 2. The general and clinical characteristics of the subjects, depending of gender.
| Characteristics | Male (n=185) |
Female (n=440) |
||||
| POAG (n=74) | Control (n=111) | P | POAG (n=238) | Control (n=202) | P | |
| No coexistence of diseases | 13 (17.6) | 28 (25.2) | 0.03 | 45 (18.9) | 80 (39.6) | <0.00 |
| Other chronic diseasea | 17 (23.0) | 42 (37.8) | 0.03 | 74 (31.1) | 50 (24.8) | 0.14 |
| Hypertension | 26 (35.1) | 38 (34.2) | 0.11 | 109 (45.8) | 58 (28.7) | 0.00 |
| Cold hands and feet | 31 (41.9) | 24 (21.6) | 0.003 | 162 (68.1) | 66 (32.7) | <0.00 |
| Migraine | 6 (8.1) | 6 (5.4) | 0.46 | 64 (26.9) | 32 (15.8) | 0.001 |
| Stroke past | 5 (6.8) | 6 (5.4) | 0.70 | 24 (10.1) | 10 (5.0) | 0.04 |
| Heart diseaseb | 47 (63.5) | 49 (44.1) | 0.01 | 137 (57.6) | 69 (34.2) | <0.00 |
| Diabetes mellitus 1/2 | 26 (35.1) | 35 (31.5) | 0.61 | 64 (26.9) | 48 (23.8) | 0.45 |
aLungs, joints, thyroid, pancreas and liver, mental, peptic ulcer and duodenum; bIschemic heart diseases, heart attack, cardiomyopathy. POAG: Primary open angle glaucoma. P: POAG vs Control.
n=625, n (%)
CPA of the examined subjects is presented in Table 3. The relative total weekly energy expenditure per kilogram of body weight was significantly lower in the group with POAG compared to the group without glaucoma. Statistically significant differences were observed in the group of women (P=0.005). The duration of moderate intensity CPA (4 METs) was significantly shorter in glaucoma patients than in control group patients, both in women (P=0.0005) and men (P=0.003).
Table 3. Current weekly energy expenditure in absolute and relative terms to PA.
| Weekly energy expenditure | Female (n=440) |
Male (n=185) |
|||||
| POAG (n=238) | Control (n=202) | P | POAG (n=74) | Control (n=111) | P | ||
| Values | Absolute (kcal/wk) | 1818±513.0 | 1766±506.1 | 0.11 | 2144±602.1 | 2118±637.7 | 0.36 |
| Relative (kcal/kg·wk) | 253.5±50.5 | 261.0±47.4 | 0.005 | 255.1±52.6 | 266.4±53.8 | 0.08 | |
| Duration of PA of varying intensity (h/wk) | 1 METs | 54.7±13.9 | 50.5±9.5 | 0.001 | 56.7±11.3 | 51.6±9.8 | 0.06 |
| 1.5 METs | 105.2±17.0 | 106.0±15.1 | 0.40 | 104.1±15.7 | 105.1±14.3 | 0.85 | |
| 4 METs | 6.1±7.7 | 8.3±10.3 | 0.0005 | 4.2±5.4 | 7.5±8.1 | 0.003 | |
| 6 METs | 1.7±4.0 | 2.5±4.9 | 0.10 | 2.1±4.0 | 2.5±4.8 | 0.89 | |
| 10 METs | 0.3±1.3 | 0.7±3.5 | 0.15 | 0.9±2.8 | 1.3±3.2 | 0.72 | |
POAG: Primary open angle glaucoma. P: POAG vs Control.
mean±SD
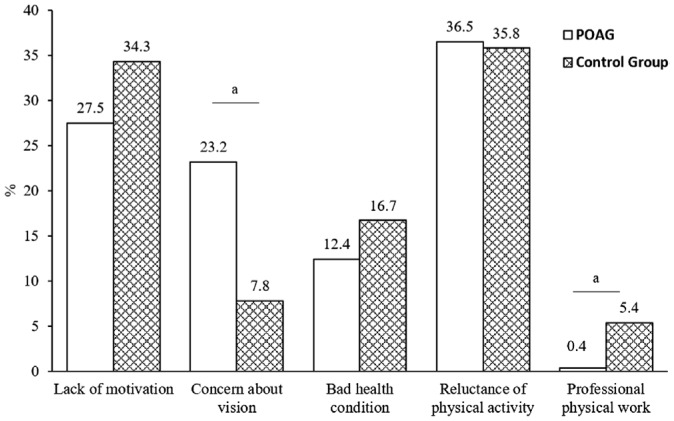
Distribution of reasons (n=437) why the subjects in both study groups did not undertake PA of intensity ≥4 METs in leisure time is depicted in Figure 1. The most common reason for not engaging with PA among the respondents from POAG group was their aversion to physical exercise (36.5%) and in lower percentage their lack of motivation (27.5%). The reluctance to exercise was as well the main reason for lack of PA among POAG-free individuals (36.5%). Significant differences were observed between the groups in terms of concerns about the impact of PA on the condition of the eyes and the performance of daily physical work.
Figure 1. Characteristics of the reasons for not engaging in regular recreation physical exercise of intensity ≥4 METs by 70.0% respondents (n=437).
aP<0.01.
Table 4 shows the characteristics of PPA by the respondents (n=232) taken into account the intensity and type of undertaken PPA, respective to gender. Significantly higher PA was reported by subjects in the control group in comparison to POAG group, regardless of sex (P<0.00). It was shown that recreational PA with an intensity of ≥4 METs was most frequently undertaken between the ages of 18 and 35y in both groups, similarly among women and men. Moreover, in this period of life there was observed the highest percentage of people with glaucoma among whom the only undertaken PA was physical education at school. The results were statistically significant for women (P<0.00) and men (P=0.002). On the other hand, no statistically significant correlations were identified between the character of the performed professional work or coexistence of systemic diseases (in particular cardiovascular diseases) and subjects PA (P>0.05).
Table 4. Characteristics of the subjects' regular PPA.
| Types of PPA (age, y) | Female (n=440) |
Male (n=185) |
||||
| POAG (n=238) | Control (n=202) | P | POAG (n=74) | Control (n=111) | P | |
| People with regular recreational PA in leisure time of intensity ≥4 METs at last 30min per day, 3-5 times in a week (n=264) | ||||||
| Gardening (56-65) | 14 (5.9) | 6 (3.0) | 0.24 | 6 (8.1) | 4 (3.6) | 0.02 |
| Types of regular exercises (18-35) | 54 (22.7) | 94 (46.5) | <0.00 | 23 (31.8) | 63 (56.8) | 0.001 |
| Team games | 16 (6.7) | 39 (19.3) | <0.00 | 7 (9.5) | 38 (34.2) | <0.00 |
| Classes at fitness clubs/resistance dynamic and static exercises | 16 (6.7) | 44 (21.8) | <0.00 | 10 (13.5) | 33 (29.7) | 0.01 |
| Running | 42 (17.6) | 74 (36.6) | <0.00 | 12 (16.2) | 35 (31.5) | 0.02 |
| Swimming | 27 (11.3) | 64 (31.7) | <0.00 | 10 (13.5) | 35 (31.5) | 0.005 |
| People with habitual PA of intensity <4 METs (n=361) | ||||||
| PA of intensity ≤1.5 METs | 25 (10.5) | 10 (4.9) | 0.03 | 10 (13.5) | 9 (8.1) | 0.24 |
| PA during education at school (8-25) | 129 (54.2) | 64 (31.7) | <0.00 | 30 (40.5) | 22 (19.8) | 0.002 |
| Professional physical work (18-55) | 11 (4.6) | 16 (5.9) | 0.15 | 2 (2.7) | 9 (8.1) | 0.23 |
| Physical work at home (18-55) | 5 (2.1) | 12 (5.9) | 0.07 | 3 (4.1) | 4 (3.6) | 0.81 |
| Total | 145 (60.9) | 92 (45.5) | 0.001 | 35 (47.3) | 35 (31.5) | 0.03 |
PPA: Past physical activity; PA: Physical activity; POAG: Primary open angle glaucoma. P: POAG vs Control.
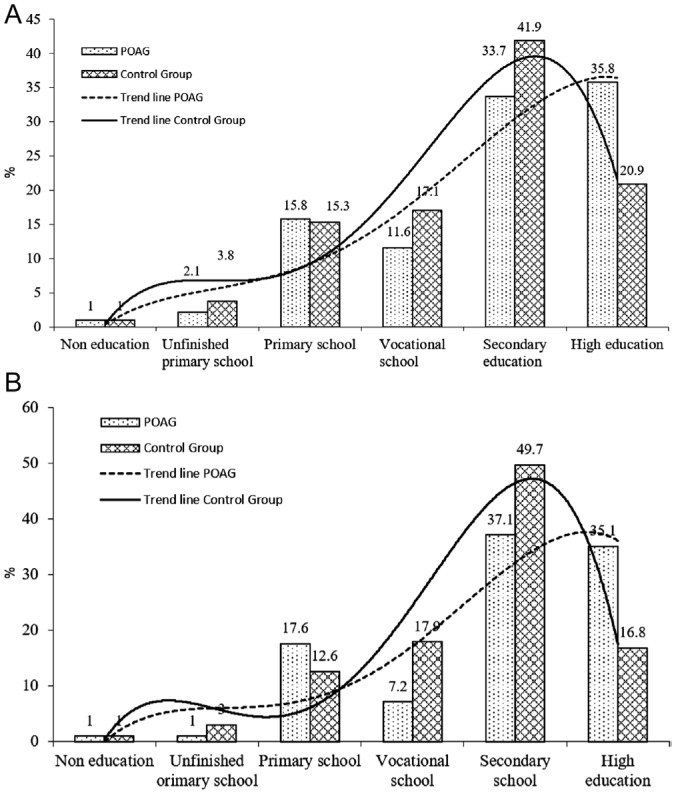
No significant differences were found in the frequency of ≥4 METs PA intensity for such sociodemographic variables as: age, sex or place of residence of the subjects (P>0.05). It was observed that the only factor considerably affecting PA was education. Higher education correlated strongly with higher CPA and PPA, both in the POAG group and the control group, and it referred to both genders (P<0.00). The highest percentage of PA during the participants' lifetime was recorded in both studied and control groups with secondary and tertiary education. It was found that people with better knowledge of their disease more often undertook PA, but the results were not statistically significant (P>0.05). Analysis of the level of education as a factor that can influence CPA and PPA is depicted in Figure 2.
Figure 2. The percentage of subjects taking regular PA 30min a day, 3-5 times per week with intensity ≥4 METs, currently (A, n=188) and in the past (B, n=264), as compared to the level of education.
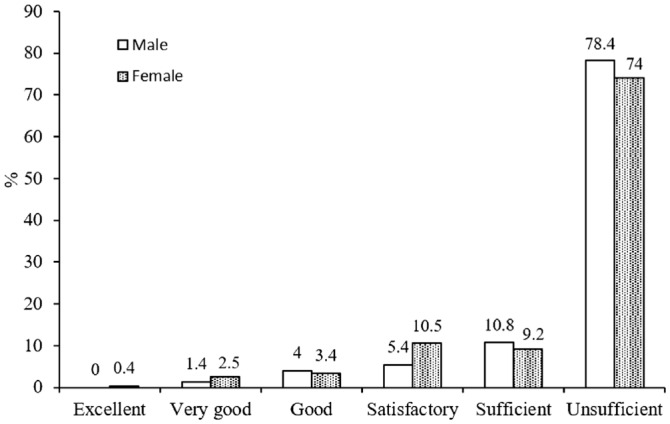
The studied POAG subjects' level of knowledge about glaucoma on a six-point scale is presented in Figure 3. The factor determining the degree of knowledge about glaucoma was the level of education. A direct correlation was observed, i.e. the lower the education, the lower the glaucoma awareness among the respondents (P>0.05). In addition, it was found that women tended to be better informed about glaucoma than men. The level of glaucoma knowledge among patients with POAG was poor and significantly lower among men than among women (P<0.00). The 74.0% of women and 78.4% of men lacked information on their disease (P>0.05). Only 4.3% of the respondents had very good and good knowledge level (women 2.5% vs men 1.4%). The 24.7% of subjects were neither aware of the diagnosed disease nor of the reason for ophthalmological treatment: this group included significantly more men (women 21.8% vs men 33.8%, P>0.05).
Figure 3. Level of knowledge about glaucoma among POAG patients (n=312).
DISCUSSION
Although glaucoma has been known for almost 160y[10], the pathomechanism of the disease remains unclear and the effectiveness of treatment, even today, is not satisfactory in all cases[8],[21]–[25]. Currently, we are aware of numerous potential factors influencing glaucoma occurrence and progression apart from increased IOP[26]. The importance of abnormal health-related behavior including insufficient PA as well as relatively poor knowledge about glaucoma and PA role[27] is increasingly emphasized as one of the above-mentioned factors.
It has been proven that the most beneficial form of workout for adults is PA with energy expenditure above 2000 kcal/wk (4200 kJ/wk). According to some scientific societies, including European Academy of Sociology (EAS), European Society of Cardiology (ESC), European Society of Hypertension (ESH), PA should be based on moderate intensity endurance effort, i.e. inducing up to 60%-70% of maximum heart rate at least 5 times a week and lasting 150min/wk[20],[28]–[29]. Regrettably, most of the respondents did not comply with these recommendations.
The results of authors' research also confirmed that the values of relative total weekly energy expenditure during PA (per kilogram of body weight) were significantly lower in the group with POAG in comparison to the control group. Moreover, duration of moderate intensity PA (≥=4 METs, recommended for the prevention of chronic non-communicable diseases) was significantly shorter in the POAG group compared to the glaucoma-free group.
Interestingly, numerous POAG subjects named worries about their eyesight as the main reason for such low PA. We assumed, based on this research, that it was influenced by low knowledge of the disease nature and lack of motivation for PA. On the other hand, another seemingly objective reason for small PA was the advanced age of the subjects (73.3±11.9y) and more frequent aversion to exercise in this age group.
As currently established, regular exercise reduces IOP and improves vascular perfusion of the retina and choroid. Moreover, better color recognition and contrast parameters were observed in these cases[30]. It has been proven that even short distances walk effectively lower IOP in glaucoma patients[31]. Furthermore, dynamic single physical effort decreases IOP by 30% in healthy people and even by 54%-60% in glaucoma patients[32]–[33].
Analysis of the data obtained and published in other studies showed that PA among adults in the USA was lower than among respondents in a similar age group in Poland and other European countries[34]. It was reported that only 11% of American adults undertook PA according to the current recommendations[35]. A higher percentage of PA was recorded in Lithuania (48%), Latvia (48%) and Estonia (57%). According to data from 2001-2010, it was estimated that 70% of healthy people in Poland did not undertake any physical exercise[36]. Active leisure time spending was reported among 33.6% of adults aged 65y and over and they were walking, cycling or gardening[37].
In addition, it was found that PA was lower in the POAG group than in the glaucoma-free group and this affected both genders. It was also shown that only 42.2% of the respondents with glaucoma undertook in the past recreational PA with an intensity of ≥4 METs in their time off their professional and household duties. The most frequently practised sports among these respondents were team games (football, volleyball, basketball) as well as fitness club activities (including resistance, static and dynamic exercises), short and long distance running and swimming. Furthermore, it was observed that, regardless of type of activity, PA was mostly undertaken at the age of 18-35y, although a more accurate assessment of PA regarding its forms in the past was difficult to assess, especially among the elderly.
In the available scientific literature, there are no comprehensive studies on the characteristics of PA type in patients with POAG, including analysis of its intensity and duration. Besides, as shown in own and other authors' research, the knowledge of patients with POAG about their disease was far from sufficient[38]–[39]. It is emphasized that older age and lower education correlated strongly with less knowledge about the disease.
By demonstrating poor knowledge of disease as well as low PA level among POAG patients, this study revelated a need for future action in order to influence these factors. Improvement could be achieved for example by creating patients' self-support groups and social support for glaucoma patients and their families. These measures can contribute to modification of the health-related behavior of glaucoma patients[40]–[41]. This is not only important for the slower progression of glaucoma but also for reducing incidence of other chronic diseases. Furthermore, such actions may contribute to the prevention of early disability and allow POAG patient to remain physically and occupationally active for the longest possible period of time.
The results of the research indicate the need to undertake educational and preventive measures in the field of modification of health-related behaviours especially PA of people with glaucoma. This may have a positive impact, not only on the course of POAG, but also on the prevention of other chronic non-communicable diseases in these patients.
Acknowledgments
Conflicts of Interest: Olszewska H, None; Kosny J, None; Jurowski P, None; Jegier A, None.
REFERENCES
- 1.Kharmyssov C, Abdildin YG, Kostas KV. Optic nerve head damage relation to intracranial pressure and corneal properties of eye in glaucoma risk assessment. Med Biol Eng Comput. 2019;57(7):1591–1603. doi: 10.1007/s11517-019-01983-2. [DOI] [PubMed] [Google Scholar]
- 2.Lee E, Kim TW, Kim JA, Kim JA, Kim H. Spontaneous retinal venous pulsation in unilateral primary open-angle glaucoma with low intraocular pressure. J Glaucoma. 2017;26(10):896–901. doi: 10.1097/IJG.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 3.Kolko M. Detection and prevention of blindness in patients with glaucoma is a socio-economical challenge. Ugeskr Laeg. 2017;179(5):V06160444. [PubMed] [Google Scholar]
- 4.Korsakova NV. The prymary open-angel glaucoma: modern theory of development (literature review) Uspekhi Gerontol. 2018;31(1):95–102. [PubMed] [Google Scholar]
- 5.Barkana Y, Dorairaj S. Re: Tham et al.: Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis (Ophthalmology 2014;121:2081-2090) Ophthalmology. 2015;122(7):e40–e41. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Souzeau E, Goldberg I, Healey PR, Mills RA, Landers J, Graham SL, Grigg JR, Usher B, Straga T, Crawford A, Casson RJ, Morgan WH, Ruddle JB, Coote MA, White A, Stewart J, Hewitt AW, Mackey DA, Burdon KP, Craig JE. Australian and new zealand registry of advanced glaucoma: methodology and recruitment. Clin Exp Ophthalmol. 2012;40(6):569–575. doi: 10.1111/j.1442-9071.2011.02742.x. [DOI] [PubMed] [Google Scholar]
- 7.Tham YC, Cheng CY. Associations between chronic systemic diseases and primary open angle glaucoma: an epidemiological perspective. Clin Exp Ophthalmol. 2017;45(1):24–32. doi: 10.1111/ceo.12763. [DOI] [PubMed] [Google Scholar]
- 8.Wostyn P. Glaucoma as a dangerous interplay between ocular fluid and cerebrospinal fluid. Med Hypotheses. 2019;127:97–99. doi: 10.1016/j.mehy.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Iyigun E, Tastan S, Ayhan H, Coskun H, Kose G, Mumcuoglu T. Life experiences of patients with glaucoma: a phenomenological study. J Nurs Res. 2017;25(5):336–343. doi: 10.1097/JNR.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 10.Czajkowski J, Matusiak D, Grabowski R. Jaskra-narastający problem społeczny XXI wieku. Materiały szkoleniowe Łódzkich Warsztatów Jaskrowych. Okulistyka-wydanie specjalne. 2004:3–8. [Google Scholar]
- 11.Hollands H, Johnson D, Hollands S, Simel DL, Jinapriya D, Sharma S. Do findings on routine examination identify patients at risk for primary open-angle glaucoma? The rational clinical examination systematic review. JAMA. 2013;309(19):2035–2042. doi: 10.1001/jama.2013.5099. [DOI] [PubMed] [Google Scholar]
- 12.McMonnies CW. Glaucoma history and risk factors. J Optom. 2017;10(2):71–78. doi: 10.1016/j.optom.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fabjani S, Richter-Müksch S, Cakmak N, Markstaller M, Weingessel B, Vécsei-Marlovits VP. Level of knowledge about glaucoma in Vienna. Wien Klin Wochenschr. 2015;127(15-16):612–618. doi: 10.1007/s00508-014-0687-1. [DOI] [PubMed] [Google Scholar]
- 14.Waterman H, Bull S, Shaw M, Richardson C. Group-based patient education delivered by nurses to meet a clinical standard for glaucoma information provision: the G-TRAIN feasibility study. Pilot Feasibility Stud. 2018;4:121. doi: 10.1186/s40814-018-0313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, Patton GC. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 16.Vélez-Gómez MC, Vásquez-Trespalacios EM. Adherence to topical treatment of glaucoma, risk and protective factors: a review. Arch Soc Esp Oftalmol. 2018;93(2):87–92. doi: 10.1016/j.oftal.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 17.De Moraes CG, Liebmann JM, Levin LA. Detection and measurement of clinically meaningful visual field progression in clinical trials for glaucoma. Prog Retin Eye Res. 2017;56:107–147. doi: 10.1016/j.preteyeres.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the five-City project1. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 19.Kriska AM, Sandler RB, Cauley JA, LaPorte RE, Hom DL, Pambianco G. The assessment of historical physical activity and its relation to adult bone parameters. Am J Epidemiol. 1988;127(5):1053–1063. doi: 10.1093/oxfordjournals.aje.a114881. [DOI] [PubMed] [Google Scholar]
- 20.Alashi A, Riaz H, Lang R, Seballos R, Feinleib S, Sukol R, Cho L, Cremer P, Jaber W, Griffin BP, Desai MY. Incremental prognostic value of exercise stress testing in primary prevention. Am J Cardiol. 2019;124(2):216–223. doi: 10.1016/j.amjcard.2019.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Xu C, Li JJ, Li Z, Mao XC. Migraine as a risk factor for primary open angle glaucoma: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97(28):e11377. doi: 10.1097/MD.0000000000011377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Höhn R, Mirshahi A, Nickels S, Schulz A, Wild PS, Blettner M, Pfeiffer N. Cardiovascular medication and intraocular pressure: results from the Gutenberg Health Study. Br J Ophthalmol. 2017;101(12):1633–1637. doi: 10.1136/bjophthalmol-2016-309993. [DOI] [PubMed] [Google Scholar]
- 23.Nowak MS, Jurowski P, Gos R, Prost ME, Smigielski J. Pulsatile ocular blood flow in subjects with sleep apnoea syndrome. Arch Med Sci. 2011;7(2):332–336. doi: 10.5114/aoms.2011.22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matlach J, Bender S, König J, Binder H, Pfeiffer N, Hoffmann EM. Investigation of intraocular pressure fluctuation as a risk factor of glaucoma progression. Clin Ophthalmol. 2019;13:9–16. doi: 10.2147/OPTH.S186526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moroi SE, Reed DM, Sanders DS, Almazroa A, Kagemann L, Shah N, Shekhawat N, Richards JE. Precision medicine to prevent glaucoma-related blindness. Curr Opin Ophthalmol. 2019;30(3):187–198. doi: 10.1097/ICU.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kapetanakis VV, Chan MP, Foster PJ, Cook DG, Owen CG, Rudnicka AR. Global variations and time trends in the prevalence of primary open angle glaucoma (POAG): a systematic review and meta-analysis. Br J Ophthalmol. 2016;100(1):86–93. doi: 10.1136/bjophthalmol-2015-307223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang YW, Zhao Y, Xie SS, Wang XR, Chen Q, Xia XB. Resilience mediates the relationship between social support and quality of life in patients with primary glaucoma. Front Psychiatry. 2019;10:22. doi: 10.3389/fpsyt.2019.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.F Piepoli M. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Int J Behav Med. 2017;24(3):321–419. doi: 10.1007/s12529-016-9583-6. [DOI] [PubMed] [Google Scholar]
- 29.Drygas W, Kostka T, Jegier A, Kuński H. Long-term effects of different physical activity levels on coronary heart disease risk factors in middle-aged men. Int J Sports Med. 2000;21(4):235–241. doi: 10.1055/s-2000-309. [DOI] [PubMed] [Google Scholar]
- 30.Wang YX, Wei WB, Xu L, Jonas JB. Physical activity and eye diseases. The Beijing Eye Study. Acta Ophthalmol. 2019;97(3):325–331. doi: 10.1111/aos.13962. [DOI] [PubMed] [Google Scholar]
- 31.Lee MJ, Wang J, Friedman DS, Boland MV, De Moraes CG, Ramulu PY. Greater physical activity is associated with slower visual field loss in glaucoma. Ophthalmology. 2019;126(7):958–964. doi: 10.1016/j.ophtha.2018.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chrzczanowicz J, Gawron-Skarbek A, Kostka J, Nowak D, Drygas W, Jegier A, Kostka T. Physical activity and total antioxidant capacity across an adult lifespan of men. Med Sci Sports Exerc. 2012;44(4):575–582. doi: 10.1249/MSS.0b013e318238b7f0. [DOI] [PubMed] [Google Scholar]
- 33.Williams PT. Relationship of incident glaucoma versus physical activity and fitness in male runners. Med Sci Sports Exerc. 2009;41(8):1566–1572. doi: 10.1249/MSS.0b013e31819e420f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000;32(9):1601–1609. doi: 10.1097/00005768-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Pomerleau J, McKee M, Robertson A, Vaasc S, Kadziauskiene K, Abaravicius A, Bartkeviciute R, Pudule I, Grinberga D. Physical inactivity in the Baltic countries. Prev Med. 2000;31(6):665–672. doi: 10.1006/pmed.2000.0761. [DOI] [PubMed] [Google Scholar]
- 36.Kostka T, Jachimowicz V. Relationship of quality of life to dispositional optimism, health locus of control and self-efficacy in older subjects living in different environments. Qual Life Res. 2010;19(3):351–361. doi: 10.1007/s11136-010-9601-0. [DOI] [PubMed] [Google Scholar]
- 37.Rowinski R, Dabrowski A, Kostka T. Gardening as the dominant leisure time physical activity (LTPA) of older adults from a post-communist country. The results of the population-based PolSenior Project from Poland. Arch Gerontol Geriatr. 2015;60(3):486–491. doi: 10.1016/j.archger.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 38.Fabjani S, Richter-Müksch S, Cakmak N, Markstaller M, Weingessel B, Vécsei-Marlovits VP. Level of knowledge about glaucoma in Vienna. Wien Klin Wochenschr. 2015;127(15-16):612–618. doi: 10.1007/s00508-014-0687-1. [DOI] [PubMed] [Google Scholar]
- 39.Perez CI, Singh K, Lin S. Relationship of lifestyle, exercise, and nutrition with glaucoma. Curr Opin Ophthalmol. 2019;30(2):82–88. doi: 10.1097/ICU.0000000000000553. [DOI] [PubMed] [Google Scholar]
- 40.Sotimehin AE, Ramulu PY. Measuring disability in glaucoma. J Glaucoma. 2018;27(11):939–949. doi: 10.1097/IJG.0000000000001068. [DOI] [PubMed] [Google Scholar]
- 41.Peralta E, Muir KW, Rosdahl JA. Systematic review of knowledge assessments for glaucoma patients. Semin Ophthalmol. 2018;33(3):377–388. doi: 10.1080/08820538.2016.1247180. [DOI] [PubMed] [Google Scholar]