Abstract
Background
Chronic kidney disease (CKD) is a growing public health problem and an important cause of morbidity and mortality. Disparities in CKD may be related to social determinants and health inequalities in low- and middle-income countries. This study determined how social determinants of health influence trends in the prevalence and mortality of CKD in Peru.
Methods
This was an ecological study based on a secondary analysis of health care and death records obtained from the Ministry of Health of Peru for the period 2010–2016. The standardized prevalence and mortality rates of CKD were descriptively reported using geospatial exploratory analysis. We also determined the association with social determinants of health according to the domains suggested by Healthy People 2020.
Results
In the studied period, CKD prevalence increased by 300% and was associated with the health insurance coverage rate (β=5.9 [95% CI 0.82 to 10.92]), proportion of people with a secondary education level (β=11.4 [95% CI 1.94 to 20.93]), mean age (β=−10.7 [95% CI −19.33 to −2.12]), monetary poverty rate (β=−2.2 [95% CI −3.88 to −0.60]) and gross domestic product per capita (β=−63.2 [95% CI −117.81 to −8.52]). The standardized mortality decreased by 10% and was associated with mean age (β=−0.6 [95% CI −1.22 to −0.06]) and the proportion of people with a primary education level (β=−0.5 [95% CI −0.9 to −0.05]).
Conclusions
During the period 2010–2016, the prevalence of CKD increased and the mortality associated with CKD decreased. The observed changes were associated with some social determinants of health, such as increased health coverage and education. The health system of Peru must be prepared to take on the challenge.
Keywords: chronic kidney disease, epidemiology, Peru, social determinants of health
Introduction
Chronic kidney disease (CKD) is a public health problem worldwide due to its increasing global burden and costs and because it is an important cause of premature morbidity and mortality.1–5 The Global Burden of Disease (GBD) expert group estimated that in 2013 reduced glomerular filtration rate accounted for 4% of deaths worldwide, with >50% of these related to cardiovascular diseases and the remaining to CKD in dialysis.6 The exact burden of CKD has yet to be fully elucidated in low- and middle-income countries (LMICs), where it is estimated that the incidence rates might be up to four times higher than those observed in developed countries.6 In high-income countries, CKD disproportionately affects socially disadvantaged groups, such as ethnic minorities and people of low socio-economic status. In the same way, the economic burden of CKD has seldom been evaluated in LMICs, where it is estimated to be significantly higher than that observed in developed countries.6,7
According to the GBD, CKD prevalence increased to 87% and the attributed mortality to 98% from 1990 to 2016.8 However, variations have been reported in some countries, such as the USA, where the prevalence has stabilized,9,10 or Korea and Taiwan, where the mortality has decreased.11,12
Sixty-three percent of the global burden of CKD occurs in LMICs; however, there is no information available to determine the prevalence and mortality in many of these countries.8 Likewise, these countries usually have insufficient healthcare expenditures and much of the disease burden is influenced by certain social determinants of health, making it difficult to use the information from high-income countries in this context.13,14 The social determinants of health have been recognized by the WHO as elements that influence public health and health inequalities.14 The role of the social determinants has recently gained greater attention as an important element in the pathway from CKD risk to the development and complications of CKD.4 Many of the determinants of CKD, such as obesity, diabetes, hypertension and endothelial dysfunction, as well as chronic inflammation, neurohormonal activation and oxidative stress, are related to the socio-economic vulnerability of the population.4 Peru is a middle-income country. Although its economy and health services coverage have improved, it is still a country with large inequalities, with around 25% of the population living in poverty and around 6% in extreme poverty.15,16 It is likely that social determinants influence the prevalence and mortality of non-communicable diseases such as CKD, as reported in other countries.13,14 Furthermore, Peru has a fragmented health system, where the Ministry of Health (MINSA) provides healthcare to about 60% of the population, mainly people living in extreme poverty, and Social Security (EsSalud) provides healthcare to about 30% of the population.17
In Peru, there are no population-based data estimating the prevalence of CKD. Although some studies estimate this prevalence to be between 16% and 18%,18,19 changes in prevalence in recent years have not been studied. Similarly, although the trend in CKD mortality was determined in a previous study,20 the influence of social determinants of health, as with studies on prevalence and in other LMICs,7 has not been assessed. Therefore the objective of this study was to determine the trends in the prevalence and mortality of CKD among patients from establishments of the MINSA during the period 2010–2016 in Peru, as well as the influence of the social determinants of health on both variables.
Methods
Design and data source
We conducted an ecological study using secondary data sources, with each region-year (e.g. Ayacucho 2015) as a unit of analysis. The main information source was the national and regional record of cases reported annually in healthcare services during the period 2010–2016 and deaths based on death certificates during the period 2010–2015, provided by the MINSA. This database contains the records of all healthcare interventions conducted in the health establishments that belong to the MINSA, and all deaths that occurred in the country as recorded in death certificates from the National Registry of Identification and Civil Status of Peru. In this study we considered the underlying cause of death for the analysis as the disease that initiated the train of morbid events leading directly to death.
In addition, we used information from the National Household Survey of Peru (ENAHO) and the Regional Information System for Decision Making (SIRTOD), both conducted by the National Institute of Statistics and Informatics of Peru. The ENAHO is registered in the online International Household Survey Network Catalog, a repository of developing country census questionnaires widely accepted and internationally tested by the United Nations Statistics Division. The ENAHO is a nationally representative database containing information on demographic, social and economic characteristics of Peruvian households collected annually since 2004. The SIRTOD is an information system that collects annual data from specialized Peruvian surveys (several of them with tested questionnaires, similar to the ENAHO) and data provided by ministry statistics offices. The SIRTOD collects around 1200 indicators in different areas and is used for the implementation of strategic programs.
Procedures
We requested information on reported cases of national healthcare interventions and mortality via the Platform for Access to Public Information (Plataforma de Acceso a la Información Pública) of the MINSA (http://www.minsa.gob.pe/portada/transparencia/solicitud/frmFormulario.asp). Data from ENAHO and SIRTOD are freely available from the following websites: http://iinei.inei.gob.pe/microdatos/ and http://webinei.inei.gob.pe:8080/SIRTOD1/inicio.html#, respectively.
Outcome variables
The outcome variables were the prevalence and mortality rates of CKD, calculated as ratios: (1) the number of cases recorded annually in healthcare establishments in 2010–2016, in the population covered by the integrated health insurance program (SIS), plus the uninsured population serviced mainly by the MINSA; and (2) the number of deaths reported in 2010–2015, in the population of each region-year assessed, by 100 000 persons. The number of cases and the number of deaths were obtained from the MINSA with the code CIE 10:N18 (chronic kidney disease), defined in the database as abnormalities of kidney structure or function, with a glomerular filtration rate of <60 mL/min/1.73 m2 present for >3 mo and implications for health. These variables were assessed by year, sex, age, group and region. We estimated the population size for each region-year using the ENAHO. We also obtained the annual age-standardized prevalence and mortality rates with the direct method using the population from WHO 2000–2025 as a reference.15
Exposure variables
The exposure variables were calculated for each region-year. Given that the ENAHO contains data representing national and regional levels, we weighted the data to obtain population-based indicators.
To obtain the social determinants of health we initially intended to use the five key domains suggested by Healthy People 2020: economic stability, education, neighbourhood and built environment, social and community context, and health and healthcare.13 However, for Peru we only had annual and region datasets for economic stability, education and health and healthcare. The remaining domains were excluded since data were available only for specific years and mainly for urban areas.
For the domain of economic stability, we considered the employment rate (proportion of employed people in the working-age population) and the monetary poverty rate (proportion of people in monetary poverty in the total population) from the ENAHO. Data on the average GDP per capita were extracted from SIRTOD.
For the domain of education, we considered the proportion of people in the primary, secondary and tertiary education levels, technical and university (proportion of people with a specific education level in the total population) obtained from the ENAHO.
For the domain of health and healthcare, we considered the rate of health insurance coverage (proportion of people with at least one type of health insurance, public, private, army) in the total population obtained from the ENAHO.
Finally, we used the mean age and proportion of women, obtained from the ENAHO, as adjustment variables to reduce the confounding bias.
Statistical analysis
The management, preparation and analysis were conducted using Stata 15.0 (StataCorp, College Station, TX, USA). The continuous variables were described using means and standard deviations, while the categorical variables were described using absolute frequencies and proportions.
We described the national trends of standardized prevalence and mortality rates of CKD for each year. Additionally, we conducted an exploratory analysis of spatial data, matching the standardized prevalence and mortality rates of CKD reported for each region with the georeferenced data of the regions (spmap in Stata) obtained from the web portal of the Ministry of the Environment of Peru. We categorized the standardized prevalence and mortality rates of CKD in quintiles of frequency and averaged the first two and the last two years to avoid the bias from measurement error associated with taking just one year as a reference, similar to a previous study.21
Multiple linear regression was used for analysing longitudinal data (xtreg in Stata). We assessed the strength of the association between social determinants (exposure variables) and outcome variables (prevalence and mortality rates of CKD). The model included a random intercept. We calculated the 95% CIs with errors corrected by robust variance. We considered coefficients with a p-value <0.05 to be statistically significant. We excluded the region of Callao in the multiple linear regression model, as information from this region was not available to calculate some variables relevant for the analysis.
Ethics statement
This study was conducted using secondary data sources obtained from several public access websites. These data are anonymous, so they do not involve any direct risk of subject identification.
Results
Trends in the prevalence of CKD at the regional and national level
During the period 2010–2016, 154 142 cases of CKD were recorded in the MINSA database (Table 1), of which 82 936 (53.8%) occurred in the age group >60 y, 56 762 (36.8%) in the age group 30–59 y and 14 444 (9.4%) in age group <30 y.
Table 1.
Trends in the standardized prevalence and mortality rates of CKD by year, Ministry of Health of Peru
| Year | Cases of CKD, n | Standardized prevalence, ×100 000 population | Deaths due to CKD, n | Deaths due to CKD, %a | Standardized mortality, ×100 000 population |
|---|---|---|---|---|---|
| 2010 | 10 316 | 54.9 | 2035 | 1.9 | 9.2 |
| 2011 | 13 579 | 68.7 | 2036 | 1.7 | 8.8 |
| 2012 | 14 901 | 74.5 | 2102 | 1.8 | 8.9 |
| 2013 | 20 622 | 98.0 | 1983 | 1.6 | 8.1 |
| 2014 | 21 319 | 98.2 | 2076 | 1.6 | 8.2 |
| 2015 | 37 214 | 170.1 | 2234 | 1.7 | 8.6 |
| 2016 | 36 191 | 163.5 | NA | NA | NA |
| Total | 154 142 | 103.9 | 12 466 | 1.7 | 8.6 |
aTotal number of deaths due to CKD divided by the total number of deaths due to all causes in Peru.
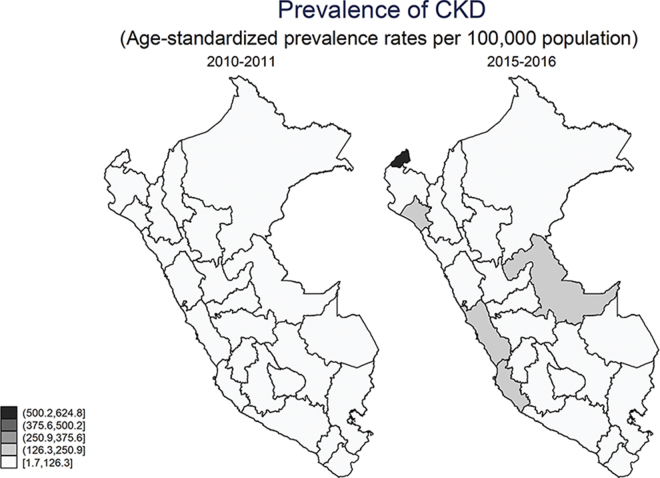
The standardized prevalence of CKD in Peru increased three times in the period 2010–2016 (Table 1). The regions with the greatest increase in prevalence, above the national average, were Tumbes, Lambayeque and Lima (Table 2 and Figure 1).
Table 2.
Standardized prevalence and mortality rates of CKD by region, Ministry of Health of Peru
| Regions | Standardized prevalence, ×100 000 population | Standardized mortality, ×100 000 population | ||||||
|---|---|---|---|---|---|---|---|---|
| 2010–2011 | 2015–2016 | Difference | Ratio | 2010–2011 | 2014–2015 | Difference | Ratio | |
| Peru (country) | 61.8 | 166.8 | 105.0 | 2.7 | 9.0 | 8.4 | −0.6 | 0.9 |
| Amazonas | 2.5 | 8.7 | 6.2 | 3.5 | 1.8 | 4.1 | 2.3 | 2.3 |
| Áncash | 14.3 | 65.1 | 50.8 | 4.6 | 4.5 | 3.3 | −1.3 | 0.7 |
| Apurímac | 9.2 | 13.1 | 3.9 | 1.4 | 8.1 | 4.5 | −3.6 | 0.6 |
| Arequipa | 38.8 | 88.7 | 50.0 | 2.3 | 3.4 | 4.6 | 1.3 | 1.4 |
| Ayacucho | 11.6 | 14.4 | 2.8 | 1.2 | 7.4 | 4.0 | −3.4 | 0.5 |
| Cajamarca | 4.0 | 30.5 | 26.6 | 7.7 | 2.8 | 2.5 | −0.3 | 0.9 |
| Callao | 613.4 | 688.1 | 74.7 | 1.1 | 12.4 | 6.1 | −6.3 | 0.5 |
| Cusco | 43.0 | 83.7 | 40.7 | 1.9 | 7.6 | 4.9 | −2.8 | 0.6 |
| Huancavelica | 7.2 | 11.6 | 4.5 | 1.6 | 11.0 | 5.2 | −5.8 | 0.5 |
| Huánuco | 9.5 | 8.4 | −1.2 | 0.9 | 6.4 | 5.4 | −1.0 | 0.8 |
| Ica | 33.2 | 256.3 | 223.1 | 7.7 | 8.6 | 12.2 | 3.6 | 1.4 |
| Junín | 10.8 | 12.5 | 1.7 | 1.2 | 8.8 | 7.9 | −0.9 | 0.9 |
| La Libertad | 77.3 | 77.0 | −0.3 | 1.0 | 8.8 | 8.8 | 0.0 | 1.0 |
| Lambayeque | 44.9 | 374.0 | 329.1 | 8.3 | 9.0 | 9.6 | 0.6 | 1.1 |
| Lima | 122.8 | 364.9 | 242.1 | 3.0 | 4.7 | 4.3 | −0.4 | 0.9 |
| Loreto | 65.6 | 157.3 | 91.7 | 2.4 | 2.6 | 0.9 | −1.8 | 0.3 |
| Madre de Dios | 44.5 | 117.0 | 72.5 | 2.6 | 12.8 | 9.1 | −3.6 | 0.7 |
| Moquegua | 14.7 | 75.7 | 61.0 | 5.1 | 9.6 | 10.7 | 1.1 | 1.1 |
| Pasco | 4.6 | 9.2 | 4.6 | 2.0 | 5.7 | 4.1 | −1.6 | 0.7 |
| Piura | 6.2 | 77.6 | 71.4 | 12.5 | 4.6 | 9.5 | 4.9 | 2.1 |
| Puno | 14.0 | 20.3 | 6.3 | 1.5 | 19.6 | 16.2 | −3.5 | 0.8 |
| San Martín | 10.1 | 50.2 | 40.1 | 5.0 | 3.2 | 3.0 | −0.2 | 0.9 |
| Tacna | 29.7 | 55.3 | 25.5 | 1.9 | 8.7 | 7.9 | −0.8 | 0.9 |
| Tumbes | 27.9 | 786.1 | 758.2 | 28.1 | 10.8 | 6.8 | −4.0 | 0.6 |
| Ucayali | 18.1 | 253.0 | 234.8 | 14.0 | 8.8 | 5.8 | −2.9 | 0.7 |
Figure 1.
Standardized prevalence of CKD in Peru, by region: comparison of the periods 2010–2011 and 2015–2016.
Trends in mortality due to CKD at the regional and national levels
During the period 2010–2015, 12 466 CKD deaths were recorded in the MINSA database (Table 1), of which 10 003 (80.2%) occurred in the age group >60 y, 2098 (16.8%) in the age group 30–59 y and 365 (3%) in the age group <30 y.
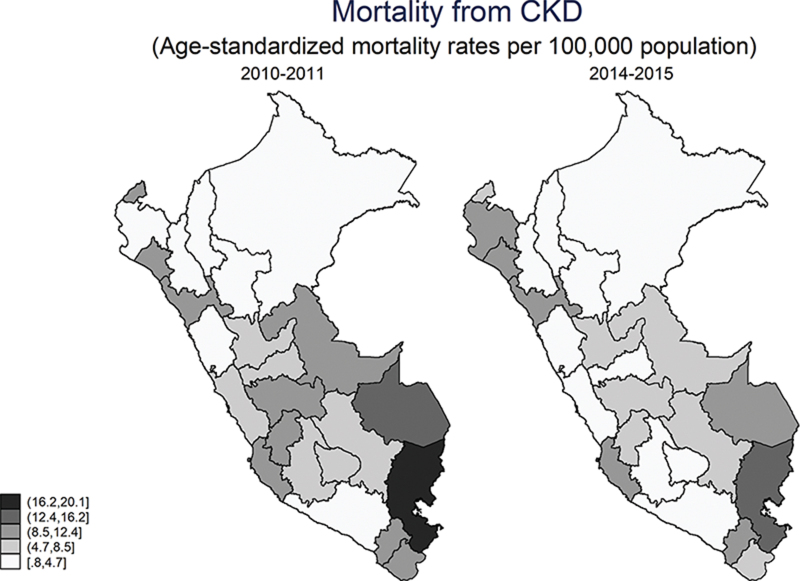
The standardized mortality rate of CKD in Peru decreased from 9.2 to 8.6 per 100 000 population in the period 2010–2015 (Table 1). The regions with the greatest decrease were Callao (−6.3), Huancavelica (−5.8) and Tumbes (−4.0), while Puno was the region with the highest mortality compared with the other regions (Table 2 and Figure 2).
Figure 2.
Standardized mortality due to CKD in Peru, by region: comparison of the periods 2010–2011 and 2014–2015.
Descriptive statistics of social determinants
During the period 2010–2016, the proportion of women for all regions was 50.7%, the mean age was 31.2, the health insurance rate was 69.8%, the proportion of people with a primary education level was 28.5%, the employment rate was 95.1%, the poverty rate was 28.4% and the log-GDP per capita was 9.3 (Table 3).
Table 3.
Descriptive statistics of social determinants
| Variables | n | Proportion | 95% CI |
|---|---|---|---|
| Women | 168 | 50.65 | 50.48 to 50.82 |
| Yearsa | 168 | 31.23 | 30.90 to 31.55 |
| Health insurance rate | 168 | 69.74 | 67.93 to 71.54 |
| Primary level | 168 | 28.52 | 28.04 to 28.99 |
| Secondary level | 168 | 24.56 | 23.58 to 25.54 |
| Tertiary level | 168 | 10.66 | 10.09 to 11.24 |
| Employment rate | 168 | 95.13 | 94.87 to 95.29 |
| Poverty | 168 | 28.37 | 25.98 to 30.76 |
| log-GDP per capitaa | 168 | 9.26 | 9.17 to 9.34 |
aYears and log-GDP per capita are expressed as the mean value, the remaining variables are expressed by proportion.
Social determinants of the prevalence of and mortality due to CKD
We found a positive association between CKD prevalence, the health insurance coverage rate (β=5.9 [95% CI 0.82 to 0.92]) and the proportion of people with a secondary education level compared with those who did not complete any education level (β=11.4 [95% CI 1.94 to 20.93]). In contrast, we found a negative association between CKD prevalence and mean age (β=−10.7 [95% CI −19.33 to −2.12]), monetary poverty rate (β=−2.2 [95% CI −3.88 to −0.60]) and log-GDP per capita (β=−63.2 [95% CI −117.81 to −8.52]) (Table 4). A negative association was also found between the CKD mortality rate, mean age (β=−0.6 [95% CI −1.22 to −0.06]) and proportion of people with a primary education level (β=−0.5 [95% CI −0.99 to −0.05]) in the region (Table 4).
Table 4.
Multivariate analysis of social determinants with the standardized prevalence and mortality rates of CKD
| Variables | Prevalence of CKD (2010–2016) | Mortality of CKD (2010–2015) | ||||
|---|---|---|---|---|---|---|
| Coefficienta | 95% CI | p-Valueb | Coefficienta | 95% CI | p-Valueb | |
| Social determinants | ||||||
| Women, % | 7.44 | −4.38 to 19.26 | 0.217 | −0.48 | −0.97 to 0.02 | 0.059 |
| Years | −10.72 | −19.33 to −2.12 | 0.015 | −0.64 | −1.22 to −0.06 | 0.031 |
| Health insurance rate | 5.87 | 0.82 to 10.92 | 0.023 | −0.01 | −0.07 to 0.05 | 0.728 |
| Primary level, % | 6.81 | −10.44 to 24.06 | 0.439 | −0.52 | −0.99 to −0.05 | 0.030 |
| Secondary level, % | 11.43 | 1.94 to 20.93 | 0.018 | 0.05 | −0.31 to 0.41 | 0.793 |
| Tertiary level, % | 9.43 | −1.56 to 20.41 | 0.093 | 0.16 | −0.33 to 0.65 | 0.524 |
| Employment rate | −1.46 | −12.64 to 9.72 | 0.798 | 0.16 | −0.25 to 0.57 | 0.447 |
| Poverty, % | −2.24 | −3.88 to −0.60 | 0.007 | 0.04 | −0.05 to 0.13 | 0.421 |
| GDP per capita | −63.17 | −117.81 to −8.52 | 0.023 | −0.19 | −4.34 to 3.97 | 0.929 |
| n | 168 | 144 | ||||
| Panel type | Random effects | Random effects | ||||
aEstimated coefficients.
bAll regressions include robust standard errors.
Discussion
During the period 2010–2016, the prevalence of CKD morbidity increased, as observed in other countries,8 and the mortality associated with CKD decreased. According to the GBD, the increase in the age-standardized prevalence rate is associated with an increase in diabetic kidney disease prevalence.8 Although there are no studies showing an increase in the prevalence of diabetes at a national level in Peru, an increase in the number of medical visits due to diabetes in public hospitals has been reported.16 However, the prevalence of CKD has not increased equally in all countries. In the USA, the prevalence of stage 1–4 CKD has stabilized over the years, as well as that of diabetic nephropathy,10 probably because of the policies in place for CKD early detection, which are less efficient in the Peruvian health system. Reversing the trend of CKD in Peru would also translate into a lower healthcare expenditure.22 We cannot rule out the possibility that the new definition of CKD and dissemination of the new guidelines in 201223 has increased the number and specificity of diagnoses and therefore caused the observed increase in prevalence.
In contrast with the global average,8 we found a decrease in mortality associated with CKD. This difference may be explained by possible underreporting of the cause of death in death records, as suggested by a previous study reporting a decrease in the coverage of causes of death in 2012–16 in Peru.24 A recent study in Peru that analysed data from 2003 to 2015 showed an increase in CKD mortality and a decrease from 2007 onward, when the MINSA started funding renal replacement therapies.20 Since the analysis of our study starts from 2010, our results might be explained by this change. A decrease in mortality of patients on hemodialysis has been also reported in Taiwan12 and the USA.25
Concerning the influence of social determinants on CKD prevalence in Peru, the positive association with the increase in the rate of health insurance coverage may be related to a greater likelihood of receiving medical care and therefore having the disease diagnosed. Indeed, the proportion of the population with access to health insurance in Peru increased from 65% in 2011 to 73% in 2015.26 Similarly, the positive association with the level of education may be related to higher self-reporting of chronic diseases such as CKD, according to the ENAHO 2011.27 Also, an association between a low level of education and an increase in chronic diseases such as CKD has been found in other countries.13,14,28,29
In our study, a higher prevalence of morbidity and mortality was associated with a lower mean age. Since diabetes and hypertension, risk factors associated with CKD and contributing 50.5% and 23.2%, respectively, to the global burden of disease,8 are occurring at a younger age in Peru,30 this might explain our findings. Similar results have been observed in other LMICs and differ from the trend in high-income countries.8
Contrary to the GBD report findings indicating that countries with a low sociodemographic index have a greater CKD prevalence compared with those with a high sociodemographic index (7.4% vs 3.1%),8 we found a lower prevalence of CKD among patients living in poverty. The same association was found in Australian Indigenous communities and among some North American populations for CKD as well as other chronic diseases.29,31 In Peru, this difference might be the result of lower self-reporting of chronic diseases by people living in poverty and extreme poverty (25.5% and 21.2%, respectively) as compared with the non-poor (40.4%), probably due to cultural aspects.25
In addition, we found that a decrease in the log-GDP per capita of the region was associated with an increase in the prevalence of CKD. The MINSA has a decentralized system for the administration and funding of healthcare services, which at the regional level is administered by the Regional Health Directorates (Direcciones Regionales de Salud).26 Poor funding of health facilities, dependent on the GDP per capita of the region, might prevent adequate screening and treatment of CKD,32 putting low-income populations at risk.33
We found a higher mortality due to CKD associated with a lower level of primary education. These results are similar to those found in a North American study reporting a lower rate of survival in people affected by chronic diseases, such as CKD, among those with a lower level of education compared with those who had finished school.24,34
Limitations
One of the limitations of this study is the use of secondary data sources, as there could be errors such as misassignment of the code, erroneous or incomplete diagnosis and errors in the recovery of cases with code N18 or subregistration of the data despite being completed by health personnel. Second, since CKD is an asymptomatic disease until a very late stage, most patients attending health centers have a severe CKD condition, whereas less severe cases are undiagnosed. Therefore the actual prevalence of CKD in Peru could be much higher than estimated. Third, due to the lack of health centeres and hemodialysis in some provinces and referral to Lima, some cases might have been erroneously attributed to that region. Moreover, findings from establishments that are part of the MINSA cannot be extrapolated to patients that are part of the social security system, which accounts for nearly 30% of the Peruvian population.17 Finally, we did not include clinical variables or other variables associated with missing social determinants of health, which could decrease the statistical significance of our findings. In spite of this, the strength of our study relies on the use of national records from the MINSA, which provides sound information on the epidemiology of CKD.
Conclusions
We determined that in Peru in 2010–2016 the prevalence of CKD increased and the mortality due to CKD decreased. We also found some social determinants associated with both prevalence and mortality, such as the level of education and the GDP per capita for each region.
Implications
Our study has some potential implications for public health in Peru. As progress has been made in the coverage of education and policyholders in Peru, the likelihood of disease self-awareness and its risk factors is increasing and, as a consequence, the reported prevalence of CKD has increased. Health education needs to be improved in the poorest population to increase self-reporting of chronic diseases. The observed increase in disease prevalence in our country must be supported by an adequate investment in health center for the diagnosis and early treatment of CKD.
Acknowledgments
None.
Contributor Information
Noé Atamari-Anahui, Universidad San Ignacio de Loyola, Vicerrectorado de Investigación, Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Avenue La Fontana 750, La Molina, Lima, Perú.
Maycol Suker Ccorahua-Rios, Asociación científica de estudiantes de medicina humana (ASOCIEMH CUSCO), Escuela de Medicina Humana, Universidad Nacional San Antonio Abad del Cusco, Avenue La Cultura 773, Cusco 08000, Perú.
Mirian Condori-Huaraka, Asociación científica de estudiantes de medicina humana (ASOCIEMH CUSCO), Escuela de Medicina Humana, Universidad Nacional San Antonio Abad del Cusco, Avenue La Cultura 773, Cusco 08000, Perú.
Yerika Huamanvilca-Yepez, Asociación científica de estudiantes de medicina humana (ASOCIEMH CUSCO), Escuela de Medicina Humana, Universidad Nacional San Antonio Abad del Cusco, Avenue La Cultura 773, Cusco 08000, Perú.
Elard Amaya, Universidad San Ignacio de Loyola, Vicerrectorado de Investigación, Centro de Excelencia en Investigaciones Económicas y Sociales en Salud, Avenue La Fontana 750, La Molina, Lima, Perú.
Percy Herrera-Añazco, Universidad San Ignacio de Loyola, Vicerrectorado de Investigación, Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Avenue La Fontana 750, La Molina, Lima, Perú.
Authors’ contributions
NA-A contributed to the design, data analysis and interpretation and writing of the first and subsequent drafts of the paper. MSC-R contributed to data analysis and interpretation and writing of the first and subsequent drafts of the paper. MC-H contributed to data analysis and interpretation and writing of the first and subsequent drafts of the paper. YH-Y contributed to data analysis and interpretation and writing of the first and subsequent drafts of the paper. EA contributed to data analysis and interpretation and writing of the first and subsequent drafts of the paper. PH-A contributed to the design, data analysis and interpretation and writing of the first and subsequent drafts of the paper.
Funding
None.
Competing interests
None declared.
Ethical approval
Not required.
References
- 1. Levey AS, Atkins R, Coresh J, et al. . Chronic kidney disease as a global public health problem: approaches and initiatives – a position statement from kidney disease improving global outcomes. Kidney Int. 2007;72(3):247–259. [DOI] [PubMed] [Google Scholar]
- 2. Coresh J. Update on the burden of CKD. J Am Soc Nephrol. 2017;28(4):1020–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nordio M, Limido A, Maggiore U, et al. . Survival in patients treated by long-term dialysis compared with the general population. Am J Kidney Dis. 2012;59(6):819–828. [DOI] [PubMed] [Google Scholar]
- 4. Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis. 2015;22(1):6–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morton RL, Schlackow I, Gray A, Emberson J, Herrington W. Impact of CKD on household income. Kidney Int Rep. 2017;3(3):610–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. George C, Mogueo A, Okpechi I, Echouffo-Tcheugui JB, Kengne AP. Chronic kidney disease in low-income to middle-income countries: the case for increased screening. BMJ Glob Health. 2017;2(2):e000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robles-Osorio ML, Sabath E. Social disparities, risk factors and chronic kidney disease. Nefrologia. 2016;36(5):577–579. [DOI] [PubMed] [Google Scholar]
- 8. Xie Y, Bowe B, Mokdad AH, et al. . Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94(3):567–581. [DOI] [PubMed] [Google Scholar]
- 9. Murphy D, McCulloch CE, Lin F, et al. . Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med. 2016;165(7):473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hsu RK, Powe NR. Recent trends in the prevalence of chronic kidney disease: not the same old song. Curr Opin Nephrol Hypertens. 2017;26(3):187–196. [DOI] [PubMed] [Google Scholar]
- 11. Shin HY, Kang HT. Recent trends in the prevalence of chronic kidney disease in Korean adults: Korean National Health and nutrition examination survey from 1998 to 2013. J Nephrol. 2016;29(6):799–807. [DOI] [PubMed] [Google Scholar]
- 12. Chang YK, Hsu CC, Chen PC, et al. . Trends of cost and mortality of patients on haemodialysis with end stage renal disease. Nephrology (Carlton). 2015;20(4):243–249. [DOI] [PubMed] [Google Scholar]
- 13. Hall YN. Social determinants of health: addressing unmet needs in nephrology. Am J Kidney Dis. 2018;72(4):582–591. [DOI] [PubMed] [Google Scholar]
- 14. Norton JM, Moxey-Mims MM, Eggers PW, et al. . Social determinants of racial disparities in CKD. J Am Soc Nephrol. 2016;27(9):2576–2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sánchez-Moreno F. El sistema nacional de salud en el Perú. Rev Peru Med Exp Salud Publica. 2014;31(4):747–753. [PubMed] [Google Scholar]
- 16. Villena JE. Diabetes mellitus in Peru. Ann Glob Health. 2015;81(6):765–775. [DOI] [PubMed] [Google Scholar]
- 17. Organización Internacional del Trabajo El sistema de salud del Perú: situación actual y estrategias para orientar la extensión de la cobertura contributiva. Lima; 2013. http://bvs.minsa.gob.pe/local/MINSA/2401.pdf. [Google Scholar]
- 18. Francis ER, Kuo CC, Bernabe-Ortiz A, et al. . Burden of chronic kidney disease in resource-limited settings from Peru: A population-based study. BMC Nephrol. 2015;16:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herrera-Añazco P, Taype-Rondan A, Lazo-Porras M, et al. . Prevalence of chronic kidney disease in Peruvian primary care setting. BMC Nephrol 2017;18:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carrillo-Larco RM, Bernabé-Ortiz A. Mortalidad por enfermedad renal crónica en el Perú: tendencias nacionales 2003–2015. Rev Peru Med Exp Salud Publica. 2018;35(3):409–415. [DOI] [PubMed] [Google Scholar]
- 21. Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005–2014. Rev Panam Salud Publica 2018;42:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Herrera- Añazco P, Pacheco-Mendoza J, Taype-Rondan A. La enfermedad renal crónica en el Perú: una revisión narrativa de los artículos científicos publicados. Acta Méd Peru. 2016;33(2):130–137. [Google Scholar]
- 23. Stevens PE, Levin A. Kidney disease: improving global outcomes chronic kidney disease guideline development work group members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–830. [DOI] [PubMed] [Google Scholar]
- 24. Vargas-Herrera J, Ruiz K, Nuñez G, et al. . Resultados preliminares del fortalecimiento del sistema informático nacional de defunciones. Rev Peru Med Exp Salud Pública. 2018;35(3):505–514. [DOI] [PubMed] [Google Scholar]
- 25. van Walraven C, Manuel DG, Knoll G. Survival trends in ESRD patients compared with the general population in the United States. Am J Kidney Dis. 2014;63(3):491–499. [DOI] [PubMed] [Google Scholar]
- 26. Lazo-Gonzales O, Alcalde-Rabanal J, Espinosa-Henao O. El sistema de salud en Perú: situación y desafíos. Lima: Colegio Médico del Perú, REP; 2016. http://web2016.cmp.org.pe/wp-content/uploads/2016/12/libroSistemaSaludPeru-.pdf [Google Scholar]
- 27. Mariños-Anticona JC. Análisis de la demanda y el acceso a los servicios de salud en el Perú. Lima: Ministerio de Salud; 2012. http://www.dge.gob.pe/publicaciones/pub_asis/asis31.pdf [Google Scholar]
- 28. Laster M, Shen JI, Norris KC. Kidney disease among African Americans: A population perspective. Am J Kidney Dis. 2018;72(5 Suppl 1):S3–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Oates GR, Jackson BE, Partridge EE, et al. . Sociodemographic patterns of chronic disease: how the mid-south region compares to the rest of the country. Am J Prev Med. 2017;52(1 Suppl 1):S31–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ramos W, López T, Revilla L, More L, Huamaní M, Pozo M. Resultados de la vigilancia epidemiológica de diabetes mellitus en hospitales notificantes del Perú, 2012. Rev Peru Med Exp Salud Publica. 2014;31(1):9–15. [PubMed] [Google Scholar]
- 31. Ritte RE, Lawton P, Hughes JT, et al. . Chronic kidney disease and socio-economic status: a cross sectional study. Ethn Health. 2017;1–17. doi: 10.1080/13557858.2017.1395814 [DOI] [PubMed] [Google Scholar]
- 32. Bellido-Zapata A, Ruiz-Muggi JE, Neira-Sánchez ER, Málaga G. Implementación y aplicación de la “Guía de práctica clínica Para el diagnóstico, tratamiento y control de la diabetes mellitus tipo 2 en el primer nivel de atención” en una red de establecimientos de salud públicos de Lima. Acta Méd Peru. 2018;35(1):14–19. [Google Scholar]
- 33. Garcia-Garcia G, Jha V, Tao Li PK, et al. . Chronic kidney disease (CKD) in disadvantaged populations. Clin Kidney J. 2015;8(1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Choi AI, Weekley CC, Chen S-C, et al. . Association of educational attainment with chronic disease and mortality: The kidney early evaluation program (KEEP). Am J Kidney Dis. 2011;58(2):228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]