Abstract
Pelvic fractures are often caused by high-energy injuries and accompanied by hemodynamic instability. Traditional open surgery has a large amount of bleeding, which is not suitable for patients with acute pelvic fracture. Navigation-guided, percutaneous puncture-screw implantation has gradually become a preferred procedure due to its advantages, which include less trauma, faster recovery times, and less bleeding. However, due to the complexity of pelvic anatomy, doctors often encounter some problems when using navigation to treat pelvic fractures. This article reviews the indications, contraindications, surgical procedures, and related complications of this procedure for the treatment of sacral fractures, sacroiliac joint injuries, pelvic ring injuries, and acetabular fractures. We also analyze the causes of inaccurate screw placement. Percutaneous screw placement under navigational guidance has the advantages of high accuracy, low incidence of complications and small soft-tissue damage, minimal blood loss, short hospital stays, and quick recovery. There is no difference in the incidence of complications between surgeries performed by new doctors and experienced ones. However, computer navigation technology requires extensive training, and attention should be given to avoid complications such as screw misplacement, intestinal injury, and serious blood vessel and nerve injuries caused by navigational drift.
Keywords: Computer navigation, Percutaneous puncture, Screw, Pelvic fracture, Sacral fracture, Acetabular fracture, Iliac fracture, Pubic fracture
Core tip: Computer-assisted navigation is a technology used in minimally invasive spinal surgery. It provides advantages such as rapid recovery and minimal trauma. Here, we discuss the indications, contraindications, surgical procedures, and related complications during percutaneous screw fixation for the treatment of sacral fractures, sacroiliac-joint injuries, pelvic ring injuries, and acetabular fractures. The advantages of navigation in the treatment of pelvic fracture are clarified. At the same time, paying attention to navigational drift is also reminded.
INTRODUCTION
There has been a rapid development of minimally invasive technology in orthopedics in recent years, and the advantages of this technology, including less trauma and rapid recovery, have been recognized by both doctors and patients. However, the procedure’s application is limited due to disadvantages such as the need for repeated fluroscopies, extensive clinician training, and high technical requirements. Computer-assisted navigation is a technology that offers a secure method for successfully undertaking minimally invasive techniques. The dislocation rate of screw placement under navigational guidance is 0.1%, which is lower than the traditional screw implantation error rate of 2.6% to 29.5%[1]. In addition, the use of navigational guidance can reduce the amount of radiation exposure experienced by surgeons[2]. Moreover, patient radiation exposure does not increase either, and may even decrease[3]. Although 3-dimensional (3D) scanning of navigation-guided percutaneous punctures may increase scan time, it can reduce unnecessary and repetitive radiation exposure during conventional minimally invasive surgery.
The radiation that a patient receives is affected by the patient’s body mass index, as patients who are overweight may require more energy to be used before a clear image is achieved. Currently, the primary types of computer navigation used in orthopedics are computed tomography (CT)-based navigation, 2-dimensional (2D) fluoroscopy-based navigation, 3D fluoroscopy-based navigation, and electromagnetic navigation (Table 1).
Table 1.
| Type | Advantages | Shortcomings | Applications |
| CT-based navigation | High resolution; preoperative planning and simulation | No real-time imaging; expensive | Spinal pedicle screw implantation; hip and knee replacement |
| 2D-fluoroscopic navigation | Latest image obtained at any time; low cost | Image distortion | Fracture reduction and internal fixation |
| 3D-fluoroscopic navigation | High-resolution three-dimensional image data; real-time high-definition visualization of trajectory | Easy to be occluded by objects during operation; more X-ray needed | Reduction and internal fixation of complex fracture |
| Imageless navigation | No requirement for image registration | Anatomic markers to be exposed; limited reconstruction of bone structure | Hip and knee surgery |
| Electromagnetic navigation | High resolution for soft tissue; no need for a direct line of sight | A stable magnetic field needed | Orthopedic tumor; orthopedic minimally invasive treatment |
| Ultrasound-based navigation | No radiation | Immature technology | Further improvement needed |
CT: Computed tomography; 2D: 2-dimensional; 3D: 3-dimensional.
The application of navigation techniques in orthopedics is common and used for conditions including spinal deformities, spinal degenerative diseases, bone tumors, joint replacements, etc[4,5]. Complex anatomical structures of the pelvis such as narrow corridors, rich muscle-ligament tissue, and neurovascular overlapping intestinal shadows may lead to the insufficient reduction of a fracture or poor screw position. Hence, the therapeutic advantages of navigation for pelvic fractures are evident[6-10]. Therefore, this article reviews the indications, contraindications, surgical procedures, and related complications of navigation-guided percutaneous puncture-screw implantation for the treatment of sacral fractures, sacroiliac joint injuries, pelvic ring injuries, and acetabular fractures. We also analyze the causes of inaccurate screw placement.
APPLICATION OF NAVIGATION IN TREATMENT OF PELVIC FRACTURES
Navigation-assisted percutaneous screw placement for treatment of sacroiliac joints and sacral fractures
Sacroiliac joint injury is often accompanied by a pelvic fracture, and these patients often exhibit unstable hemodynamics as well. Sacroiliac joint screws can be used in narrow channels, however, angle deviation may lead to injury of the sacral foramen or penetration of the bone cortex. Anatomical variants of the sacrum and sacroiliac joint, obesity, excessive bowel gas, and osteoporosis may affect the accuracy of screw placement[2,11]. Traditional minimally invasive screw placement is prone to damaging blood vessels and nerves, the sacral canal, the gastrointestinal tract, and the urogenital system[2]. Although some studies have reported that the sacroiliac joint can be safely repaired without the use of an intraoperative computer-navigation system[12], there are high requirements for both surgeons and surgical positioning accuracy. Therefore, navigation-guided screw placement is conducive to the accurate positioning of the screw and to the safety of the surgery.
Indications and contraindications
Biomechanical technology has shown that navigation-guided percutaneous puncture-screw implantation can provide sufficient stability for pelvic fractures[13]. It is indicated for sacroiliac joint dislocations and Dennis type I and type II sacrum fractures with no displacements or slight displacements. Contraindications include sacral fractures with obvious displacement or high instability, and sacral fractures with obvious neurological dysfunctions. When a fracture deformity score is more than 70, navigation cannot improve the accuracy of screw placement[14,15]. In general, if a fracture displacement is greater than 10 mm, the cross-sectional contact area is reduced by more than 50%, and the safety of a screw placement is significantly reduced[16]. However, when the displacement is more than 10 mm and there is a device that can maintain the reduction, such as a traction bed, a percutaneous screw fixation using navigation for the sacral fracture is feasible[17].
Surgical technique
Patients are anesthetized using general anesthesia and placed in a supine or prone position according to the surgeon’s preference. A reference tracker is fixed to the contralateral iliac wing (with attention given to the position of the tracker to avoid an overabundance of metal artifacts). A 3D scan is then performed, using the fracture site as the center. The acquired images are then matched with the preoperative CT data. The puncture point should be located at the one third position starting from the posterior superior iliac spine to the anterior superior iliac spine of the patient’s posterior pelvic ring. A small skin incision is made under the guidance of navigation. It is important that the incision location is not chosen based on experiences[18,19], as the lateral tension of the patient’s muscle can create pressure on the guide wire cannula, which may lead to incorrect screw placement. After the guide wire sleeve is calibrated, a guide wire (diameter, 3.2 mm) is inserted, and the sleeve is then moved while the needle enters it until the guide wire breaks through the sacroiliac joint. At this point a 6.5 mm-8.0 mm diameter screw is inserted through the guide wire. The process can refer to Figure 1[19].
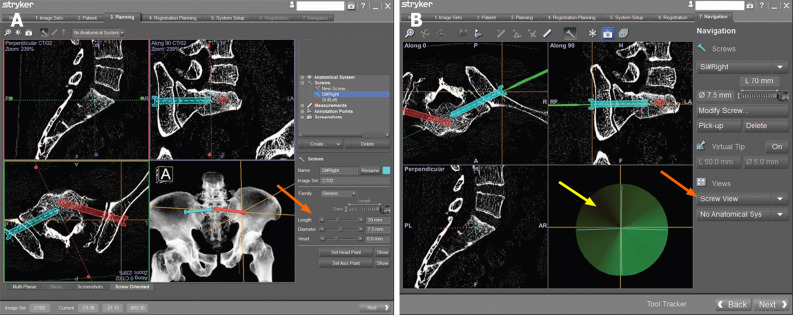
Figure 1.
Procedure of sacral screw implantation. A: Navigation planning to design the length, diameter, and the best trajectory of screws; B: The user interface of the screw view mode of navigation, guiding the screw implantation. When the right lower corner of the image shows green (yellow arrow), it would be the best time to implant a guide wire.
The relative spatial position of the reference tracker and pelvis should not be changed during the operation, which is key to ensuring accurate navigation. If the sacroiliac joint is significantly displaced by more than 10 mm, it can be further fixed according to the method of Takao[6] to ensure that there is no change in relative positioning. When the angle between the screw and the vertical line of the bone surface is too large, the risk of positional error during screw insertion increases[20]. Therefore, pre-drilling with the navigational drilling tool is recommended if the angle of the screw to be inserted is > 35° in the axial position.
Complications
The accuracy of navigation-guided placements is significantly higher than that of conventional percutaneous placements[2]. Ghisla et al[21] followed 21 patients with posterior pelvic rings that had been fixed with sacroiliac screws under the guidance of 3D navigation. They found only one case with cortical destruction; there were no other obvious complications in any of the other patients. Improper placement of S1 and S2 screws can be a devastating complication in sacral-fracture surgery or sacroiliac-joint injury[22]. If the sacral injury is serious, the S2 nerve is more likely to be injured due to a narrow channel. Moreover, rectal injury may also occur during the surgery.
Navigation-assisted percutaneous screw placement in the treatment of pubic-branch fractures
Treating the anterior ring of the pelvis was once controversial. It was thought that surgery is necessary only when the pubic symphysis separated more than 25 mm, thus few pubic-branch fractures would need fixation. In recent years however, biomechanical data has confirmed that the anterior ring of the pelvis bears 30% of the tension from the entire pelvis. Therefore, it is necessary to fix the anterior ring and reconstruct the stability of the pelvis. Traditional treatment methods have included open reduction and internal fixation or limited incision and implantation of a titanium plate by minimally invasive plate osteosynthesis technology. However, patient injury can be substantial, and the economic cost of a titanium plate is higher than a screw, so percutaneous puncture technology is now universally preferred.
Indications and contraindications
Treatment of pubic-branch fractures by percutaneous screw fixation under navigation is indicated when there is no displacement, or slight displacement, of a pubic-branch fracture, and the closed reduction of the pubic branch fracture can reach a functional reduction standard[23]. Treatment using navigation is contraindicated when there is a fracture at the site of needle insertion, an open pelvic fracture, or a comminuted pubic-branch fracture.
Surgical technique
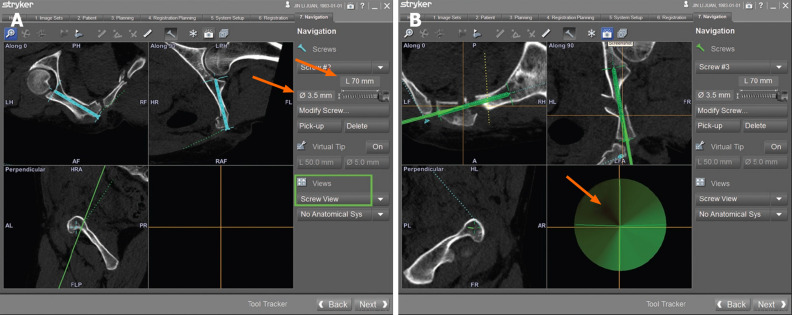
Fractures of the pubic branch are classified into three types according to Nakatani fracture system[24]. The surgical scheme for types I and II is retrograde pubic cannulated screw implantation[25,26], and for type III, it is antegrade implantation of screws. The surgical position of the patient should be supine and general anesthesia is used. After routine disinfection, a reference tracker is fixed on the iliac crest of the healthy side. After activating the tracker on the C-arm, patient, and sleeve, 3D scanning is carried out. The position of the guide-wire sleeve is then monitored in real time using the screw-viewing angle mode (Figure 2[25]). In general, when the pubic branch is fractured at a low position, the needle entry point should be close to the pubic symphysis. When the pubic branch fracture is in a high position, the needle point should be close to the pubic tubercle. If the fracture is a Nakatani III type, the point of insertion should be the midpoint of the line between the vertex of the greater trochanter and the protrusion of the iliac node. After selecting the appropriate puncture point, a 20 mm skin incision should be made. A guide wire is then inserted after determining the accurate insertion point and direction, and a hollow screw is inserted[12]. For men, 6.5 mm screws are safe to use; however, these may penetrate the cortex in women[27].
Figure 2.
Procedure of transpubic screw implantation. A: Navigation planning; B: The user interface of the screw view mode of navigation.
Complications
The accuracy of placement of hollow screws using navigation guidance is significantly higher than that of traditional methods[28,29]. If the reduction of a pubic fracture is poor, the possibility of screw perforation will be greater. Injuries of the spermatic cord, uterine ligament, or neurovascular injury are complications associated with pubic-branch fractures[29,30]. Therefore, care must be taken when making surgical incisions, subcutaneous tissue should be bluntly separated, and soft-tissue protective sleeves should be added when placing screws. In addition, special care needs to be taken to avoid injury to the corona mortis when treating pubic fractures[31]. These can be dangerous vascular injuries that are associated with high mortality[32,33].
Navigation-assisted percutaneous screw placement for acetabular fractures
The treatment of acetabular fractures has always been difficult due to bleeding, the high incidence of postoperative traumatic arthritis[34], heterotopic ossification[35], and other issues. The treatment goal for these fractures is to restore the flatness of the joint surface and stability[36]. If the joint surface can be restored through closed reduction, then a traditional operation is unnecessary. Percutaneous screw fixation under navigational guidance can, however, improve the safety of the surgery and reduce trauma and risk of pressure ulcers[37].
Indications and contraindications
The indications of navigation treatment for acetabular fractures are mainly non-displaced fractures or displaced fractures which can be anatomically reduced by closed reduction[38-42]. Contraindications include comminuted fracture, soft tissue incarceration, and other fractures that cannot be anatomically reduced. In general, open reduction and internal fixation is the standard treatment for acetabular fracture displacement. It is difficult to restore the articular surface via closed reduction if the fracture block is substantially displaced. Articular-surface irregularity is the main factor in the later stage of arthritis, and it has been reported that the risk of arthritis is more than 10%[17], even when satisfactory reduction (displacement < 2 mm[43,44]) has been obtained. Therefore, navigation-guided percutaneous puncture for acetabular fractures should only be applied to non-displaced acetabular fractures or acetabular fractures that can be restored to anatomic reduction following closed reduction[17,45].
Surgical technique
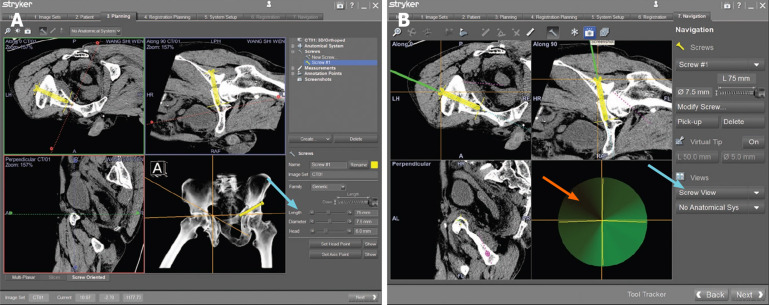
In the treatment of acetabular fractures, the appropriate position (upward, prone, or lateral) is selected according to the surgeon’s preference and general anesthesia is used. A reference tracker is fixed to the anterior, superior iliac spine, or the ischial tuberosity, following routine disinfection, and should then be calibrated and 3D scanned. The data are then matched with the preoperative scanned data. A skin incision is first made using the navigation guide, then a drill-guided pin as long as the screw is inserted. The depth of the screw is then monitored through real-time 3D navigation (Figure 3[46]). After inserting all of the guide pins, several 6.5 mm screws should be implanted, and the safety of the screws be confirmed through standard position fluoroscopy. The retrograde anterior column screw technique is used to treat the low anterior column fracture of the acetabulum. In retrograde pubic screw fixation, a guide wire is used to make a channel, and a probe is used to detect whether there is a perforation of the cortical bone. Only then are a guide wire and a screw inserted[47].
Figure 3.
Procedure of periacetabular screw implantation. A: Navigation planning; B: The user interface of the screw view mode of navigation.
In the process of screw placement, a safety channel is affected by the thickness of the screw and the angle of insertion. With the increase in screw length, the safety channel becomes narrow. It has been reported that the diameter of the anterior column screw is 6.5 mm, which is safe[29,45,48-50]. Morandi et al[47] consider the insertion of screws above 90 mm in the acetabulum to be unsafe because of the need for a larger anterior oblique angle, which can increase the brittleness of the screws. However, short screws can achieve a mechanical strength similar to long screws[45].
Complications
The perforation rate of screw placement under navigational guidance is significantly lower than that under conventional fluoroscopy, and the volume of bleeding is also significantly reduced[42,46,48,51,52]. The decrease in bleeding volume may be related to the decrease in puncture times, surgery choice, and surgical time[17]. In addition, the incidence of heterotopic ossification also decreases, which may be related to surgical choice[53] and time[54]. Under the guidance of 3D navigation, 3D fluoroscopy can be used to observe the reduction during surgery, so as to reduce traumatic arthritis caused by the reduction quality.
CAUSES OF INACCURATE PLACEMENT OF SCREWS IN NAVIGATION-GUIDED PERCUTANEOUS SCREW INSERTION
The main role of navigation is to accurately guide the operator in the placement of screws. However, if it is used or operated incorrectly, the accuracy of the navigation becomes questionable. This is primarily due to: (1) The camera and tracker fixed on the patient do not keep stationary and exhibit relative displacement[19,46]. This scenario may be caused by the tracker not being firmly fixed, or the fracture being displaced after the reduction; (2) Navigation-guided devices are sleeves, not guide wires or screws; (3) The flexibility of the guide wire causes a deviation during insertion[46]; (4) The notch is too small, which causes the guide wire to deviate during insertion, and it cannot be correctly positioned along the expected image-guided track[45,55]; and (5) Soft-tissue wrapping. Without the use of a soft-tissue protective sleeve, the guide wire, drill bit, screw, etc. will be twisted by soft tissue during insertion, which affects the accuracy of the navigation.
Although navigation can provide accurate virtual navigation routes and real-time imaging prompts, even when 3D navigation is used, perforation caused by the guide wire or screw cannot be completely avoided due to the possibility of technical problems, the technical expertise of the operator, or the complexity of the anatomy[55]. Therefore, the operator must combine both tactile feedback and the visual feedback displayed on a computer screen to determine the accuracy of screw placement. The combination of 3D fluoroscope navigation and CT-based preoperative planning enables the operator to successfully insert a guide wire in a short amount of time[17].
CONCLUSION
Percutaneous screw placement under navigational guidance has the advantages of high accuracy, low incidences of complications and small soft-tissue damage, minimal blood loss, short hospital stays, and quick recovery. Under the premise of mastering navigation skills, there is no difference in the incidence of complications between surgeries performed by new doctors and experienced ones in terms of navigation-assisted minimally invasive treatments of pelvic fractures. The use of screws requires that the degree of fracture displacement is not large, and that the screws are able to bear enough shear force. However, computer navigation technology requires extensive training, and attention should be given to avoid complications such as screw misplacement and serious vascular and nerve injuries caused by navigational drift.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interests for this article.
Manuscript source: Invited manuscript
Peer-review started: February 10, 2020
First decision: April 29, 2020
Article in press: May 26, 2020
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A S-Editor: Wang J L-Editor: Wang TQ E-Editor: Liu JH
Contributor Information
Tong Yu, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China.
Xue-Liang Cheng, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China.
Yang Qu, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China.
Rong-Peng Dong, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China.
Ming-Yang Kang, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China.
Jian-Wu Zhao, Department of Orthopedics, the Second Hospital of Jilin University, Changchun 130014, Jilin Province, China. jianwu@jlu.edu.cn.
References
- 1.Balling H. 3D image-guided surgery for fragility fractures of the sacrum. Oper Orthop Traumatol. 2019;31:491–502. doi: 10.1007/s00064-019-00629-8. [DOI] [PubMed] [Google Scholar]
- 2.Berger-Groch J, Lueers M, Rueger JM, Lehmann W, Thiesen D, Kolb JP, Hartel MJ, Grossterlinden LG. Accuracy of navigated and conventional iliosacral screw placement in B- and C-type pelvic ring fractures. Eur J Trauma Emerg Surg. 2020;46:107–113. doi: 10.1007/s00068-018-0990-z. [DOI] [PubMed] [Google Scholar]
- 3.Schuetze K, Eickhoff A, Dehner C, Schultheiss M, Gebhard F, Richter PH. Radiation exposure for the surgical team in a hybrid-operating room. J Robot Surg. 2019;13:91–98. doi: 10.1007/s11701-018-0821-6. [DOI] [PubMed] [Google Scholar]
- 4.Karkenny AJ, Mendelis JR, Geller DS, Gomez JA. The Role of Intraoperative Navigation in Orthopaedic Surgery. J Am Acad Orthop Surg. 2019;27:e849–e858. doi: 10.5435/JAAOS-D-18-00478. [DOI] [PubMed] [Google Scholar]
- 5.Thakkar SC, Thakkar RS, Sirisreetreerux N, Carrino JA, Shafiq B, Hasenboehler EA. 2D versus 3D fluoroscopy-based navigation in posterior pelvic fixation: review of the literature on current technology. Int J Comput Assist Radiol Surg. 2017;12:69–76. doi: 10.1007/s11548-016-1465-5. [DOI] [PubMed] [Google Scholar]
- 6.Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N. Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury. 2014;45:988–994. doi: 10.1016/j.injury.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Wong JSY, Lau JCK, Chui KH, Tiu KL, Lee KB, Li W. Three-dimensional-guided navigation percutaneous screw fixation of fragility fractures of the pelvis. J Orthop Surg (Hong Kong) 2019;27:2309499019833897. doi: 10.1177/2309499019833897. [DOI] [PubMed] [Google Scholar]
- 8.Tonetti J, Jouffroy P, Dujardin F. Reconstruction of pelvic ring and acetabular fractures: What lies ahead? Orthop Traumatol Surg Res. 2019;105:799–800. doi: 10.1016/j.otsr.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Zwingmann J, Hauschild O, Bode G, Südkamp NP, Schmal H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2013;133:1257–1265. doi: 10.1007/s00402-013-1788-4. [DOI] [PubMed] [Google Scholar]
- 10.Xiang Z, Wei D, Liu M, Duan X, Ma J, Fang Y, Kong Q, Huang F, Cen S, Zhong G. [Minimally invasive fixation under computer-assisted navigation for treatment of periacetabular fractures, anterior and posterior pelvic ring fractures] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2015;29:10–13. [PubMed] [Google Scholar]
- 11.Peng KT, Li YY, Hsu WH, Wu MH, Yang JT, Hsu CH, Huang TJ. Intraoperative computed tomography with integrated navigation in percutaneous iliosacral screwing. Injury. 2013;44:203–208. doi: 10.1016/j.injury.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 12.Roetman B, Ilchuk I, Khatib B, Goerigk U, Gothner M. [Precise sacroiliac joint screw insertion without computed tomography, digital volume tomography or navigation systems] Oper Orthop Traumatol. 2019;31:474–490. doi: 10.1007/s00064-019-0607-7. [DOI] [PubMed] [Google Scholar]
- 13.Li B, He J, Zhu Z, Zhou D, Hao Z, Wang Y, Li Q. Comparison of 3D C-arm fluoroscopy and 3D image-guided navigation for minimally invasive pelvic surgery. Int J Comput Assist Radiol Surg. 2015;10:1527–1534. doi: 10.1007/s11548-015-1157-6. [DOI] [PubMed] [Google Scholar]
- 14.Teo AQA, Yik JH, Jin Keat SN, Murphy DP, O'Neill GK. Accuracy of sacroiliac screw placement with and without intraoperative navigation and clinical application of the sacral dysmorphism score. Injury. 2018;49:1302–1306. doi: 10.1016/j.injury.2018.05.027. [DOI] [PubMed] [Google Scholar]
- 15.Ricci, WM, Linn M, Gardner M, McAndrew C. What's New in Orthopaedic Trauma. J Bone Joint Surg Am. 2014;96:1222–1230. [Google Scholar]
- 16.Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2006;20:S37–S43. [PubMed] [Google Scholar]
- 17.Takao M, Hamada H, Sakai T, Sugano N. Clinical Application of Navigation in the Surgical Treatment of a Pelvic Ring Injury and Acetabular Fracture. Adv Exp Med Biol. 2018;1093:289–305. doi: 10.1007/978-981-13-1396-7_22. [DOI] [PubMed] [Google Scholar]
- 18.Khan JM, Lara DL, Marquez-Lara A, Rosas S, Hasty E, Pilson HT. Intraoperative CT and Surgical Navigation for Iliosacral Screws: Technique for Patients With Sacral Dysmorphism. J Orthop Trauma. 2018;32 Suppl 1:S24–S25. doi: 10.1097/BOT.0000000000001213. [DOI] [PubMed] [Google Scholar]
- 19.Yu T, Zheng S, Zhang X, Wang D, Kang M, Dong R, Qu Y, Zhao J. A novel computer navigation method for accurate percutaneous sacroiliac screw implantation: A technical note and literature review. Medicine (Baltimore) 2019;98:e14548. doi: 10.1097/MD.0000000000014548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takao M, Hamada H, Sakai T, Sugano N. Factors influencing the accuracy of iliosacral screw insertion using 3D fluoroscopic navigation. Arch Orthop Trauma Surg. 2019;139:189–195. doi: 10.1007/s00402-018-3055-1. [DOI] [PubMed] [Google Scholar]
- 21.Ghisla S, Napoli F, Lehoczky G, Delcogliano M, Habib N, Arigoni M, Filardo G, Candrian C. Posterior pelvic ring fractures: Intraoperative 3D-CT guided navigation for accurate positioning of sacro-iliac screws. Orthop Traumatol Surg Res. 2018;104:1063–1067. doi: 10.1016/j.otsr.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the "vestibule" concept. J Orthop Trauma. 2000;14:264–269. doi: 10.1097/00005131-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Liu HS, Duan SJ, Liu SD, Jia FS, Zhu LM, Liu MC. Robot-assisted percutaneous screw placement combined with pelvic internal fixator for minimally invasive treatment of unstable pelvic ring fractures. Int J Med Robot. 2018;14:e1927. doi: 10.1002/rcs.1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Starr AJ, Nakatani T, Reinert CM, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: what predicts fixation failure? J Orthop Trauma. 2008;22:81–87. doi: 10.1097/BOT.0b013e318162ab6e. [DOI] [PubMed] [Google Scholar]
- 25.Yu T, Qu Y, Zhang XW, Wang Y, Jiang QY, Jiang ZD, Zhu XJ, Zhao JW. A screw-view model of navigation aid retrograde transpubic screw fixation for anterior pelvic ring fracture: A case report with 28 months follow-up and technical note. Medicine (Baltimore) 2018;97:e13646. doi: 10.1097/MD.0000000000013646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quercetti N, 3rd, Horne B, DiPaolo Z, Prayson MJ. Gun barrel view of the anterior pelvic ring for percutaneous anterior column or superior pubic ramus screw placement. Eur J Orthop Surg Traumatol. 2017;27:695–704. doi: 10.1007/s00590-016-1864-x. [DOI] [PubMed] [Google Scholar]
- 27.Chen KN, Wang G, Cao LG, Zhang MC. Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: a study of 164 virtual three-dimensional models. Injury. 2009;40:1067–1072. doi: 10.1016/j.injury.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 28.Gao H, Luo CF, Hu CF, Zhang CQ, Zeng BF. Minimally invasive fluoro-navigation screw fixation for the treatment of pelvic ring injuries. Surg Innov. 2011;18:279–284. doi: 10.1177/1553350611399587. [DOI] [PubMed] [Google Scholar]
- 29.Stevenson AJ, Swartman B, Bucknill AT. Percutaneous internal fixation of pelvic fractures. Unfallchirurg. 2017;120:10–18. doi: 10.1007/s00113-016-0225-x. [DOI] [PubMed] [Google Scholar]
- 30.Zhou KH, Luo CF, Chen N, Hu CF, Pan FG. Minimally invasive surgery under fluoro-navigation for anterior pelvic ring fractures. Indian J Orthop. 2016;50:250–255. doi: 10.4103/0019-5413.181791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stavropoulou-Deli A, Anagnostopoulou S. Corona mortis: anatomical data and clinical considerations. Aust N Z J Obstet Gynaecol. 2013;53:283–286. doi: 10.1111/ajo.12076. [DOI] [PubMed] [Google Scholar]
- 32.Rich C, Rayner J, Raukar N. Nondisplaced pubic ramus fracture associated with exsanguination and death. Am J Emerg Med. 2018;36:342.e1–342.e2. doi: 10.1016/j.ajem.2017.10.062. [DOI] [PubMed] [Google Scholar]
- 33.Garrido-Gómez J, Pena-Rodríguez C, Martín-Noguerol T, Hernández-Cortes P. Corona mortis artery avulsion due to a stable pubic ramus fracture. Orthopedics. 2012;35:e80–e82. doi: 10.3928/01477447-20111122-25. [DOI] [PubMed] [Google Scholar]
- 34.Cahueque M, Martínez M, Cobar A, Bregni M. Early reduction of acetabular fractures decreases the risk of post-traumatic hip osteoarthritis? J Clin Orthop Trauma. 2017;8:320–326. doi: 10.1016/j.jcot.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salar N, Bilgen MS, Bilgen ÖF, Ermutlu C, Eken G, Durak K. Total hip arthroplasty for acetabular fractures: "Early Application". Ulus Travma Acil Cerrahi Derg. 2017;23:337–342. doi: 10.5505/tjtes.2016.55675. [DOI] [PubMed] [Google Scholar]
- 36.Hsu CL, Chou YC, Li YT, Chen JE, Hung CC, Wu CC, Shen HC, Yeh TT. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int Orthop. 2019;43:1969–1976. doi: 10.1007/s00264-018-4111-8. [DOI] [PubMed] [Google Scholar]
- 37.Fritz A, Gericke L, Höch A, Josten C, Osterhoff G. Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury. 2020;51:352–356. doi: 10.1016/j.injury.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 38.Hong G, Cong-Feng L, Cheng-Fang H, Chang-Qing Z, Bing-Fang Z. Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based computerized navigation. Arch Orthop Trauma Surg. 2010;130:1177–1183. doi: 10.1007/s00402-010-1095-2. [DOI] [PubMed] [Google Scholar]
- 39.Crowl AC, Kahler DM. Closed reduction and percutaneous fixation of anterior column acetabular fractures. Comput Aided Surg. 2002;7:169–178. doi: 10.1002/igs.10040. [DOI] [PubMed] [Google Scholar]
- 40.Stöckle U, König B, Dahne M, Raschke M, Haas NP. [Computer assisted pelvic and acetabular surgery. Clinical experiences and indications] Unfallchirurg. 2002;105:886–892. doi: 10.1007/s00113-002-0438-z. [DOI] [PubMed] [Google Scholar]
- 41.He J, Tan G, Zhou D, Sun L, Li Q, Yang Y, Liu P. Comparison of Isocentric C-Arm 3-Dimensional Navigation and Conventional Fluoroscopy for Percutaneous Retrograde Screwing for Anterior Column Fracture of Acetabulum: An Observational Study. Medicine (Baltimore) 2016;95:e2470. doi: 10.1097/MD.0000000000002470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ochs BG, Gonser C, Shiozawa T, Badke A, Weise K, Rolauffs B, Stuby FM. Computer-assisted periacetabular screw placement: Comparison of different fluoroscopy-based navigation procedures with conventional technique. Injury. 2010;41:1297–1305. doi: 10.1016/j.injury.2010.07.502. [DOI] [PubMed] [Google Scholar]
- 43.Simonian PT, Routt ML Jr, Harrington RM, Tencer AF. Internal fixation of the unstable anterior pelvic ring: a biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J Orthop Trauma. 1994;8:476–482. [PubMed] [Google Scholar]
- 44.Keil H, Aytac S, Grützner PA, Franke J. Intraoperative Imaging in Pelvic Surgery. Z Orthop Unfall. 2019;157:367–377. doi: 10.1055/a-0732-5986. [DOI] [PubMed] [Google Scholar]
- 45.Chui KH, Chan CCD, Ip KC, Lee KB, Li W. Three-dimensional navigation-guided percutaneous screw fixation for nondisplaced and displaced pelvi-acetabular fractures in a major trauma centre. Int Orthop. 2018;42:1387–1395. doi: 10.1007/s00264-017-3659-z. [DOI] [PubMed] [Google Scholar]
- 46.Zhao JW, Yu T, Chu GY, Zhang XW, Wang Y, Zhu XJ, Jiang QY, Jiang ZD, Wang DS. Accuracy and safety of percutaneous periacetabular screw insertion using screw view model of navigation in acetabular fracture: A case report. Medicine (Baltimore) 2018;97:e13316. doi: 10.1097/MD.0000000000013316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morandi MM, Daily D, Kee C, Barton RS, Solitro GF. Safe Supra-Acetabular Pin Insertion in Relation to Intraosseous Depth. J Orthop Res. 2019;37:1790–1797. doi: 10.1002/jor.24323. [DOI] [PubMed] [Google Scholar]
- 48.Chen H, Tang P, Yao Y, She F, Wang Y. Anatomical study of anterior column screw tunnels through virtual three-dimensional models of the pelvis. Eur J Orthop Surg Traumatol. 2015;25:105–110. doi: 10.1007/s00590-013-1410-z. [DOI] [PubMed] [Google Scholar]
- 49.Feng X, Fang J, Lin C, Zhang S, Lei W, Li Y, Tang S, Chen B. Axial perspective to find the largest intraosseous space available for percutaneous screw fixation of fractures of the acetabular anterior column. Int J Comput Assist Radiol Surg. 2015;10:1347–1353. doi: 10.1007/s11548-015-1149-6. [DOI] [PubMed] [Google Scholar]
- 50.Attias N, Lindsey RW, Starr AJ, Borer D, Bridges K, Hipp JA. The use of a virtual three-dimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures. J Bone Joint Surg Br. 2005;87:1520–1523. doi: 10.1302/0301-620X.87B11.16614. [DOI] [PubMed] [Google Scholar]
- 51.Xu P, Wang H, Liu ZY, Mu WD, Xu SH, Wang LB, Chen C, Cavanaugh JM. An evaluation of three-dimensional image-guided technologies in percutaneous pelvic and acetabular lag screw placement. J Surg Res. 2013;185:338–346. doi: 10.1016/j.jss.2013.05.074. [DOI] [PubMed] [Google Scholar]
- 52.Luo CF, Zhou KH, Gao H, Hu CF, Chen J, Zeng BF. [Minimally invasive surgery of pelvic-acetabular fractures with fluoro-navigation] Zhonghua Yi Xue Za Zhi. 2007;87:3030–3034. [PubMed] [Google Scholar]
- 53.Elhassan Y, Abdelhaq A, Piggott RP, Osman M, McElwain JP, Leonard M. Heterotopic Ossification following acetabular fixation: Incidence and risk factors: 10-year experience of a tertiary centre. Injury. 2016;47:1332–1336. doi: 10.1016/j.injury.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 54.Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. J Bone Joint Surg Br. 2011;93:229–236. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 55.Wong JM, Bewsher S, Yew J, Bucknill A, de Steiger R. Fluoroscopically assisted computer navigation enables accurate percutaneous screw placement for pelvic and acetabular fracture fixation. Injury. 2015;46:1064–1068. doi: 10.1016/j.injury.2015.01.038. [DOI] [PubMed] [Google Scholar]
- 56.Kubicek J, Tomanec F, Cerny M, Vilimek D, Kalova M, Oczka D. Recent Trends, Technical Concepts and Components of Computer-Assisted Orthopedic Surgery Systems: A Comprehensive Review. Sensors (Basel) 2019;19:5199. doi: 10.3390/s19235199. [DOI] [PMC free article] [PubMed] [Google Scholar]