Abstract
Purpose
The COVID-19 pandemic transformed the personal and professional lives of radiology trainees. The purpose of this study was to broadly summarize the impact of COVID-19 on radiology trainees and their training programs via data collected during the early pandemic.
Materials and Methods
An online survey was distributed to radiology chief residents in residencies throughout North America with responses collected between March 20th, 2020 and May 15th, 2020, which coincided with the development of initial COVID-19 peaks in North America. A subset of COVID-19 pandemic questions included resident wellness, imaging opinions, residency infrastructure change, and opinions regarding the Core Exam delay.
Results
One hundred forty chief residents from 86 institutions responded to COVID-19-related questions. Nearly all responding programs (99%; 85/86) reported institutional positive cases of COVID-19. Most residents (94%; 132/140) thought laboratory testing provided more value than imaging. Fifty-seven percent of respondents (80/140) would use COVID-19-related terminology when encountering chest CT findings supportive of viral pneumonia in symptomatic patients. There was little reported change in the number of residents on call (no change reported in >80% of programs). Fifty-nine percent of residents (83/140) reported increased stress related to the COVID-19 pandemic. The majority of programs (93%) had fewer residents on service (80/86 responding programs).
Conclusions
COVID-19 dramatically affected radiology residencies during the early pandemic period. As we enter future phases of the COVID-19 pandemic, careful thought should also be given to rebuilding the radiology resident experience.
Introduction
A survey is distributed to chief residents in North America every spring to characterize residency training environments broadly.1 In 2020, the survey distribution coincided with the preparation and active management of the COVID-19 pandemic and followed the rise in the incidence of new COVID-19 diagnoses throughout the United States. On March 11th, 2020, the World Health Organization declared the COVID-19 pandemic.2 On March 17th, 2020, the American Board of Radiology (ABR) announced that the Core Exam would be delayed from its late May/early June administration until “at least” September 1st, 2020.3 The survey was distributed to chief residents on March 20th, 2020. This allowed the survey to capture the impact of the early pandemic on radiology residents and their training programs. This is important because while suggestions have been made regarding the imaging of patients,4 preferred reporting of suspicious findings,5 and adjustments to radiology training programs,6 there is a lack of organized cross-sectional information regarding whether changes have actually been implemented and what their effects were on the radiology trainee experience. The purpose of this study is to summarize the responses of the COVID-19-related survey questions.
Materials and Methods
An annual anonymous online electronic survey using SurveyMonkey (Palo Alto, CA) was distributed to chief residents across North America via e-mail. In 2020, a subset of questions was included to investigate trainee sentiment, and program environment and response, in light of the COVID-19 pandemic. Our Institutional Review Board (IRB) designated this study as nonhuman research and exempt. The survey consisted of 108 total questions, 10 of which were designated as COVID-19-related questions. Presented data includes chief resident survey responses collected between March 20th, 2020, and May 15th, 2020, totaling 8 weeks. Although the pandemic is still in progress at the time of writing this manuscript, the data collection period likely represents the initiation and acceleration phases of COVID-19 in the United States7 (Fig 1 ). For select data, responses were stratified temporally into first half (March 20th, 2020 through April 17th, 2020) and second half (April 18th, 2020 through May 15th, 2020). Respondents were asked to provide their residency program names to identify responses from multiple chief residents within a single program. However, individuals remained anonymous to maximize the accuracy of objective and subjective responses. COVID-19 specific questions targeted the following areas: (i) changes to resident and attending staffing, residency program education, and call coverage; (ii) trainee sentiment and well-being; (iii) trainee perspectives on the value of imaging for COVID-19; and (iv) trainee perspectives on reporting COVID-19 related imaging findings. Additionally, the ABR announced on March 17th, 2020 that the Core Exam will be delayed “at least” until September 1st, 2020.3 Questions regarding the Core Exam delay were also incorporated. A list of the included COVID-19-related questions is shown in Supplemental Table 1.
FIG 1.
The timing of responses in relation to the US curve during the early COVID-19 pandemic. Data are represented as new daily confirmed COVID-19 cases (A) and cumulative cases daily (B). Most responding programs (95%) and individuals (96%) reported from institutions in the United States. The first half and second half in collection are represented in white and grey respectively. Data adapted from the CDC7.
If a single institution had multiple responding chief residents, the most recent response was used for institution-specific queries. Select data, including chest CT reporting patterns of COVID-19, resident stress, and reduction of radiology residents on service, were grouped by region, as defined by the US Census Bureau (Northeast, West, Midwest, and South). Responses from Mexico were grouped with the Western United States and responses from Canada were grouped with the Northeastern United States. These same select variables, including chest CT reporting patterns of COVID-19, resident stress, and reduction of radiology residents on service, were also analyzed with a Z test for the proportion of individuals that responded during weeks 1-4 (March 20th, 2020 through April 17th, 2020) vs weeks 5-8 (April 18th, 2020 through May 15th, 2020) of the survey to assess for temporal differences in response rates. The value of laboratory testing vs the value of imaging was also analyzed with the Z test.
Results
Responses
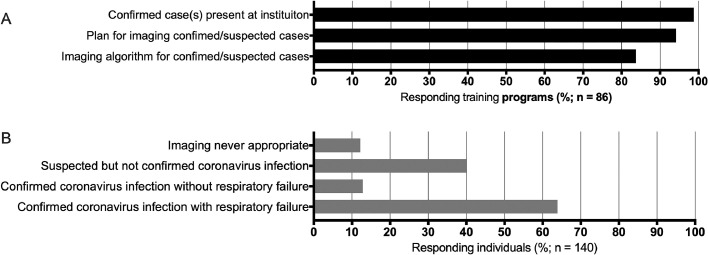
One hundred forty chief residents from 86 institutions responded to the COVID-19-related questions. Nearly all responding programs (99%; 85/86 programs) reported positive cases of COVID-19 at their institution (Fig 2 A). The single institution that did not report a positive case was in the first week of the survey (March 20th, 2020 through March 26th, 2020). Most responding institutions (81/86 programs; 94%) had an action plan for imaging patients with suspected COVID-19 (Fig 2A). Many responding programs reported the use of institutional algorithms for imaging patients with suspected or confirmed infection (84% 72/86 programs).
FIG 2.
Most programs had confirmed COVID-19 cases and a plan for imaging (A), and individuals have variable sentiment on imaging appropriateness (B). Respondents were allowed to choose multiple answers (ie, ‘select all that apply’).
Imaging Patients with Suspected or Confirmed COVID-19
Responding chief residents had variable sentiments on imaging appropriateness (Fig 2) and CT terminology for reporting findings that may be seen with COVID-19 (Fig 3 ). Sixty-four percent of respondents (85/140) indicated that confirmed COVID-19 cases with respiratory failure would be an appropriate indication for imaging. Few respondents (13%; 18/140) indicated that imaging is appropriate in patients with confirmed COVID-19 without respiratory failure, and 40% (56/140 respondents) indicated that suspected but not confirmed COVID-19 is an appropriate indication for imaging (Fig 2).
FIG 3.
Most trainees report that laboratory testing provides more diagnostic value for COVID-19 than imaging (A) and sentiment regarding use of pandemic-related CT reporting terminology is variable across North America (B).
Regarding resident perceptions about imaging's value in COVID-19 diagnosis, most residents (94%; 132/140) responded that laboratory testing provided more value than imaging. Some residents (43%; 60/140) noted that they would not use the terms “coronavirus” or “COVID-19” when encountering ground-glass opacities or consolidation on CT in a patient with symptoms; some reported that imaging could not differentiate an infectious organism, and suggested use of less specific verbiage such as “viral pneumonia.” Other respondents (57%; 80/140) reported they would use such terminology, with stated rationale including exposure risks and high local disease prevalence in an active pandemic (indicated in a free comment box). The geographic distribution of CT terminology sentiments is demonstrated in Figure 3.
Program Staffing, Resident Presence, and Call Changes
The majority of programs (93%) had fewer residents on service (80/86 responding programs) and more resident days off at home (69%; 59/86 responding programs, Fig 4 A-B). There were variable changes in resident and attending call coverage, summarized in Figure 4A. There was little reported change in the number of residents on call, and the duration of resident call shifts (no change reported in >80% of programs).
FIG 4.
COVID-19 related staffing changes in North American radiology trainees and training programs. Pooled data from 86 programs, grouped by overall responses (A) and geographic distribution (B).
Resident Wellness
Fifty-nine percent of responding individuals (83/140) reported increased levels of stress related to the COVID-19 pandemic. On a program level, 43% (37/86 responding programs) indicated that residents had issues with childcare, and 24% (21/86 responding programs) noted that the COVID-19 pandemic was associated with loss of vacation. These stress, childcare difficulty, and loss of vacation data are summarized in Figure 5 .
FIG 5.
Well-being related parameters vary between programs and participants during the COVID-19 pandemic. Programs reported variable vacation loss and childcare difficulties (A) and most individuals reported increased levels of stress (B). There was reported geographic variability in stress (C) and a decreased percentage of individuals reporting stress during the last half of the survey (D).
Resident Educational Experience During the COVID-19 Pandemic
Fifty-nine percent of responding programs (51/86) reported fewer educational conferences. Nearly all responding programs (94%; 81/86 responding programs) used video conferencing software for educational conferences. A minority of respondents (36%; 50/140 responding individuals) preferred video over an in-person educational conference. Some programs (37%) reported using video conferencing software for readout (32/86 responding programs). These data are summarized in Figures 6 A and B.
FIG 6.
COVID-19 pandemic impact on radiology trainee education (A), learning style preference (B), and reported expected effects on the 2020 Core Exam cohort (C).
ABR Core Exam Rescheduled
Responses regarding ABR Core Exam rescheduling are shown in Figure 6C. The majority (90%) of respondents thought the Core Exam rescheduled for the fall would increase stress in fourth-year radiology residents (126/140 respondents). Most thought the Core Exam rescheduling would result in a worse educational experience for fourth-year radiology residents (74%; 104/140 respondents), and 3 respondents (2%) thought it would result in a better educational experience. Most thought the Core Exam rescheduling would result in scheduling difficulties along with those highlighted in Figure 6C. Forty-eight percent (67/140 respondents) thought that the ABR would seriously re-evaluate if the Core Exam should be administered exclusively at current testing sites in Tucson and Chicago.
Weeks 1-4 versus 5-8 patterns
There was no significant difference between residents who would not use “COVID-19” or “coronavirus” describing possible positive findings in a chest CT dictation (35 of 63 residents [56%] in the first 4 weeks would not use COVID-19 terminology compared to 45 of 77 residents [58%] in the last 4 weeks; p= 0.73). During the same time, there was a slight increase in programs with residents off service in the last 4 (weeks 1-4 = 27 of 31 programs [87%] vs weeks 5-8 = 53 of 55 programs [96%]; p = 0.11). During weeks 1-4, 60 of 63 residents (95%) thought laboratory testing for COVID-19 (ie, reverse transcription-polymerase chain reaction [RT-PCR]) was more valuable than imaging for diagnosis, compared to 72 of 77 residents (94%) during weeks 5-8 (p = 0.66). There was less resident reported stress in the last 4 weeks compared to the first 4 weeks (weeks 1-4 = 43 of 63 residents [68%] reported increased stress vs weeks 5-8 = 40 of 77 residents [52%]), which did not achieve statistical significance at p < 0.05 (of note, significance would be met at p = 0.051).
Discussion
This survey provides information regarding radiology trainee experience and sentiment during the early COVID-19 pandemic. These data are important because they confirm that radiology departments implemented changes in practice to address COVID-19. However, we observed variability in response to several queries, including CT reporting style, imaging appropriateness, and staffing changes during the early pandemic. Furthermore, these data confirm that social distancing measures, along with reductions in volumes, have impacted the resident experience, including resident well-being and education.
Survey data collection during the early COVID-19 pandemic
A pandemic of this scale and gravity has not been encountered in contemporary history. As such, we did not have prior experiences to draw from, nor did we have the benefit of hindsight when we formulated the survey questions (Fig. 1A and B). At the time of distribution, on March 20th, 2020, there were just over 15,000 confirmed cases in the United States, compared to over 1.4 million at the time of submission of this manuscript in May 2020.7 Thus, a retrospective analysis may provide a more comprehensive assessment of the impact of COVID-19 on radiology training programs. On the other hand, this timing is a strength because it allowed the survey to obtain multi-institutional perspectives regarding radiology management during the likely initiation and acceleration phases of the overall US infection curve. It is important to note, that although we display the overall US infection curve, it does not provide the granularity of local peak timing across the continent, which is highly variable; this may affect responses of imaging departments. Regardless, we observed that only 1 institution did not have confirmed cases of COVID-19, and that single report was obtained during the first week of the survey.
Resident sentiment regarding imaging in COVID-19
The overwhelming majority of respondents (94%) in the current survey indicated that laboratory testing provided more value than imaging for COVID-19 diagnosis. This is important because it clarifies sentiment regarding imaging's value for diagnosing COVID-19. Furthermore, this survey found variability in imaging's perceived value for different aspects of COVID-19 related management, particularly initial diagnosis.
The Diamond Princess cruise ship study highlights the challenges of COVID-19 diagnosis, including through clinical suspicion, laboratory testing, and imaging.8 At one time, the Diamond Princess had arguably the highest concentration of patients with COVID-19 in the world, which provided the opportunity to compare laboratory testing via RT-PCR with CT imaging findings in a relatively large patient cohort. Several RT-PCR confirmed cases had lung opacities on chest CT but were reportedly completely asymptomatic. On the other hand, some patients with RT-PCR-confirmed infections and symptoms had normal chest CTs. These data suggest that imaging alone is not particularly sensitive for diagnosing COVID-19. This is in contrast with one of the earliest COVID-19 related imaging diagnostic utility studies that suggested chest CT may be a primary tool for detecting COVID-19 given its reported sensitivity of 97%.9 However, some suggest the early literature was possibly hampered by selection bias via preferential imaging of patients with severe symptoms, which would increase CT's sensitivity for COVID-19 diagnosis. In any case, the COVID-19 imaging literature has rapidly evolved.10
Systematic reviews have identified bilateral ground-glass opacities as one of the most encountered CT patterns in COVID-19.11 Even so, these findings are nonspecific and can be seen in many other disease entities, including non-COVID-19 viral pneumonia.12 This poses a dilemma for radiologists encountering lung opacities during the COVID-19 pandemic. If imaging cannot reliably identify a specific infectious agent, should a radiologist even include the terms “coronavirus” or “COVID-19” in a radiology report in an unconfirmed patient with appropriate symptomatology? We asked this question, and a slight minority (43%) indicated that they would not use such terminology. Several of these individuals indicated rationale via free response, stating that imaging cannot differentiate an infectious organism and suggested the use of less specific verbiage such as “viral pneumonia.” On the other hand, some individuals that would use disease-specific terminology (ie, “coronavirus”) indicated that their rationale included high local disease prevalence during a pandemic of a known infectious agent. Although attending COVID-19 reporting sentiment was not assessed, resident reporting sentiment may mirror that of attendings. Some residents indicated that the desired use of COVID-19 specific verbiage was directed by their institution's cardiothoracic radiology section. Near the end of our data collection period, a description of CO-RADS, a standardized reporting system for reporting COVID-19 on CT chest, was published.13 Future studies reporting utility of CO-RADS, and potential modifications, may prove useful for further characterization of COVID-19, determination of utility moving forward in the current pandemic, and potential application in other disease entities.
Staffing and call changes during the pandemic
The majority of programs (93%) reported a reduced number of residents on clinical service and more resident days off at home (77%). Reducing radiology resident presence for most institutions was a necessary measure to decrease the risk of transmission and thus help “flatten the curve.” Ultimately, efforts to “flatten the curve” are directed at keeping the number of cases requiring medical treatment below a theoretical line representing healthcare capacity. In this paradigm, an infected healthcare worker may serve as a “double-hit”; they may both accelerate the infection curve and decrease healthcare capacity. Reducing infections in healthcare workers is critical. In line with the importance of social distancing in healthcare workers, most programs reported decreased resident staffing in the first half of data collection, and nearly all in the last half. However, our data suggested that there were not dramatic changes to the time and duration of resident call. Although we did not explicitly ask if programs’ call structures were changed, only a minority of responding programs indicated greater or fewer number of residents or attendings on call (<20% in all categories). In some cases, residents may have been reassigned to nonradiology services. We did not query reassignment in this survey, and retrospective analysis may identify the frequency of reassignment in this pandemic.
Well-being and stress during the pandemic
A slight majority of responding individuals (59%) noted an increased level of stress attributed to the COVID-19 pandemic. Contributing factors to increased stress were not thoroughly investigated, and further studies may be helpful for future crises. However, childcare is a topic we queried. Childcare during the COVID-19 pandemic has proven to be challenging for many, including healthcare workers. Schools, libraries, and childcare facilities closed across the continent, while many healthcare workers worked on-site or remotely. The fear of becoming infected at work, and bringing illness home to family and children, is common to all healthcare workers, including radiology residents. Depending on the circumstance, the demands of healthcare workers may be compounded by home education requirements for older children, and the safeguarding and interaction needed for younger children. Furthermore, most healthcare workers likely did not have an emergency childcare plan for this pandemic. A study published in 2014 querying general healthcare workers’ response to a hypothetical disaster, such as an earthquake or influenza pandemic, reported that only 28% of those who would need childcare have an emergency childcare plan in place.14 In our study, nearly half of the respondents reported known childcare related problems at their own institution. However, we expect this number is lower than in reality, because not all chief residents have children or may not be privy to the experiences of colleagues with children. A retrospective assessment of childcare challenges faced by those with children may be more illustrative of the COVID-19 pandemic's impact on the well-being of families with children. Coronavirus outbreaks, although not to the scale of SARS-CoV-2, have occurred approximately every decade for the past 30 years.15 This may happen again. Here we did not objectively assess program's means to combat stress and decreased social interactions, or their success; information which is vital to know for future emergencies. Nonetheless, we recommend that when institutions develop and adjust future disaster plans, they take into account potential challenges affecting well-being, including childcare for healthcare workers.
Resident education and the Core Exam
Resident education has been affected by the COVID-19 pandemic, as residents broadly report spending less time on service, which reduces the benefit of live cases and individualized teaching. Furthermore, economic hardship may have caused decreased availability of support staff, consequently redirecting faculty from teaching to administrative duties. In keeping with this, many respondents reported an overall reduced number of conferences. But, efforts have been made to preserve radiology trainee education, namely through videoconferencing. Coupled with the digital nature of radiology, videoconferencing facilitates flexibility. Some institutions reported videoconference use for resident readout, and nearly all institutions reported videoconference use for education. By necessity, the COVID-19 pandemic likely lowered the threshold for videoconference use, which may continue after the fear of infection subsides. Videoconferencing may be particularly advantageous for multidisciplinary conferences (eg, tumor board). Many multidisciplinary conferences draw individuals from different parts of the hospital, and members on site may have significant transit times; videoconferencing largely eliminates this problem. Furthermore, videoconferencing facilitates interactions beyond regular work hours and traditional meeting locations, which may be helpful for projects requiring collaboration.
Resident evaluation, much like resident education, has also been affected by the COVID-19 pandemic. The ABR announced that the Core Exam would be delayed until the fall (“at least until September 1st”) shortly before this survey was disseminated.3 Since then, plans have evolved, but residents expressed their opinions on the current survey, which included expected increased stress for fourth years, challenges with studying, and a worse educational experience. Another consideration is the possibility that 2 classes will prepare and sit for the Core Exam in 1 academic year; R4s in fall 2020 and R3s in spring 2021. Of note, the first iteration of the Core Exam had its primary administration in fall 2014. Anecdotally, the timing of that examination required radical call changes at our institution. The current study indicates that radical changes for the 2020-2021 call schedule are expected. We also asked residents if they expect the ABR will re-evaluate the Core Exam location. Currently, the Core Exam is offered in 2 locations; Chicago and Tucson. However, what if secondary peaks in COVID-19 occur at the time of the rescheduled examination? If institutional travel bans are in place, will exceptions be granted for examinees? In addition to potential safety concerns, travel and lodging fees for the ABR examination are not trivial, and many currently experience increased financial strain related to the COVID-19 pandemic. Further exploration of the opinions regarding ABR-mediated examinations would help elucidate the demand and feasibility for more local options in the current pandemic and beyond.
Limitations
There are several general limitations to the presented data. Not all institutions are accounted for, and resident perspective and experiences vary between and within institutions. Furthermore, the COVID-19 pandemic evolved rapidly during the survey and continues to evolve. In many regards, we did not predict COVID-19’s effect on the healthcare system at the time of survey design. For example, we did not explore if radiology trainees were reassigned to other specialties, nor did we identify the most substantial sources of stress. Future retrospective surveys could be instrumental for broadly determining how programs were most impacted, what challenges and triumphs were experienced, and how radiology training will be different after this pandemic.
In conclusion, these findings serve as an important reminder that radiology resident training has rapidly and, in many respects, drastically changed. As we enter future phases of the COVID-19 pandemic, including containment and ultimately recovery, careful thought should also be given to rebuilding the radiology resident experience.
Disclosures
All other authors claim no relevant disclosures or conflicts of interest related to the present article. RLW received personal fees from Clarity Pharmaceuticals outside the submitted work. DHB and MJH received salary support from National Institutes of Health TOP-TIER grant T32-EB021955 during the study design period.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1067/j.cpradiol.2020.06.012.
Appendix. Supplementary materials
References
- 1.Ballard DH, Summers D, Hoegger MJ, et al. Results of the 2019 survey of the American Alliance of Academic Chief Residents in radiology. Acad Radiol. 2020 doi: 10.1016/j.acra.2020.04.042. Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Timeline - COVID-19. World Health Organization Website. Available at: https://www.who.int/news-room/detail/27-04-2020-who-timeline—covid-19. Accessed May 18, 2020.
- 3.Coronavirus Updates. American Board of Radiology Website. 2020. Available at:https://www.theabr.org/announcements/coronavirus-updates. Accessed June 11, 2020.
- 4.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: A multinational consensus statement from the Fleischner Society. Radiology. 2020;296:172–180. doi: 10.1148/radiol.2020201365. https://pubmed.ncbi.nlm.nih.gov/32255413/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology. 2020;2 doi: 10.1097/RTI.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alvin MD, George E, Deng F, et al. The Impact of COVID-19 on radiology trainees. Radiology. 2020 doi: 10.1148/radiol.2020201222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention Website. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed May 18, 2020.
- 8.Inui S, Fujikawa A, Jitsu M, et al. Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiology. 2020;2 doi: 10.1148/ryct.2020204002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raptis CA, Hammer MM, Short RG, et al. Chest CT and coronavirus disease (COVID-19): A critical review of the literature to date. AJR Am J Roentgenol. 2020:1–4. doi: 10.2214/AJR.20.23202. [DOI] [PubMed] [Google Scholar]
- 11.Salehi S, Abedi A, Balakrishnan S, et al. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 12.Hope MD, Raptis CA, Shah A, et al. >Six signatories. A role for CT in COVID-19? What data really tell us so far. Lancet. 2020;395:1189–1190. doi: 10.1016/S0140-6736(20)30728-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS – A categorical CT assessment scheme for patients with suspected COVID-19: definition and evaluation. Radiology. 2020 doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charney RL, Rebmann T, Flood RG. Emergency childcare for hospital workers during disasters. Pediatr Emerg Care. 2015;31:839–843. doi: 10.1097/PEC.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 15.Perlman S. Another decade, another coronavirus. N Engl J Med. 2020;382:760–762. doi: 10.1056/NEJMe2001126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.