Abstract
Patient: Male, 40-year-old
Final Diagnosis: Ventricular standstill
Symptoms: Seizure-like activity
Medication: —
Clinical Procedure: —
Specialty: Cardiology
Objective:
Rare disease
Background:
Transient abrupt loss of consciousness due to sudden but pronounced decrease in cardiac output caused by a change in heart rate and rhythm is termed Stokes-Adams disease. Causes of Stokes-Adams syndrome are 1) transition from normal rhythm to high grade block, 2) slowing of idioventricular rhythm in the course of complete heart block, and 3) abnormal ventricular rhythm such as ventricular tachycardia and ventricular fibrillation. Paroxysmal ventricular standstill is one of the rarest causes of Stokes-Adams attack. It is well documented that some patients with a diagnosis of epilepsy actually have a cardiac cause for their convulsions. Brevity of these episodes sometimes makes diagnosis difficult.
Case Report:
We present a case of 40-year-old builder who was normally fit and healthy who developed paroxysmal ventricular standstill. He presented to the Emergency Department with multiple episodes of seizure-like activity. Blood tests which included antibody screen were normal except for hypophosphatemia. Computed tomography head scan was normal. He was commenced on intravenous phenytoin infusion which did not abort his seizure-like episodes. Eventually, ventricular standstill was recorded on cardiac monitoring. The seizure-like episodes were determined to be Stokes-Adams attacks. He underwent transcutaneous pacing and then transvenous pacing with eventual permanent pacemaker insertion. He did not have further episodes at yearly follow-up.
Conclusions:
This case serves as a reminder of the diagnostic dilemma between syncope and seizures. Misdiagnosing cardiac dysrhythmia for epilepsy could lead to adverse consequences for the patient. It is incumbent upon the emergency physician to perform cardiac monitoring on all patients who present with syncope or convulsion in order that dysrhythmia is observed during such episode.
MeSH Keywords: Arrhythmias, Cardiac; Electrocardiography; Syncope
Background
Transient abrupt loss of consciousness due to sudden but pronounced decrease in cardiac output caused by a change in heart rate and rhythm is termed Stokes-Adams disease, coined by Huchard [1] in 1899, in honor of Stokes [2] who wrote an important paper to draw attention to this condition in 1846 and Adams [3] who described a type of this condition in 1827. Morgagni [4] was, however, one of the earliest individuals to describe this clinical condition in 1761 and in the same article described a patient with similar condition described by Gerbezius in 1719. Causes of Stoke-Adams attack include high grade atrioventricular (AV) block (i.e., complete AV block and Mobitz type II AV Block) and ventricular tachycardia while ventricular fibrillation is not often a cause of Stoke-Adams attack as it is only rarely self-terminating. Paroxysmal ventricular standstill is one of the rarest causes of Stokes-Adams attack.
Starling (1921) described a 51-year-old male with periodic Stokes-Adams syncope in ventricular standstill with unimpaired conduction between attacks [5]. Lewis in 1925 described 2 cases of intermittent ventricular standstill in patients with normal AV conduction [6]. Parkinson et al. looked at 28 reported cases and 5 recorded cases and in only one case of a 43-year-old male, was ventricular standstill followed by normal rhythm with un-impaired AV conduction [7]. Lawrence et al. (1944) presented a case of 71-year-old retired gardener who developed palpitations and multiple episodes of unconsciousness. Electrocardiography (ECG) showed paroxysmal heart block and ventricular standstill [8]. Harold Cookson, who coined the term paroxysmal ventricular standstill, reported 3 cases in 1952. Two of these had normal rhythm and conduction before and following standstill [9]. Ford and Hick [10] in 1954 described a 63-year-old man with numerous fainting spells who was found to have ventricular standstill with normal PR interval immediately before and after the episode. Robert et al. [11] in 1973 published a case report of a 60-year-old female with multiple episodes of convulsion initially started on diphenylhydantoin sodium and was noted to have transient ventricular standstill with a normal PR interval post the episode. A permanent pacemaker was eventually installed.
Leonard et al. (2002) reported a case of a 5-year-old girl referred to the Accident and Emergency Department with 3 days history of abdominal pains, intermittent fever, profuse vomiting, and brief generalized seizures, which were found to be Stokes-Adams attacks due to ventricular standstill [12]. You et al. in 2007 [13] published a case report of a 62-year-old male with dizziness and generalized seizures who was reported to have ventricular standstill with sinus rhythm and normal PR interval in between attacks. Sidhu et al. (2012) reported a case of 60-year-old healthy male who presented at the outdoor patient department with 1-year history of occasional dizziness.
His 24-hour Holter monitoring revealed ventricular arrest for 1 minute and 51 seconds. He was successfully treated with a permanent pacemaker [14]. Jaiswal et al. (2014) described a case of 50-year-old female who was admitted for nausea, vomiting, and chest pains who never had syncopal episodes and was recorded to be in ventricular standstill for more than 10 seconds [15].
Sengupta et al. in 2014 described a case of 23-year-old female at 35 weeks’ gestation who presented with worsening dyspnea, palpitations, and dizziness and was admitted until delivery for cardiac monitoring, which revealed multiple episodes of ventricular standstill and self-terminating broad complex tachycardia [16]. Lynch et al. in 2014 reported 4 cases, with age range from 14 months old to 82 years old, who all have episode of loss of consciousness attributed to ventricular standstill [17]. Khan et al. in 2016 presented a case of 49-year-old female with borderline hypokalemia who developed asymptomatic ventricular standstill and subsequent third-degree AV block following administration of intravenous (IV) erythromycin [18]. Lee et al. (2017) recorded a case of 24-year-old female who was 6-month post-partum and a known asthmatic with Takotsubo syndrome who presented to the Emergency Department with chest pains and shortness of breath. She later developed recurrent syncopal episodes which progressed to cardiac arrest and ventricular standstill was recorded on rhythm analysis [19]. Mu et al. in 2019 described a case of 70-year-old male who developed syncope after recurrent bout of dizziness who initially had a reassuring ECG but subsequently experienced paroxysmal ventricular standstill on repeat ECG tracing during an episode of syncope in the Emergency Department [20].
Case Report
A 40-year-old builder who suddenly became floppy in a sitting position while narrating a nightmare he had the night before to his work colleague. He fell face forward and lay on the ground for about 2 to 3 seconds. His colleagues thought he was play acting until they turned him over and saw he was bleeding from his forehead. He regained consciousness about a minute later. He had another episode just as they were getting him on his feet and 3 similar episodes with the ambulance crew.
In the Emergency Department, he had 10 episodes of brief periods of unresponsiveness. These were characterized by eye rolling and shaking of hands and feet. These episodes lasted approximately 30 seconds followed by 30 seconds of lying still. Subsequently, the patient would sit up in bed and try to get off and thereby requiring restraint. During his lucid period, he denied any previous similar episodes or family history of seizures. He stated he was in perfect health prior to this presentation. He denied any recreational drug use and admitted to binge drinking during weekends. Examination during a lucid period, showed a middle-aged male with bruising to the forehead. His respiratory rate (RR) was 20 breaths per minute, blood pressure (BP) was 188/96 mmHg, pulse rate (PR) 95 beats per minute, temperature 35.9°C, SaO2 100% (O/A), with normal neurological and cardiovascular examination. An impression of pseudo-seizure was made by the attending Emergency Department physician. He was connected to a cardiac monitor and given oxygen at 15 L. He had two 12-lead ECG recordings in between episodes, and both showed sinus rhythm with right bundle branch block (Figures 1, 2).
Figure 1.
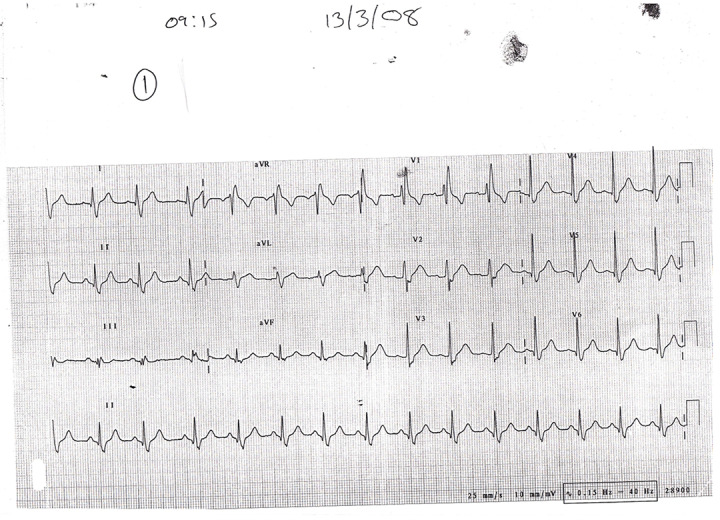
ECG on ED presentation showing Sinus rhythm and right bundle branch block. ECG – electrocardiogram; ED – Emergency Department.
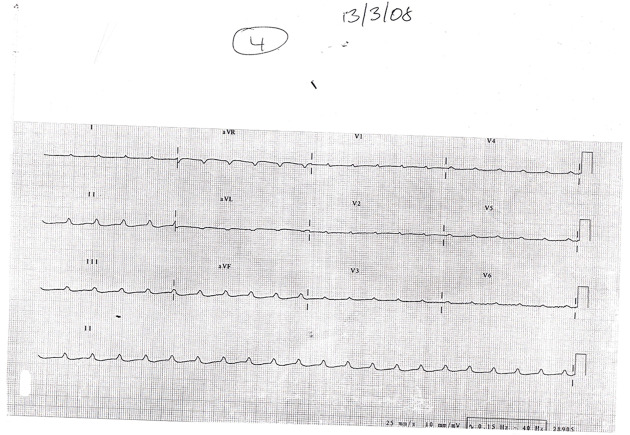
Figure 2.
Repeat ECG in the ED still showing sinus rhythm and right bundle branch block. ECG – electrocardiogram; ED – Emergency Department.
Blood tests results revealed Na+ 137 mmol/L (normal range, 133–146 mmol/L), K+ 3.7 mmol/L (normal range 3.5–5.3 mmol/L), Ca2+ 2.38 mmol/L (normal range, 2.2–2.60 mmol/L), PO4+ 0.26 mmol/L (normal range, 0.80–1.50 mmol/L), Mag2+ 0.85 mmol/L (normal range, 0.70–1.00 mmol/L), glucose 10.2 mmol/L (normal range, 3.0–7.8 mmol/L) and lactate 2.6 mmol/L (normal range, 1.3 mmol/L). Antibody screen which included vasculitis screen and connective tissue disorder were within normal limit. Hepatitis B and C with HIV tests were negative. He was commenced on a phenytoin infusion due to the numerous seizure-like attacks. A computed tomography (CT) scan of the head was requested to rule out any intracranial event. The scan result was normal and on return to the Emergency Department, he had another episode of brief loss of consciousness. A rhythm of ventricular standstill (Figure 3) was seen on the defibrillator during this episode and a 12-lead ECG was obtained towards the tail-end of his seizure-like episode. He was given IV atropine 500 mcg immediately with no effect and underwent transcutaneous pacing. Echocardiogram was normal and revealed no structural heart disease. He was transferred to a cardiac center for temporary pacing wires and eventually a permanent pacemaker insertion. The patient’s review at yearly pacemaker check revealed no further episodes.
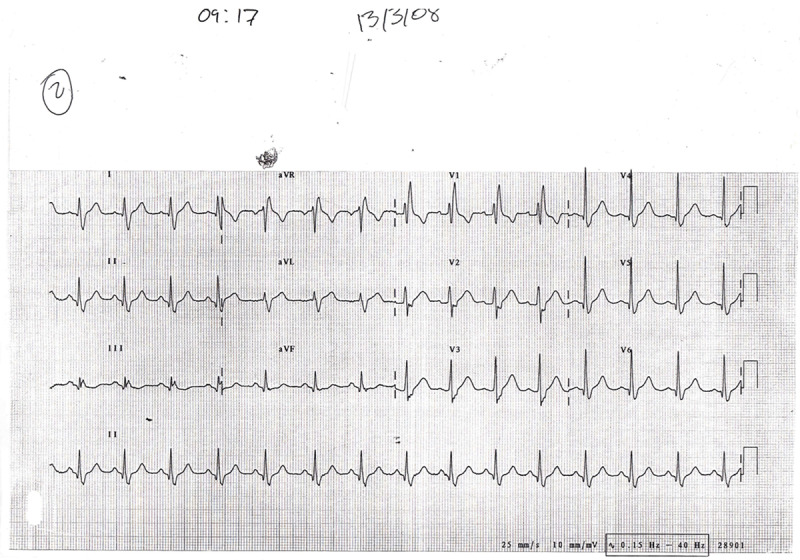
Figure 3.
ECG during seizure-like episode showing P waves with absence of ventricular conduction. ECG – electrocardiogram.
Discussion
This patient was having brief periods of ventricular standstill (Figure 3) presenting as seizure like activities. These were in fact Stokes-Adams attacks. Robert et al. [11] in 1973 and You et al. [13] in 2007 both alluded to the fact that it is possible to have ventricular standstill presenting as seizure like activity. Myoclonus or convulsion can occur after an episode of syncope referred to as convulsive syncope. Zaidi et al. [21] in 2000 reported that 20% to 30% of epileptics are misdiag-nosed. Mohler in 1923 observed that when ventricular standstill is greater than 16 to 18 seconds, convulsion occurs [22]. The prevalence of ventricular standstill is unclear. In many cases, ventricular standstill occurs in people with structural heart disease but may also occur without a pre-existing cardiac condition. The causes of ventricular standstill can be broadly divided into primary and secondary. Primary ventricular standstill is caused by conditions such as myocarditis, acute coronary syndrome, and cardiomyopathy (e.g., arrhythmogenic right ventricular cardiomyopathy). Secondary ventricular standstill is caused by hypoxia, acidosis, hypokalemia, hyperkalemia, hypothermia, massive pulmonary embolism, antiarrhythmic drugs such as adenosine, cocaine overdose, or induced by tachycardia pause. Epileptic seizures can affect the heart rate leading to arrhythmia [23]. The most common arrhythmia associated with epilepsy is ictal tachycardia (80% to 100% of all seizures) [24]. Ictal bradycardia occurs in fewer than 6% of seizures. This slowing of the heart rate may be severe enough to cause ictal asystole.
Ictal asystole is an important differential diagnosis to ventricular standstill which must be recognized by neurologists, cardiologists, and emergency physicians. Ictal asystole is defined as the absence of ventricular complexes for more than 4 seconds accompanied by electrographic seizure onset [25]. Most recent studies define ictal asystole as an R-R interval longer than 3 seconds It is a rare condition usually associated with temporal lobe epilepsy. The exact mechanism of ictal asystole is not fully understood but may be due to involvement of the central autonomic network which controls parasympathetic and sympathetic output or alternatively involvement of vasovagal reflex pathway [26,27]. Ictal asystole can lead to sudden unexpected death. Simultaneous ECG and video-electroencephalogram (EEG) monitoring are essential for diagnosis [28]
Ventricular standstill often occurs in relation to conduction blocks though it can occur without them. Once discovered, ventricular standstill requires immediate treatment. Treatment usually requires temporary pacing wires and eventually permanent pacemaker insertion. There is no clinical guideline to guide appropriate intervention for ventricular standstill.
Conclusion
This case serves as a reminder of the diagnostic dilemma between syncope and seizures. Misdiagnosing cardiac dysrhythmia for epilepsy could lead to adverse consequences for the patient. Our case was slightly more challenging due to seizure like activity in the patient. It is incumbent upon the emergency physician to perform cardiac monitoring on all patients who present with syncope or convulsion in order that dysrhythmia is observed during such episode. The brevity of these episodes may sometimes make such diagnosis difficult.
Footnotes
Department and Institution where work was done
Emergency Department, University College London Hospital, London, U.K.
Conflict of interest
None.
References:
- 1.Huchard H. [Clinical treatment of heart and aortic diseases.] 3rd ed. Paris: Octave Doin; 1899. [in French] [Google Scholar]
- 2.Stokes W. Observations of some cases of permanently slow pulse. Dublin Q J Med Sci. 1846;11:73–8. [Google Scholar]
- 3.Adams R. Cases of diseases of the heart accompanied with pathological observations. Dublin Hosp Rep. 1827;4:353–53. [Google Scholar]
- 4.Morgagni GB. [The seats and causes of diseases investigated by anatomy.] (Translated by B Alexander) Venezia. 1761;3:54. [in Latin] [Google Scholar]
- 5.Starling HJ. Heart block influenced by the vagus. Heart. 1921;8:31. [Google Scholar]
- 6.Lewis T. The mechanism and graphic registration of the heart beat. 3rd ed. London: Shaw and Sons; 1925. p. 421. [Google Scholar]
- 7.Parkinson J, Papp C, Evans W. The electrocardiogram of Stokes-Adams attack. Br Heart J. 1941;3:171–99. doi: 10.1136/hrt.3.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrence JS, Forbes GW. Paroxysmal heart block and ventricular standstill. Br Heart J. 1944;6(2):53–60. doi: 10.1136/hrt.6.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cookson H. Paroxysmal ventricular standstill. Br Heart J. 1952;14:350–56. doi: 10.1136/hrt.14.3.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hick FK. Stokes-Adams seizures: Case report of paroxysmal ventricular standstill and its production by carotid sinus pressure. Circulation. 1954;9:857–59. doi: 10.1161/01.cir.9.6.857. [DOI] [PubMed] [Google Scholar]
- 11.Haslam RH, Jameson HD. Cardiac standstill simulating repeated epileptic attacks. JAMA. 1973;224:887–89. [PubMed] [Google Scholar]
- 12.Leonard PA, Burns JE. Failure to recognise ventricular standstill. Emerg Med J. 2002;19:86–87. doi: 10.1136/emj.19.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.You CF, Chong CF, Wang TL, et al. Unrecognized paroxysmal ventricular standstill masquerading as epilepsy: A Stokes-Adams attack. Epileptic Disord. 2007;9(2):179–81. doi: 10.1684/epd.2007.0105. [DOI] [PubMed] [Google Scholar]
- 14.Sidhu M, Singh HP, Chopra AK, et al. Surviving ventricular standstill for 111 seconds during Holter Monitoring. Ann Noninvasive Electrocardiol. 2012;17(1):61–62. doi: 10.1111/j.1542-474X.2011.00482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaiswal S, Aldave APN, Wool KJ. Ventricular standstill: An uncommon electrophysiological abnormality caused by profound vagal tone. N Am J Med Sci. 2014;6(4):178–80. doi: 10.4103/1947-2714.131245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sengupta A, Slater TA, Sainsbury PA. The investigation and management of broad complex tachycardia and ventricular standstill presenting in pregnancy: A case report. Obstet Med. 2014;7(3):131–34. doi: 10.1177/1753495X14539679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynch RM, Ballesty L, Maicoo R. “Be still my beating heart”: Ventricular standstill occurring in different age groups. Afr J Emerg Med. 2014;4(4):e12–15. [Google Scholar]
- 18.Khan S, Ramzy J, Papachristos D, et al. Ventricular standstill following intravenous Erythromycin and borderline hypokalemia. Eur J Case Rep Intern Med. 2016;3(3):375. doi: 10.12890/2016_000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee N, Lee KW, D’Ambrosio MM, et al. Takotsubo syndrome-associated ventricular standstill in a peripartum patient: Case report and review of the literature. Clin Case Rep. 2017;6(2):283–87. doi: 10.1002/ccr3.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mu Y, Supino M. Elusive cardiac dysrhythmia in high-risk syncope. Am J Emerg Med. 2019;37(10):1992.e1–e3. doi: 10.1016/j.ajem.2019.158381. [DOI] [PubMed] [Google Scholar]
- 21.Zaidi A, Clough P, Cooper P. Misdiagnosis of epilepsy: Many seizure-like attacks have a cardiovascular cause. J Am Coll Cardiol. 2000;36:181–84. doi: 10.1016/s0735-1097(00)00700-2. [DOI] [PubMed] [Google Scholar]
- 22.Mohler H. Adams-Stokes syndrome, heart block in association with diabetes. Circulation. 1923;81:1324–45. [Google Scholar]
- 23.Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia. 2000;41(5):542–48. doi: 10.1111/j.1528-1157.2000.tb00207.x. [DOI] [PubMed] [Google Scholar]
- 24.Sevcencu C, Struijk JJ. Autonomic alteration and cardiac changes in epilepsy. Epilepsia. 2010;51(5):725–37. doi: 10.1111/j.1528-1167.2009.02479.x. [DOI] [PubMed] [Google Scholar]
- 25.Moseley BD, Ghearing GR, Munger TM, Britton JW. The treatment of ictal asystole with cardiac pacing. Epilepsia. 2011;52(4):e16–19. doi: 10.1111/j.1528-1167.2010.02972.x. [DOI] [PubMed] [Google Scholar]
- 26.Van der Lende M, Surges R, Sander JW, Thijs RD. Cardiac arrhythmia during or after epileptic seizures. J Neurol Neurosurg Psychiatry. 2016;87:69–74. doi: 10.1136/jnnp-2015-310559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palma J-A, Benarroch EE. Neural control of the heart: Recent concepts and clinical correlations. Neurology. 2014;83:261–71. doi: 10.1212/WNL.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 28.Kishk N, Nawito A, El-Damaty A, Ragab A. Ictal asystole: Acase presentation. BMC Neurol. 2018;18(1):100. doi: 10.1186/s12883-018-1105-5. [DOI] [PMC free article] [PubMed] [Google Scholar]