Abstract
Introduction: Hospitalization of patients in the intensive care units always has negative consequences such as anxiety and concern for patients and their families. This study aimed to investigate the effect of programmed family presence in intensive care units on patients’ and families’ anxiety.
Methods: This was a quasi-experimental study conducted in Iran. The eligible patients and a member of their families were assigned into two groups (N = 80) through convenience sampling. The family members in the experimental group were allowed to attend twice a day for 15 minutes in a planned way beside the patient and contribute to their clinical primary care. In the control group, the family members had a strict limitation to visit their patients based on the usual policy. Anxiety in both groups at the beginning and on the third day of patient’s admission was measured, using Spielberger’s questionnaire. The data were analyzed with SPSS version13.
Results: The mean score of anxiety in the control group did not show significant difference in patients and in families, however it had decreased significantly in the experimental group after the intervention for both patients and families. The results showed that mean differences between the two groups was statistically significant in patients and families.
Conclusion: The planned presence of the family of patients in coronary care unit (CCU) played a crucial role in reducing the anxiety of patients and their family. Furthermore, it is recommended that strategies of visiting policy in intensive care units (ICUs) should be revised and the possibility be provided for the families’ planned presence and participation in the patient care.
Keywords: Anxiety, Coronary care units, Patient, Family, Patients’ visitors
Introduction
The intensive care unit (ICU) is a place where patients with acute, complex, and critical disorders and life-threatening conditions are admitted.1 Hospitalization in the ICU, sudden onset of the event, and severity of the disease are associated with a high level of anxiety for both patients and their families.2 In general, ICU admission is a traumatic event for patients and their family members.3-5 It has been reported that patients in the ICU suffer from sleep disorders, anxiety and worry in the first 48 hours of admission due to different stressors, such as being in a stressful and alien environment, lack of knowledge of the treatment process, fear of the future, problems that are likely to occur, and unsuccessful resuscitation and death of other patients.6 Such stressors can seriously affect the comfort of patients, stimulate the stress response mechanisms, increase oxygen consumption,7 and change the hemodynamic status of the patients.8 There is evidence suggesting that in the cardiovascular patients who need intensive care, the prevalence of psychological disorders such as anxiety and depression is estimated at 40% and 30%, respectively.9 Anxiety in these patients increases the risk of cardiovascular attack,10 exacerbates and prolongs the disease, interferes with the treatment, and finally delays the healing.11 Furthermore, it has been known that survivors of these intensive units recall high levels of depression, severe anxiety, and social isolation after discharge.12 One of the psychological stressors in patients admitted to the ICU that may lead to anxiety is being away from the family, which is mainly because of the structure and philosophy of the intensive care unit where strict visiting policies are applied.13
This situation is not only stressful and scary for the patients, but also for their family members,12-14 because the family has a fundamental and important role in human health and well-being.15 The family is as an open and coherent system in which any threat to one of the members is considered a threat to the whole system.16 In other words, all aspects of the family health can be affected by the health status of the sick member.17 Accordingly, an acute and incurable illness or hospitalization of a family member is considered a stressful incident, which causes the family to suffer from an emotional crisis, depression and anxiety.18-20 It can suddenly disturb the health of the family and change its structure.6 This situation is exacerbated when patients need admission in intensive care units.21 With ICU admission of a critically ill patient, the whole family is affected.22
In fact, ICU admission can cause some problems and negative consequences for the family, such as psychological disorders.6,23 Families who cannot cope with ICU hospitalization of a beloved one may experience an emotional crisis and show negative reactions like shock, anxiety, depression, and sleep disorders.19,24 As a result of this critical and stressful situation, the family does not have enough time to be prepared to encounter these problems25,26 and often feel confused and desperate.6 In other words, 50% of the families cannot understand the explanations of the medical staff regarding the prognosis, diagnosis, and treatment of their patients.21
The points above indicate the necessity and importance of special attention to emotional support of these patients and their families. However, strict visiting policies are traditionally applied in the ICU, because it is believed that the presence of the patients’ family in these units increases the risk of infectious complications.13,27 Some other studies have shown that ICU nurses perceive patients’ visits as a source of increased workload and burnout.28,29 Disorganization of patient care and more interruptions due to the extended presence of families in the ICU are the other reasons for adhering strict visiting policy in intensive care units.30 There is also concern that with open visitation policy, stress of family members will increase because of feeling to be obligated to stay in the ICU.31,32 As well as, it is believed that in addition to increasing infection risk and compromised nursing care, open visits can also cause tachycardia, hypertension, dysrhythmia or produce interruption in patient’s rest.33 However, some scientific evidence reject this false impression and demonstrate that implementation of open visiting policies is not associated with high rates of infectious complications and can even lead to a significant reduction in cardiovascular morbidity and mortality.34,35 Moreover, some studies suggest that by changing limited visitation time to an extended and flexible model, length of ICU delirium and ICU stay will reduce.36
Visitation strategy dose not impact only on patients. In fact, strict ICU visitation policies result in isolation and anxiety in patients13 and it also affects the family members.15 The family members of ICU patients experience doubts and concerns whether adequate care is provided for their patients because they are away from their beloved ones, cannot make contact with their patients, and are unaware of the care environment.37 In this situation, the presence of the family members in the ICU, who are allowed to visit their patients, can satisfy their emotional needs. It also provides the opportunity to train families, increase their satisfaction and, therefore, reduce their complaints.38 The regular presence of family members as a source of familiar sensory stimuli has also some benefits for the patients. It may result in faster enhancement of the patient’s cognitive status, improve the prognosis, and decrease the length of ICU stay.39,40 However, there are still concerns about negative attitudes towards the family presence in the intensive care units and strict visiting policies that are applying in the almost Iranian hospitals. Therefore, more comprehensive studies in this regard can make grounds for changing the current attitude and providing more emotional support for patients and their families. Though, other studies had focused on open visiting hours, in this study a planned and structured visiting policy was designed that is more compatible with the intensive care units setting. In addition, in view of dependency of most critically ill patients, allowing a family member to participate in the patient primary care; which is another distinctive aspect of the intervention in this study. Furthermore, most similar studies had only focused on the patients’ outcomes30,41,42; this study was considered both the patients’ and families’ outcome owing to importance of family. Accordingly, patients who admitted in coronary care units (CCUs) usually suffer from sudden heart disorders such as life-threatening dysrhythmias, acute pulmonary edema, myocardial infarction, cardiogenic shock, etc.43 which are critical, unexpected and more stressful for both patients and families, this study aimed at evaluation the effect of planned family presence in the CCU on the anxiety level of patients and their families.
Materials and Methods
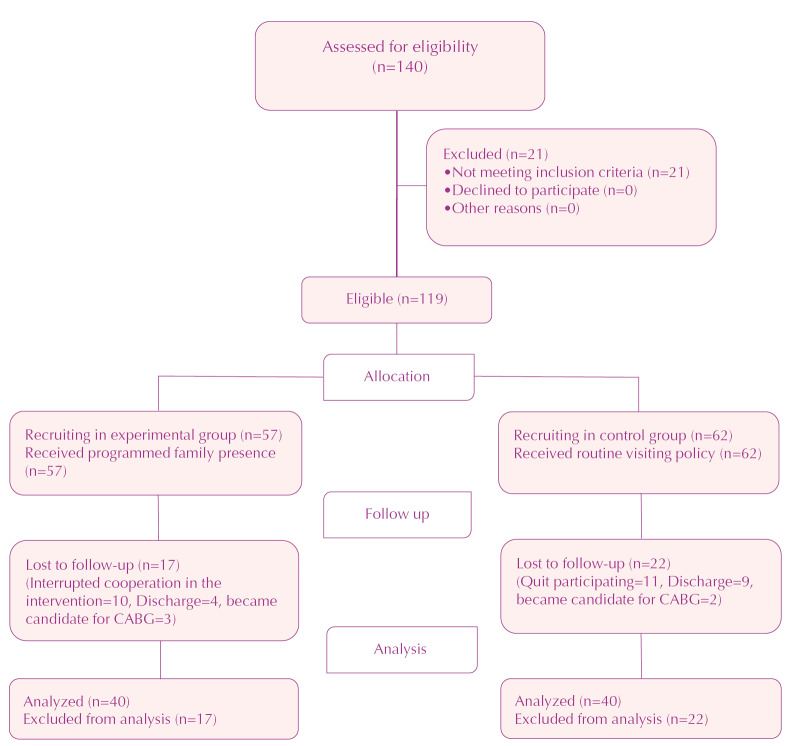
This quasi-experimental study was conducted in CCU of one hospital in Sari, Iran. The study setting contained 15 beds overall. The study population comprised patients admitted to the CCU and their families who met the inclusion criteria which being 18-60 years of age; being completely conscious and alert; no history of mental illness, thyroid disease, or previous hospitalization in the intensive care unit, and not being a member of the health care team. The exclusion criteria were withdrawal of the patient or family member from the study; disturbing the peace and discipline of the unit; disallowed interference in the patient care; irregular presence in the ICU during data collection; patient discharge or transfer to another unit before the end of the intervention; and special incidents during the intervention such as cardiopulmonary resuscitation, intubation, or open heart surgery because of its increasing anxiety. A pilot study was conducted in one group include 15 patients and 15 family members to determine the sample size. These subjects were not included in the main study. Based on the mean and standard deviation of the dependent variable (anxiety) in the pilot study and by using related formula, 80 participants, including 40 patients and 40 family members in each group, were studied. In order to avoid data contamination between groups because of their social interaction, the sampling was done consecutively. In other words, the control group was selected as the first group for sampling through tossing a coin. Then, the eligible subjects were selected through convenience sampling in each group. When the required sample size (40 patients; 40 relatives) was achieved in the control group, the sampling was started in the experimental group (40 patients; 40 relatives) after the last patient in the control group was discharged (Figure 1). It should be mentioned that the researchers assessed the eligibility and recruited the participants if they signed an informed consent form. The informed consent contained some explanations about voluntary participation, the right to quit at any time, data confidentiality, and the mechanism of any probable complaint. It was signed by both patients and their families of both groups.
Figure 1.
Flow chart of the study
A questionnaire was applied to collect the demographic characteristics of the patients and family members, and the State-Trait Anxiety Inventory (STAI) was used to determine the level of anxiety. The STAI consists of 20 questions based on a 4-point Likert scale. The total score of this inventory ranges from 20 to 80 (20-39=mild anxiety, 40-59=moderate anxiety, and 60-80=severe anxiety). The STAI has been validated in Iranian population and its validity and reliability (Cronbach’s alpha=0.94) was confirmed.44 In this study, the content validity and the reliability of the questionnaire were confirmed by expert opinions (n = 12) and internal consistency through the pilot study (n=15) with α=0.89, respectively. The STAI was applied once in the first 24 hours of CCU admission and then at the end of the third day in both groups.
Before conducting the study, formal permission was obtained from the manager of hospital and also the manager and head nurse of CCU. The intervention included planned presence of a preferred family member who met the inclusion criteria and it was performed from the first day of admission to CCU for 3 days. The selected family members attended the CCU twice a day (at 10am in the morning and 5 PM in the evening shift), each time for 15 minutes. They were allowed to enter the CCU, after coordination with the nurse in charge, to visit and provide emotional support for their beloved ones, touching them, participating in some primary care activities, such as dressing, washing their face, combing their hair, brushing their teeth, feeding and taking the patient to the bathroom. In addition, they had a chance to interact with the nurses and ask their questions about the clinical condition of their patient to be more informed and confident. Before the family members entered the unit, the researchers notified them that they had to observe the rules of the unit and be careful not to disturb other patients’ privacy and peace or make trouble for nursing care during the time they visited their patient. To prevent crowding of the CCU environment, the family members entered to the unit in turn, after permission of in charge nurse. Moreover, for ethical considerations, other visitors of the patients followed the routine visiting policy. In addition, there was an opportunity for families of ineligible patients to visit their patients like the main participants if they wanted, but in different time to control the setting.
In the control group, no specific intervention was conducted and all visitors, including family members, relatives, friends, colleagues, etc., were allowed to visit their patients according to the visitation policies on Mondays, Wednesdays, and Fridays between 3-4 PM. The visitors were allowed to enter the unit one by one. Each visitor had the permission to be with the patient for only 3-5 minutes and then leave the unit for the next visitor to come in. There was no priority between first-degree relatives, other relatives or friends in terms of the duration of visiting. None of the visitors was allowed to engage in patient care.
The data collection process took 5 months. Descriptive and inferential statistics were used for data analysis by using SPSS software (version 13). To compare the dependent variable within each group and between groups, paired and independent t test was applied, respectively. P values less than 0.05 were considered significant. The normality of the data distribution was assessed by the Shapiro-Wilk test.
Results
The majority of patients were men (52.5%) in the experimental group and women (52.5%) in the control group, but there was no statistically significant difference between the two groups. Most patients (97.5%) were married and were 40-57 years old. They were often hospitalized in the CCU due to acute coronary syndrome (47.5%) and were on complete bed rest (80%). Other reasons for hospitalization were dysrhythmias, diagnostic procedures such as angiography or percutaneous coronary intervention, or other diseases like deep vein thrombosis, endocarditis, and congestive heart failure. The family members of the patients were mostly women (66.25%) and married (91.25%), and were 27-42 years old. The majority of them had a child-parent relationship with the patients (76.25%). In general, the patients and their families in both experimental and control groups were similar in terms of demographic characteristics (Table 1).
Table 1. Characteristics of patients and family members .
| Control (n = 40) | Experiment (n = 40) | P value | ||
| No. (%) | No. (%) | |||
| Patients | ||||
| Agea | 56.45 (5.10) | 54.10 (10.11) | 0.06 | |
| Gender | 0.65 | |||
| Female | 21 (52.5) | 19 (47.5) | ||
| Male | 19 (47.5) | 21 (52.5) | ||
| Marital status | 0.35 | |||
| Single | 0 (0) | 1 (2.5) | ||
| Married | 40 (100) | 38 (98) | ||
| Widow | 0 (0) | 1 (2.5) | ||
| Educational level | 0.93 | |||
| Higher education | 3 (7.5) | 4 (10) | ||
| Diploma | 0 (0) | 0 (0) | ||
| High school | 5 (12.5) | 6 (15) | ||
| Pre-tertiary | 32 (80) | 30 (75) | ||
| Admission reason | ||||
| Acute coronary syndrome | 21 (52.5) | 17 (42.5) | 0.10 | |
| Cardiac dysrhythmias | 6 (15) | 8 (20) | ||
| Diagnosticb procedures | 13 (32.5) | 10 (25) | ||
| Othersc | 0 (0) | 5 (12.5) | ||
| Mobility status | ||||
| Out of bed | 2 (5) | 1 (2.5) | 0.52 | |
| Relative bed rest | 8 (20) | 5 (12.5) | ||
| Complete bed rest | 30 (75) | 34 (85) | ||
| Family Members | ||||
| Agea | 39.82 (9.17) | 39.20 (9.46) | 0.82 | |
| Gender | ||||
| Female | 23 (57.5) | 30 (75) | 0.09 | |
| Male | 17 (42.5) | 10 (25) | ||
| Marital status | ||||
| Single | 2 (5) | 5 (12.5) | 0.23 | |
| Married | 38 (95) | 35 (87.5) | ||
| Widow | 0 (0) | 0 (0) | ||
| Educational level | ||||
| Higher education | 7 (17.5) | 12 (30) | 0.10 | |
| Diploma | 4 (10) | 2 (5) | ||
| High school | 19 (47.5) | 10 (25) | ||
| Pre-tertiary | 10 (25) | 16 (40) | ||
| Relationship with the patient | ||||
| Parent-child | 31 (77.5) | 30 (75) | 0.48 | |
| Sister or brother | 1 (2.5) | 3 (7.5) | ||
| Spouse | 6 (15) | 6 (15) | ||
| Othersa | 2 (5) | 1 (2.5) | ||
a Mean (SD); b Angiography or percutaneous coronary intervention; cEndocarditis, deep vein thrombosis, chronic, heart failure; dGrandchildren, daughter in law.
The results showed that the mean (SD) anxiety score of the patients in the control group was 52.2 (5.56) in the first 24 hours of CCU admission and 50.22(5.10) at the end of the third day (P =0.06). In the experimental group, the mean anxiety score was 50.90 (4.60) before the intervention which was reduced to 45.15 (6.43) after the intervention. This difference was statistically significant (P <0.001) (Table 2). The comparison of the mean differences between the two groups was statistically significant, too (P =0.01) (Table 3).
Table 2. Anxiety of patients in control and experiment groups .
| Anxiety | Control group (n = 40) | Experiment group (n = 40) | ||
|
First day
No. (%) |
Third day
No. (%) |
First day
No. (%) |
Third day
No. (%) |
|
| Mild (20-39) | 0 (0) | 1(2.5) | 2 (5) | 9 (22.5) |
| Moderate (40-59) | 36 (90) | 37(92.5) | 37 (92.5) | 30 (75) |
| Severe (60-80) | 4 (10) | 2(5) | 1 (2.5) | 1 (2.5) |
| Mean (SD) | 52.25 (5.56) | 50.22 (5.10) | 50.90 (4.60) | 45.15 (6.43) |
| P value | 0.06 | > 0.001* | ||
*Statisticaly significant.
Table 3. Comparision of mean differences of anxiety score in patients and family members .
| Group | Patient | Family member | ||
| Control | Experiment | Control | Experiment | |
| Difference of mean scores (SD) | 2.03 (6.58) | 5.75 (7.13) | 0.25 (7.28) | 5.75 (5.46) |
| Statistical indicatora |
t =-2.42, df =78, P =0.01* |
t =-4.169, df =78, P <0.001* |
||
*Statisticaly significant; aIndependent t test was used.
The results also showed that the mean (SD) score of the family’s anxiety in the control group was 50.05 (7.14) and 50.30 (6.58) on the first and third day of CCU admission, respectively. The difference was not statistically significant (P =0.82). In the experimental group, the mean score of anxiety was 50.50(4.11) before and 44.75(5.86) after the intervention, indicating a significant difference (P < 0.001) (Table 4). The mean difference was statistically significant between the two groups (P <0.001) (Table 3).
Table 4. Anxiety of family members in control and experiment groups .
| Anxiety | Control gruop (n = 40) | Experiment gruop (n = 40) | ||
|
First day
No. (%) |
Third day
No. (%) |
First day
No. (%) |
Third day
No. (%) |
|
| Mild (20-39) | 2(5) | 1 (2.5) | 0 (0) | 6 (15) |
| Moderate (40-59) | 34 (85) | 36 (90) | 39 (97.5) | 34 (85) |
| Severe (60-80) | 4 (10) | 3 (7.5) | 1(2.5) | 0 (0) |
| Mean (SD) | 50.05 (7.14) | 50.30 (6.58) | 50.50 (4.11) | 44.75 (5.86) |
| P value | P = 0.82 | P < 0.001* | ||
*Statisticaly significant.
Discussion
The results of this study showed the majority of patients and their families suffer from moderate anxiety at the time of admission to CCU. In fact, the results of other studies also indicate that the patients and their families experience a high level of anxiety in the early days of ICU admission, which can have harmful effects on their health.6,9,13,18 ICU admission often results in excessive psychological and physical distress in the patients45 and their relatives.46,47 One of the reasons for anxiety in patients is being away from the family due to the strict visiting policies.13 Moreover, lack of information about the treatment process and uncertainty about the quality of care, considering the limitations in presence at the patient’s bedside, can cause anxiety, fear, and worry in families.48-50, In fact, family members endure high levels of anxiety behind closed doors and experience physical and psychological barriers to communicate with their patient.51 Inadequate contact with the patient and being away from his/her treatment environment lead to an incomplete or even incorrect perception of nurses’ and physicians’ behavior, which can exacerbate the current crisis the families are experiencing.52 Therefore, it is necessity to address this problem. It is noticeable that in this study, the prevalence of anxiety in patients and their families was higher than that reported in some other studies which can be due to some cultural differences. Day et al., studied anxiety in family members of patients admitted to intensive care unit and reported 20.7% of family members to experience moderate to severe anxiety.19 This difference can be attributed to a very strong relationship among family members in the Iranian culture, with almost every incident to a member affecting other members. The admission of one family member to the ICU almost always results in moderate to high anxiety in the rest of the family, as well as, the patient. In accordance with the results of this study, some other studies conducted in Iran have shown a high prevalence of anxiety in ICU patients53,54 and their family members.55,56
The findings of this study showed that planned presence of the family at the patient’s bedside in intensive care unit and their participation in some primary care of the patient had positive effects on the reduction of anxiety of the patients. Although anxiety reduction in this study may not seem too high in the statistical results, it can still be considered important clinically because of strong emotional dependency between family members and the religious beliefs about patients visit in Iran.57 This finding is compatible with other studies were done in Iran.7,41 In a study, 64 patients admitted to the ICU in Iran, and reported the presence of the family and their participation in the process of patient care to have caused sensory stimulation in the patients and reduced patients’ anxiety, resulting in increasing oxygen saturation level. So, allowing family members to be present at the patient’s bedside will have physical outcomes and can be viewed as a non-pharmacological intervention.7 Also, another study showed that scheduled visit method has a significant effect to reduce anxiety of patients who admitted to CCU because of angina pectoris 41. Fumagalli et al., compared restricted and none-restricted ICU visiting policies and concluded that the presence of the family at the patient’s bedside through implementing open visiting policies could reduce the anxiety of the patients. In addition, it can decrease cardiovascular complications through hormone balancing.34 In another study, the participants stated that the presence of the relatives at their bedside reduced their anxiety.58 Therefore, it is believed, not only do not the open visitation policies disturb the patients, but they also create a support system for them.59 The presence of family members in the ICU can improve process of dealing with the problems caused by the disease.16 It should be emphasize that although most studies have shown different benefits of open visitation,60 a few hospitals have implemented this strategy.61 This implies that regardless of the advantages of open visitation, some obstacles like the attitude of the healthcare team and managers towards this policy have limited its applications.60,62 Moreover, environmental factors, especially in the intensive care unit, are another barrier.62 Therefore, choosing more flexible and acceptable strategies such as ‘unrestricted’ or ‘flexible’ visitation policies could help overcome some of these barriers.60 In this study, the planned presence of the families in the CCU was considered an unrestricted policy that is more compatible with the setting and the context of the intensive care unit compared to open visitation. However, it was totally different from the current restricted visiting hours. In addition, the families were allowed to contribute to some primary care activities during their presence in the CCU.
As another result, the planned presence of family members at the patient’s bedside in coronary care unit reduces the family members’ anxiety, too. In general, when patients are admitted to intensive care unit, the family members are distraught and face a crisis. During this crisis, they need to communicate effectively, clearly and continuously with their patients and the health care team. According to the literature, the most common reason for anxiety in the patients’ families is lack of sufficient information about prognosis, treatment and care of their patients.46,63 Moreover, unfamiliarity with the ICU environment and its complex equipment are the other reasons for anxiety.46 Hence, the health care team, especially the nurses, are responsible for providing the required information to and supporting the patients’ families and observing their needs.63,64 This can happen through a flexible and unrestricted visiting policy such as the intervention of the current study in which the families had an opportunity to interact with nurses during their presence in patient’s bedside. As a result, their emotional and informational needs were met through questioning and answering. Therefore, their mental pressure reduces, and they can cope with the crisis more efficiently.62,65 In this regard, the findings of a study by Sadeghi et al., in Iran demonstrated that periodic family visits increased the satisfaction of the families and reduced their anxiety.38 It should be mentioned although this study was done in ICU and the modification for visiting policy and hours was a bit different from the current study, both showed this strategy will be effective. Moreover, according to other studies, family members feel relaxed and less anxious if they visit their patients in the intensive care units.29,66 Therefore, it is necessary to implement some strategies to reduce the limitations of ICU visiting policies and increase the presence of family members at the patient’s bedside to enhance their communication and participation in patient care. This is because visitation based on a very strict and limited policy, such as the current visitation policies commonly practiced,13,59,61,67 seems to be inefficient in meeting the needs of the ICU patients and their families.
Since this study was conducted on conscious patients hospitalized in the CCU, the results cannot be generalized to unconscious patients and their families. It is recommended a similar study be performed in such patients. Moreover, since some cultural factors may affect the relationship between patients and their families and their perceived level of anxiety, it is suggested a multicenter and multinational study be conducted to compare the effectiveness of such interventions in different cultural contexts. Although the quality of this study was examined and approved by a reliable panel, including some faculty members, expert in research methodology, conducting another study with a randomized controlled design will produce more authentic results since this study had a non-randomized design.
Conclusion
The results of this study showed that planned family presence at the patient’s bedside and their participation in care can reduce the level of anxiety in both the patients and their families. Therefore, since patients and their families experience moderate to severe anxiety during CCU admission, it is suggested that current restricted visiting policies be replaced with more flexible visiting strategies such as planned and supervised presence of family members to control the anxiety and its undesirable consequences. Involving families in patient care seems to have an effective role in reducing the level of anxiety, too. In fact, the families need to interact more with their critically ill beloved ones and be involved in caring activities. Since there is some resistance against open visitation in the intensive care units, this strategy would be an acceptable solution for a gradual shift in this policy.
Acknowledgments
This article is the result of approved project in Nursing and Midwifery Care Research Center, Tehran University of Medical Sciences (grant No. 32260). We appreciate it for its financial support. In addition to thanking all family members and patients participated in this study, authors would like to appreciate all nurses for their cooperation.
Ethical Issues
The study was registered in the Iranian Registry of Clinical Trials (Identifier: IRCT2016041727442N1) and approved by the Ethics Committee of Tehran University of Medical Sciences (Code No. 9311449003).
Conflict of Interest
The authors declared no potential conflicts of interest.
Author’s Contributions
SHK prepared the proposal; did intervention and data gathering and drafted the manuscript. MI contributed to the conception and design of this study, supervised the whole study process including the data collecting, analyzing and interpreting. Also, she drafted the manuscript; HSEG consulted in preparing report document of the research. ZR did the data interpretation.
Research Highlights
What is the current knowledge?
Admission in intensive care unit usually is an unpredictable and unexpected event and exposes both patients and families to an emotional crisis.
Restricted visiting policy in intensive care units produces more psychological pressure to patients and their families.
What is new here?
The study highlights the positive impact of family presence in CCU through reducing anxiety of both patients and families.
Participation of families in patient’ care sounds to meet psychological needs of them and diminish their anxiety.
There is a real need for a planned and more flexible visiting policy in intensive care units to control undesirable effects of psychological stress in patients and their families.
References
- 1.Banu SH. EEG in ICU: A monitoring tool for critically ill patient. Bangladesh Crit Care J. 2014;2(1):28–34. doi: 10.3329/bccj.v2i1.19954. [DOI] [Google Scholar]
- 2.Płaszewska-Żywko L, Gazda D. Emotional reactions and needs of family members of ICU patients. Anaesthesiol Intensive Ther. 2012;44(3):145–9. [PubMed] [Google Scholar]
- 3.Johansson M, Wåhlin I, Magnusson L, Runeson I, Hanson E. Family members’ experiences with intensive care unit diaries when the patient does not survive. Scand J Caring Sci. 2018;32(1):233–40. doi: 10.1111/scs.12454. [DOI] [PubMed] [Google Scholar]
- 4.McAdam JL, Dracup KA, White DB, Fontaine DK, Puntillo KA. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med. 2010;38(4):1078–85. doi: 10.1097/CCM.0b013e3181cf6d94. [DOI] [PubMed] [Google Scholar]
- 5.Muretti AM, Al-Hindawi A, Nenadlova K, Green J, Edginton T, Vizcaychipi MP. Management of post-traumatic stress disorder (PTSD) in patients’ relatives and intensive care personnel in a teaching hospital. J Anesth Surg. 2017;4(3):55–64. doi: 10.15436/2377-1364.17.074. [DOI] [Google Scholar]
- 6.Zanetti TG, Stumm EMF, Ubessi LD. Stress and coping in families of patients in an intensive care unit. Rev Pesqui. 2013;5(2):3608–19. doi: 10.9789/2175-5361.2013v5n2p3608. [DOI] [Google Scholar]
- 7.Yousefi H, Naderi M, Daryabeigi R. The effect of sensory stimulation provided by family on arterial blood oxygen saturation in critical care patients. Iran J Nurs Midwifery Res. 2015;20(1):63–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Dijkstra BM, Gamel C, van der Bijl JJ, Bots ML, Kesecioglu J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. J Clin Nurs. 2010;19(7-8):1030–9. doi: 10.1111/j.1365-2702.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 9.Peris A, Bonizzoli M, Iozzelli D, Migliaccio ML, Zagli G, Bacchereti A. et al. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care. 2011;15(1):R41. doi: 10.1186/cc10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eken C, Oktay C, Bacanli A, Gulen B, Koparan C, Ugras SS. et al. Anxiety and depressive disorders in patients presenting with chest pain to the emergency department: a comparison between cardiac and non-cardiac origin. J Emerg Med. 2010;39(2):144–50. doi: 10.1016/j.jemermed.2007.11.087. [DOI] [PubMed] [Google Scholar]
- 11.Nasiri M, Rahimiyan B, Jahanshahi M, Hajiyan K, Nikfar J. Stressors associated with hospitalization in the stressful cardiac care unit. Iranian Journal of Critical Care Nursing. 2011;4(3):141–8. [Persian] [Google Scholar]
- 12.Hunter JD, Goddard C, Rothwell M, Ketharaju S, Cooper H. A survey of intensive care unit visiting policies in the United Kingdom. Anaesthesia. 2010;65(11):1101–5. doi: 10.1111/j.1365-2044.2010.06506.x. [DOI] [PubMed] [Google Scholar]
- 13.Berwick DM, Kotagal M. Restricted visiting hours in ICUs: time to change. JAMA. 2004;292(6):736–7. doi: 10.1001/jama.292.6.736. [DOI] [PubMed] [Google Scholar]
- 14.Whitton S, Pittiglio LI. Critical care open visiting hours. Crit Care Nurs Q. 2011;34(4):361–6. doi: 10.1097/CNQ.0b013e31822c9ab1. [DOI] [PubMed] [Google Scholar]
- 15.Maruiti MR, Galdeano LE, Farah OGD. Anxiety and depressions in relatives of patients admitted in intensive care units. Acta Paul Enferm. 2008;21(4):636–42. doi: 10.1590/S0103-21002008000400016. [DOI] [Google Scholar]
- 16.Bellou P, Gerogianni KG. The contribution of family in the care of patient in the hospital. Health Sci J. 2007;1(3):1–6. [Google Scholar]
- 17.Salehi-Tali S, Ahmadi F, Zarea K, Fereidooni-Moghadam M. Commitment to care: the most important coping strategies among family caregivers of patients undergoing haemodialysis. Scand J Caring Sci. 2018;32(1):82–91. doi: 10.1111/scs.12432. [DOI] [PubMed] [Google Scholar]
- 18.Bolosi M, Peritogiannis V, Tzimas P, Margaritis A, Milios K, Rizos DV. Depressive and anxiety symptoms in relatives of intensive care unit patients and the perceived need for support. J Neurosci Rural Pract. 2018;9(4):522–8. doi: 10.4103/jnrp.jnrp_112_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Day A, Haj-Bakri S, Lubchansky S, Mehta S. Sleep, anxiety and fatigue in family members of patients admitted to the intensive care unit: a questionnaire study. Crit Care. 2013;17(3):R91. doi: 10.1186/cc12736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmidt M, Azoulay E. Having a loved one in the ICU: the forgotten family. Curr Opin Crit Care. 2012;18(5):540–7. doi: 10.1097/MCC.0b013e328357f141. [DOI] [PubMed] [Google Scholar]
- 21.Pryzby BJ. Effects of nurse caring behaviours on family stress responses in critical care. Intensive Crit Care Nurs. 2005;21(1):16–23. doi: 10.1016/j.iccn.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J. et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–28. doi: 10.1097/ccm.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 23.Van Horn ER, Kautz D. Promotion of family integrity in the acute care setting: a review of the literature. Dimens Crit Care Nurs. 2007;26(3):101–7. doi: 10.1097/01.DCC.0000267803.64734.c1. [DOI] [PubMed] [Google Scholar]
- 24.Shorofi SA, Jannati Y, Roohi Moghaddam H. he psychosocial needs of the families of the patients admitted to intensive care units: a review of literature. Clinical Excellence. 2014;3(1):46–57. [Persian] [Google Scholar]
- 25.Chang Y, Lin YP, Chang HJ, Lin CC. Cancer patient and staff ratings of caring behaviors: relationship to level of pain intensity. Cancer Nurs. 2005;28(5):331–9. doi: 10.1097/00002820-200509000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Fridh I, Forsberg A, Bergbom I. Close relatives’ experiences of caring and of the physical environment when a loved one dies in an ICU. Intensive Crit Care Nurs. 2009;25(3):111–9. doi: 10.1016/j.iccn.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 27.Azoulay E, Pochard F, Chevret S, Arich C, Brivet F, Brun F. et al. Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med. 2003;29(9):1498–504. doi: 10.1007/s00134-003-1904-y. [DOI] [PubMed] [Google Scholar]
- 28.Giannini A, Miccinesi G, Prandi E, Buzzoni C, Borreani C. Partial liberalization of visiting policies and ICU staff: a before-and-after study. Intensive Care Med. 2013;39(12):2180–7. doi: 10.1007/s00134-013-3087-5. [DOI] [PubMed] [Google Scholar]
- 29.Rosa RG, Falavigna M, Robinson CC, da Silva DB, Kochhann R, de Moura RM. et al. Study protocol to assess the effectiveness and safety of a flexible family visitation model for delirium prevention in adult intensive care units: a cluster-randomised, crossover trial (The ICU Visits Study) BMJ Open. 2018;8(4):e021193. doi: 10.1136/bmjopen-2017-021193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosa RG, Tonietto TF, da Silva DB, Gutierres FA, Ascoli AM, Madeira LC. et al. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45(10):1660–7. doi: 10.1097/ccm.0000000000002588. [DOI] [PubMed] [Google Scholar]
- 31.Berti D, Ferdinande P, Moons P. Beliefs and attitudes of intensive care nurses toward visits and open visiting policy. Intensive Care Med. 2007;33(6):1060–5. doi: 10.1007/s00134-007-0599-x. [DOI] [PubMed] [Google Scholar]
- 32.Garrouste-Orgeas M, Philippart F, Timsit JF, Diaw F, Willems V, Tabah A. et al. Perceptions of a 24-hour visiting policy in the intensive care unit. Crit Care Med. 2008;36(1):30–5. doi: 10.1097/01.ccm.0000295310.29099.f8. [DOI] [PubMed] [Google Scholar]
- 33.Ghiyasvandian SH, Abbaszadeh A, Ghojazadeh M, Sheikhalipour Z. The personal social factors of nurses beliefs about open visiting in icu of Sina-Tabriz hospital: based on reasoned-action theory of Ajzen-Fishbein. Medical Journal of Tabriz University of Medical Sciences. 2010;32(3):50–6. [Persian] [Google Scholar]
- 34.Fumagalli S, Boncinelli L, Lo Nostro A, Valoti P, Baldereschi G, Di Bari M. et al. Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit: results from a pilot, randomized trial. Circulation. 2006;113(7):946–52. doi: 10.1161/circulationaha.105.572537. [DOI] [PubMed] [Google Scholar]
- 35.alavati M, Najafvandzadeh M, Oshvandi K, Homayonfar S, Soltanian A. The effects of programmed visiting on physiological indexes in CCU patients. Avicenna J Nurs Midwifery Care. 2012;20(3):43–53. [Persian] [Google Scholar]
- 36.Eghbali-Babadi M, Shokrollahi N, Mehrabi T. Effect of family-patient communication on the incidence of delirium in hospitalized patients in cardiovascular surgery ICU. Iran J Nurs Midwifery Res. 2017;22(4):327–31. doi: 10.4103/1735-9066.212985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McAdam JL, Puntillo K. Symptoms experienced by family members of patients in intensive care units. Am J Crit Care. 2009;18(3):200–9. doi: 10.4037/ajcc2009252. [DOI] [PubMed] [Google Scholar]
- 38.Sadeghi Z, Payami M, Moosavi Nasab SN. Effect of family participation in ICU patients care on family’s anxiety level. Preventive Care in Nursing & Midwifery Journal. 2013;2(2):10–7. [Google Scholar]
- 39.Gerber CS. Understanding and managing coma stimulation: are we doing everything we can? Crit Care Nurs Q. 2005;28(2):94–108. doi: 10.1097/00002727-200504000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Hasanzadeh F, Hoseini Azizi T, Esmaily H, Ehsaee M. Impact of familiar sensory stimulation on level of Consciousness in patients with head injury in ICU. Journal of North Khorasan University of Medical Sciences. 2012;4(1):121–33. doi: 10.29252/jnkums.4.1.121. [DOI] [Google Scholar]
- 41.Bashti S, Aghamohammadi M, Heidarzadeh M. The impact of family visits on the level of anxiety in patients with angina pectoris hospitalized in intensive care units. Journal of Health and Care. 2016;18(2):161–9. [Persian] [Google Scholar]
- 42.Rosa RG, Falavigna M, da Silva DB, Sganzerla D, Santos MMS, Kochhann R. et al. Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU visits randomized clinical trial. JAMA. 2019;322(3):216–28. doi: 10.1001/jama.2019.8766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mokhtar S. Evolution of the concept of coronary care and the emergent roleof critical care. Egypt J Crit Care Med. 2018;6(1):1–3. doi: 10.1016/j.ejccm.2018.04.001. [DOI] [Google Scholar]
- 44. Mahram B. Spielberger Test Standardization in Mashhad [thesis]. Tehran: Allameh Tabatabaei University; 1994.
- 45.Quinio P, Savry C, Deghelt A, Guilloux M, Catineau J, de Tinténiac A. A multicenter survey of visiting policies in French intensive care units. Intensive Care Med. 2002;28(10):1389–94. doi: 10.1007/s00134-002-1402-7. [DOI] [PubMed] [Google Scholar]
- 46.Chien WT, Chiu YL, Lam LW, Ip WY. Effects of a needs-based education programme for family carers with a relative in an intensive care unit: a quasi-experimental study. Int J Nurs Stud. 2006;43(1):39–50. doi: 10.1016/j.ijnurstu.2005.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaakinen JR, Coehlo DP, Steele R, Tabacco A, Hanson SMH. Family Health Care Nursing: Theory, Practice, and Research. 4th ed. Philadelphia: FA Davis Company; 2014. [Google Scholar]
- 48.Karlsson C, Tisell A, Engström A, Andershed B. Family members’ satisfaction with critical care: a pilot study. Nurs Crit Care. 2011;16(1):11–8. doi: 10.1111/j.1478-5153.2010.00388.x. [DOI] [PubMed] [Google Scholar]
- 49.Cypress BS. The lived ICU experience of nurses, patients and family members: a phenomenological study with Merleau-Pontian perspective. Intensive Crit Care Nurs. 2011;27(5):273–80. doi: 10.1016/j.iccn.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 50.Sarhadi M, Navidian A, Fasihi Harandy T, Kheykhaei A. Assessment of psychosocial needs of the family members of the patients hospitalized in ICU and CCU. Iran J Crit Care Nurs. 2014;6(4):259–68. [Google Scholar]
- 51.Rodríguez Martínez Mdel C, Rodríguez Morilla F, Roncero del Pino A, Morgado Almenara MI, Theodor Bannik J, Flores Caballero LJ. et al. Family involvement in the critically ill patient basic care. Enferm Intensiva. 2003;14(3):96–108. doi: 10.1016/s1130-2399(03)78114-0. [DOI] [PubMed] [Google Scholar]
- 52.Abbaszadeh A, Salmani N, Rassouli M. Hospitalized children’s mothers’ perceptions of nursing care behaviors. Iran J Nurs Res. 2014;9(2):28–37. [Persian] [Google Scholar]
- 53.Beyraghi N, Tonekaboni SH, Vakili GH. Anxiety and depression in patients admitted in cardiac care unit, Taleghani hospital, Tehran, Iran, 2003. Hormozgan Medical Journal. 2006;9(4):261–4. [Persian] [Google Scholar]
- 54.Hedayati E, Hazrati M, Momen Nasab M, Shokoohi H, Afkari F. The relationship between spiritual well-being and anxiety of aged people admitted in coronary care units. Salmand: Iranian Journal of Ageing. 2016;11(3):432–9. doi: 10.21859/sija-1103432. [DOI] [Google Scholar]
- 55.Rabie Siahkali S, Avazeh A, Eskandari F, Khalegh Doost Mohamadi T, Mazloom S, Paryad E. A survey on psychological and environmental factors on family anxiety of the hospitalized patients in intensive care units. Iran J Crit Care Nurs. 2011;3(4):175–80. [Persian] [Google Scholar]
- 56. Rahmani R. Study on Prevalence of Depression, Anxiety, and Stress in Family Caregivers of Patients and Effective Factors, in Intensive Care Units of Hospitals Affiliated to Tehran University of Medical Sciences in 2015-16 [dissertation]. Tehran: Tehran University of Medical Sciences; 2016. [Persian].
- 57.Azimi Lolaty H, Bagheri-Nesami M, Shorofi SA, Golzarodi T, Yazdani Charati J. The effects of family-friend visits on anxiety, physiological indices and well-being of MI patients admitted to a coronary care unit. Complement Ther Clin Pract. 2014;20(3):147–51. doi: 10.1016/j.ctcp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 58.Happ MB, Swigart VA, Tate JA, Arnold RM, Sereika SM, Hoffman LA. Family presence and surveillance during weaning from prolonged mechanical ventilation. Heart Lung. 2007;36(1):47–57. doi: 10.1016/j.hrtlng.2006.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spreen AE, Schuurmans MJ. Visiting policies in the adult intensive care units: a complete survey of Dutch ICUs. Intensive Crit Care Nurs. 2011;27(1):27–30. doi: 10.1016/j.iccn.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 60.McAdam JL, Puntillo KA. Open visitation policies and practices in US ICUs: can we ever get there? Crit Care. 2013;17(4):171. doi: 10.1186/cc12763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu V, Read JL, Scruth E, Cheng E. Visitation policies and practices in US ICUs. Crit Care. 2013;17(2):R71. doi: 10.1186/cc12677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khaleghparast S, Joolaee S, Ghanbari B, Maleki M, Peyrovi H, Bahrani N. Obstacles and facilitators of open visiting policy in intensive care units: a qualitative study. Int J Med Res Health Sci. 2016;5(7S):452–6. [Google Scholar]
- 63.Imanipour M, Heidari Z, Seyedfatemi N, Haghani H. Effectiveness of informational support on anxiety among family carers of patients undergone open heart surgery. Hayat. 2012;18(3):33–43. [Persian] [Google Scholar]
- 64.Nantz S, Hines A. Trauma patients’ family members’ perceptions of nurses’ caring behaviors. J Trauma Nurs. 2015;22(5):249–54. doi: 10.1097/jtn.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 65.Guzzetta CE, Taliaferro E, Proehl JA. Family presence during invasive procedures and resuscitation. J Trauma. 2000;49(6):1157–9. doi: 10.1097/00005373-200012000-00036. [DOI] [PubMed] [Google Scholar]
- 66.Lee LY, Lau YL. Immediate needs of adult family members of adult intensive care patients in Hong Kong. J Clin Nurs. 2003;12(4):490–500. doi: 10.1046/j.1365-2702.2003.00743.x. [DOI] [PubMed] [Google Scholar]
- 67.Ramos FJ, Fumis RR, de Azevedo LC, Schettino G. Intensive care unit visitation policies in Brazil: a multicenter survey. Rev Bras Ter Intensiva. 2014;26(4):339–46. doi: 10.5935/0103-507x.20140052. [DOI] [PMC free article] [PubMed] [Google Scholar]