Abstract
Objectives
This study aims to investigate the rate of type D personality in Turkish patients with fibromyalgia (FM) and evaluate its associations with clinical parameters of FM as well as its effects on health-related quality of life (HRQoL).
Patients and methods
The study included 100 patients with FM (14 males, 86 females; mean age 34.6±7.4 years; range, 22 to 49 years) fulfilling 1990 American College of Rheumatology diagnostic criteria and 50 healthy controls (9 males, 41 females; mean age 32.6±6.5 years; range, 21 to 50 years). Type D personality was assessed using the type D scale-14 (DS-14). FM disease severity was determined by Fibromyalgia Impact Questionnaire (FIQ), functional status by Stanford Health Assessment Questionnaire (HAQ), and HRQoL by Nottingham Health Profile (NHP). Severity of pain and fatigue were measured by visual analog scale (VAS).
Results
The frequency of type D personality was 33% in FM patients and 12% in controls (odds ratio=3.612, 95% confidence interval 1.398-9.333) (p=0.006). Type D FM patients scored higher in tender point count (TPC), FIQ, HAQ, VAS-pain and all NHP subgroups except energy (p<0.01). Type D personality was found to be correlated with FIQ, TPC, HAQ, VAS-pain and NHP subgroups except energy (p<0.01).
Conclusion
Based on our findings, assessment of personality characteristics of patients with FM may hold the key for the treatment of the disease. Besides, a better understanding of personality-related pain in FM patients may provide a more targeted approach to pain treatment.
Keywords: Fibromyalgia, pain, personality, quality of life
Introduction
Fibromyalgia (FM) is a common disorder characterized by unexplained widespread pain associated with ‘tender points’ which tend to be painful to touch.[1] Its pathogenesis has been thought as an altered processing of pain arising from neuroendocrine, neurotransmitter and sleep perturbation.[2,3] Although the main symptom of FM is pain, patients may also experience additional symptoms such as fatigue, depression, sleep disorders, stiffness, headache, dizziness, muscle spasms and paresthesia.[4,5] In epidemiological studies, the prevalence of FM in general population was reported to range from 7.3 to 12.9%.[6] In previous researches, it has been found to be linked with various psychiatric disorders including depression,[7,8] anxiety,[9,10] post-traumatic stress disorder,[11] alexithymia,[12,13] panic disorder,[14] migraine,[15,16] restless leg syndrome[17] and irritable bowel syndrome.[18] Furthermore, psychological symptoms were found to be associated with disease severity, poor physical fitness and deterioration in quality of life (QoL) in the patients with FM.[19]
Type D personality is a distressed personality type involving two personality traits, namely negative affectivity and social inhibition, which are described as tendency to experience negative emotions and to inhibit self-expression in social relationships, respectively.[20] Individuals with negative affectivity commonly concentrate on negative aspects of life and are likely to experience negative feelings such as distress, dissatisfaction, irritability, anxiety and depression.[21] Socially inhibited individuals tend to feel unsafe and vulnerable in social interactions. The prevalence of type D personality is 21% in the general population and increases in cardiovascular diseases such as coronary heart disease and hypertension.[22] In previous studies, type D personality was reported to be associated with poor clinical outcomes in ischemic heart disease,[23] cardiac arrhythmias,[24] and peripheral arterial disease.[25] Although there are sufficient numbers of studies focusing on the relationship between type D personality and cardiovascular diseases; few data are available on the role of type D personality on FM.
We hypothesized that FM might be associated with type D personality. we aimed to investigate the rate of type D personality in Turkish patients with FM and evaluate its associations with clinical parameters of FM as well as its effects on health- related quality of life (HRQoL).
Patients and Methods
The study included 100 patients with FM (14 males, 86 females; mean age 34.6±7.4 years; range, 22 to 49 years) applying to physical medicine and rehabilitation clinics of Derince Training and Research Hospital and Medipol University Esenler Hospital, between December 2015 and May 2016. FM was diagnosed based on 1990 American College of Rheumatology diagnostic criteria:[26] (i) chronic pain which occurs on both sides of the body, both axial and peripheral, below and above the waist; (ii) minimum 11 of 18 tender points with digital palpation with an approximate force of 4 kg/cm[2]. Tender point count (TPC) was measured by the same physician. Control group included 50 age and sex-matched healthy subjects (9 males, 41 females; mean age 32.6±6.5 years; range, 21 to 50 years). Exclusion criteria for both patients and controls were inflammatory rheumatic diseases such as rheumatoid arthritis, ankylosing spondylitis, Sjögren’s syndrome; endocrine diseases such as diabetes mellitus, thyroid and parathyroid disorders, and malignancies. Disease severity was determined by Fibromyalgia Impact Questionnaire (FIQ).[27] Functional status was evaluated by Stanford Health Assessment Questionnaire (HAQ),[28] and HRQoL by Nottingham Health Profile (NHP).[29] Severity of pain and fatigue was measured by using 10-cm visual analog scale (VAS).[30]
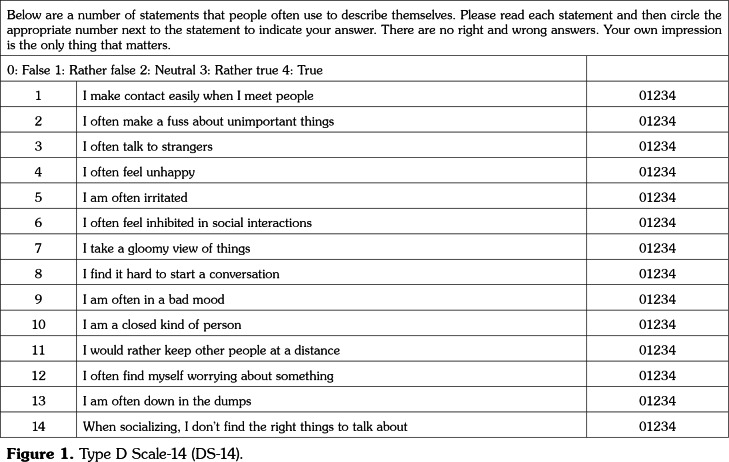
Type D personality was assessed by a psychiatrist using the Turkish version of type D scale-14 (DS-14).[31] DS-14 (Figure 1) was developed in 2005 by Denollet[22] as a measure of negative affectivity and social inhibition in order to be used in epidemiologic and clinical studies. It includes two subscales which assess negative affectivity and social inhibition. Each subscale consists of seven items and each item is scored between 0 and 4. Scores ≥10 in negative affectivity and social inhibition subscales indicate type D personality. FM patients were divided into two groups as type D and non-type D patients.
The study protocol was approved by the Kocaeli University Medical School Ethics Committee. A written informed consent was obtained from each participant. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Figure 1. Type D Scale-14 (DS-14).
Statistical analysis
Statistical analyses were carried out using IBM SPSS for Windows, version 21.0 (IBM Inc., Armonk, NY, USA). Descriptive statistics (mean, median, standard deviation, minimum, maximum and frequencies) were used for assessing the demographics and clinical parameters. Differences among groups were evaluated by using independent samples t-test. Chi-square test was used to compare groups of categorical variables. The presence of correlation was determined by Pearson’s correlation coefficient. P values <0.01 were considered statistically significant.
Results
Age did not significantly differ between FM patients and healthy controls (p=0.096). Demographic and clinical patient data are given in Table 1. According to DS-14, the frequency of type D personality was 33% in FM patients and 12% in healthy controls (odds ratio=3.612, 95% confidence interval 1.398-9.333) (p=0.006) (Table 2).
Table 1. Demographic and clinical patient data.
| Mean±SD | Min-Max | |
| Age (year) | 34.6±7.4 | 22-49 |
| Pain (VAS, 10 cm) | 6.7±1.7 | 4-10 |
| Fatigue (VAS, 10 cm) | 4.2±3.4 | 0-10 |
| Tender point count | 13.8±2.4 | 11-18 |
| FIQ | 71.4±14.9 | 43-100 |
| HAQ | 0.8±0.7 | 0-3 |
| NHP-pain | 72.5±17.5 | 25-100 |
| NHP-physical mobility | 32.8±24.5 | 0-75 |
| NHP-energy | 40.0±41.4 | 0-100 |
| NHP-sleep | 64.1±24.2 | 0-100 |
| NHP-social isolation | 30.4±36.3 | 0-100 |
| NHP-emotional reactions | 61.9±27.2 | 0-100 |
| SD: Standard deviation; Min: Minimum; Max: Maximum; VAS: Visual analog scale; FIQ: Fibromyalgia Impact Questionnaire; HAQ: Stanford Health Assessment Questionnaire; NHP: Nottingham Health Profile. | ||
Table 2. Prevalence of type D personality in fibromyalgia patients and controls.
| n | % | Difference | 95% Confidence | p | |
| Fibromyalgia patients (n=100) | 33 | 33 | 3,612 | 1.4-9.3 | 0.006* |
| Healthy controls (n=50) | 6 | 12 | |||
| CI: Confidence interval; * p<0.01 was considered statistically significant | |||||
A comparison of type D (n=33) and non- type D FM patients (n=67) showed that type D FM patients scored significantly higher in TPC, FIQ, HAQ, VAS-pain, and all NHP subgroups except energy (p<0.01). There was no statistically significant difference in VAS-fatigue among groups (p>0.01) (Table 3).
Table 3. Comparison of clinical variables and HRQoL between type D and non-type D fibromyalgia patients.
| Type D FM patients (n=33) | Non-type D FM patients (n=67) | p | |
| Mean±SD | Mean±SD | ||
| Pain (VAS, 10 cm) | 8.6±0.8 | 5.8±1.2 | <0.00001* |
| Fatigue (VAS, 10 cm) | 4.5±3.2 | 4.0±3.5 | 0.6 |
| Tender point count | 15.7±2.3 | 12.9±1.9 | <0.00001* |
| Fibromyalgia impact questionnaire | 86.3±8.4 | 64.1±11.4 | <0.00001* |
| Stanford health assessment questionnaire | 1.2±0.8 | 0.5±0.5 | <0.00001* |
| NHP-pain | 89.2±10.7 | 64.3±14.1 | <0.00001* |
| NHP-physical mobility | 53.4±16.9 | 22.6±21.0 | <0.00001* |
| NHP-energy | 45.5±42.1 | 37.3±41.1 | 0.358 |
| NHP-sleep | 80.0±19.4 | 56.2±22.6 | <0.00001* |
| NHP-social isolation | 60.6±37.2 | 15.5±25.1 | <0.00001* |
| NHP-emotional reactions | 83.7±14.1 | 51.5±25.1 | <0.00001* |
| HRQoL: Health-related quality of life; FM: Fibromyalgia; SD: Standard deviation; VAS: Visual analog scale; NHP: Nottingham Health Profile; * p<0.01 was considered statistically significant. | |||
Negative affectivity and social inhibition were found to be significantly correlated with TPC, FIQ, HAQ, VAS-pain and all NHP subgroups except energy (p<0.01). When the correlation coefficients were analyzed, both negative affectivity and social inhibition showed the highest correlation with VAS-pain. There was no statistically significant correlation between negative affectivity and social inhibition and VAS-fatigue (p>0.01) (Table 4).
Table 4. Correlation of type DS-14 components with clinical parameters and HRQoL.
| Negative affectivity | Social inhibition | ||
| Pain (VAS, 10 cm) | r | 0.801 | 0.777 |
| p | <0.00001* | <0.00001* | |
| Fatigue (VAS, 10 cm) | r | 0.138 | 0.071 |
| p | 0.170 | 0.483 | |
| Tender point count | r | 0.624 | 0.555 |
| p | <0.00001* | <0.00001* | |
| Fibromyalgia impact questionnaire | r | 0.758 | 0.703 |
| p | <0.00001* | <0.00001* | |
| Stanford health assessment questionnaire | r | 0.615 | <0.00001* |
| p | 0.626 | <0.00001* | |
| NHP-pain | r | 0.691 | 0.676 |
| p | <0.00001* | <0.00001* | |
| NHP-physical mobility | r | 0.667 | 0.554 |
| p | <0.00001* | <0.00001* | |
| NHP-energy | r | 0.151 | 0.128 |
| p | 0.135 | 0.205 | |
| NHP-sleep | r | 0.470 | 0.494 |
| p | <0.00001* | <0.00001* | |
| NHP-social isolation | r | 0.533 | 0.692 |
| p | <0.00001* | <0.00001* | |
| NHP-emotional reactions | r | 0.684 | 0.568 |
| p | <0.00001* | <0.00001* | |
| DS-14: Type D scale-14; HRQoL: Health-related quality of life; VAS: Visual analog scale; NHP: Nottingham Health Profile; * p<0.01 was considered statistically significant. | |||
Discussion
Type D personality is based on two stable personality traits: negative affectivity and social inhibition.[20] Previous studies have suggested that patients with FM have negative affectivity[32] and poor social QoL.[33] However, to our knowledge, there are only two studies in the literature examining the frequency of type D personality in patients with FM. In a 559-case cross-sectional study from Netherlands, the prevalence of type D personality in patients with FM was reported to be 56%.[34] In another study performed in Israel, 30% of FM patients were found to have type D personality.[35] In the present study, 33% of FM patients were found to have Type D personality; this rate was significantly higher than that of healthy controls (12%). In previous studies, the frequency of type D personality construct in Turkey was described as follows: 27.7% in hemodialysis patients[31] and 56.8% in patients with multiple sclerosis.[36] Our study has demonstrated that type D personality trait is common among Turkish patients with FM. To the best of our knowledge, this is the first study to report the rate of type D personality in Turkish FM patients.
In our study, type D FM patients showed poorer HRQoL in terms of pain, physical mobility, sleep, and social and emotional functions and more impairment in functional status compared to non-type D FM patients. Moreover, negative affectivity and social inhibition were found to be correlated with HAQ and all HRQoL domains except energy in FM patients. Similarly, in a study of van Middendorp et al.,[34] type D personality was reported to be associated with worse mental health and poor QoL regarding social and emotional functioning. Additional studies have also confirmed the negative impact of type D personality on HRQoL in other diseases. In a study of Mols and Denollet[37] conducted on patients with chronic pain, chronic lung diseases, sleep disorders, traumatic brain injury, vertigo, melanoma and diabetic ulcers, a significant relationship was found between type D personality and poor physical and mental health status. Moreover, Schiffer et al.[38] conducted a prospective study on patients with chronic heart failure to investigate the impact of type D personality and its stability over time on health status. They found more improvement in health status over time in non-type D patients as compared to type D patients. On the other hand, Erkol Inal et al.[39] reported an association between type D personality trait and mental domains of HRQoL in Turkish patients with ankylosing spondylitis.
In the present study, FM patients with this type of personality showed higher disease severity compared to non-type D subjects. Moreover, negative affectivity and social inhibition were found to be correlated with FIQ and TPC levels. To the best of our knowledge, this study is the first to demonstrate an association between type D personality and disease severity in the patients with FM. Possible mechanisms that may explain poor clinical outcomes in type D FM patients include dysregulation of hypothalamic-pituitary- adrenal axis,[40] tumor necrosis factor-alpha (TNF-α) dysregulation[41] and increased oxidative stress in cardiac diseases.[23] Since elevated levels of TNF-α,[42] hypothalamic-pituitary-adrenal axis disturbances,[43] and oxidative stress[44] also play a role in the onset and continuation of FM; these pathways may also explain the relationship between type D personality and disease severity in the patients with FM. Besides, non-adherence to medication and reluctance to contact a healthcare provider may be additional factors in this relation.[40]
In the current study, VAS-pain scores of FM patients with type D personality were higher than those of non-type D patients. Additionally, negative affectivity and social inhibition showed the strongest correlation with pain severity among clinical parameters. The relationship between negative affectivity and pain is explained by psychological aspects of pain perception.[45] Emotional factors modulate pain perception via various pathways including projections from the midbrain periaqueductal grey to brainstem nuclei, including the rostroventral medulla and locus coeruleus, to the dorsal horn of the spinal cord. These tracts comprehend opioids, norepinephrine and serotonin, and have inhibitory and excitatory effects on medulla spinalis afferent projection neurons. Outputs from anterior cingulate cortex, prefrontal cortex, and amygdala reach periaqueductal grey, indicating that these descending systems might be stimulated by emotional factors.[45] Further studies conducted on patients with other chronic pain syndromes are required to elucidate the relationship between type D personality and pain.
We found no difference in VAS-fatigue and NHP-energy scores of type D and non-type D patients with FM. Also, no significant correlation existed between VAS-fatigue and negative affectivity or social inhibition. These findings indicate that type D personality components, namely negative affectivity and social inhibition, are mainly linked with pain, but not fatigue symptoms in patients with FM.
This study has two limitations. First is the relatively small study sample, while second is the cross sectional design of the study which is inadequate to reflect the changes in parameters and to detect cause-and-effect relationships.
In conclusion, type D personality is prevalent among Turkish patients with FM, with a rate of 33%. It is associated with poor HRQoL regarding pain, physical mobility, sleep, and social and emotional functions. Presence of type D personality should be taken into account in FM to develop new treatment strategies for patients who have inadequate response to conventional therapies. In case of type D personality in a FM patient, we should be in collaboration with a psychiatrist. Besides medical therapy, group therapies including both cognitive-behavioral approaches and exercises may be considered in this process.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Hudson JI, Goldenberg DL, Pope HG Jr, Keck PE Jr, Schlesinger L. Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med. 1992;92:363–367. doi: 10.1016/0002-9343(92)90265-d. [DOI] [PubMed] [Google Scholar]
- 2.Perrot S, Winkelmann A, Dukes E, Xu X, Schaefer C, Ryan K, et al. Characteristics of patients with fibromyalgia in France and Germany. Int J Clin Pract. 2010;64:1100–1108. doi: 10.1111/j.1742-1241.2010.02418.x. [DOI] [PubMed] [Google Scholar]
- 3.Tomasevic-Todorovic S, Pjevic M, Boskovic K. Fibromyalgia-up to date aspects of pathophysiology diagnosis and treatment. Med Pregl. 2010;63:507–511. doi: 10.2298/mpns1008507t. [DOI] [PubMed] [Google Scholar]
- 4.Martinez JE, Casagrande Pde M, Ferreira PP, Rossatto BL. Correlation between demographic and clinical variables and fibromyalgia severity. Rev Bras Reumatol. 2013;53:460–463. doi: 10.1016/j.rbr.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Jones CJ, Rutledge DN, Aquino J. Predictors of physical performance and functional ability in people 50+ with and without fibromyalgia. J Aging Phys Act. 2010;18:353–368. doi: 10.1123/japa.18.3.353. [DOI] [PubMed] [Google Scholar]
- 6.Neumann L, Buskila D. Epidemiology of fibromyalgia. Curr Pain Headache Rep. 2003;7:362–368. doi: 10.1007/s11916-003-0035-z. [DOI] [PubMed] [Google Scholar]
- 7.Offenbaecher M, Glatzeder K, Ackenheil M. Self- reported depression, familial history of depression and fibromyalgia (FM), and psychological distress in patients with FM. Z Rheumatol. 1998;57:94–96. doi: 10.1007/s003930050245. [DOI] [PubMed] [Google Scholar]
- 8.Chang MH, Hsu JW, Huang KL, Su TP, Bai YM, Li CT, et al. Bidirectional Association Between Depression and Fibromyalgia Syndrome: A Nationwide Longitudinal Study. J Pain. 2015;16:895–902. doi: 10.1016/j.jpain.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Janssens KA, Zijlema WL, Joustra ML, Rosmalen JG. Mood and Anxiety Disorders in Chronic Fatigue Syndrome, Fibromyalgia, and Irritable Bowel Syndrome: Results From the LifeLines Cohort Study. Psychosom Med. 2015;77:449–457. doi: 10.1097/PSY.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 10.Thieme K, Turk DC, Flor H. Comorbid depression and anxiety in fibromyalgia syndrome: relationship to somatic and psychosocial variables. Psychosom Med. 2004;66:837–844. doi: 10.1097/01.psy.0000146329.63158.40. [DOI] [PubMed] [Google Scholar]
- 11.Cohen H, Neumann L, Haiman Y, Matar MA, Press J, Buskila D. Prevalence of post-traumatic stress disorder in fibromyalgia patients: overlapping syndromes or post-traumatic fibromyalgia syndrome. Semin Arthritis Rheum. 2002;32:38–50. doi: 10.1053/sarh.2002.33719. [DOI] [PubMed] [Google Scholar]
- 12.Avila LA, de Araujo Filho GM, Guimarães EF, Gonçalves LC, Paschoalin PN, Aleixo FB. Characterization of the pain, sleep and alexithymia patterns of patients with fibromyalgia treated in a Brazilian tertiary center. Rev Bras Reumatol. 2014;54:409–413. doi: 10.1016/j.rbr.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 13.Castelli L, Tesio V, Colonna F, Molinaro S, Leombruni P, Bruzzone M, et al. Alexithymia and psychological distress in fibromyalgia: prevalence and relation with quality of life. Clin Exp Rheumatol. 2012;30:70–77. [PubMed] [Google Scholar]
- 14.Malt EA, Berle JE, Olafsson S, Lund A, Ursin H. Fibromyalgia is associated with panic disorder and functional dyspepsia with mood disorders. A study of women with random sample population controls. J Psychosom Res. 2000;49:285–289. doi: 10.1016/s0022-3999(00)00139-2. [DOI] [PubMed] [Google Scholar]
- 15.Vij B, Whipple MO, Tepper SJ, Mohabbat AB, Stillman M, Vincent A. Frequency of Migraine Headaches in Patients With Fibromyalgia. Headache. 2015;55:860–865. doi: 10.1111/head.12590. [DOI] [PubMed] [Google Scholar]
- 16.Marcus DA, Bhowmick A. Fibromyalgia comorbidity in a community sample of adults with migraine. Clin Rheumatol. 2013;32:1553–1556. doi: 10.1007/s10067-013-2310-7. [DOI] [PubMed] [Google Scholar]
- 17.Yunus MB, Aldag JC. Restless legs syndrome and leg cramps in fibromyalgia syndrome: a controlled study. BMJ. 1996;312:1339–1339. doi: 10.1136/bmj.312.7042.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sivri A, Cindaş A, Dinçer F, Sivri B. Bowel dysfunction and irritable bowel syndrome in fibromyalgia patients. Clin Rheumatol. 1996;15:283–286. doi: 10.1007/BF02229708. [DOI] [PubMed] [Google Scholar]
- 19.Del Pozo-Cruz J, Alfonso-Rosa RM, Castillo-Cuerva A, Sañudo B, Nolan P, Del Pozo-Cruz B. Depression symptoms are associated with key health outcomes in women with fibromyalgia: a cross-sectional study. Int J Rheum Dis. 2017;20:798–808. doi: 10.1111/1756-185X.12564. [DOI] [PubMed] [Google Scholar]
- 20.Denollet J. Type D personality. A potential risk factor refined. J Psychosom Res. 2000;49:255–266. doi: 10.1016/s0022-3999(00)00177-x. [DOI] [PubMed] [Google Scholar]
- 21.Mikkelsen EG, Einarsen S. Relationships between exposure to bullying at work and psychological and psychosomatic health complaints: the role of state negative affectivity and generalized self-efficacy. Scand J Psychol. 2002;43:397–405. doi: 10.1111/1467-9450.00307. [DOI] [PubMed] [Google Scholar]
- 22.Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005;67:89–97. doi: 10.1097/01.psy.0000149256.81953.49. [DOI] [PubMed] [Google Scholar]
- 23.Kupper N, Gidron Y, Winter J, Denollet J. Association between type D personality, depression, and oxidative stress in patients with chronic heart failure. Psychosom Med. 2009;71:973–980. doi: 10.1097/PSY.0b013e3181bee6dc. [DOI] [PubMed] [Google Scholar]
- 24.Denollet J, Tekle FB, van der Voort PH, Alings M, van den Broek KC. Age-related differences in the effect of psychological distress on mortality: Type D personality in younger versus older patients with cardiac arrhythmias. Biomed Res Int. 2013;2013:246035–246035. doi: 10.1155/2013/246035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aquarius AE, Denollet J, de Vries J, Hamming JF. Poor health-related quality of life in patients with peripheral arterial disease: type D personality and severity of peripheral arterial disease as independent predictors. J Vasc Surg. 2007;46:507–512. doi: 10.1016/j.jvs.2007.04.039. [DOI] [PubMed] [Google Scholar]
- 26.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 27.Sarmer S, Ergin S, Yavuzer G. The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol Int. 2000;20:9–12. doi: 10.1007/s002960000077. [DOI] [PubMed] [Google Scholar]
- 28.Küçükdeveci AA, Sahin H, Ataman S, Griffiths B, Tennant A. Issues in cross-cultural validity: example from the adaptation, reliability, and validity testing of a Turkish version of the Stanford Health Assessment Questionnaire. Arthritis Rheum. 2004;51:14–19. doi: 10.1002/art.20091. [DOI] [PubMed] [Google Scholar]
- 29.Kücükdeveci AA, McKenna SP, Kutlay S, Gürsel Y, Whalley D, Arasil T. The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res. 2000;23:31–38. doi: 10.1097/00004356-200023010-00004. [DOI] [PubMed] [Google Scholar]
- 30.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 31.Alçelik A, Yıldırım O, Canan F, Eroğlu M, Aktaş G, Şavlı H. Preliminary psychometric evaluation of the type D personality construct in Turkish hemodialysis patients. J Mood Dis. 2012;2:1–5. [Google Scholar]
- 32.Staud R, Robinson ME, Vierck CJ Jr, Cannon RC, Mauderli AP, Price DD. Ratings of experimental pain and pain-related negative affect predict clinical pain in patients with fibromyalgia syndrome. Pain. 2003;105:215–222. doi: 10.1016/s0304-3959(03)00208-2. [DOI] [PubMed] [Google Scholar]
- 33.Verbunt JA, Pernot DH, Smeets RJ. Disability and quality of life in patients with fibromyalgia. Health Qual Life Outcomes. 2008;6:8–8. doi: 10.1186/1477-7525-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Middendorp H, Kool MB, van Beugen S, Denollet J, Lumley MA, Geenen R. Prevalence and relevance of Type D personality in fibromyalgia. Gen Hosp Psychiatry. 2016;39:66–72. doi: 10.1016/j.genhosppsych.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Ablin JN, Zohar AH, Zaraya-Blum R, Buskila D. Distinctive personality profiles of fibromyalgia and chronic fatigue syndrome patients. e2421PeerJ. 2016;4 doi: 10.7717/peerj.2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demirci S, Demirci K, Demirci S. The effect of type d personality on quality of life in patients with multiple sclerosis. Noro Psikiyatr Ars. 2017;54:272–276. doi: 10.5152/npa.2016.12764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mols F, Denollet J. Type D personality among noncardiovascular patient populations: a systematic review. Gen Hosp Psychiatry. 2010;32:66–72. doi: 10.1016/j.genhosppsych.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 38.Schiffer AA, Pedersen SS, Widdershoven JW, Denollet J. Type D personality and depressive symptoms are independent predictors of impaired health status in chronic heart failure. Eur J Heart Fail. 2008;10:802–810. doi: 10.1016/j.ejheart.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 39.Erkol İnal E, Demirci K, Doğru A, Şahin M. Ankylosing Spondylitis patients with Type D personality have worse clinical status. Mod Rheumatol. 2016;26:138–145. doi: 10.3109/14397595.2015.1054098. [DOI] [PubMed] [Google Scholar]
- 40.Denollet J, Conraads VM. Type D personality and vulnerability to adverse outcomes in heart disease. Cleve Clin J Med. 2011;78:13–19. doi: 10.3949/ccjm.78.s1.02. [DOI] [PubMed] [Google Scholar]
- 41.Denollet J, Vrints CJ, Conraads VM. Comparing Type D personality and older age as correlates of tumor necrosis factor-alpha dysregulation in chronic heart failure. Brain Behav Immun. 2008;22:736–743. doi: 10.1016/j.bbi.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 42.Ablin J, Neumann L, Buskila D. Pathogenesis of fibromyalgia - a review. Joint Bone Spine. 2008;75:273–279. doi: 10.1016/j.jbspin.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 43.Crofford LJ, Pillemer SR, Kalogeras KT, Cash JM, Michelson D, Kling MA, et al. Hypothalamic- pituitary-adrenal axis perturbations in patients with fibromyalgia. Arthritis Rheum. 1994;37:1583–1592. doi: 10.1002/art.1780371105. [DOI] [PubMed] [Google Scholar]
- 44.Romano GF, Tomassi S, Russell A, Mondelli V, Pariante CM. Fibromyalgia and chronic fatigue: the underlying biology and related theoretical issues. Adv Psychosom Med. 2015;34:61–77. doi: 10.1159/000369085. [DOI] [PubMed] [Google Scholar]
- 45.Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013;14:502–511. doi: 10.1038/nrn3516. [DOI] [PMC free article] [PubMed] [Google Scholar]