An insightful paper by Dowd et al. (1) highlights the importance of demography for analyzing coronavirus disease 2019 (COVID-19)–related mortality. The authors underscore the role of population age structure and intergenerational contacts for understanding differences in cross-country fatality and estimate the potential impact of the pandemic on different populations, acknowledging the need for additional information on the prevalence of comorbidities. We aim to interpret the proposed scenarios considering the widely different prevalence of chronic conditions by age in three of the countries discussed in the original paper. We argue that the burden of chronic diseases has the potential to offset the possible benefits of younger populations with different epidemiological characteristics.
Age is fundamental to understanding differences in mortality risks. Indeed, age is a marker of the gradual accumulation of permanent damage over the life course and, consequently, is highly associated with chronic diseases and disabilities (2–4). Epidemiologic, social, and built environments amplify this association. As a result, the prevalence of chronic diseases at any given age can be expected to differ substantially in high-, low-, and middle-income settings. Since there is evidence that individuals with preexisting chronic conditions are at an increased risk of severe COVID-19 disease (5–8), it is essential to understand age-related health differences with respect to these conditions to shed light on the COVID-19 burden across countries.
Dowd et al. (1) applied the estimated age-specific case-fatality rates of COVID-19 from Italy to younger—and less healthy—populations. By doing this, they implicitly assumed that the age prevalence of underlying comorbidities is similar in Italy, Brazil, and Nigeria. However, these populations have very different epidemiological profiles.
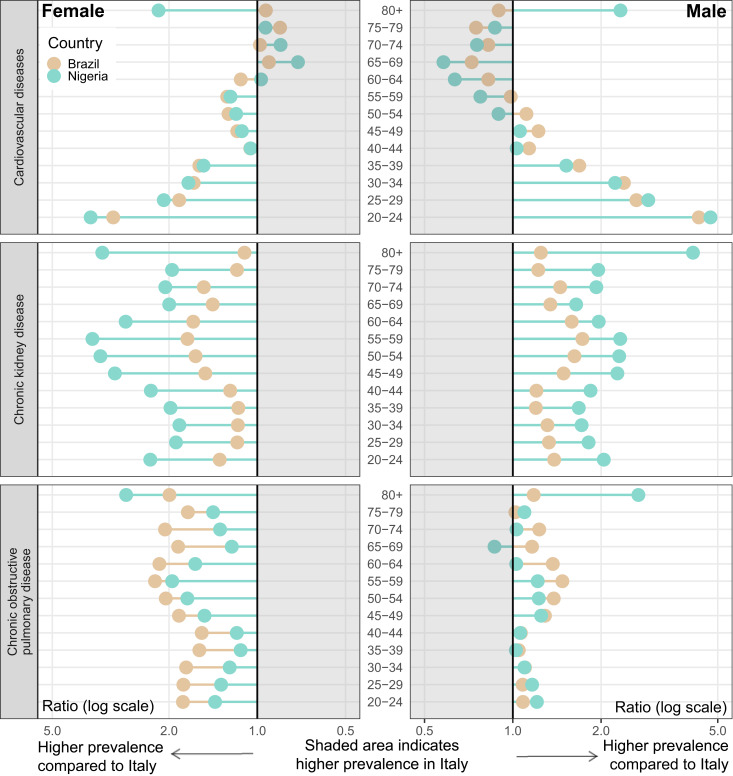
Fig. 1 shows the ratios of the age-specific prevalence of underlying comorbidities of Brazil and Nigeria with respect to Italy using the Global Burden of Disease database (9) for cardiovascular disease, chronic obstructive pulmonary disease (COPD), and chronic kidney disease, health conditions most frequently observed in deaths and hospitalization from COVID-19 (5–8). Relative to Italy, the prevalence of chronic kidney and COPD in Brazil and Nigeria is considerably greater at most ages. Brazil and Nigeria have a substantially higher prevalence of cardiovascular diseases at adult ages but a lower prevalence at older ages.
Fig. 1.
Relative prevalence by health condition and age in Brazil and Nigeria compared to Italy: female and male, 2017. Source: ref. 9.
The influence of chronic disease prevalence on the steep age gradient to severe outcomes from COVID-19 is still unclear. If this influence is considerable, the differences across populations presented here suggest that younger individuals in low- and middle-income countries may be at a substantially higher risk of severe COVID-19 illness than individuals of the same age in high-income settings once age-related health conditions are considered.
Demography science is not limited to the study of population distribution by age. Demographers can help elucidate other sources of between- and within-age variations in social distancing levels and infection, hospitalizations, and fatality rates as severe acute respiratory syndrome coronavirus 2 spreads in different settings. Besides chronic diseases, other potential factors include population density, household size and composition, hygienic and sanitary conditions, access to healthcare services, case notification systems, migration and displacement patterns, interregional inequalities, labor-market structure, economic disparities and welfare programs, endemic and other epidemic diseases, early-life conditions, epigenetic mechanisms, and immunosenescence.
Acknowledgments
We thank Ugofilippo Basellini and Alyson van Raalte for their helpful comments and suggestions. This project was funded by the European Research Council under grant number 716323.
Footnotes
The authors declare no competing interest.
References
- 1.Dowd J. B., et al. , Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. U.S.A. 117, 9696–9698 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crimmins E., Vasunilashorn S., Kim J. K., Alley D., Biomarkers related to aging in human populations. Adv. Clin. Chem. 46, 161–216 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuh D., Shlomo Y. B., Ezra S., A Life Course Approach to Chronic Disease Epidemiology (Oxford University Press, New York: ), ed. 2, 2004). [Google Scholar]
- 4.Yashin A. I., Vaupel J. W., Iachine I. A., A duality in aging: The equivalence of mortality models based on radically different concepts. Mech. Ageing Dev. 74, 1–14 (1994). [DOI] [PubMed] [Google Scholar]
- 5.Huang C., et al. , Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., et al. , Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395, 1054–1062 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remuzzi A., Remuzzi G., COVID-19 and Italy: What next? Lancet 395, 1225–1228 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richardson S. et al.; and the Northwell COVID-19 Research Consortium , Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA, 10.1001/jama.2020.6775 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute for Health Metrics and Evaluation , GBD Results Tool. http://ghdx.healthdata.org/gbd-results-tool. Accessed 20 April 2020.